
Orthopaedic surgery
فرع الجراحه
\
كلية طب الموصل
upper limbs trauma 3
د
.
ساهر حبيب
دكتوراه
(
بورد
)
اختصاص جراحة العظام والكسور

Fractures single bone of forearm
It is much less common than the fracture of both bones . It's
importance always that, if one forearm bone fractured ,the
dislocation of the proximal or distal radio - ulnar joint to be
excluded by good x-ray .
Treatment and complication are similar to both bone fractures, but
non union is liable to occur due to intact fellow bone
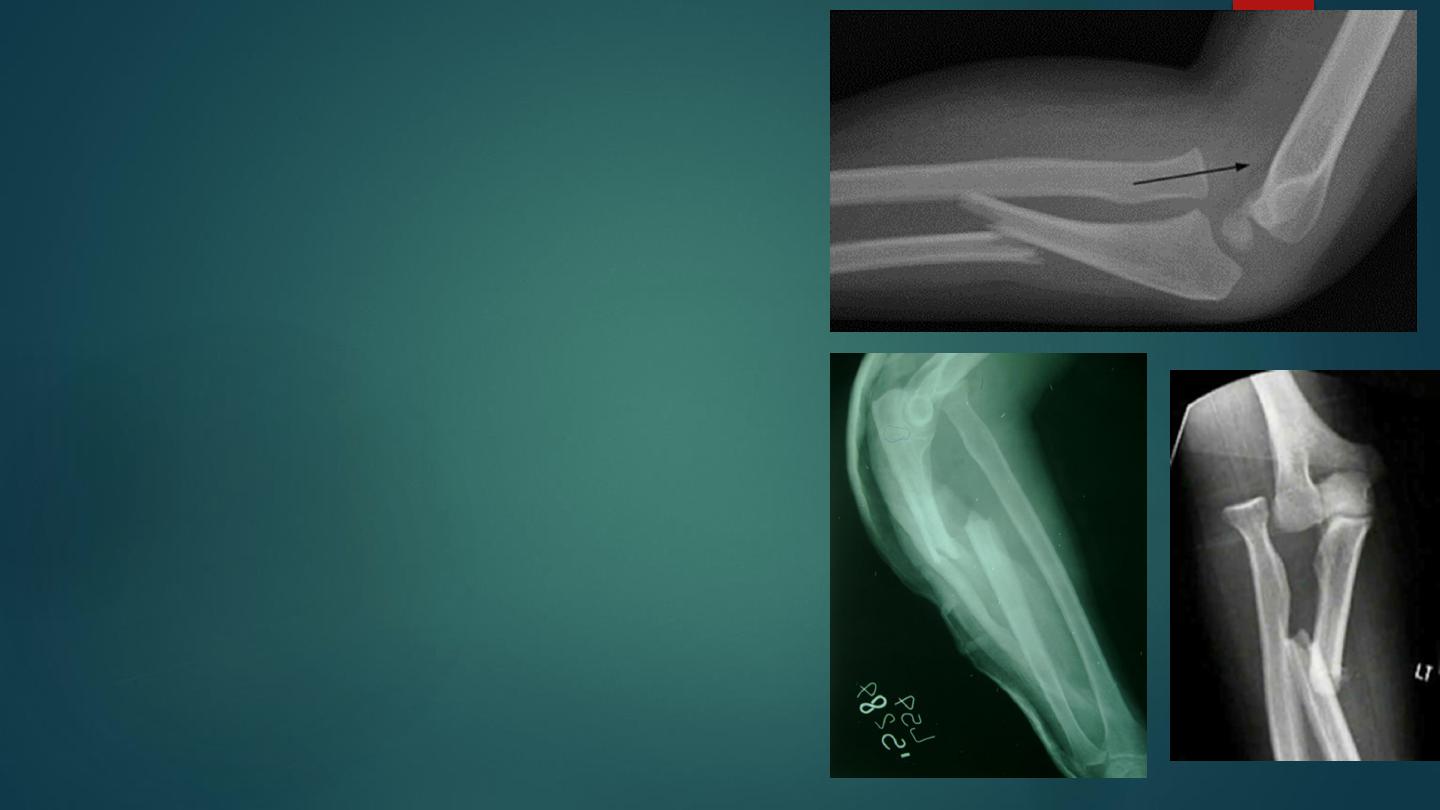
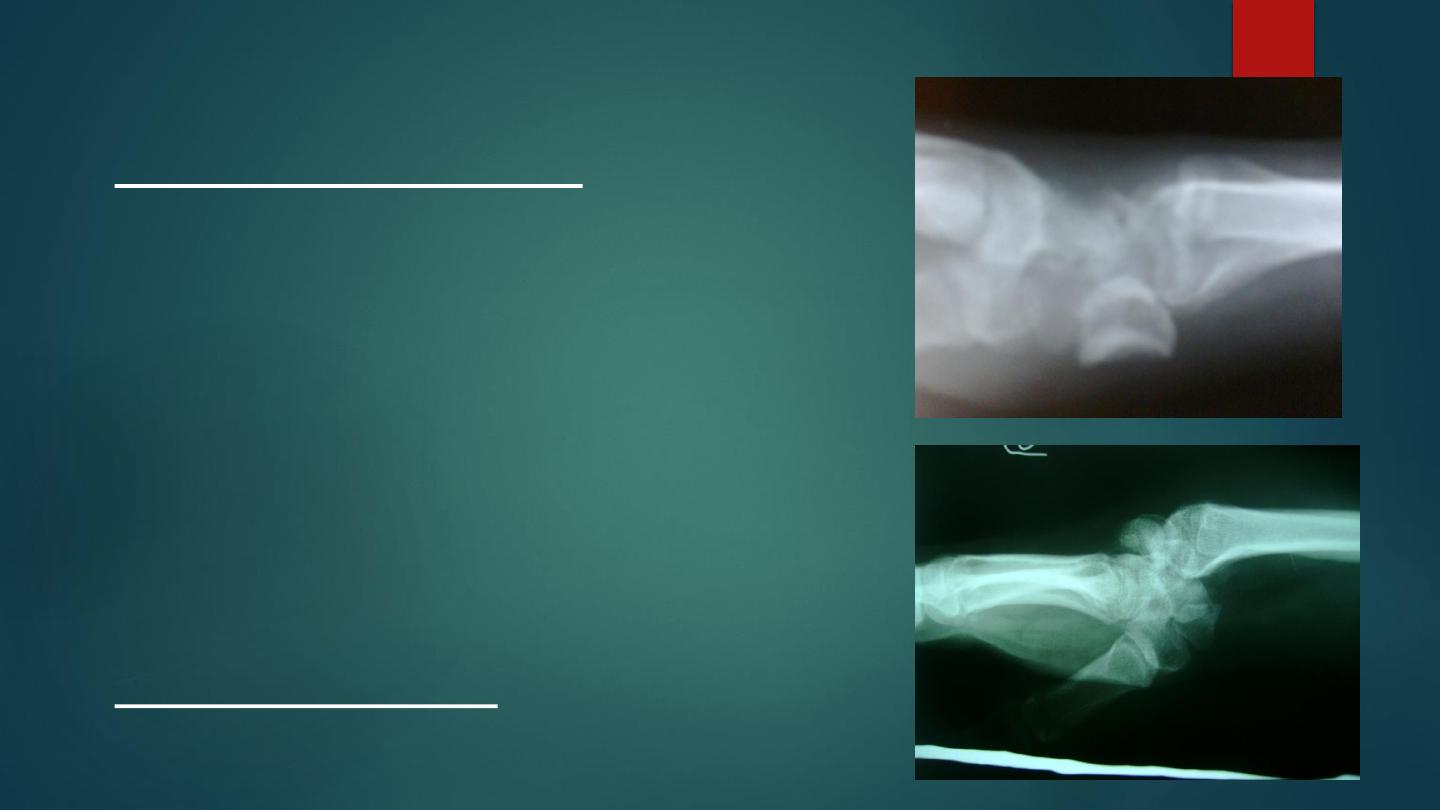
Monteggia fracture
dislocation of the ulna
It is fracture of the proximal third of the ulna with
dislocation or subluxation of the proximal radio- ulnar
joint. The ulnar deformity is usually obvious but the
dislocated head of radius is masked by the swelling .
When there is isolated fracture ulna in x-ray it is
essential to take true anteroposterior and lateral views of
the elbow ; the normal radial head is usually pointing
towards the capitulum, in Monteggia it is not ; in
addition to appearance of the fracture.
The most important point in the treatment is to restore
the length of the fractured ulna and only in this case the
dislocation will be reduced and remain stable ; so in
adult this mean operation (reduction and fixation by
plate and screws) if the dislocation not reduced , then
open reduction of the joint .
In children if the fracture is green- stick then manipulation
under anesthesia can be helpful, but if the fracture is
complete and displaced the best treatment is open
reduction and fixation like adult .
Complication :
1- nerve injury : which occur either due to manipulation or
during surgery .
2- malunion : unless the fracture has been perfectly reduced ,
the radial head remain dislocated and limiting elbow flexion ,
limitation of pronation and supination ; if this happened in
children no treatment but if occur in adult then excision of the
head of the radius can be done .
3- non union of the ulna : the treatment by rigid internal
fixation and bone graft .

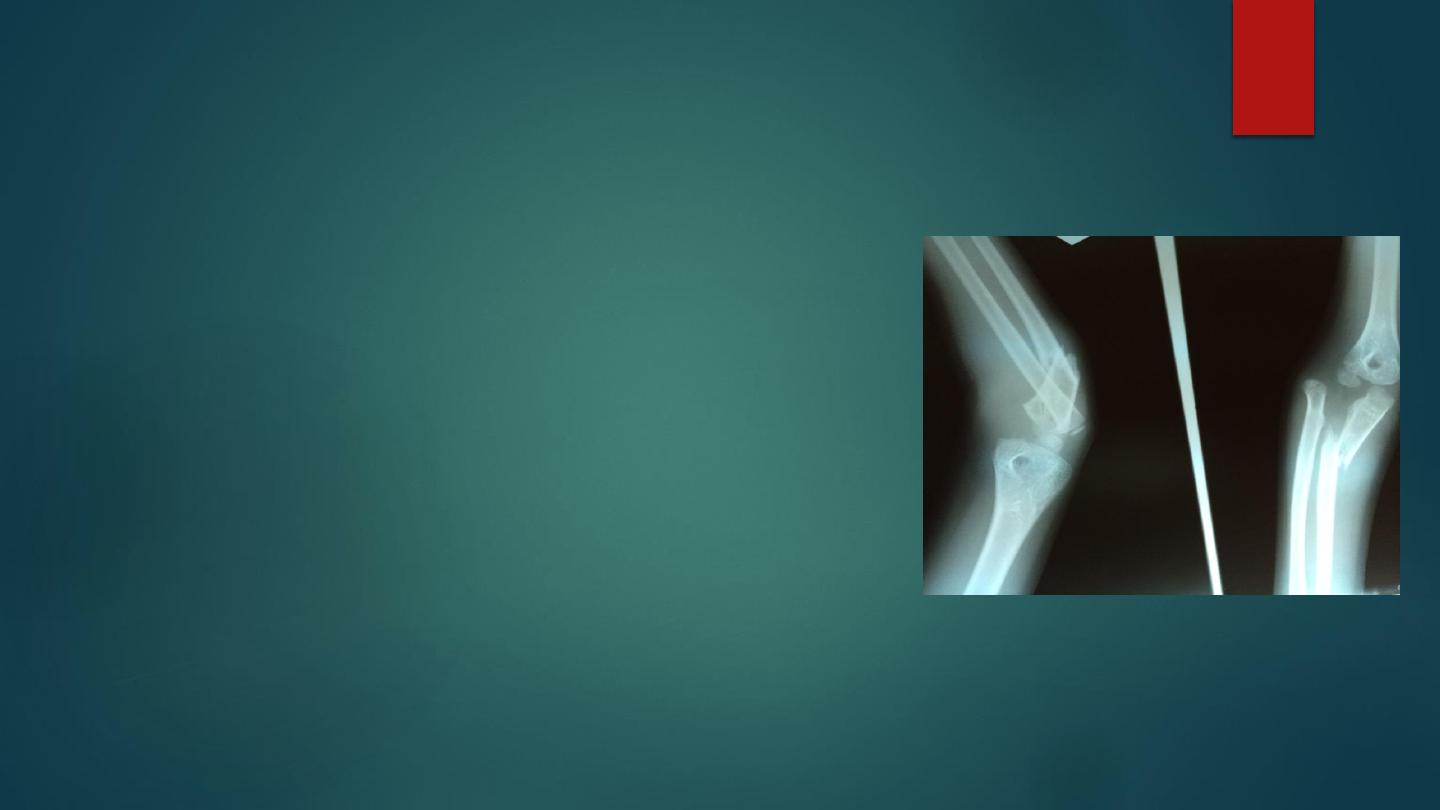
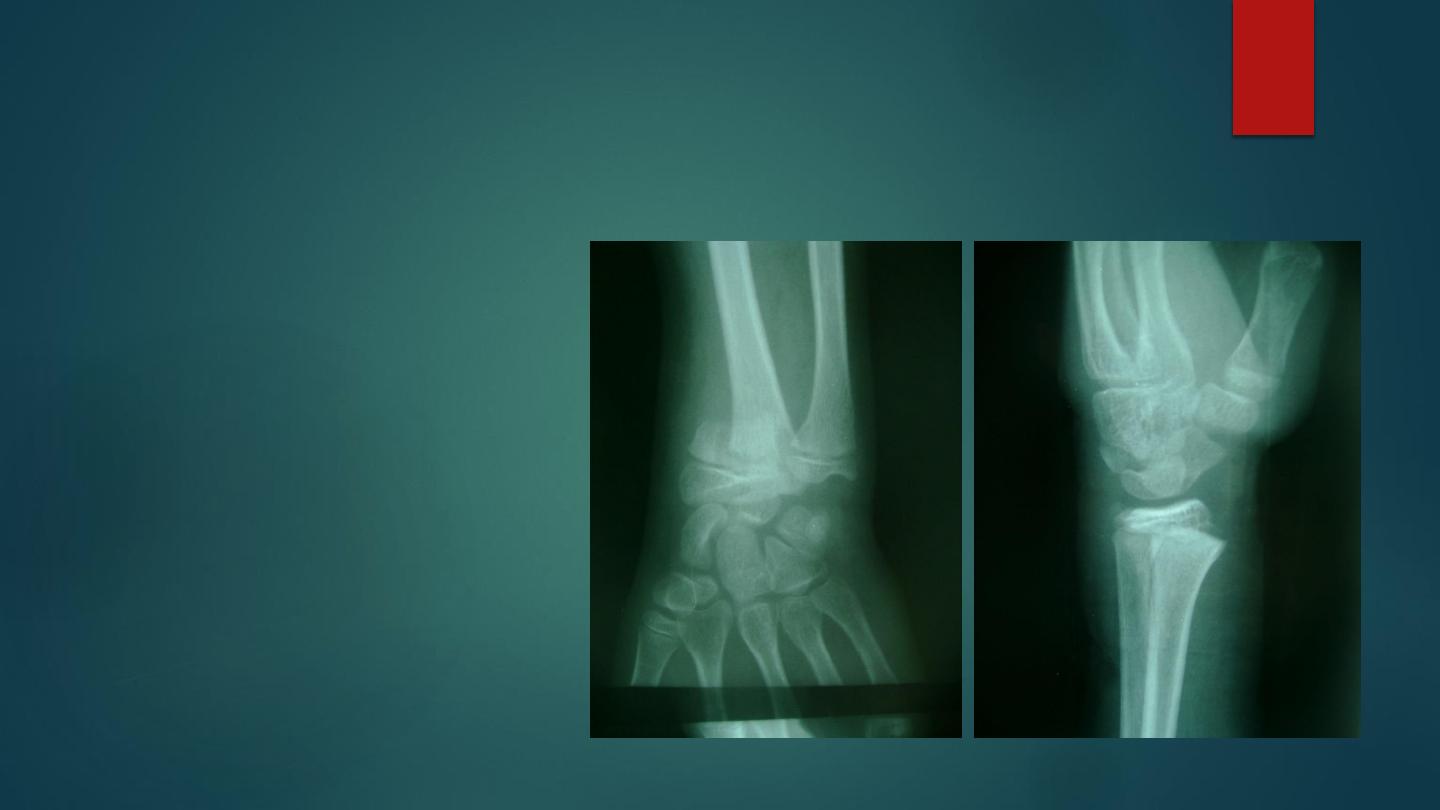
Galeazzi fracture dislocation of the radius
:
It is caused by fall on the hand , there is fracture in the lower third of the
radius and dislocation of the inferior radio- ulnar joint.
It is much more common than Monteggia , there is prominence and
tenderness over the lower end of the ulna is in examination . Balloting the
distal end of the ulna is positive ( piano key sign). Distal ulnar nerve
examination is important.
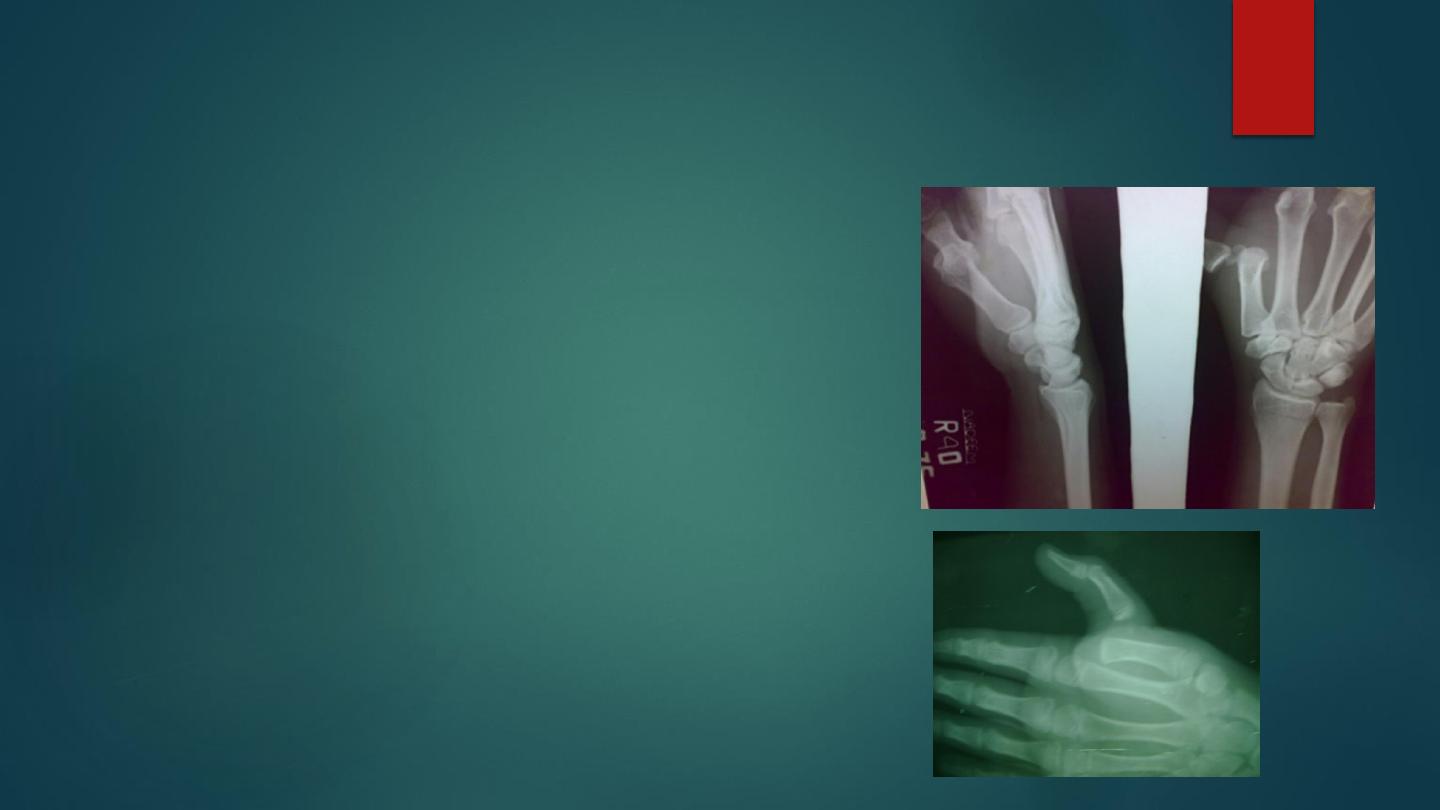
X – ray shows a transverse or short oblique fracture is seen in the lower third
of the radius, with angulations or overlap. The inferior radioulnar joint is
subluxated or dislocated.
The most important point in the treatment is to restore the length of the
fractured radius , otherwise the dislocation will not reduced .
In children close reduction is possible but if fail , then open reduction and
fixation .
In adult , the treatment will be by open reduction and internal fixation .
The most important complication is limitation of pronation and supination .
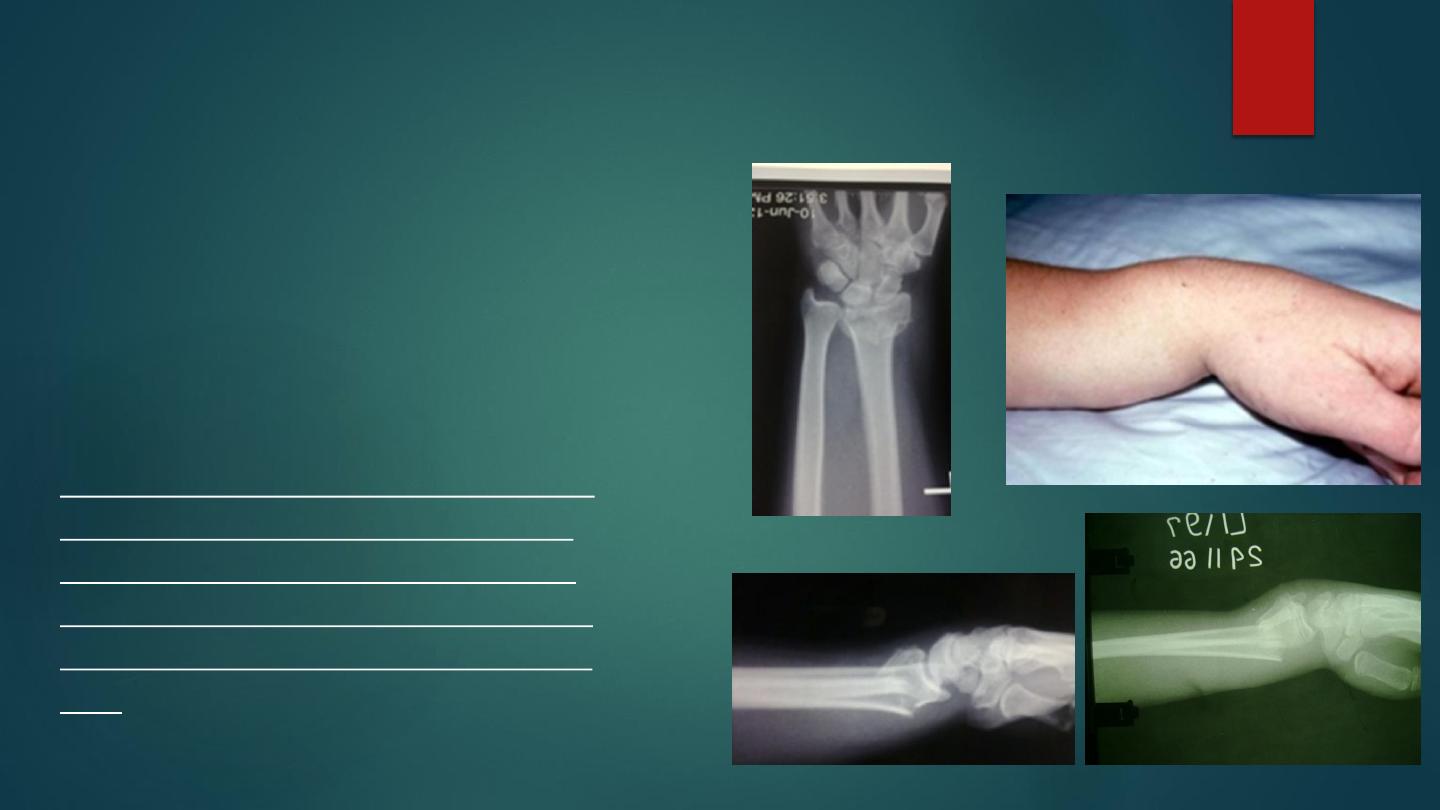
Fractures of the distal radius
Colles's fracture
This fracture is described by Abraham
colles` in 1814 , it is the commonest
fracture in persons over 40 years,
especially women with osteoporosis,
but it occur in all age groups.
It is a transverse fracture of the distal
end ( distal inch )of the radius with
dorsal and lateral displacement and
tilting of the distal fragment, with or
without fracture of styloid process of
ulna.
It is occur due to fall on out stretched hands, force is
applied in the length of the forearm with the wrist in
extension.
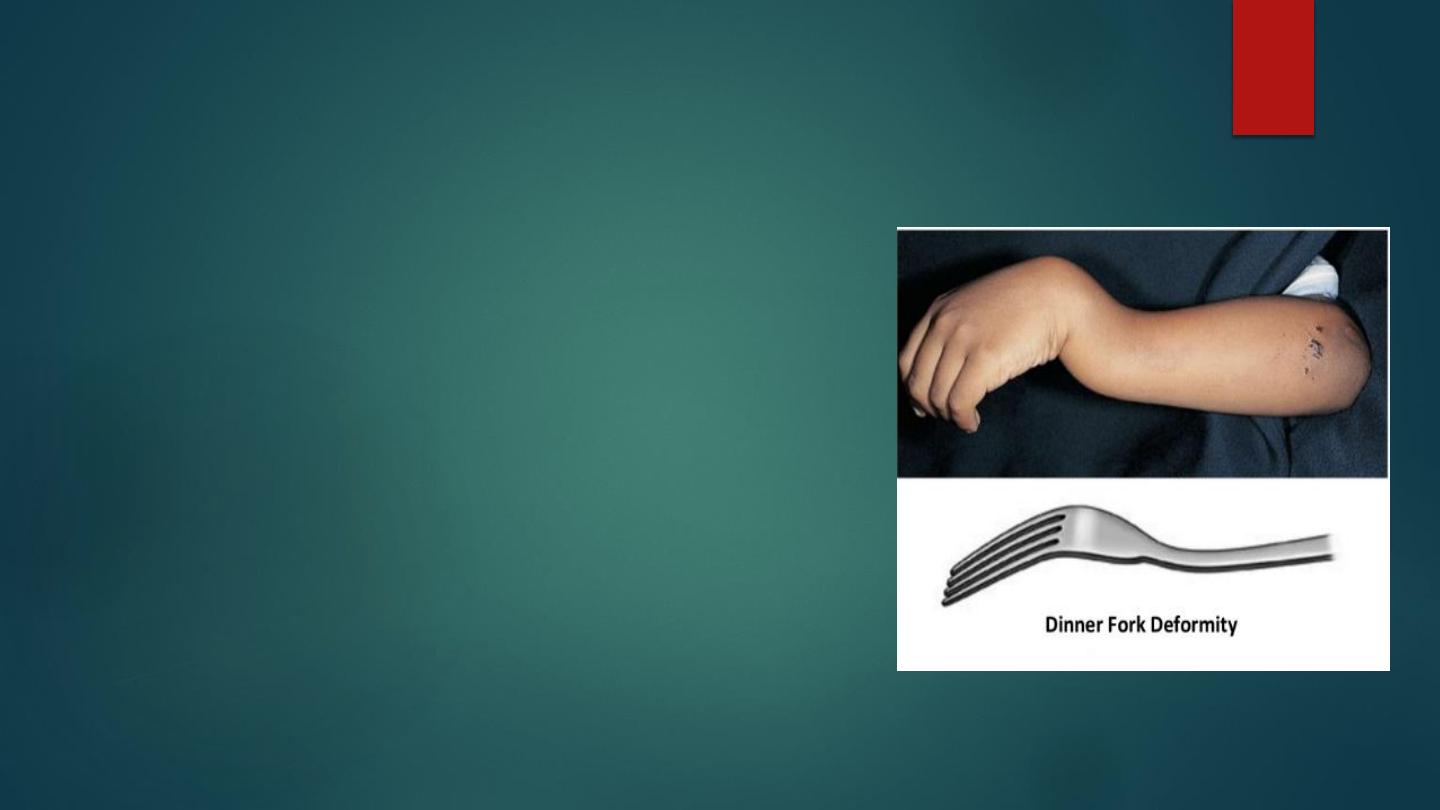
The bone fracture at the corticocancellous junction
and the distal fragment collapses into extension,
dorsal displacement, impaction, radial tilt and
shortening, give the typical deformity ' dinner-fork'.
The patients give history of fall on outstretched
hand, there is pain , loss of function , swelling,
tenderness, and ' dinner-fork' deformity .
X-ray shows a transverse fracture of the radius at the
corticocancellous junction , and the distal fragment is
displaced posteriorly, often ulnar styloid process
fracture, there might be impaction of the distal piece
,some time severely comminuted or crushed .

Treatment :
Undisplaced fracture treated by a dorsal cast applied for 4 weeks then
physiotherapy.
Displaced fracture : It must be reduced under general anesthesia, the
reduction must be by longitudinal traction against counter-traction by
assistant on the hand to disimpact fragments , some time add wrist
extension to ensure disimpaction , the distal fragment then pushed into
place by pressing on the dorsum while manipulating the wrist into
flexion , ulnar deviation and pronation (20 degrees in each plane ).
A dorsal slab applied in neutral position with slight ulnar deviation from
just below the elbow to the metacarpal necks and check by x-ray, slab
changed to full cast one week later and continue for 4- 5 weeks.
Shoulder and fingers exercise then started immediately, and x-ray
repeated weekly for 6 weeks to prevent and correct redisplacement.
The fracture usually unite in 6 weeks.
Surgery some time used if conservative failed by external fixation or
internal fixation.

Complications :
Early :
1-vascular damage and compartment syndrome : radial artery (rare)
2- nerve damage median nerve (rare) .
3- skin damage.
4-triangular fibrocartilage complex injuries.
5- 5-Reflex sympathetic dystrophy ( Sudeck`s dystrophy) caused by a
localized sympathetic over activity
Late complication :
1- malunion : it is common due to unreduced fracture or due to
redisplacement .
2- delayed union and non union ( rare) .
3-stiffness of the wrist ,fingers, elbow and shoulder
4-tendon rupture of extensor pollicis longus .
5-carpal- tunnel syndrome .

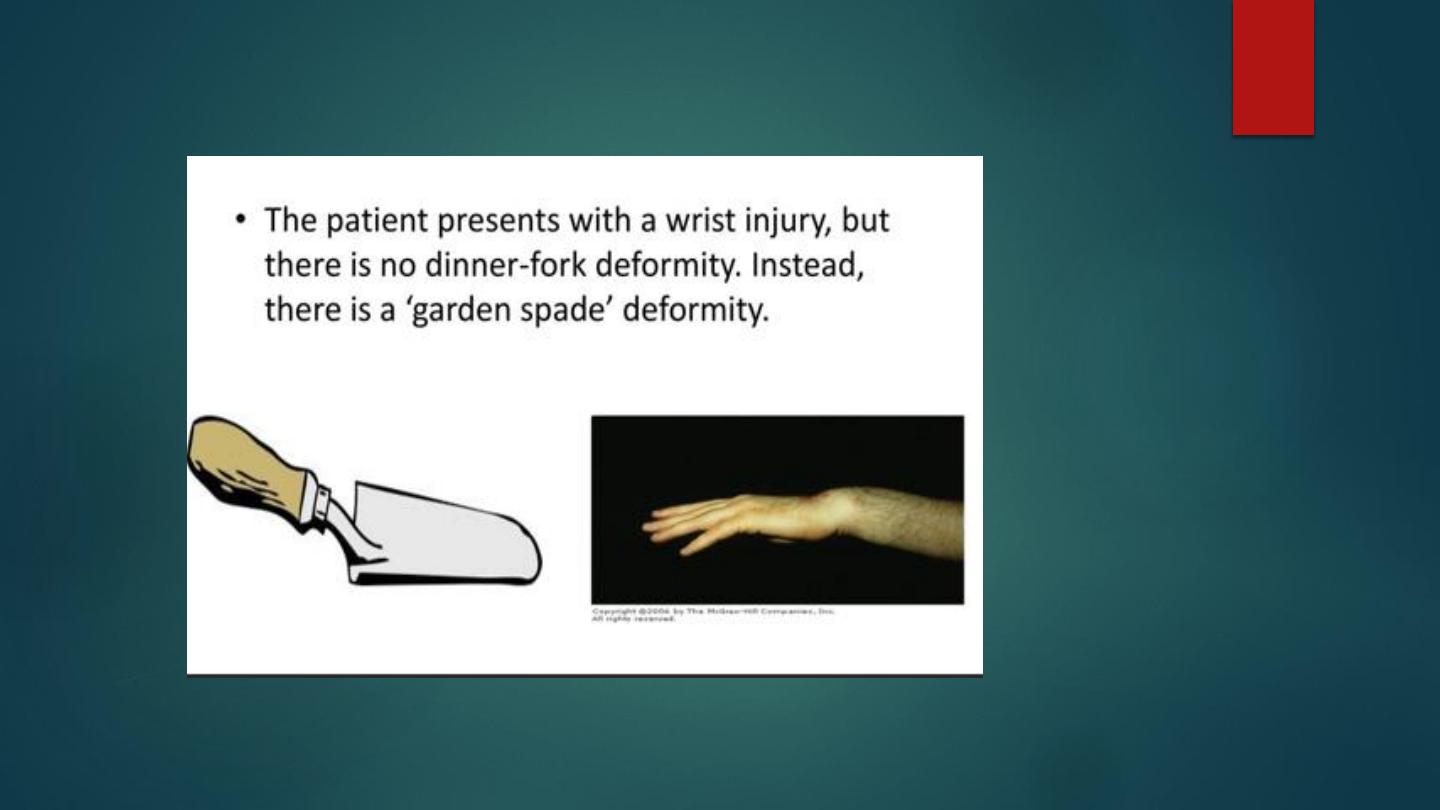
Smith fracture ( reverse Colles's)
it is rare fracture, the distal segment is displaced in
volar direction , caused by fall on the back of the
hand.
There is pain and swelling in wrist, but no dinner
fork deformity.
X ray show fracture through distal radial
metaphysis, the distal fragment is displaced and tilted
anteriorly.
Treated by manipulation under anesthesia by
traction and extension of the wrist, the forearm is
immobilized in a above elbow cast for 6 weeks,
Open reduction and internal fixation commonly
used.
Fracture- separation of the lower radial epiphysis ( salter
harris fracture )
It is common injury in children, it
might be greenstick or displaced.
The lower fragment displaced
dorsally.
Treated by manipulation under
anesthesia and splintage in cast
for 3-4 weeks.
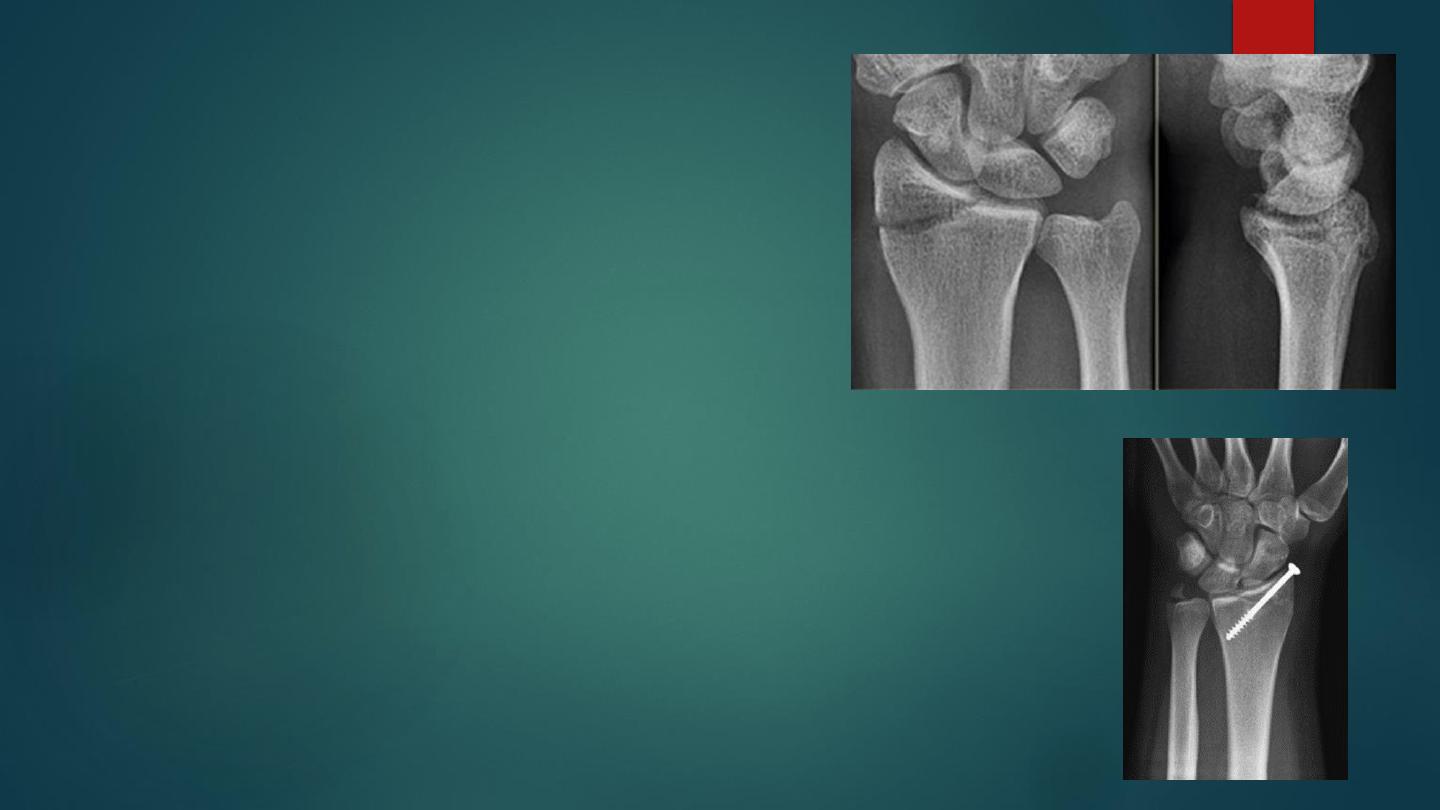
Radial styloid process
fracture
Here the fracture line extend from the
articular surface of the radius laterally.
If there is displacement , the fracture
should be reduced by manipulation under
anesthesia , then back slab below elbow tell
the neck of the metacarpal ; imperfect
reduction will lead to osteoarthritis , so if
the fracture not reduced perfectly by
manipulation then open reduction and
fixation by screw or k wire .
chauffeur’s fracture
Fracture-subluxation (Barton’s fracture)
It is intra articular fracture of the lower end of
the radius with subluxation of the wrist joint .
It might be volar or dorsal.
The fracture line run obliquely into the wrist
joint .
The distal segment displaced anteriorly or
posteriorly carrying the carpus with it .
The fracture easily reduced but it is unstable so
it can easily redisplaced,
the best treatment will be by open reduction
and internal fixation by special plate called
Buttress plate .

Volar Barton managed by open reduction and
plate fixation

Carpal bones
X-ray appearance of the
normal carpus X-ray of a
normal wrist showing the
shape and disposition of the
eight carpal bones: (a)
scaphoid; (b) lunate; (c)
triquetrum overlain by
pisiform; (d) trapezium; (e)
trapezoid; (f) capitate; and (g)
hamate.

Fracture scaphoid bone
It is common in young adults , fracture of the
scaphoid is the commonest of all carpal fractures.
It is caused by fall on out stretched hands.
The most important point in scaphoid fractures is
its blood supply which directed from distal to
proximal direction.
The blood supply is diminished proximally and is
result into non union or a vascular necrosis.
The patient give history of fallen on the ground,
pain around wrist, the appearance may be normal,
there is fullness and tenderness in the anatomical
snuff box ; other diagnostic sign is that, proximal
pressure along the axis of the thumb is painful .

Anteroposterior X-ray, lateral and oblique views are all essentials . Some
time recent fracture show itself only in oblique view as transverse line .
Usually the fracture is transverse and through the narrowest part of the
bone (the waist) , but it could be in the proximal pole or in the tubercle ;
two weeks after injury the fracture will be more obvious.
A few weeks after the injury evidence of non union or a vascular necrosis
appear of the proximal segment.
If union is delayed , cavitations appear on either side of the fracture .
In old ununited fracture there will be sclerosis at the edge and the
appearance will be as there is extra carpal bone .
Sclerosis of the proximal fragment is pathgnomonic of avascular necrosis
of the proximal fragment .
If clinical picture suggest scaphoid fracture but x ray negative, patient
treated as scaphoid and x-ray repeated every 2 weeks.

Treatment :
Most of fracture of the scaphoid are undisplaced fracture and treated by
immobilization in a plaster cast until fracture united ,
usually 8-12 weeks
.
The cast will be applied from upper forearm to just short of the
metacarpo-phalangeal joint of the fingers but it should incorporating the
proximal phalanx of the thumb ; the wrist is held in slight dorsiflexion
and radial deviation, and the thumb forward in ( GLASS HOLDING )
position and it should be retained for 8 weeks .
After 8 weeks the cast removed and the wrist examined clinically and
radiologically , if there is no tenderness and the x-ray show sign of
healing , the wrist is left free.
If there is local tenderness or the fracture is still visible in x-ray , the cast
is reapplied for further 4 weeks and after that either the wrist become
painless and the fracture healed so the cast removed or the x-ray show
sign of delayed healing then we should do fixation and bone grafting .
In unusual cases the fracture Displaced and it should be treated by open
reduction and fixation by special compression screw .

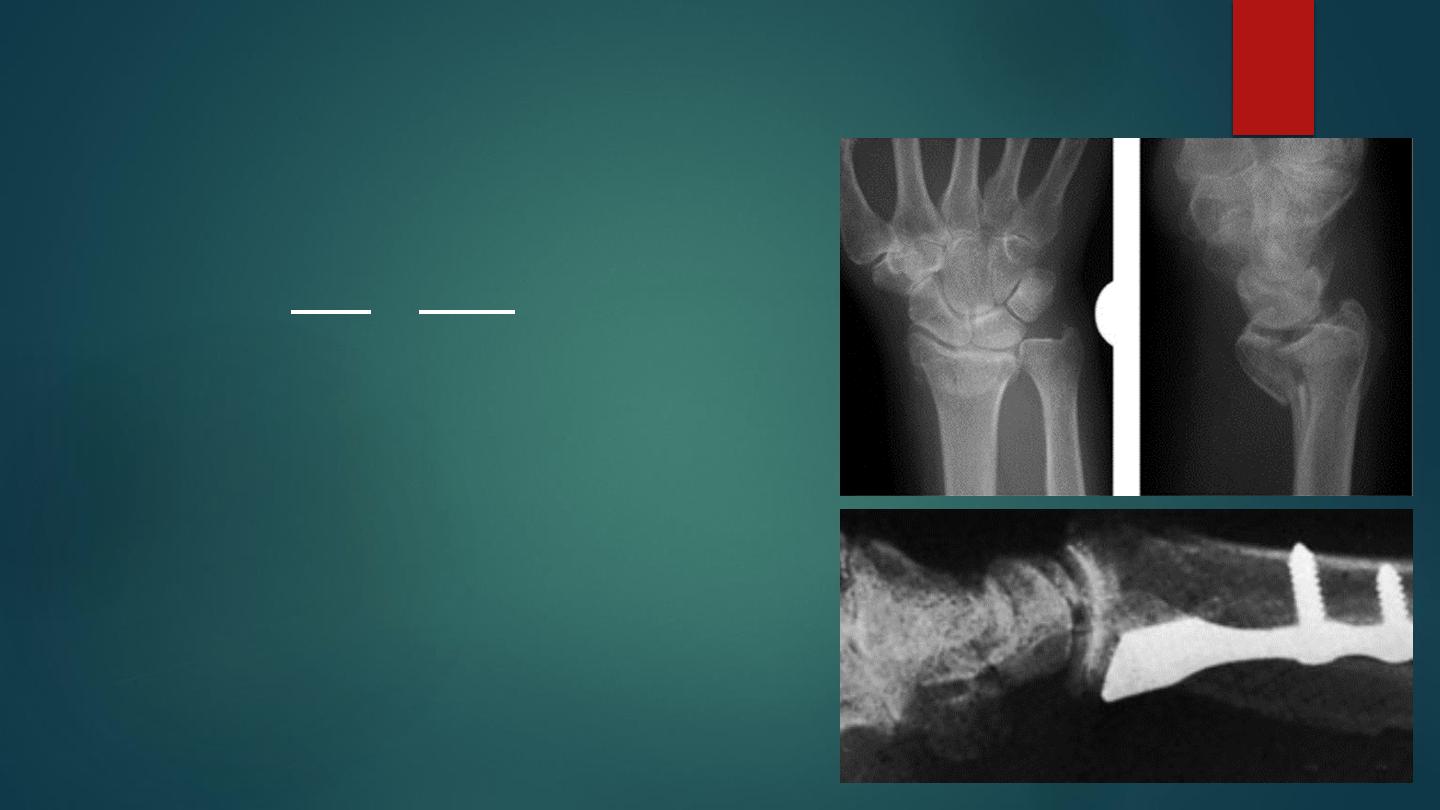
Ulnar side wrist injuries
The distal radio-ulnar joint is
often injured with a radial
fracture; it can also be
damaged in isolation,
particularly after hyper
pronation. The triangular
fibrocartilage complex )TFCC(
can be torn, the ulnar styloid
avulsed or the articular
surfaces of the ulnocarpal joint
or distal radio-ulnar joint
damaged
There is tenderness over the
distal radio-ulnar joint and pain
on rotation of the forearm. The
distal ulna may be unstable; the
piano-key sign is elicited by
holding the patient’s forearm
pronated and pushing sharply
forwards on the head of the
ulna.

A lateral x-ray in pronation and
supination shows incongruity of the
distal radio-ulnar joint. The
anteroposterior view may show an
avulsed ulnar styloid. Arthrography,
MRI and arthroscopy may be needed
to confirm the diagnosis.
Instability usually resolves if the arm
is held in supination for 6 weeks;
occasionally a K-wire is needed to
maintain the reduction. If the
dislocation is irreducible, this may be
due to trapped soft tissue, which will
have to be removed. Chronic
instability may require reconstructive
surgery. A TFCC tear should be
repaired and the ulnocarpal capsule
reefed. A displaced fracture at the
base of the ulnar styloid, if painful or
associated with instability of the
radio-ulnar joint, should be fixed with
a small screw.
Dislocations of wrist
Dislocation of the lunate bone:
lunate bone is liable to dislocate anteriorly on fall in
extended wrist, lateral x-ray shows the lunate
displaced in front of wrist. Lunate dislocation
treated by manipulation in extension, local pressure
and fixation by Kirschner wires followed by plaster
for 4 weeks.
If reduction failed , the dislocated bone excised.
Lunate dislocation might be complicated by median
nerve compression, avascular necrosis of the lunate,
and osteoarthritis.
Pure dislocation of wrist is rare, treated by
manipulation and percutaneous fixation by
Kirschner wires

LUNATE DISLOCATION

Bennett`s fracture-subluxation
This fracture occur at the base of the first metacarpal
bone associated with subluxation and it commonly
resulted from longitudinal violence. The fracture is
oblique extend into carpometacarpal joint and it is
unstable .
Clinically : the thumb looks short and the
carpometacarpal region swollen .
X-rays show the fracture at the base of the metacarpal
bone.
Treatment : Perfect reduction is essential by
manipulation ( pulling the thumb then abducting and
extending it), then reduction held by well molded
plaster .
Open reduction and internal fixation by screw or k –
wire indicated if the fracture are unstable, it is the
reliable method of treatment in this injury.
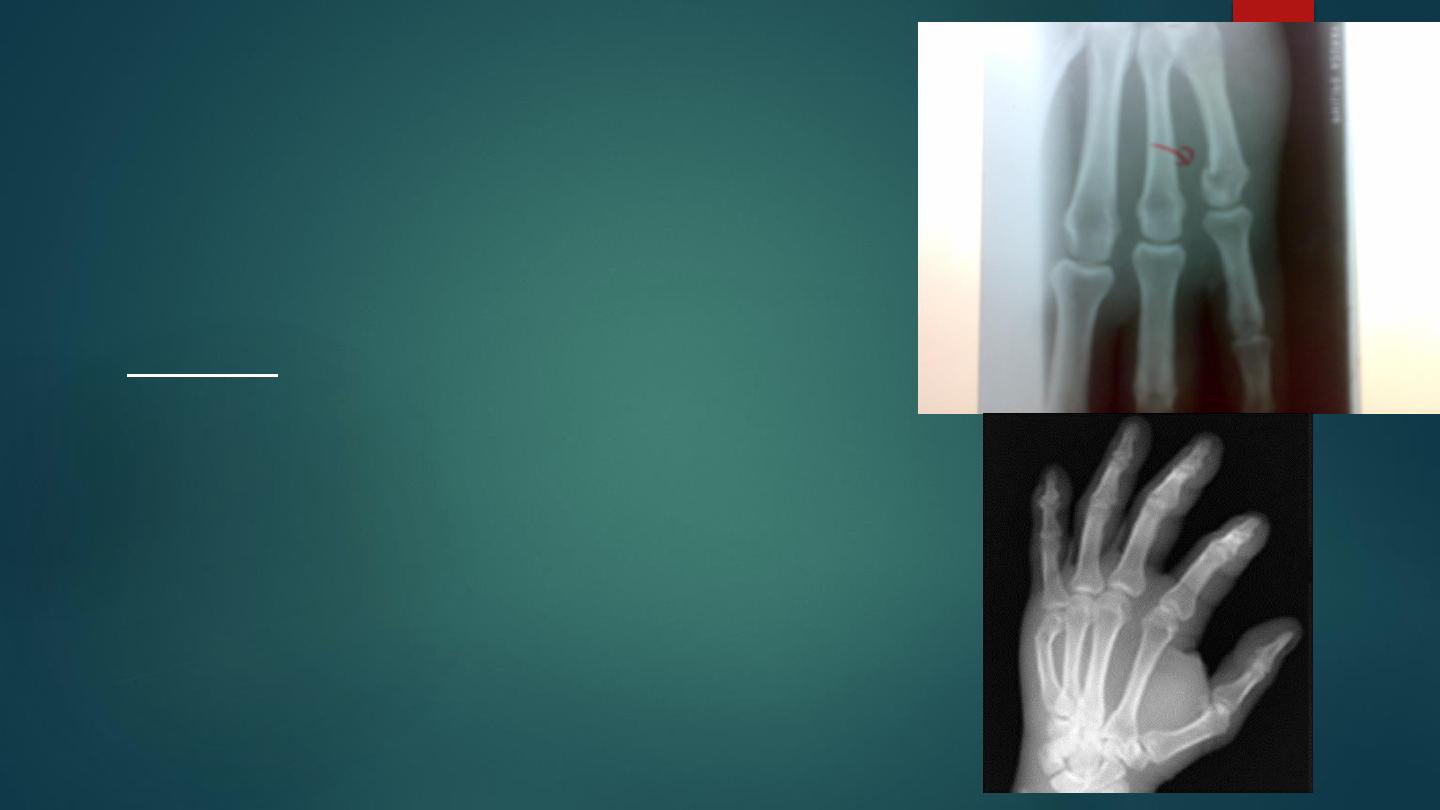
Fracture of the metacarpal neck
A blow may fracture the metacarpal neck , usually of the fifth
finger the (BOXER`S) fracture . There is pain , tenderness,
local swelling with flattening of the knuckle .
X-ray shows an impacted transverse fracture with volar
angulation of the distal fragment .
Treatment :
conservative treatment : by manipulation and holding the
fracture by splint in a position the metacarpo-phalangeal joint of
the fifth finger is in flexion and the interphalangeal joints are in
extension for 2-3 weeks then the hand is mobilized .
The patient is warned that the knuckle profile may be
permanently lost.
If the fracture severely displaced may need reduction and
fixation this done by percutaneous pinning or by open reduction
and fixation by Kirschner wire, malunion is common.
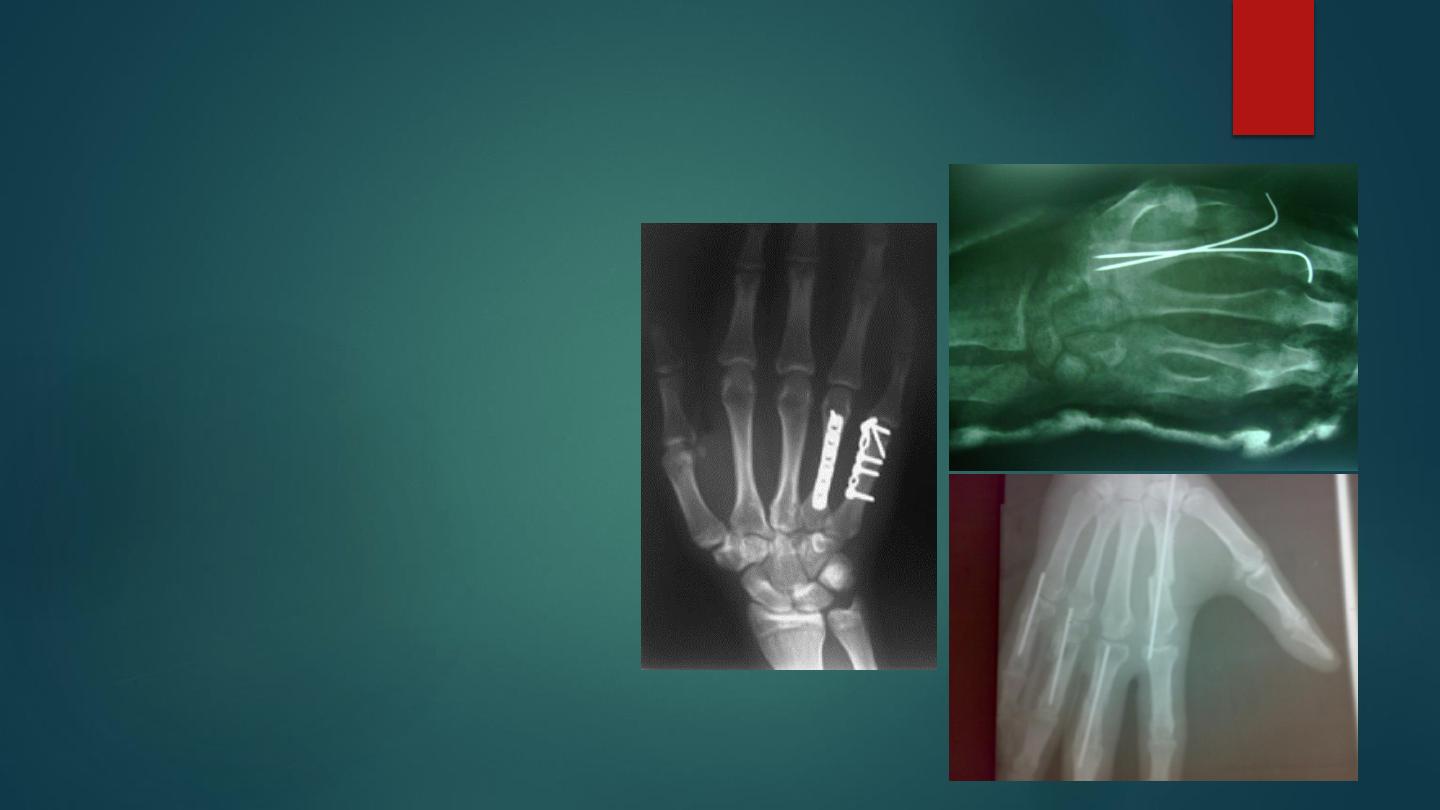
Other fractures of the metacarpal bones:
these injuries are common, result
from fall or blow on hand.
Fractures might be any pattern,
and affect base, shaft, neck, or
head of metacarpal, it may be
single or multiple. The treatment
depend on degree of
displacement. Undisplaced
fractures and stable fractures after
reduction treated by splintage for
3 weeks.
Unreducible, unstable, or
multiple metacarpal fractures
treated by open reduction and
internal fixation.

GENERAL PRINCIPLES OF
TREATMENT OF HAND INJURIES
Most hand injuries can be dealt with under local or regional anesthesia; a
general anesthetic is only rarely required. If the circulation is threatened, it
must be promptly restored, if necessary by direct repair or vein grafting.
Swelling must be controlled by elevating the hand and by early and
repeated active exercises.
Incorrect splintage is a potent cause of stiffness; it must be appropriate and
it must be kept to a minimum length of time. If a finger has to be splinted,
it may be possible simply to tape it to its neighbor so that both move as
one; if greater security is needed, only the injured finger should be splinted

If the entire hand needs splinting, this must always be in the
‘
position of safety
’ – with the metacarpo-phalangeal joints flexed at
least 70 degrees and the interphalangeal joints almost straight.
Sometimes an external splint, to be effective, would need to
immobilize undamaged fingers or would need to hold the joints of
the injured finger in an unfavorable position )e.g. flexion of the
interphalangeal joints(. If so, internal fixation may be required )K-
wires, screws or plates). Skin cover Skin damage demands wound
toilet followed by suture, skin grafting, local flaps, pedicled flaps or
)occasionally( free flaps. Treatment of the skin takes precedence
over treatment of the fracture. Nerve and tendon injury Generally,
the best results will follow primary repair of tendons and nerves.
Occasionally grafts are require
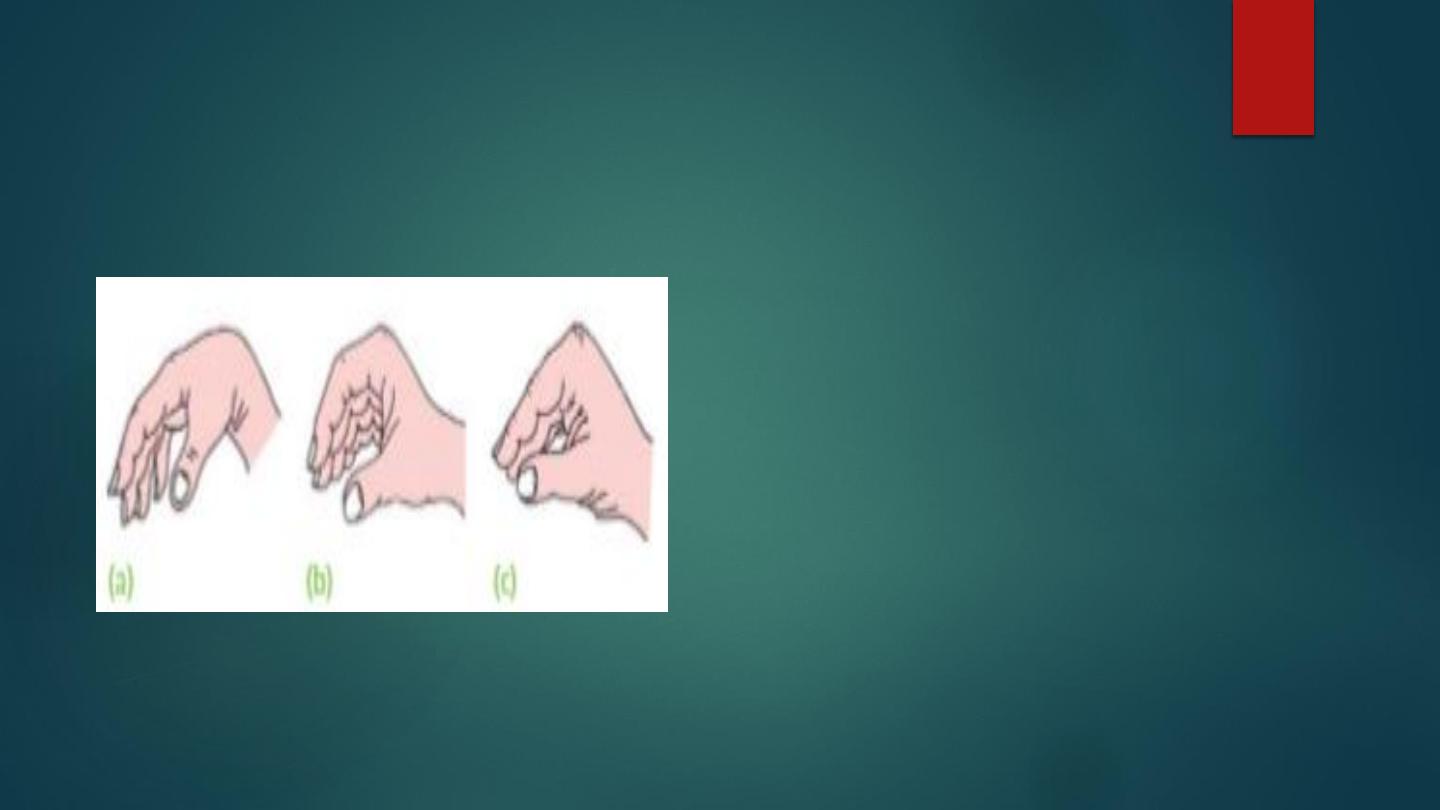
Splintage of the hand Three
positions of the hand: (a) The
position of relaxation, (b) the
position of function (ready for
action) and (c) the position of
safe immobilization, with the
ligaments taut

Fractures of
phalanges:
Different patterns of
fractures might occur,
treated like metacarpal
fractures.
Immobilization should
be kept to a minimum by
splintage in functional
position for 3 weeks.
Surgical treatment
indicated for multiple or
unstable fractures on
same principle of long
bone fractures.
Dislocation of the metacarpo-phalangeal and
interphalangeal joints
Dislocation of the metacarpo-
phalangeal and interphalangeal
joints: the common cause is
forced hyperextension, it
should reduced without
delayed by traction and direct
pressure, x-ray used for
diagnosis and checking
reduction. If the dislocation is
unreducible or unstable after
reduction, operation is
required.
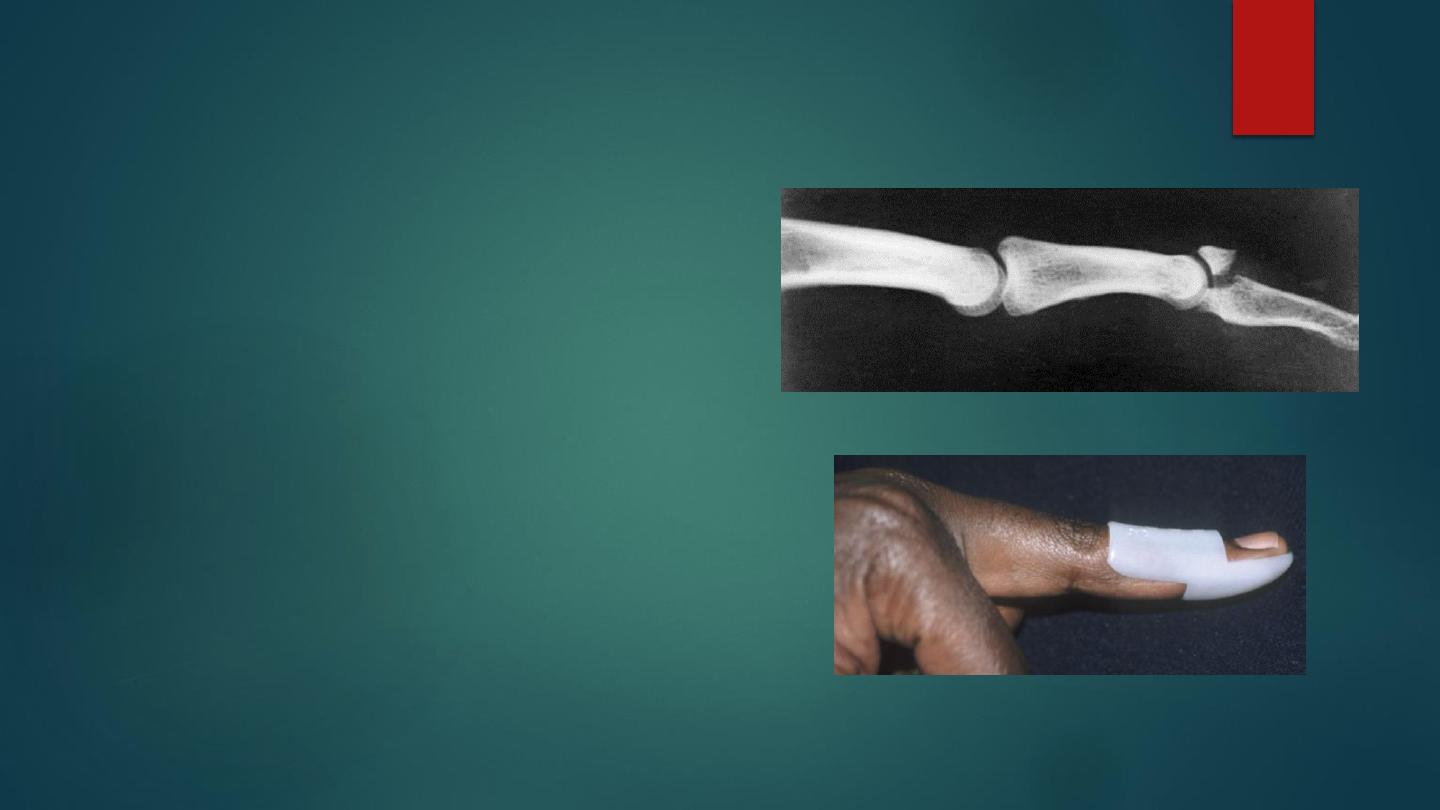
Mallet finger injury:
This injury might fellows a
tendinous avulsion, a small
flake of bone fracture, or a
large dorsal bone fragment.
After as sudden flexion injury
the terminal phalanx droops in
flexion and cannot be actively
extended .
The treatment by immobilizing
the terminal joint in slight
hyperextension by special
mallet splint for 6 weeks or
occasionally k-wire used.
Fracture of the tuft
The tip of the finger may be
struck by a hammer or caught in a
door, and the bone shattered. The
fracture is disregarded and
treatment is focused on
controlling swelling and
regaining movement. The painful
hematoma beneath the finger nail
should be drained by piercing the
nail with a hot paper clip. If the
nail bed is shattered and
cosmoses is important, it should
be meticulously repaired under
magnification
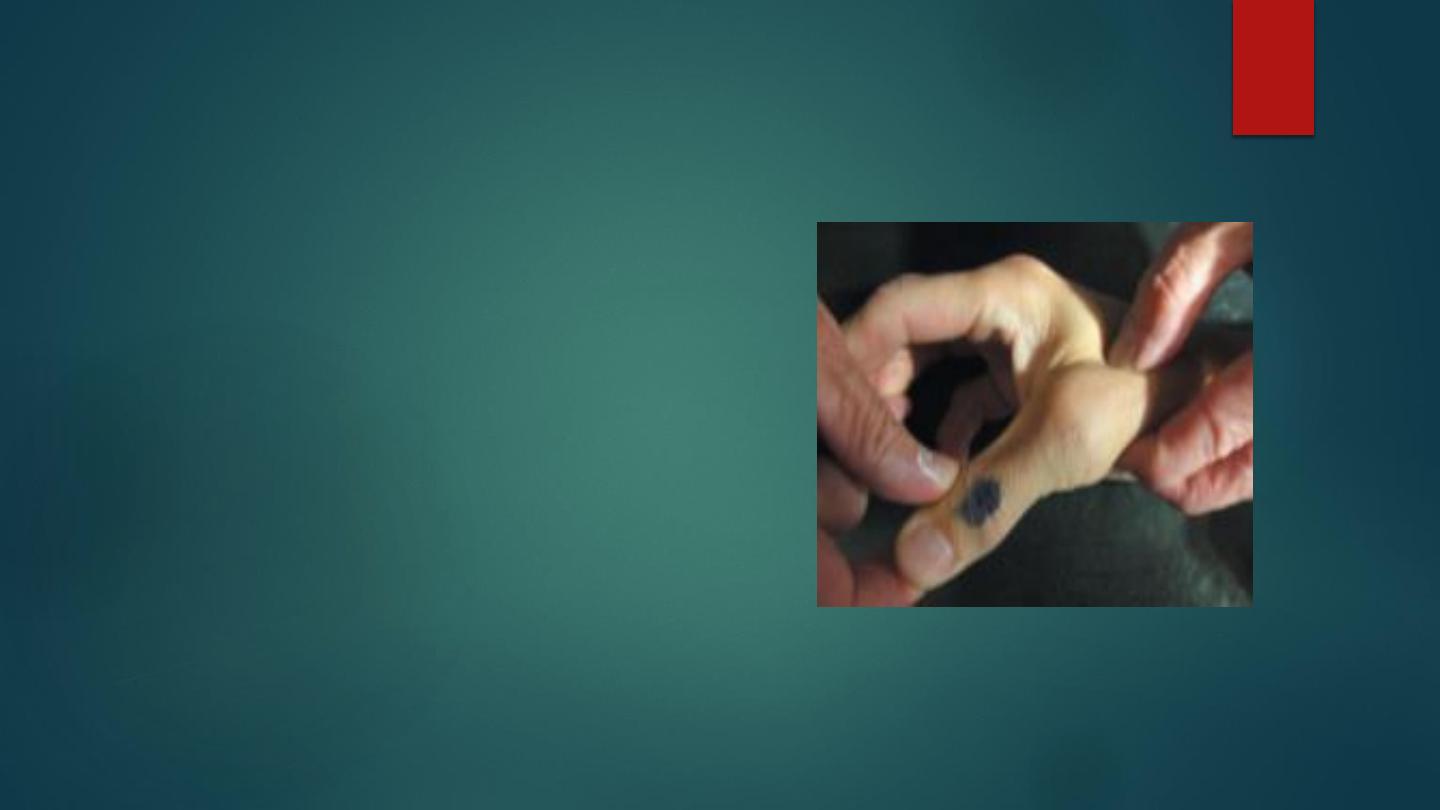
GAMEKEEPER’S THUMB; (‘SKIER’S THUMB’)
The ulnar collateral ligament injury of the
thumb .
On examination there is tenderness and
swelling precisely over the ulnar side of the
thumb metacarpophalangeal joint.
Partial tears can be treated by a short period
(2–4 weeks) of immobilization in a splint
followed by increasing movement. Pinch
should be avoided for 6–8 weeks. Complete
tears need operative repair.

Open injuries
(mangled hand)

Over 75 per cent of work
injuries affect the hands;
inadequate treatment costs the
patient (and society) dear in
terms of functional disability
Open injuries comprise tidy or
‘clean’ cuts, lacerations,
crushing and injection injuries,
burns and pulp defects
Exam for : skin damage ,
vascular state , sensation and
tendons examination
Management as open wound
The precise mechanism of injury
must be understood. Was the
instrument sharp or blunt? Clean
or dirty? The position of the
fingers )flexed or extended( at the
time of injury will influence the
relative damage to the deep and
superficial flexor tendons. A
history of high pressure injection
predicts major soft-tissue damage,
however innocuous the wound
may seem. What are the patient’s
occupation, hobbies and
aspirations? Is he or she right-
handed or left handed?
