Ahmed MH A’zzaw
FCABMS (Uro.)Senior Lecturer
College of Medicine
University of Mosul
Scrotal Pathologies
AnatomyAnatomy
Incompletely descended testis (Undescended Testis):
The testis is arrested in some part of its path to the scrotum.Incidence: 4% of boys are born with one or both testes incompletely descended.
Half of these reach the scrotum during the first month of life.
two thirds of these reach the scrotum during the first three months of life
incidence of testicular maldescent at the age of one year is around 1 per cent
In 10% of unilateral cases there is a family history.
Pathology
The epithelial elements are immature histologically and by late puberty irreversible destructive changes halt spermatogenesis and limit the production of androgens.Early repositioning of an incompletely descended testis can preserve function
Clinical features
The scrotum is empty & underdevelopedMore common on the right
Bilateral in 20% of cases.
Secondary sexual characteristics are typically
normal.
The testis may be:
• intra-abdominal, lying extraperitoneally above the internal inguinal ring.• inguinal, it may or may not be palpable
• in the superficial inguinal pouch, in which case it must be distinguished from retractile testis.
Hazards of incomplete descent
Sterility in bilateral cases (especially intra-abdominal testes)
Pain as a result of trauma
Indirect inguinal hernia often present
Torsion of the testis
Epididymo-orchitis
Atrophy of an inguinal testis before puberty may possibly be caused by recurrent minor trauma
Testicular cancer is more common in an incompletely descended testes
N.B. orchidopexy may or may not diminish the risk of testicular cancer but it does improve the prospect of early diagnosis
Treatment
Orchidopexy is usually performed after the age of one yearThe testes should be brought down into the scrotum before the boy starts school.
Orchidectomy should be considered if the incompletely descended testis is atrophic
Hormone treatment with human chorionic gonadotrophin is appropriate only when there is established hypogonadism.
ECTOPIC TESTIS
The testis is abnormally placed outside this pathThe sites of ectopic testis are:
• at the superficial inguinal ring: superfecial to the inguinal canal
• the perineum
• the root of the penis
• the femoral triangle.
An ectopic testis is usually fully developed. The main hazard is liability to injury.
Treatment: orchidopexy
N.B.: Retractile testis is normal testis with active cremasteric reflex
INJURIES TO THE TESTIS
Blunt or penetrating trauma
Contusion and rupture of the testis are associated with a collection of blood around the testis and cannot usually be distinguished with certainty without exploration.
O/E: scrotal swelling, bruises, Loss of testicular contour
U/S is the investigation of choice
Haematocele ( collection of blood between two layers of tunica vaginalis) should be drained and the tunica albuginea repaired after evacuation of haematoma.
A severely damaged testis may have to be removed.
ABSENT TESTIS
‘Vanishing’ testis: a condition in which a testis develops but disappears before birth.Cause: prenatal torsion.
True agenesis of the testis is rarer.
Laparoscopy is useful in distinguishing these causes of clinically absent testis from intra-abdominal maldescended testis.
Scrotal Swelling
Scrotal swelling with pain:
Epididymitis
Orchitis
Testicular trauma
Testicular torsion
Incarcerated scrotal hernia
Testicular tumor
Scrotal Swelling without pain:
HydroceleSpermatocele
Varicocele
Hematocele
Scrotal hernia
Testicular tumor
TORSION OF THE TESTIS ( Torsion of spermatic cord)
Rotation of the testis around the vertical axis of the cordIt is time limited due to arterial obstruction & the patient might lose his testis by ischemia (gangrene) if the diagnosis is delayed (6 hours).
It may develop spontaneously during sleep.
Straining at stool, lifting a heavy weight, trauma, and coitus are all possible precipitating factors.
Clinical features
Most common between 10 and 25 years of ageSudden agonizing pain in the groin and the lower abdomen.
The patient feels nauseated and may vomit.
The testis lie transversely high and the tender twisted cord can be palpated above it.
Testicular elevation does not relief pain
Loss of cremasteric reflex
Diagnosis
Doppler ultrasound scan will confirm the absence of the blood supply to the affected testisTreatment
Exploration for torsionIf the testis is viable when the cord is untwisted then it is fixed (orcheopexy).
An infarcted testis (gangrenous) should be removed (orchidectomy).
The other testis should also be fixed because the anatomical predisposition is likely to be bilateral.
N.B: In the first hours it may be possible to untwist the testis manually, then early orcheopexy to avoid recurrent torsion
VARICOCELE
It is a varicose dilatation of the veins draining the testis ( abnormal dilatation of the pampiniform plexus)Most varicoceles present in adolescence or early adulthood
Usually on the left.
Clinical Features
Usually symptomlessThere may be dragging scrotal discomfort
The scrotum on the affected side hangs lower than normal
On palpation, with the patient standing, the varicose plexus feels like a bag of worms.
Infertility ?
Investigations: Scrotal Doppler U/S
Treatment
Operation is not indicated for asymptomatic varicocele.Indicatioins: pain, infertility, cosmetic
Types of operations:
Varicocele ligation
laparoscopic ligation
Embolisation of the testicular vein under radiographic control
HYDROCELE
Hydrocele is an abnormal collection of serous fluid in a part of the processus vaginalis, usually the tunica.Vaginal hydrocele abnormal collection of serous fluid between the two layers of tunica vaginalis.
In congenital hydrocele, the processus vaginalis is patent and
connects with the peritoneal cavity.
Etiology
Acquired hydroceles are primary (idiopathic), or secondary to testicular disease.A hydrocele can be produced in four different ways
• by excessive production of fluid within the sac, e.g. secondary hydrocele
• by defective absorption of fluid; this appears to be the explanation for most primary hydroceles although the reason why the fluid is not absorbed is obscure
• by interference with lymphatic drainage of scrotal structures
• by connection with the peritoneal cavity via a patent processus
vaginalis (congenital).
Clinical features
Primary vaginal hydrocele is most common in middle and later life but can also occur in older children presents withscrotal swelling
Painless
Typically translucent (transillumination +ve)
It is possible to ‘get above the swelling’ on examination of the scrotum
N.B: in a young man; there may be a testicular tumour, so scrotal US should be done.
Treatment
Congenital hydroceles are treated by herniotomy if they do not resolve spontaneouslyAcquired hydroceles: excision of the wall
N.B: A secondary hydrocele may subsides when the primary lesion resolves.
Epididymal cystsThey represent cystic degeneration of the epididymis.
Filled with a crystal-clear fluid.
Found in middle age
The cysts are multilocular
Excision may cause obstruction of the epididymis therefore it is better to leave it.
Spermatocele
A unilocular retention cyst derived from some portion of the sperm-conducting mechanism of the epididymis.Typically lies in the epididymal head above and
behind the upper pole of the testis.
The fluid contains spermatozoa
Small spermatoceles can be ignored. Larger ones can be aspirated or excised through a scrotal incision.
EPIDIDYMO-ORCHITIS
Inflammation confined to the epididymis is epididymitis
Infection spreading to the testis is epididymo-orchitis.
Acute epididymo-orchitis
Mode of infection
Infection reaches the epididymis via the vas from a primary infection of the urethra, prostate or seminal vesicles
Blood-borne infections of the epididymis are less common
N.B: Acute epididymo-orchitis can follow any form of urethral
instrumentation. It is particularly common when an indwellingcatheter is associated with infection of the prostate.
Clinical features
The initial symptoms are those of urinary tract infection.The epididymis and testis swell and become painful.
Fever
The scrotal wall, at first red, oedematous and shiny, may become adherent to the epididymis.
Resolution may take 6–8 weeks to complete.
Occasionally, an abscess may form and discharge of pus through the scrotal skin.
N.B: Acute epididymo-orchitis develops in about 18% of males suffering from mumps. The main complication is testicular atrophy, which may cause infertility if the condition is bilateral.
Investigations
GUE
Urine C&S
WBC count
Scrotal U/S
Treatment
Broad spectrum antibiotics for 2 weeks (3rd generation cephalosporin or quinolones)Scrotal support
Supportive therapy (analgesics, antipyretics, anti emetics, IVF)
If suppuration occurs(Abscess): drainage is necessary.
TUMOURS OF THE TESTES
Most testicular neoplasms are malignant
It is one of the most common forms of cancer in young men.Maldescent predisposes to malignancy
The lymphatic drainage of the testes is to the para-aortic lymph nodes near the origin of the gonadal vessel.
The inguinal lymph nodes are affected only if the scrotal skin is involved.
Classification
They are classified according to their predominant cellular type:
• GCTs:
Seminoma (40%):
The enlarged testis is smooth and firm.
metastasize via the lymphatics.
Hematogenous spread is uncommon.
Nonseminomatous GCT or Teratoma (32%):
Arises from totipotent cells in the rete testis and often contains a variety of cell types, of which one or more predominate.
They may secrete human chorionic gonadotrophin (HCG) & alpha-fetoprotein.
Combined seminoma and teratoma (14%)
Classification
• 2. Interstitial tumours (1.5%):arise from Leydig or Sertoli cells
• 3. Lymphoma (7%)
4. Other tumours (5.5%)
Clinical features
testicular lump which is usually painlesssensation of heaviness occurs when the testis is two or three times its normal size
The testis is enlarged, smooth, firm and heavy
Secondary hydrocele
Secondary retroperitoneal deposits may be palpable, just above the umbilicus, hepatic enlargement, enlarged supraclavicular nodes
Symptoms of metastatic disease: abdominal or lumbar pain, chest pain, dyspnoea and haemoptysis
Rarely, patients present with severe pain and acute enlargement of the testis because of haemorrhage into a neoplasm
Between 1% and 5% of cases have gynaecomastia (mainly the teratomas).
Investigations
Tumour markers (HCG, alpha-fetoprotein and lactate dehydrogenase)
U/S scanning of the testis
CXR: pulmonary metastases especially in teratoma
Investigations
CT scan and MRI are the most useful means of detecting secondaries and f monitoring the response to therapy.Staging
Treatment
Radical orchidectomy through inguinal approach.
Further Mx:
Further treatment depend on staging and histological diagnosis (after orchidectomy):Seminomas
RadiosensitiveHighly sensitive to cisplatin, which is used for patients with metastatic disease.
Teratomas
less sensitive to radiation
Chemotherapy:
Cisplatin, methotrexate, bleomycin and vincristine : used in combination with great success.
For both seminoma & teratomas: Retroperitoneal lymph node dissection is sometimes needed when retroperitoneal masses remain after chemotherapy
Prognosis
Seminoma: the 5 years survival after orchidectomy and radiotherapy or chemotherapy:
If there are no metastases 95%.
If there are metastases 75%
Teratoma: 5-year survival rate:
stage 1 - 2: of more than 85%stage 3 - 4 : about 60%
Idiopathic scrotal gangrene- Necrotizing fasciatis (Fournier’s gangrene)
Fulminating inflammation of the subcutaneous tissues, which results in an obliterative arteritis of the arterioles to the scrotal skinMost commonly occurs in immunocompromised patients
Causative organisms: mixed infection of Haemolytic streptococci (sometimes microaerophilic), Staphylococcus, E. coli, Clostridium welchii.
Clinically:
Sudden scrotal inflammationRapid onset of gangrene and loss of scrotal skin leading to exposure of the scrotal contents
The absence of any obvious cause in over half the cases.
The condition can follow minor injuries or procedures in the perineal area, such as a bruise, scratch, urethral dilatation, injection of haemorrhoids or opening of a periurethral abscess.
Clinical features
Sudden pain in the scrotum, prostration, pallor and pyrexia.Cellulitis spreads until the entire scrotal coverings slough, leaving the testes exposed but healthy
Treatment
The microorganisms are usually sensitive to gentamicin and a cephalosporinWide excision of the necrotic scrotal skin
Many patients die despite active treatment
Vesicoureteral reflux
VURVUR
Definition:
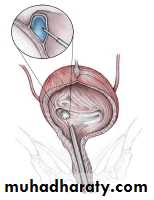
VUR results from abnormal retrograde flow of urine from the bladder into the upper urinary tract.
It is caused by primary or secondary incompetence of the ureterovesical valve mechanism.
Epidemiology
Overall incidence in children is >10%Asymptomatic children have an incidence of 17%
VUR is present in 70% of infants with urinary tract infection.
More importantly, between 30% and 50% of children with reflux will have renal scarring.
Reflux is the second most common cause of prenatal hydronephrosis and accounts for 37% of cases.
Adults with urinary tract infection (UTI) have a 5% incidence of reflux.
Epidemiology
Younger children affected more than older childrenGirls more than boys (female–male ratio 5:1)
VUR occurs more often in Caucasian than in Afro-Caribbean children.
Siblings of an affected child have a 40% risk of reflux, and routine screening of siblings is recommended.
Pathogenesis
The ureter passes obliquely through the bladder wall (1–2 cm), where it is supported by muscular attachments that prevent urine reflux during bladder filling and voiding.
The normal ratio of intramural ureteric length to ureteric diameter is 5:1.
Reflux occurs when the intramural length of ureter is too short (ratio <5:1).
The appearance of the ureteric orifice changes with increasing severity of reflux, classically described as stadium, horseshoe, golf-hole, or patulous.
Classification
Primary reflux (1%) results from a congenital abnormality of the ureterovesical junction.Secondary reflux results from urinary tract dysfunction associated with elevated intravesical pressures.
Iatrogenic Causes
A. PROSTATECTOMYB. WEDGE RESECTION OF THE POSTERIOR VESICAL NECK
C. URETERAL MEATOTOMY
D. RESECTION OF URETEROCELE
Congenital Causes
A. TRIGONAL WEAKNESS (PRIMARY REFLUX)
B. FAMILIAL REFLUX
C. URETERAL ABNORMALITIES
CAUSES
• Other causes
• Voiding Dysfunction
• Vesical Trabeculation
• Contracted Bladder
• Eagle-Barrett(Prune Belly) Syndrome
• Edema of the Vesical Wall
Secondary to Cystitis
Etiology
• Primary reflux is caused by lateral displacement of the ureteral orifice during embryogenesis and a shorter intramural tunnel for the ureter, resulting in a poor muscular backing. A weaker valve mechanism is therefore available to close the orifice during bladder contractions.
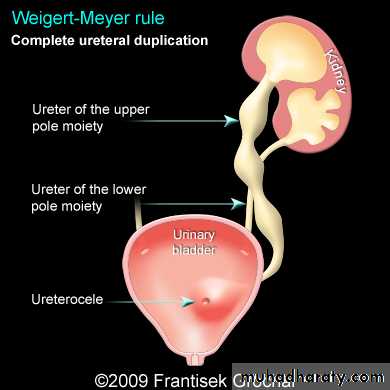
• Ureteral duplication is commonly associated with reflux into the lower pole ureter, again owing to its abnormally short intramural tunnel.
Etiology
3. Ureteral ectopia without ureterocele may be associated with reflux.4. Abnormalities of the bladder wall such as diverticula, radiation cystitis, and cyclophosphamide cystitis may predispose to vesicoureteral reflux. UTI may be associated with transient reflux, due to the inflamed bladder wall.
5. Elevated intravesical pressure from any cause may lead to reflux. Common causes are posterior urethral valves, detrusor hyperreflexia, and prostatic enlargement in adults.
Etiology
7. Prune-belly syndrome is a congenital condition characterized by deficient anterior abdominal musculature, bilateral cryptorchidism, bilateral megaureter, and often bilateral vesicoureteral reflux.8. Iatrogenic reflux may result from any surgical procedure that disrupts the trigonal muscle, such as prostatectomy. Resection of the ureteral orifice can also produce reflux.
9. Dysfunctional voiding or elimination syndromes can lead to reflux. Voiding patterns should always be elicited in the medical history.
Grading of VUR
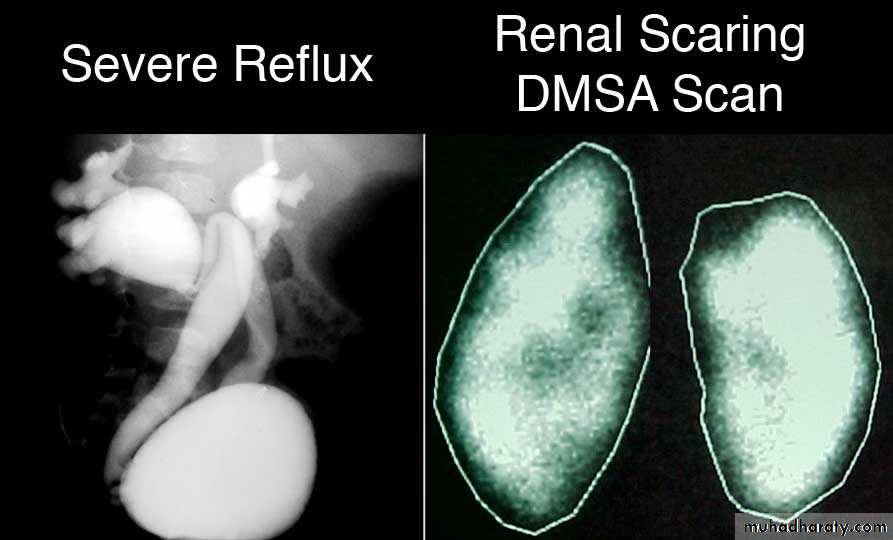
The degree of reflux is graded I–V.Grading is based on the appearance of contrast agent in the collecting system during voiding cystourethrography (VCUG(.
COMPLICATIONS
Hydroureteronephrosis(1) Increased work load
(2) High hydrostatic pressure
(3) Weak ureteral musculature
reflux nephropathy
Pyelonephritis
Vesicoureteral reflux is one of the common contributing factors leading to the development of cystitis, particularly in females.
When reflux is present, bacteria reach the kidney and the urinary tract cannot empty itself completely, so infection is perpetuated.
Complications
VUR associated with UTI can result in reflux nephropathy with hypertension and progressive renal failure.Presentation
Vesicoureteral reflux rarely causes symptoms.Most patients present as recurrent UTI or pyelonephritis: have symptoms of fever, dysuria, suprapubic or abdominal pain, failure to thrive, vomiting, and diarrhea.
In more advanced stages, the patient may present with uremia or hypertension.
Investigations
Urinalysis and culture to diagnose UTI
Urinary tract ultrasound scan to diagnose reflux
The VCUG:
the definitive examination
to diagnose and grade reflux and establish reversible causes
must include a voiding phase:
in some cases, reflux may be seen only during the elevated intravesical pressures associated with micturition.
in visualizing the urethra, may allow the diagnosis of outflow obstruction to be made (e.g., posterior urethral valves).
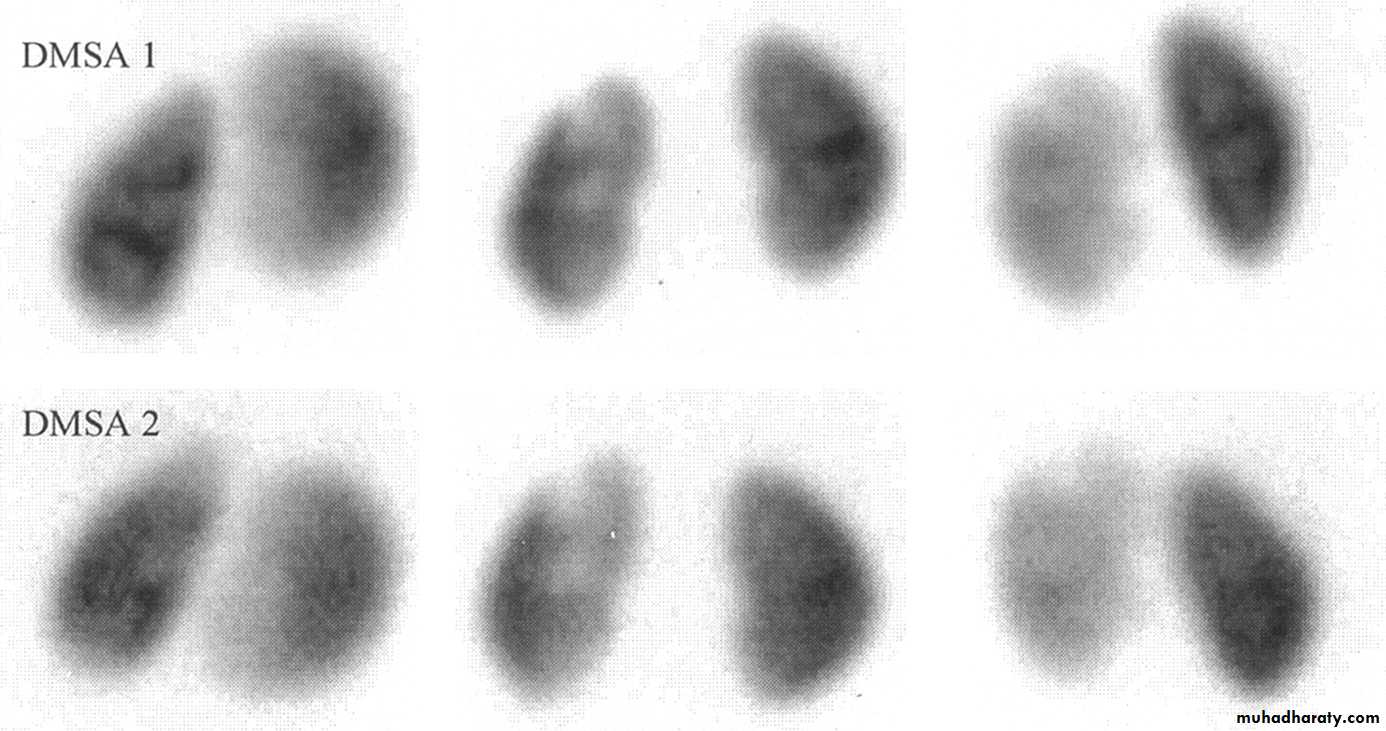
DMSA scan to detect and monitor associated renal cortical scarring.
The intravenous urography (IVU) findings are usually normal in lower grades of reflux.
Urodynamic assessment if suspicious of voiding dysfunction
Cystoscopy: to study position and morphology of ureteric orifices and exclude secondary causes.
MCUG
Management
Correct underlying problems contributing to secondary reflux.Depending on:
the grade of reflux as determined by VCUG
the age of the patient at diagnosis
unilateral versus bilateral disease
Most primary VUR grade I–II cases will resolve spontaneously (~85%), with 50% resolution in grade III.
Observation and medical treatment are initially recommended.
Medical management
Low-dose antibiotic prophylaxis should be given to keep the urine sterile and lower the risk of renal damage until reflux resolves.Indicated in cases of low-grade vesicoureteral reflux without outlet obstruction or another abnormality.
Good patient compliance is necessary.
Long-term antibiotic suppression with a regimen of amoxicillin (neonate), trimethoprim/sulfamethoxazole, nitrofurantoin, or other antibiotic agent at one-fourth to one-half the usual dose daily is commonly used.
Anticholinergic drugs are given to treat bladder overactivity.
Medical management
If the patient remains asymptomatic, urine cultures are obtained periodically (e.g., every 3 months) during treatment. US and radionuclide cystogram should be obtained at yearly intervals.
If acute (breakthrough) infection occurs, a full course of appropriate antibiotics is given and a prophylactic regimen is then instituted.
Clinicians perform a dimercaptosuccinic acid scan (DMSA) to look for renal scarring at this juncture.
Surgery is often recommended after breakthrough UTI.
Resolution of vesicoureteral reflux with antibiotic prophylaxis
G1= 90%G2= 60%
G3= 50%G4= 30%
G5= 0%Surgical therapy
Indicated in patients with:high-grade primary reflux (grades 4 and 5)
those with low-pressure reflux and significant hydroureter
persistant reflux in girls after puberty
patients in whom medical management has failed:
persistence of reflux after 3 to 4 years of antibiotic prophylaxis
multiple breakthrough infections
new or increased renal scarring
deterioration of renal function
noncompliance with medication
Surgical therapy
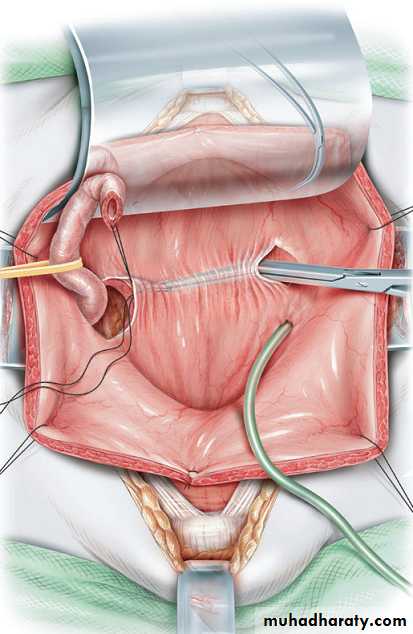
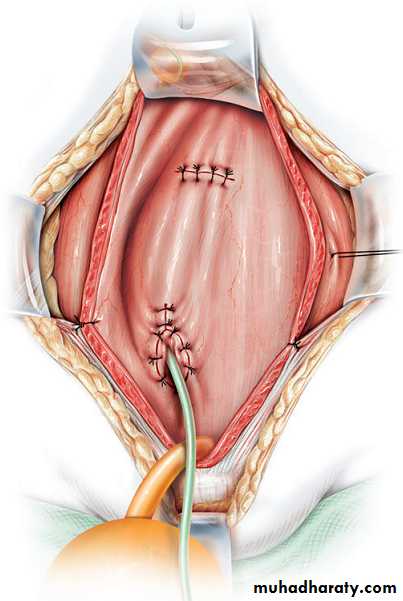
Techniques of ureteral re-implantation include the following:
Intravesical methods involve mobilizing the ureter and advancing it across the trigone (Cohen repair) or reinsertion into a higher, medial position in the bladder (Politano–Leadbetter repair(
Extravesical techniques involve attaching the ureter into the bladder base and suturing muscle around it (Lich–Gregoir procedure(
Has a 98% cure rate.
Surgical therapy
Approximately 1% of patients have obstruction of the ureterovesical junction after ureteral reimplantation that requires reoperation.In patients with massive ureteral dilatation, tapering of the distal ureter may be necessary during reimplantation.
Rarely, temporary supravesical diversion is necessary in patients who are severely uremic.
Alternatively, endoscopic subtrigonal injection of Deflux into the ureteral orifice has 70% success, and 95% with repeated treatments.