Introduction to NeurologyFifth Stage
Dr.Bashar Shaker
College of Medicine – Univ. of Mosul
Nervous system disorders are common, accounting for around 10% of the UK’s general practice consultations, 20% of acute medical admissions, and most chronic physical disability.
Neurological management requires
knowledge of a range of common conditions, which can then be applied to individual patients after careful history-taking, with lesser contributions arising from targeted examination and considered investigation.Pathological and anatomical localisation of symptoms and signs is important.
If the presentation is not an emergency, time can be taken to reach a diagnosis.The history should provide a hypothesis for the site and nature of the potential pathology, with a focused direct examination may refine, and
direct appropriate further investigations
Cells of the nervous system
Astrocytes form the structural framework for neuronsand control their biochemical environment, their foot processes adjoining small blood vessels and forming the blood–brain barrier.
Oligodendrocytes are responsible for the formation and maintenance of the myelin sheath, which surrounds axons and is essential for maintaining the speed and consistency of action potential propagation along axons. Microglial cells derive from monocytes/macrophages and play a role in fighting infection and removing damaged cells.
Communication between cells is by synaptic transmission that involves the release of neurotransmitters to interact with structures on the target cell’s surface, including ion channels and other cell surface receptors .
At least 20 different neurotransmitters are known to act at different sites in the nervous system,
most of which are potentially amenable to pharmacological manipulation.
Neurotransmitters
Excitatory - GlutamateInhibitory - GABA
Excitatory - Inhibitory - Dopamine
The major anatomical components of the nervous system
Anatomy of the cerebral cortexAnatomy of the cerebral cortex
Cortical lobar functionsCortical lobar functions
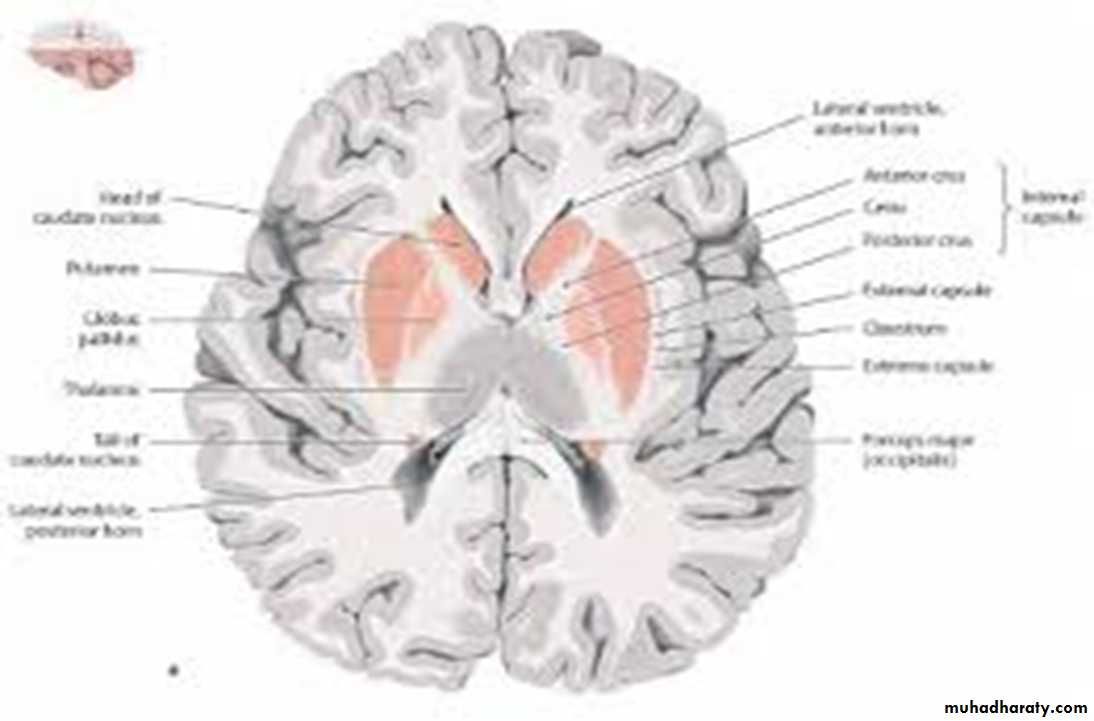
Deep to the grey matter in the cortices, and the white matter(composed of neuronal axons), are collections of cells known as The basal ganglia that are concerned with motor control;
The thalamus, which is responsible for the level of attention to sensory perception;
The limbic system, concerned with emotion and memory; and The hypothalamus, responsible for homeostasis, such as temperature and appetite control.
The cerebral ventricles contain cerebrospinal fluid (CSF), which cushions the brain during cranial movement
The brainstem
In addition to containing all the sensory and motor pathways entering and leaving the hemispheres, the brainstem houses the
nuclei and projections of most cranial nerves, as well as other important collections of neurons in the reticular formation.
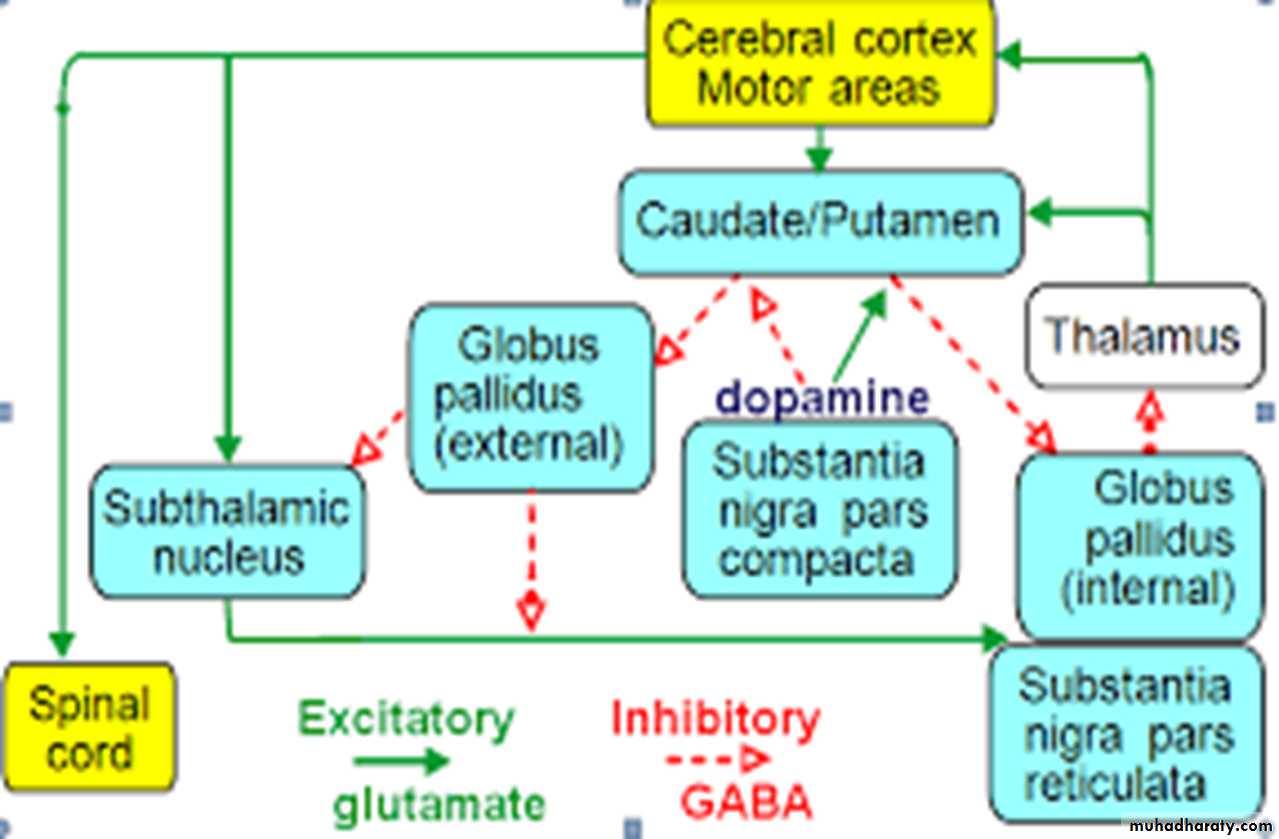
The extrapyramidal system
Circuits between the basal ganglia and the motor cortex constitute the extrapyramidal system, which controls muscle tone, body posture and the initiation of movement.The cerebellum
The cerebellum fine-tunes and coordinates movement initiated by the motor cortex, including articulation of speech.It also participates in the planning and learning of skilled movements through reciprocal connections with the thalamus and cortex.
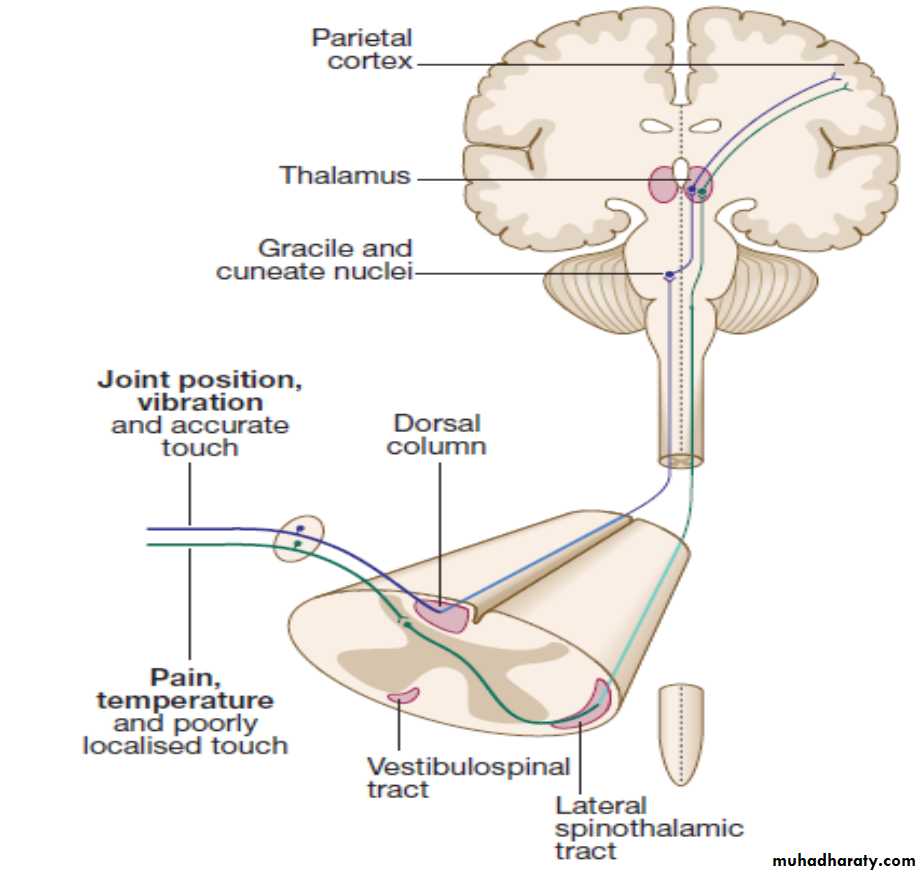
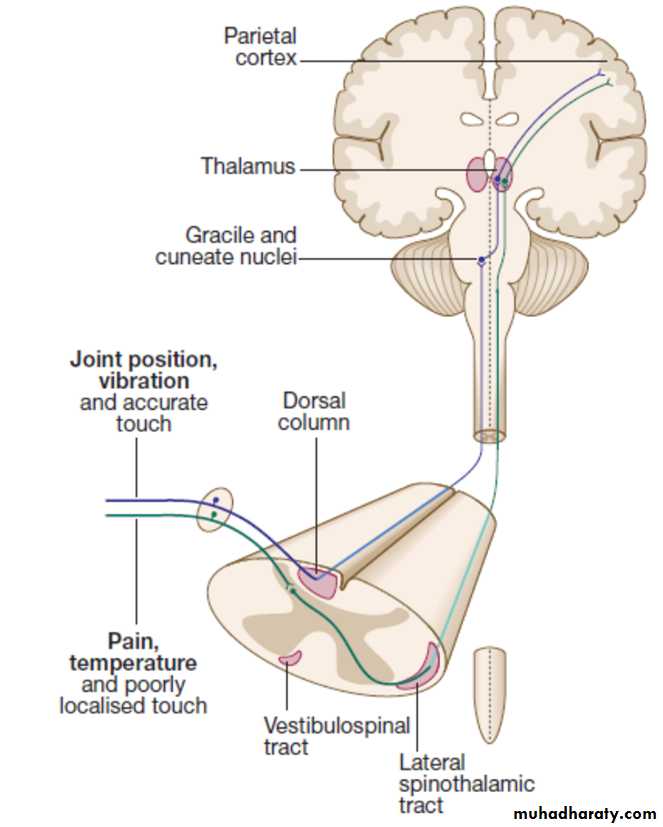
The spinal cord
The spinal cord is the route for virtually all communication between the extracranial structures and the CNS.Afferent and efferent fibres are grouped in discrete bundles but collections of cells in
the grey matter are responsible for lower-order motor reflexes and the primary processing of sensory information.
The motor system
The main somatic sensory pathways
The key diagnostic questions
Where is the lesion?• Is it neurological?
• If so, to which part of the nervous system does it localise?
Central versus peripheral
Sensory versus motor versus both
What is the lesion?
• Hereditary or congenital
• Acquired:
Traumatic
Infective
Neoplastic
Degenerative
Inflammatory or immune-mediated
Vascular
Functionall
How to take a neurological history
Introduction
• Age and sex
• Handedness
Presenting complaint
• Symptoms
• Overall pattern: intermittent or persistent?
• If intermittent, how often do symptoms occur and how long do they
last?
• Speed of onset: seconds, minutes, hours, days, weeks, months,
years, decades?
• Better, worse or the same over time?
• Associated symptoms (including non-neurological)
• Disability caused by symptoms
• Change in walking
• Difficulty with fine hand movements, e.g. writing, fastening buttons,
• Effect on work, family life and leisure
• Previous neurological symptoms and whether similar to current symptoms
• Previous medical history• Domestic situation
• Driving licence status
• Medications (current and at time of symptom onset)
• Alcohol/smoking habits
• Recreational drug and other toxin exposure
• Family history and developmental history
• What are patient’s thoughts/fears/concerns?
How to ‘localise’ neurological disease
The evolution of symptoms
Patterns of motor loss accordingto the anatomical site of the lesionNeurological Examination
High mental functionsSpeech
Cranial nerves
Limbs
Cerebellar function
Examination of cranial nerves
Examination of cranial nervesExamination of gait and posture
Examination of gait and postureAbnormal speech and language
Speech disturbance may be isolated to disruption of sound output (dysarthria) or may involve language disturbance (dysphasia).
Dysphonia (reduction in the sound/volume) is usually due to mechanical laryngeal disruption, whereas dysarthria is more typically neurological in origin.
Dysphasia is always neurological and localises to the dominant cerebral hemisphere (usually left, regardless of handedness).
Limbs
Motor :Inspection,Tone , Power , Reflexes , Coordination.
Sensory:
Sensory modalities
Root values of tendon reflexes
Distinguishing signs in upper versus lowermotor neuron syndromesInvestigations
Lumbar punctureLumbar puncture (LP) is the technique used to obtain both a CSF sample and an indirect measure of intracranial pressure.
After local anaesthetic injection, a needle is inserted between lumbar spinous processes (usually between L3 and L4) through the dura and into the spinal canal.
CSF is normally clear and colourless, and the tests that are usually performed include a naked eye examination of the CSF and centrifugation to determine the colour of the supernatant (yellow, or xanthochromic, some hours after subarachnoid haemorrhage).
Routine analysis involves a cell count, as well as glucose and protein concentrations.
CSF assessment is important in investigating infections (meningitis or encephalitis), subarachnoid haemorrhage and inflammatory conditions (multiple sclerosis, sarcoidosis and
cerebral lupus).
If there is a cranial space-occupying lesion causing raised intracranial pressure, LP presents a theoretical risk of downward shift of intracerebral contents, a potentially fatal process known as coning .Consequently, LP is contraindicated if there is any clinical suggestion of raised intracranial pressure (papilloedema), depressed level of consciousness, or focal neurological signs suggesting a cerebral lesion, until imaging (by CT or MRI) has excluded a space-occupying lesion or hydrocephalus.
When there is a risk of local haemorrhage (thrombocytopenia, disseminated intravascular coagulation or anticoagulant treatment), then caution should be exercised or specific measures should be taken. LP can be safely performed in patients on antiplatelet drugs or low-dose heparin, but may be unsafe in patients who are fully anticoagulated due to the increased risk of epidural
haematoma.
Electroencephalography
The electroencephalogram (EEG) detects electrical activity arisingin the cerebral cortex via electrodes placed on the scalp to record
the amplitude and frequency of the resulting waveforms. With
closed eyes, the normal background activity is 8–13 Hz (known
as alpha rhythm), most prominent occipitally and suppressed on
eye opening. Other frequency bands seen over different parts
of the brain in different circumstances are beta (faster than 13/
sec), theta (4–8/sec) and delta (slower than 4/sec).
Generalised epileptic discharge, as seen in epilepsy syndromes such as childhood absence or
juvenile myoclonic epilepsy.
Focal sharp waves over the right parietal region (circled), with spread of discharge to cause a generalised tonic–clonic
seizure
Nerve conduction studies
Electrical stimulation of a nerve causes an impulse to travel both efferently and afferently along the underlying axons.Nerve conduction studies (NCS) make use of this, recording action potentials as they pass along peripheral nerves and (with motor nerves) as they pass into the muscle belly.
Electromyography
Electromyography (EMG) is usually performed alongside NCS and involves needle recording of muscle electrical potential during rest and contraction.At rest, muscle is electrically silent but loss
of nerve supply causes muscle membrane to become unstable, manifest as fibrillations, positive sharp waves (‘spontaneous
activity’) or fasciculations.
Motor unit action potentials are recorded
during muscle contraction.Other abnormal activity, such as myotonic discharges, may signify abnormal ion channel
conduction, as in myotonic dystrophy or myotonia congenita.
Evoked potentials
The cortical response to visual, auditory or electrical stimulation can be measured as an evoked potential (EP).
Assessing the latency (the time delay) and amplitude can give information about the integrity of the relevant pathway.
Visual evoked potential (VEP) recording. The abnormality isin the left hemisphere, with delay in latency and a reduction in signal of the P100.