
Orthopaedic surgery
فرع الجراحه
\
كلية طب الموصل
peripheral nerve injuries
د
.
ساهر حبيب
دكتوراه
(
بورد
)
اختصاص جراحة العظام والكسور

Anatomy of peripheral nerve
contains:
Efferent (sensory) fibers.
Afferent (motor) fibers.
Sympathetic ( vasomotor and
sudomotor) fibers.
Each nerve fiber (axon) is
covered by Schwan cell.
Connective tissue covers
individual fibers (endoneurium),
bundle of fibers (perineurium)
and the whole nerve
(epineurium
).

Peripheral Nerves injuries
Nerve may be damaged by
ischaemia, pressure ,traction,
bullets, laceration

Pathology of nerve injuries
1- Transient ischemia (anoxia)
Acute nerve compression causes numbness and tingling within 15
minutes, loss of pain sensibility after 30 minutes and muscle
weakness after 45 minutes. These changes are due to transient
endoneurial anoxia and they leave no trace of nerve damage.

2- Neurapraxia
reversible physiological nerve conduction block in
which there is loss of some types of sensation and
muscle power followed by spontaneous recovery
after a few days or weeks. It is due to mechanical
pressure causing segmental demyelination and is
seen typically in ‘crutch palsy’, pressure paralysis in
states of drunkenness (‘Saturday night palsy’) and
the milder types of tourniquet palsy.

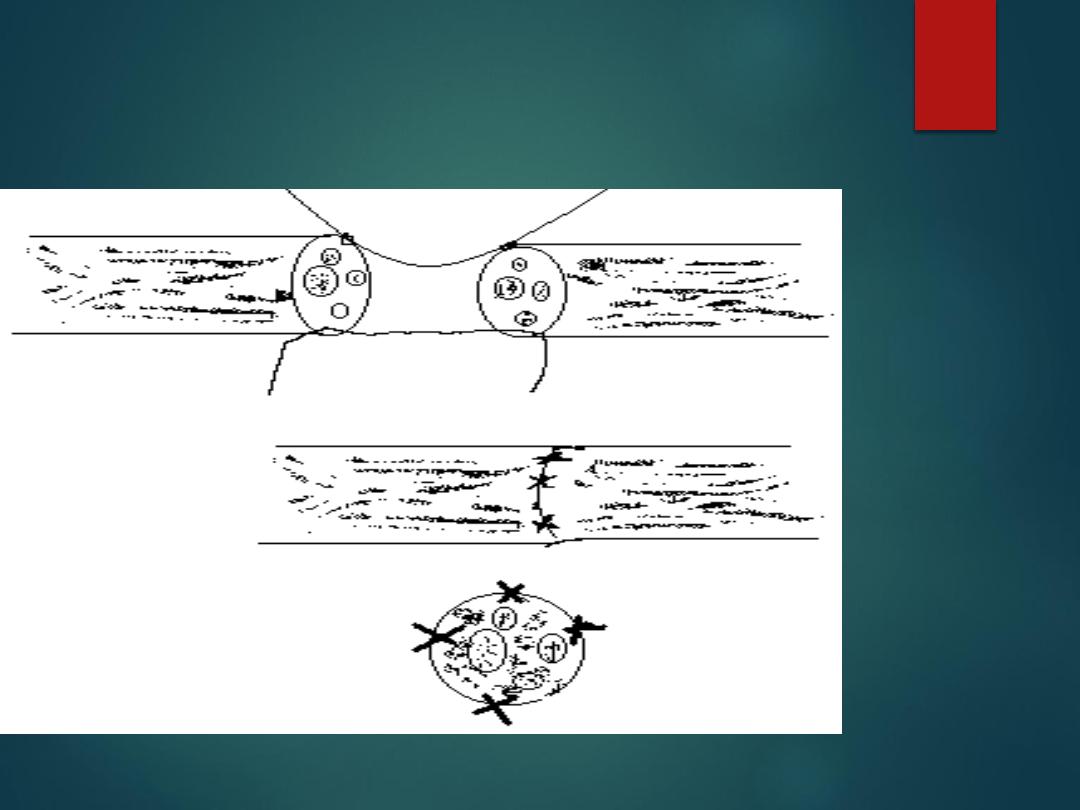
3- Axonotmesis
(axonal interruption)
This is a more severe form of nerve injury, seen typically
after closed fractures and dislocations. The term means,
literally, axonal interruption. There is loss of conduction but
the nerve is in continuity and the neural tubes are intact.
Distally the axon undergo wallerian degeneration , then,
axonal processes grow at a speed of 1–2 mm per day, the
larger fibers slowly acquiring a new myelin coat. Eventually
they join to end-organs, which enlarge and start functioning
again
.

4- Neurotmesis
neurotmesis mean division of the nerve trunk, such as may occur
in an open wound, recovery will not occur. As in axonotmesis,
there is rapid wallerian degeneration, but here the endoneurial
tubes are destroyed over a variable segment and scarring
preventing any hope of regenerating axons from entering the
distal segment and regaining their target organs. Instead,
regenerating fibres mingle with proliferating Schwann cells and
fibroblasts in a jumbled knot, or ‘neuroma’, at the site of injury.
Even after surgical repair, function may be adequate but is never
normal.

The ‘double crush’ phenomenon There is
convincing evidence that proximal compression
of a peripheral nerve renders it more susceptible
to the effects of a second, more peripheral injury.
This may explain why peripheral entrapment
syndromes are often associated with cervical or
lumbar spondylosis. A similar type of ‘sensitization’
is seen in patients with peripheral neuropathy due
to diabetes or alcoholism.

Clinical features
Nerve injuries are easily missed. Always test for nerve
injuries in any trauma.
Sensory loss, numbness, anesthesia should be mapped.
On examination (should be systematic) Sudomotor changes;
the skin dry, shiny and smooth, wasting of muscles, and
ulcers .
Muscle weakness , certain movement lost or weak. The
examination must be repeated at intervals.
Postural deformities; e.g.claw hand after ulnar nerve injuries.

Assessment of nerve recovery
Repeated tests for light touch and power.
Motor recovery is slower than sensory recovery.
Tinel’s sign: peripheral tingling on percussing the nerve at site of
injury.
It should progress at 1mm/day as axonal regeneration takes place.
Nerve conduction test and Electromyogram (EMG).

Principals of treatment
Nerve exploration
: indicated in clean cut wound by sharp object or when nerve
seen to be divided or when nerve recovery delayed.
Primary repair
: the best as it can done safely.
Delayed repair
: weeks or months after injuries. The stump brought together and
end resected and repaired.
Nerve guide
:It is now apparent that nerve gaps can regenerate through a tube
which excludes the surrounding tissue from each end. The tubes can be autogenous
vein, freeze-dried muscle, silicone or metal; soluble guides )flexible at body
temperature) which dissolve over weeks or months are also used.
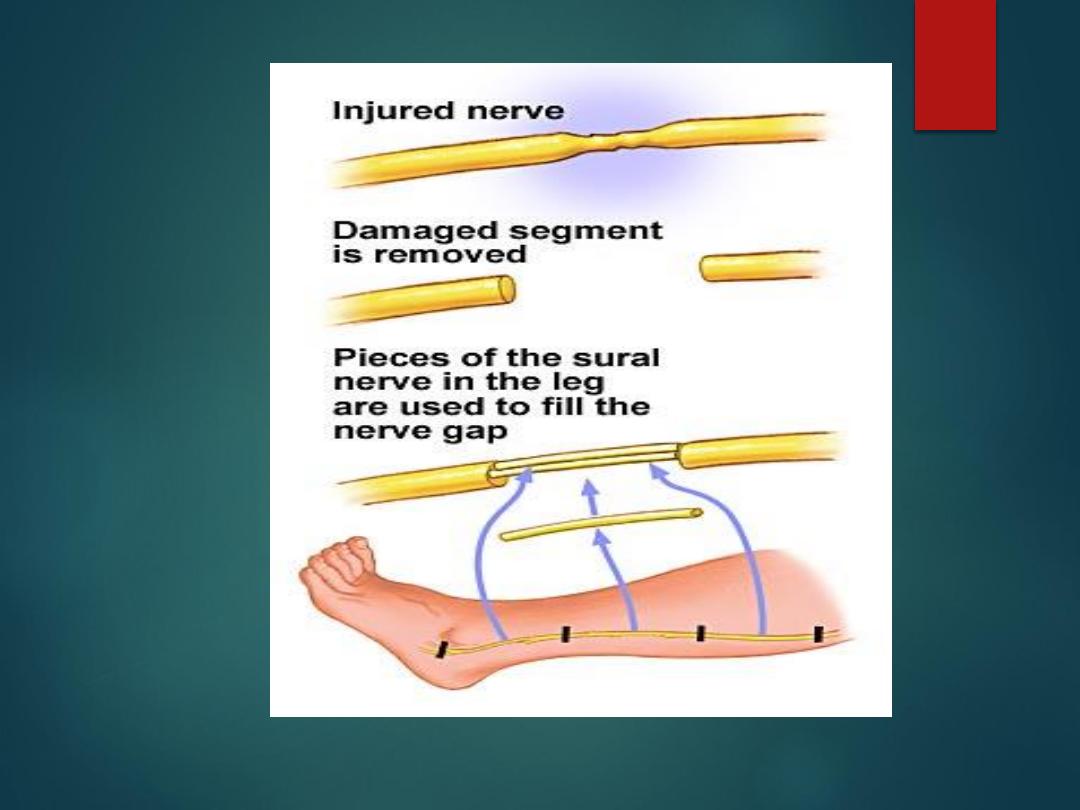
Nerve grafting
: to close gaps. Sural nerve ( up to 40 cm )is commonly used.
Nerve transfer:
may used in sever injuries, e.g. for proximal brachial plexus
injuries.
Tendon transfer
: for nerve injuries unlikely to heal. healthy tendons transferred to
paralyzed ones.
Care of paralyzed parts is very important.
Eipneural repair

Prognosis
Depended on the following factors:
• Type of lesion
. neurapraxia always recover.
neurotmesis wouldn't improve unless repaired
• Level of lesion
: the proximal is worse.
• Type of nerve
: mixed nerve worse.
• Size of gap
. Larger gap worsen prognosis
• Age
. younger is better
• Delay in repair
. No repair after one year.
• Associated lesions
. Compound fractures and infection
, vascular injury worsen prognosis.
• Surgical technique
. Trained team, good facility, use of
microscope better.
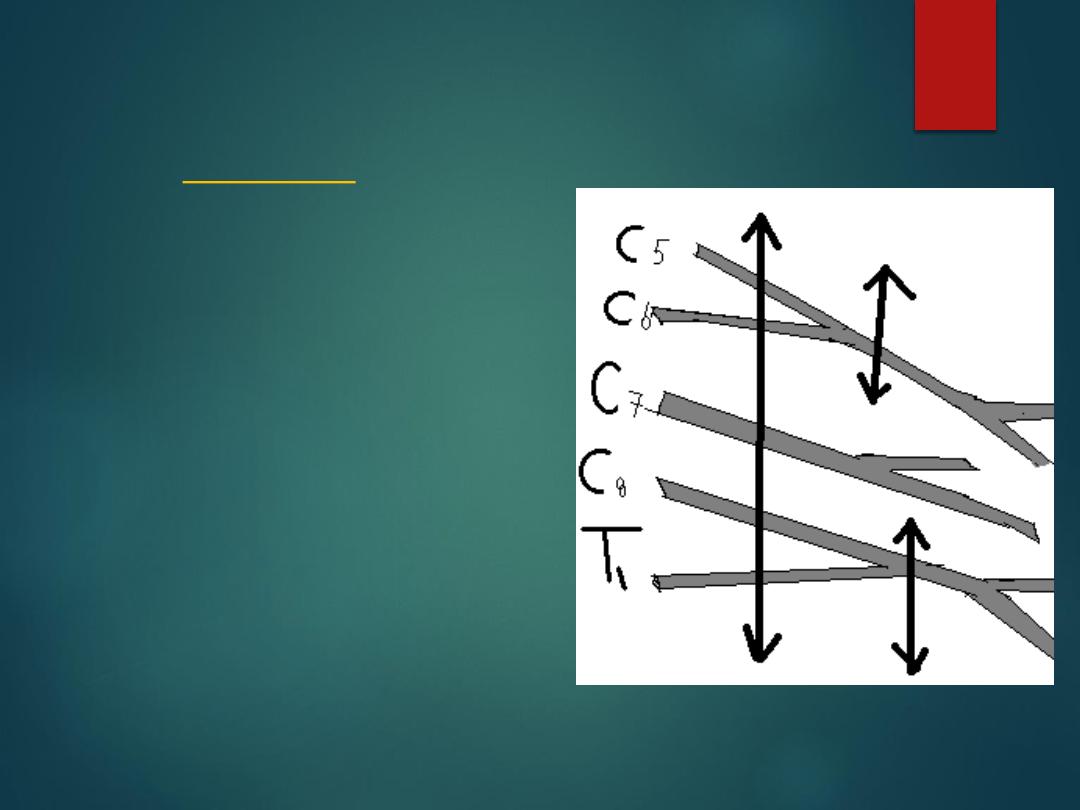
Brachial plexus injuries
( Traumatic )
Sever traction is the
commonest cause, some
time caused by stab , shell
or bullet.
Clinical feature depend
on severity and site of
injures. There's motor and
sensory defect.
The proximal injuries had
bad prognosis.
(Birth injuries)
Caused by traction during difficult labor
1.the most common is the upper root lesions (
Erb’s palsy) C5, C6, C7 nerve root injury, the
limb is adducted, internally rotated and
pronated.. (waiter tip position).
2. The lower root lesion C8 –T1(Klumpke’s
palsy) the muscles of hand and finger paralyzed,
hand clawing and possibly horner syndrome.
3. Complete , The limb is flail and pale.
Associated with Horner syndrome.

Erbs palsy klumpke
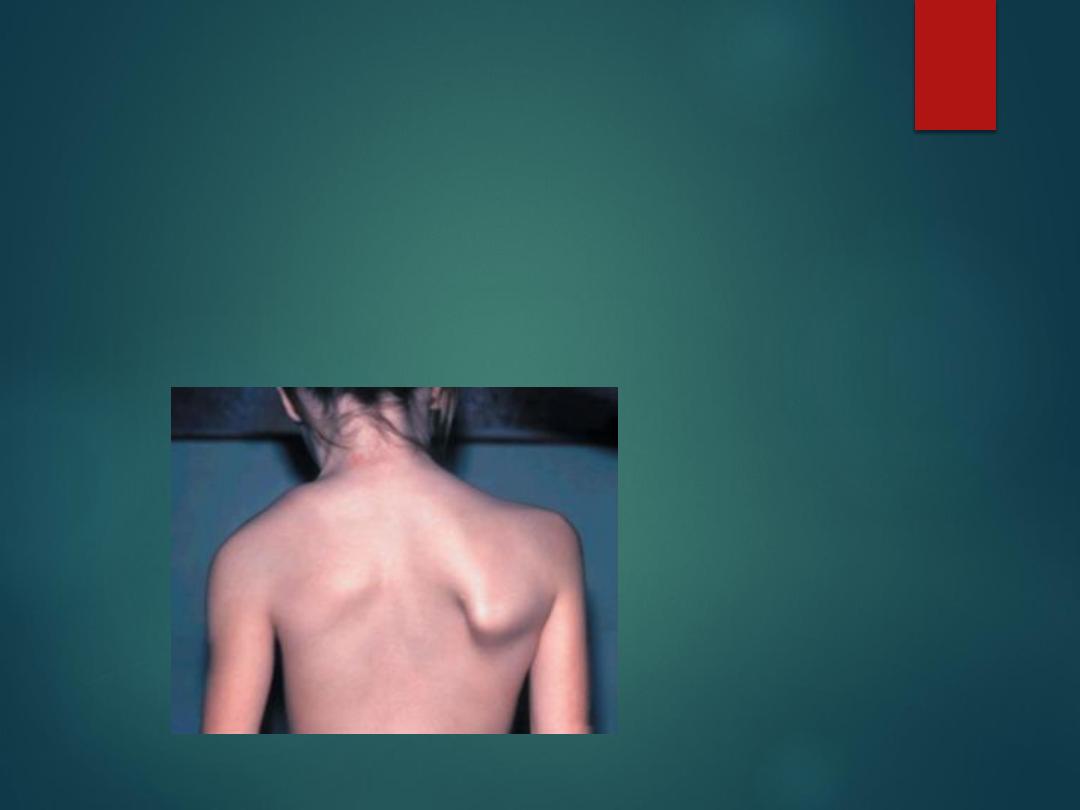
Long thoracic nerve injury
(C5,C6,C7
)
After trauma or surgery like radical mastectomy.
Paralysis of serratus anterior causes medial winging of the
scapula.

Spinal accessory nerve
C2-C6
Following an open wound or operation, typically
there is mild winging of the scapula on attempting
active abduction against resistance; unlike the
deformity in serratus anterior palsy, this
disappears on flexion or forward thrusting of the
shoulder. Often the true nature of the problem is
not appreciated and diagnosis is delayed for weeks
or months. In late cases there may be wasting of
the trapezius.
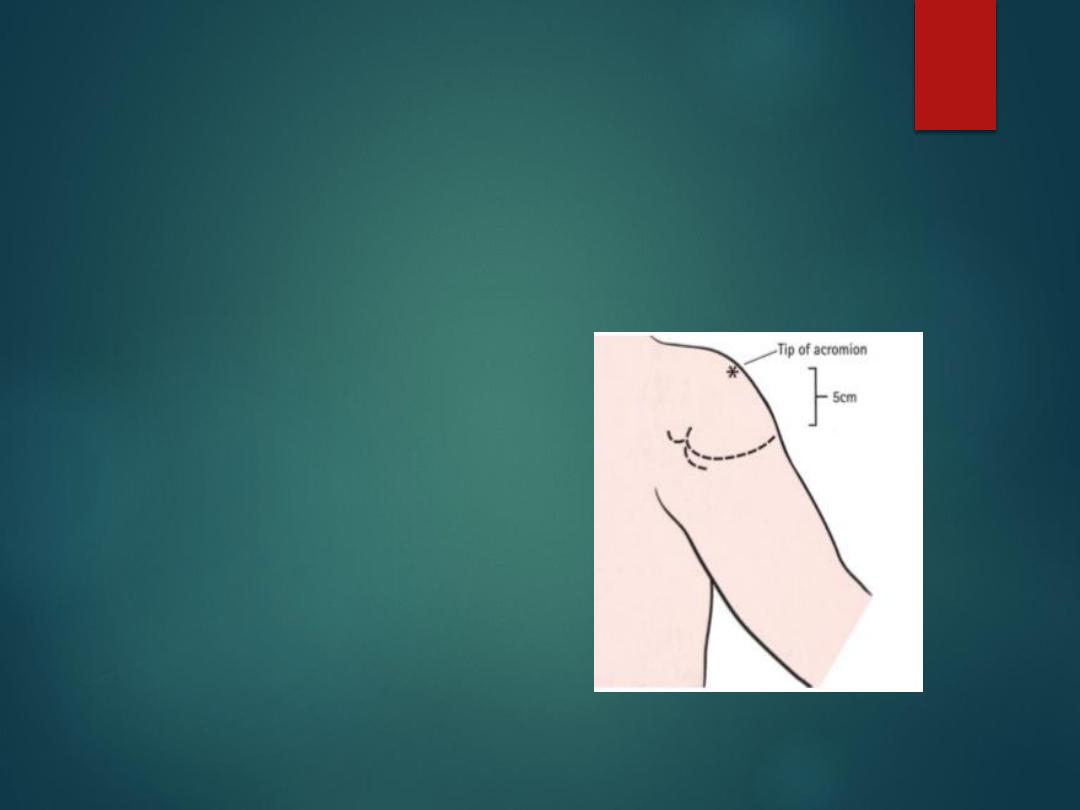
Axillary nerve
(C5,C6)
Injured after shoulder dislocation or fracture of the neck of
humerus.
Wasting of the deltoid.
Weak shoulder abduction.
A patch of Numbness over deltoid.
Radial nerve
Radial nerve may be injured at arm or elbow or axilla.
Low lesions
at elbow : Cannot extend metacarpophalangeal joint.
High lesions
at level of humerus: Wrist drop due to paralysis of forearm
extensors. There is patch of anesthesia on dorsum of first wed space.
Very high lesions
. At level of axilla. The triceps also paralyzed. “Saturday night
palsy” and “Crutch palsy”.
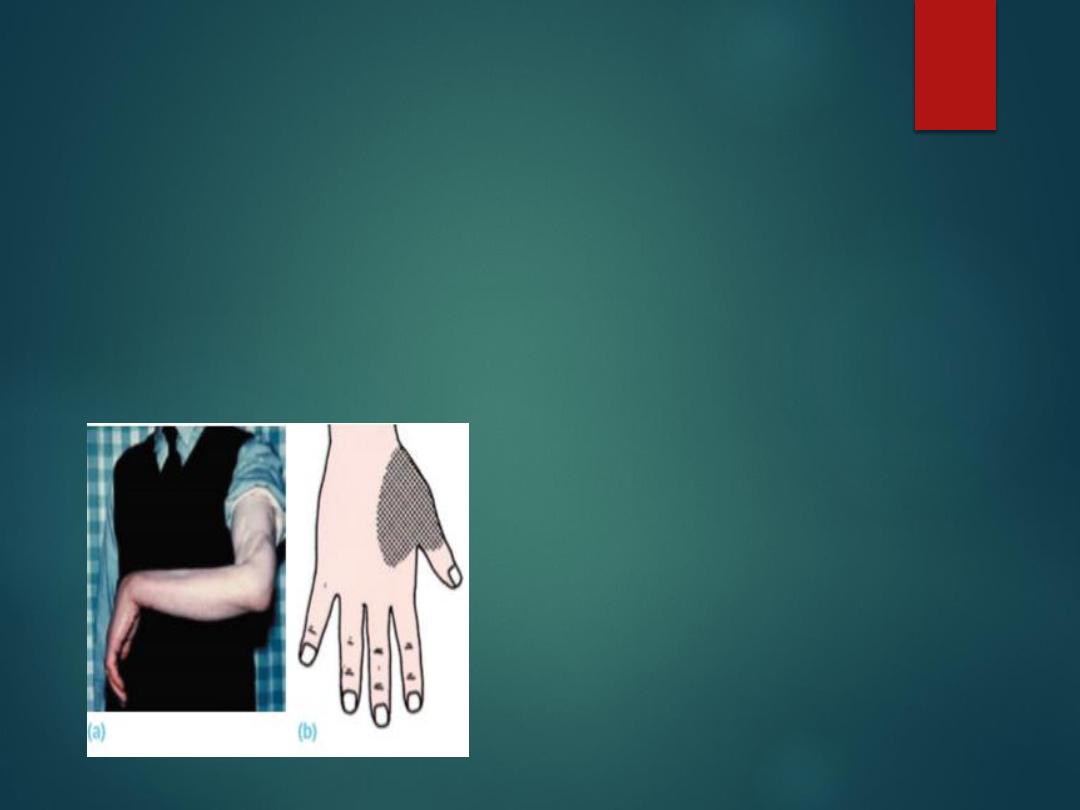
Radial nerve palsy (a) This man developed a
complete drop-wrist palsy following a severe
open fracture of the humerus and division of
the radial nerve. (b) The typical area of sensory
loss

Treatment of radial nerve injuries
Clean Open wound treated by
primary repair.
If injures associated with closed
fractures and there is no sign of
recovery after 6 weeks surgical
exploration is indicated.
Tendon transfer used if no recovery
achieved.
Physiotherapy used while waiting
for recovery.

Ulnar nerve
low lesions
Usually associated with cut wrist or at lower forearm.
There is anesthesia and Numbness in ulna side of one and a half fingers.
Claw hand deformity: hyperextension of MPJ of ring and middle fingers.
Wasting of hypothenar and interosseous muscles.
Weakness of thumb adduction; “Froments sign”: inability to grip a paper
between the thumb and index finger.
High lesions
Accompany fractures and dislocations around the elbow.
Same motor and sensory loss but “less clawing”.
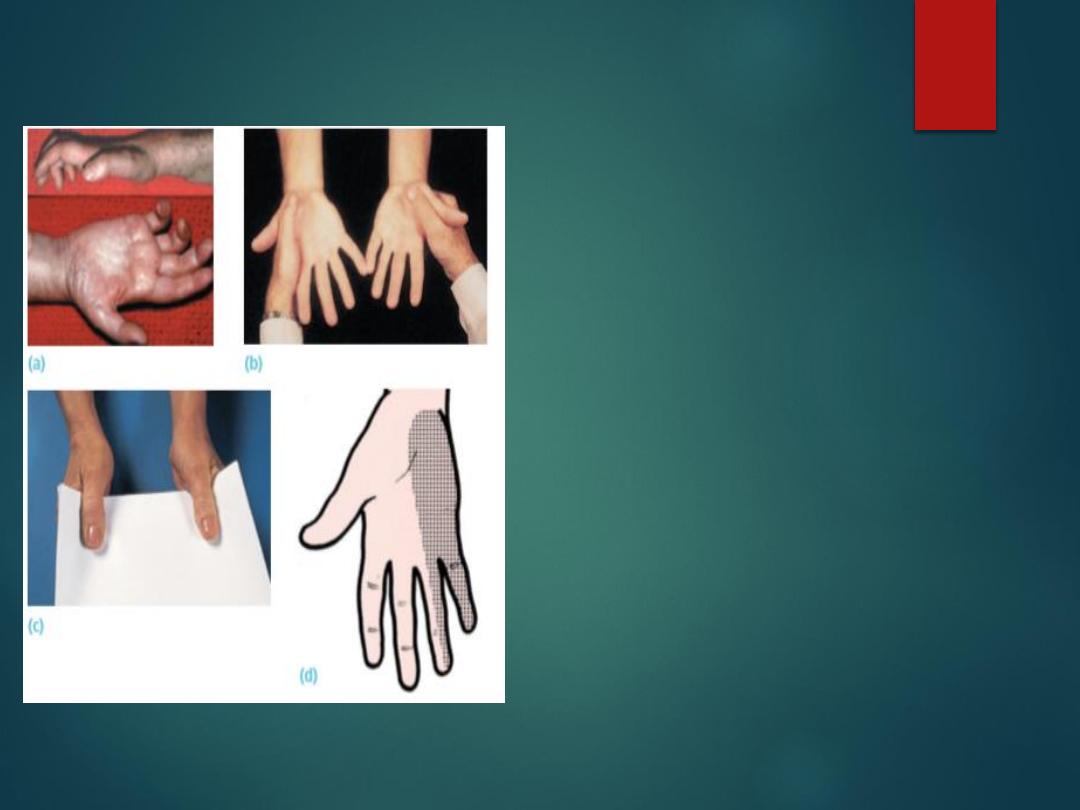
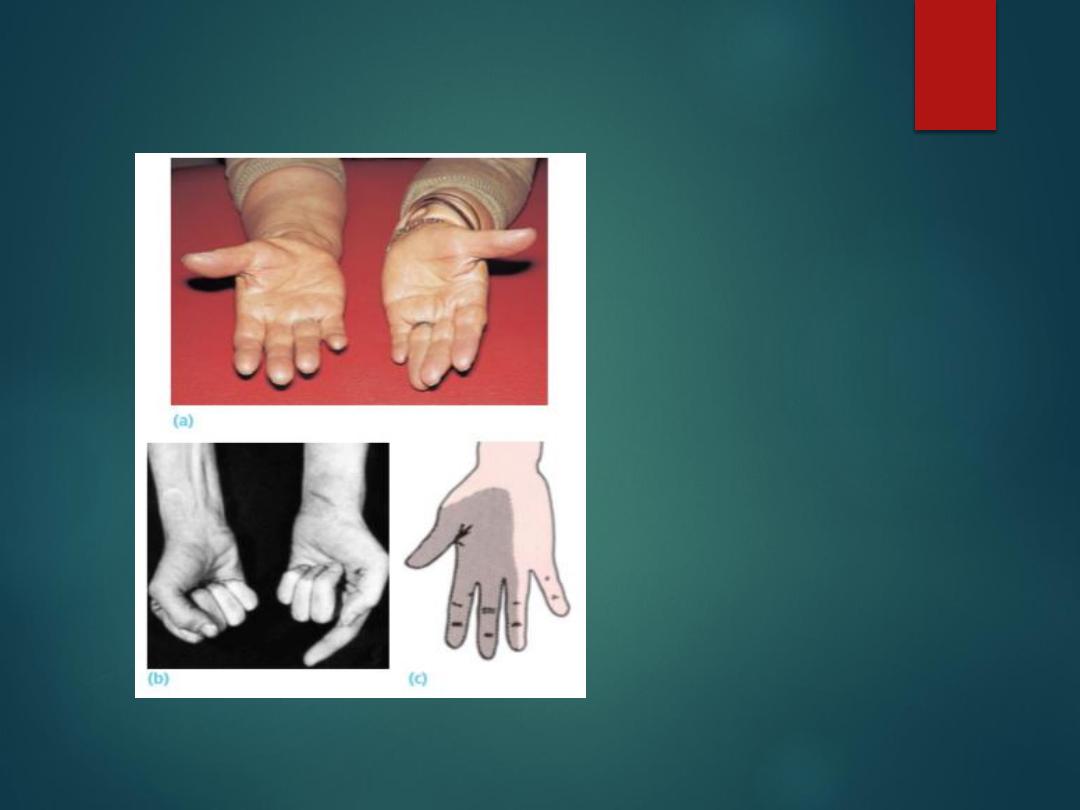
Ulnar nerve palsy (a) Clawing of the ring
and little fingers and wasting of the
intrinsic muscles. (b) A good test for
interosseous muscle weakness. Ask the
patient to spread his fingers )abduct( as
strongly as possible and then force his
hands together with the little fingers
apposed; the weaker side will collapse (the
left hand in this case). (c) Froment’s sign:
the patient is asked to grip a card firmly
between thumbs and index fingers;
normally this is done using the thumb
adductors while the interphalangeal joint is
held extended. In the right hand, because
the adductor pollicis is weak, the patient
grips the card only by acutely flexing the
interphalangeal joint of the thumb )flexor
pollicis longus is supplied by the median
nerve). (d) Typical area of sensory loss.
Median nerve
low lesions
Follow cut wrist or carpal dislocation.
Numbness over three and a half radial fingers.
Weakness of thumb abduction.
Wasting of thenar eminence.
High lesion
With elbow dislocation or stabs or gun shots.
Above + weak flexors of thumb, index, middle fingers and
wrist.
Pointing index sign.
Median nerve lesions
(a) Wasting of the
thenar eminence on the
right side. (b) In high
median nerve lesions,
the long flexors to the
thumb and index
fingers are also
paralyzed and the
patient shows the
‘pointing index sign’.
(c) Typical area of
sensory loss.

Sciatic nerve
May occur at different level and by different mechanism ;
Gunshots, traumatic hip dislocation, after total hip replacement or
intramuscular injection.
Hamstrings and all muscles below knee are paralyzed.
Sensation below knee is lost except medial side.
Patient walk with drop foot
Common peroneal may be injured alone or with sciatic nerve
.

Common Peroneal nerve
Injuries or trauma around knee or neck of fibula.
Skin traction or tight cast. Prolonged lying with leg
externally totated.
Patient has foot drop and cannot dorsifles or evert
the foot.
High stepping gait.
Sensation lost over dorsum of foot
.

Tibial nerve
Penetrating wounds may divide the nerve.
Patient cannot plantarflex the foot.
Sensation is lost in sole of the foot.
Pressure sores develop later
.

How would managed patient with foot
drop
1- detailed history should be taken, foot drop might result from injury
to sciatic nerve or common peroneal from leg to vertebra. Prolapsed
disc, plexus injuries, hip fractures and dislocations, stabs, bullet, knee
injures, local pressure, compartment syndrome of leg might be the
cause.
2- detailed clinical examination including the neurological,
muscloskeletal ,back examination , with documentation of sensory
and motor defect. To repeat the examination and to check the
changes. Electromyography, X-ray , MRI, CT scan might used.
3- start physiotherapy by electrical stimulation to prevent muscle
atrophy, dynamic splintage, preserve joint mobility and to protect the
foot while waiting for nerve recovery.
4. Treatment nerve injury itself according to its cause, if the wound is
cutting direct repair indicated, prolapsed disc removed, if theirs
closed injury we can wait for 6 weeks if no improvement the nerve
should be explored and repaired.
5- reconstructive procedure might used if no improvement occur or in
neglected cases like tendon transfer or arthrodesis
.
