Trigger finger ( digital stenosing tenosynovitis) :
It is intermittent 'deformity', usually of the ring , thumb or middle finger. The patient complains that, when the hand is clenched and then opened, the finger (or thumb) gets stuck in flexion; with a little more effort, it suddenly snaps into full extension. A flexor tendon may become trapped at the entrance to the sheath; on forced extension it passes the constriction with snap (triggering). A tender nodule can be felt in front of the affected sheath.The usual cause is thickening of fibrous tendon sheath following trauma or overuse or RA.
Treatment: Early cases may be cured by rest and local injection of steroid placed at entrance of the tendon sheath. If symptom persist the fibrous sheath is incised surgically, allowing the tendon to move freely.Ganglion:
It arises from cystic degeneration in the joint capsule or tendon sheath, the distended cyst contains a glairy fluid, it is seen most commonly on the back of the wrist. The patient, often a young adult, presents with a painless lump, usually on the back of the wrist, and to less degree in volar side. Occasionally there is a slight ache. The lump is well defined, cystic and not tender. It may be attached to one of the tendons.Ganglion
Treatment: The ganglion is harmless, often disappears after some months, so there should be no haste about treatment. If the lesion continues to be troublesome, it can be aspirated. If it recurs, excision is justified, but the patient should be told that there is a 30 per cent risk of recurrence, even after careful surgery.
CARPAL TUNNEL SYNDROME
This is the commonest and best known of all the nerve entrapment syndromes. In the normal carpal tunnel there is barely room for all the tendons and the median nerve . Any swelling in this canal is likely result in compression and ischemia of the nerve. it is common in women at the menopause, in rheumatoid arthritis, in pregnancy and in myxoedema.Clinical features: The usual age group is 40-50 years . The history is most helpful in making the diagnosis. Pain and parasthesia occur in the distribution of the median nerve in the hand. Night after night the patient is woken with burning sensation, patients tend to seek relief by hanging the arm over the side of the bed or shaking the arm. A helpful tests are (Tinels sign); sensory symptoms can often be reproduced by percussing over the median nerve
phalen’s test ; holding the wrist fully flexed for a minute or two reproduced the symptoms . In late cases there is wasting of the thenar muscles. weakness of thumb abduction and sensory impairment in the median nerve territory. Electrodiagnostic tests is diagnostic; which show slowing of nerve conduction across the wrist.
Treatment: Definitive treatment is the surgical treatment. Open surgical division of the transverse carpal ligament usually provides a quick and simple cure. Endoscopic carpal tunnel release offers an alternative. Light splints that prevent wrist flexion can help those with night pain or with pregnancy-related symptoms. Steroid injection into the carpal canal when surgery contraindicated, provides temporary relief.
DUPUYTREN'S CONTRACTURE
It is a nodular hypertrophy and contracture of the palmer aponeurosis It is familial, it is more common in Anglo-Saxon, diabetic, AIDS patients ,epileptic treated by phenytoin.Clinical features: A middle aged man complain of a nodular thickening in the palm extend to ring and little finger. One hand usually affected more than other. It produce flexion contracture of metacarpo- phalangeal joints and proximal inter- phalangeal joints. Similar node may be seen in sole of foot. Dupuytren’s contracture should differentiated from contractures result from skin scar or tendon lesions. Surgical treatment through Z -plasty incision is the treatment, followed by physiotherapy and splintage.
DUPUYTREN'S CONTRACTURE
Acute infections of the hand:
Infection of the hand is frequently limited on one of several well-defined compartments:• 1- Nail- fold infection (paronychia).
• 2- The pulp space (whitlow, felon).
• 3- Thenar space infection.
• 4- Subcutaneous tissues elsewhere.
• 5- Tendon sheaths infection ( suppurative tenosynovitis).
• 6- Mid-palmar deep space infection.
It is usually caused by a Staphylococcus which has been implanted by trivial or unobserved injury.
Pathology and Clinical features
Acute inflammation and suppuration in small closed compartments (e.g. The pulp space or tendon sheath) may cause an increase in pressure to levels at which the local blood supply is threatened, In neglected cases tissue necrosis is an imminent risk. Even if this does not occur, the patient may end up with a stiff and useless hand unless the infection is rapidly controled. Usually there is a history of trauma like thorn prick , but it may have been so trivial as to pass unnoticed. The patient may feel ill, feverish and the pain becomes throbbing, with obvious redness and tension in the tissues, tenderness over the site of infection, finger movements may be markedly restricted.
Paronychia
FELONPrinciples of treatment :
• 1- Antibiotics: As soon as the diagnosis is made and specimens have been taken for microbiological investigation, antibiotic treatment is started - usually with, flucloxacillin and, in severe cases, with fusidic acid, or a cephalosporin as well. This may later be changed when bacterial sensitivity is known.• 2- Rest , Analgesics and elevation : In a mild case the hand is rested in a sling. In a severe case the arm is elevated while the patient is kept in hospital under observation. Analgesics are given for pain.
• 3- Drainage: If there are signs of an abscess (throbbing pain, marked tenderness and toxaemia), the pus should drained. A tourniquet and either general or regional block anesthesia are essential. The incision should be made at the site of maximal tenderness, but never across a skin crease. Necrotic tissue is excised and the area thoroughly washed and cleansed. The wound is left open and covered with light dressings. A pus specimen is sent for microbiological investigation.
• 4- Splintage and physiotherapy: splint should be applied always with the joints in the position of function. Early active exercises encouraged.
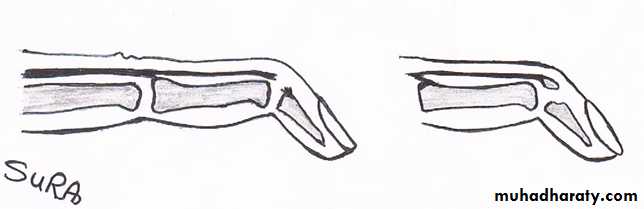
• Mallet finger:
Mallet finger is avulsion of extensor tendon from distal phalanx of a finger. It is caused by sudden forced flexion of the distal interphalangeal joint for instance, by a blow on the tip of the finger from a ball. In a few cases a small fragment of bone is avulsed with the tendon.The patient is unable fully to extend the distal interphalangeal joint. Immediate treatment is to splint the finger for 4-6 weeks with the distal interphalangeal joint fully extended . Splintage must be continuous and uninterrupted if a good result is to be achieved . Surgical treatment used some time to repair injury or to reconstruct the deformity.