Cerebral Oedema and Increased Intracranial Pressure (Intracranial Hypertension)
Cerebral Oedema• Vasogenic Oedema
• Cytotoxic Oedema
Vasogenic Oedema
It is the most common form of brain oedema encountered in clinical practice.This type is due to increased permeability of cerebral capillaries with resultant accumulation of plasma or its filtrate to enter the extracellular space of the brain. This type is seen commonly in trauma, primary and metastatic tumours and focal inflammation like brain abscess.
Cytotoxic Oedema
Derangement of cellular metabolism which result in inadequate functioning of the sodium and potassium pump leading to cellular retention of sodium and water and cell swelling.This type is seen in various intoxications (e.g., dinitrophenol), Reye’s syndrome and sever hypothermia.
Increased Intracranial Pressure (Intracranial Hypertension)
• The adult skull :• Brain.
• Cerebrospinal Fluid (CSF).
• Blood.
Increased Intracranial Pressure (Intracranial Hypertension)
The normal supine intracranial pressure is 5-15 mmHg (60-180 mmH2O).
An increase in the volume of any one of the contents of the skull will result in an increase in the intracranial pressure (ICP).
The brains ability to compensate for raised ICP is rapidly exhausted.
Raised ICP is dangerous to the brain.
(Intracranial Hypertension)
Etiology:1. Localized masses like:
a. Haematomas: epidural, subdural, and intracerebral.
b. Neoplasms: gliomas, meningiomas, and metastases.
c. Abscesses (brain abscesses).
d. Focal oedema due to traumas, infection, and tumours.
(Intracranial Hypertension)
2. Obstruction to CSF pathways: as seen in:a. Obstructive hydrocephalus.
b. Communicating hydrocephalus.
3. Obstruction to major venous sinuses as a result of:
a. Depressed skull fracture over major venous sinuses.
b. Thromboembolic disease from contraceptive pills.
(Intracranial Hypertension)
4. Diffuse brain oedema or swelling: due to encephalitis, meningitis, diffuse head injury, subarachnoid haemorrhage, Reye's syndrome, water intoxication from fluid overload.
5. Idiopathic intracranial hypertension is a disease most commonly found in adult female patients (also called pseudotumour cerebri).
6. Systemic hypertension can cause breakdown of the blood brain barrier and causes hypertensive encephalopathy.
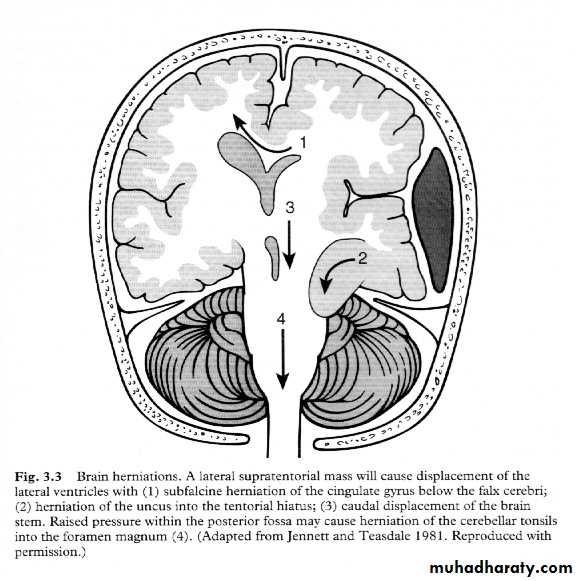
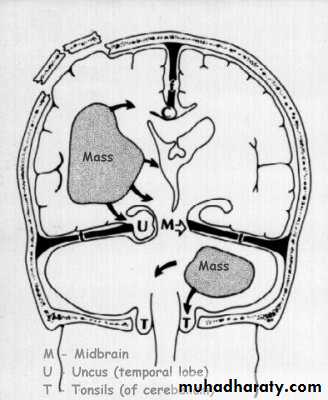
Cerebral Herniation
a. Subfalcine Herniationb. Uncal Herniation
c. Tentorial Herniation
d. Tonsillar Herniation
Cerebral Herniation
Cerebral Herniation
c. Transtentorial Herniation
c. Transtentorial Herniation
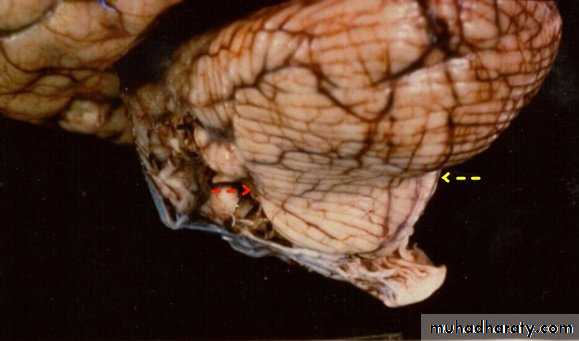
d. Foramen magnum herniation(Tonsillar Herniation)
d. Foramen magnum herniation
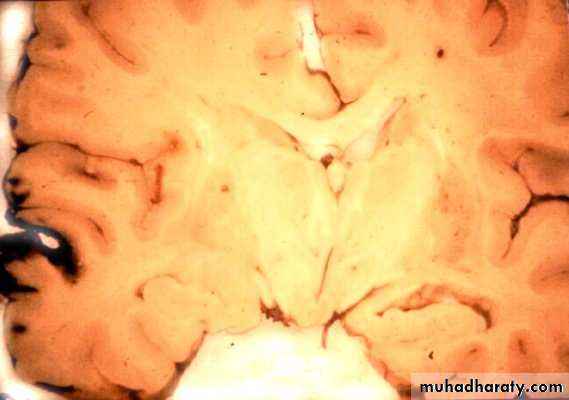
a. Subfalcine Herniation
a. Subfalcine Herniation
Increased Intracranial Pressure (Intracranial Hypertension)
• Without symptoms and signs.
• Headache.
• Nausea and vomiting.
• Drowsiness or altered mental status.
Increased Intracranial Pressure (Intracranial Hypertension)
• 5. Papilloedema• 6. Sixth nerve palsy (False localizing sign).
• 7. At later stages the triad of bradycardia, hypertension and respiratory irregularities.
• 8. In infants: tense bulging fontanelle.
Investigations of Intracranial Hypertension
A. Skull X- RayB. Computed Tomography (CT Scan) of Brain.
C. Magnetic Resonance Imaging (MRI) of Brain
Skull X-ray findings in increased intracranial pressure
• Sutural separation in children.• ‘Copper-beating’ marking of the cranial vault.
• Thinning of dorsum sellae.
• Erosion of the posterior clinoid process.
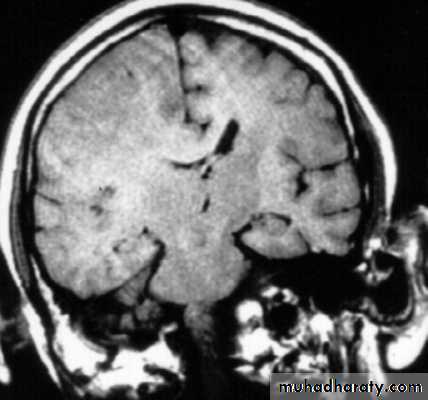
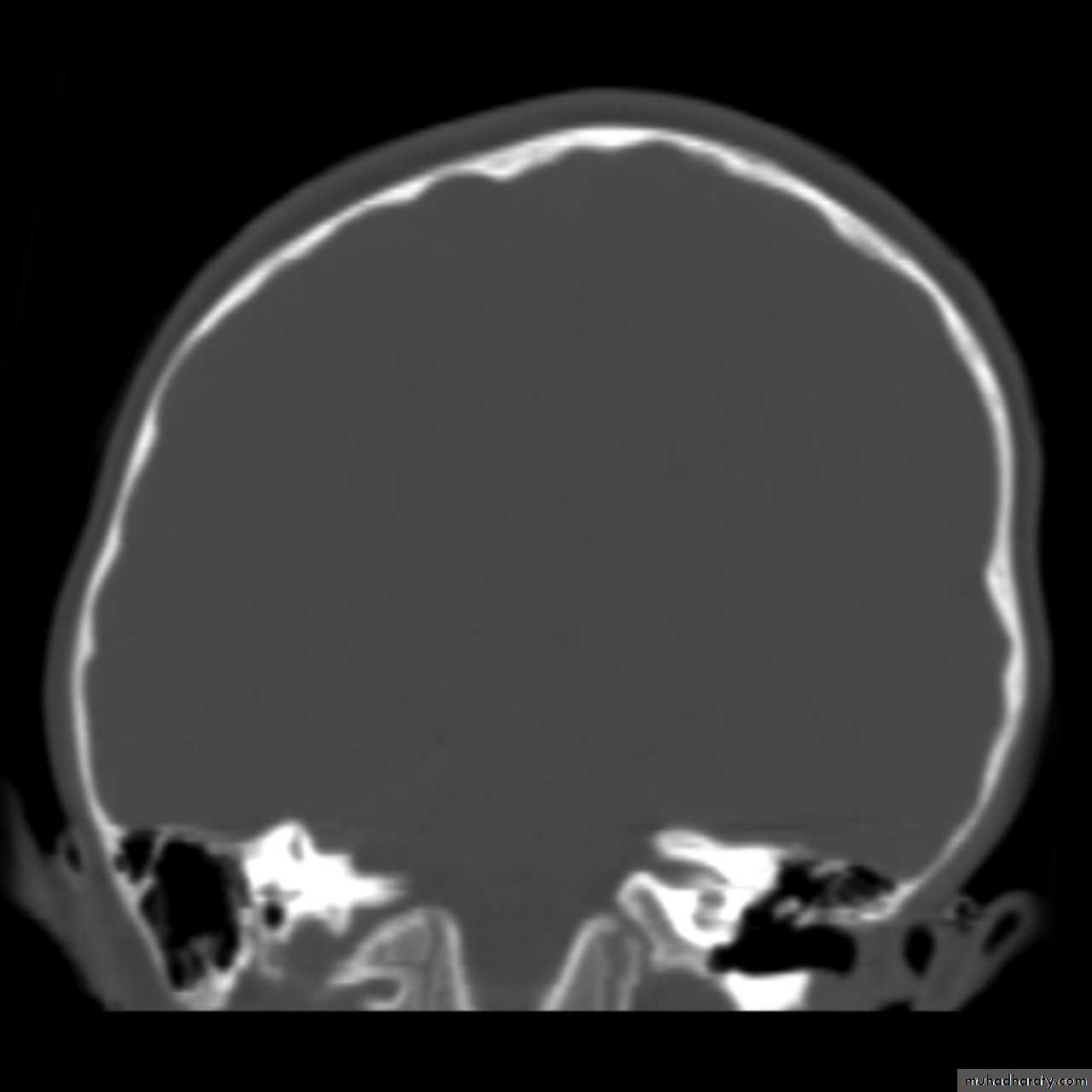
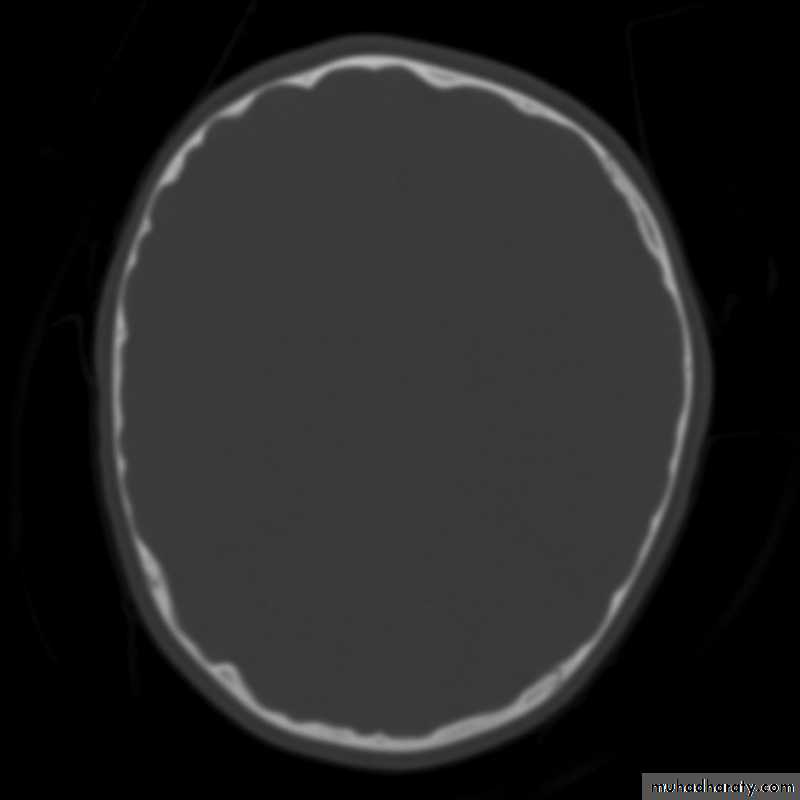
Copper-beating’ marking
Copper-beating’ marking
Copper-beating’ marking
Copper-beating’ marking
Copper-beating’ marking
Copper-beating’ marking
Treatment of Intracranial Hypertension
• Head position (Head elevation).• Hyperventilation: PCO2 down to (30-34 mmHg).
• Hypertonic solutions including:
• Mannitol, dose of 1g/kg
• Hypertonic saline.
• Furosemide (Loop diuretic): act by
Reducing cerebral oedema.
Reduce CSF production.
Act synergistically with mannitol.
Treatment of Intracranial Hypertension
• 5. Steroids (dexamethasone 4mg, 6-hourly).• Stabilizing the blood brain barrier (BBB).
• Reducing oxygen free radicals.
• 6. Ventricular drainage.
• 7. Barbiturates: reducing cerebral metabolism.
• 8. Hypothermia down to 34°C is a brain protective agent.
• 9. Surgical intervention.
Benign intracranial hypertension
Benign intracranial hypertension, also known as pseudotumour cerebri, is, as its name implies, a disease of raised intracranial pressure, which usually runs a self-limiting course.
Although termed ‘benign’, this condition can cause blindness due to severe papilloedema.
The pathogenesis is poorly understood.
The condition usually occurs in obese females.
Aetiology
Hypoparathyroidism.Vitamin A excess (used to treat acne)
Pernicious anaemia.
Drug reaction—tetracycline, nalidixic acid, sulfamethoxazole, indomethacin, danazole, lithium carbonate, oral contraceptive steroids.
A similar condition results from venous sinus thrombosis.
Clinical features:
• Headaches• Visual disturbance.
The headaches have the features of raised intracranial pressure in that they are worse in the morning and exacerbated by straining, stooping and coughing.
The visual problems result from:
• Papilloedema
• Secondary optic atrophy
• Diplopia due to sixth cranial nerve palsy.
Investigations
The CT and/or MRI scan will show no cause for the papilloedema and the ventricles will often be smaller than usual.
Digital subtraction cerebral angiography or magnetic resonance venography may be performed to exclude thrombosis of a venous sinus as the cause.
If the CT scan or MRI shows no mass or lesion a lumbar puncture is usually performed; the pressure will be raised. CSF examination is normal in benign intracranial hypertension but biochemistry and cytological investigations should be performed to exclude underlying pathology.
Medical (Conservative) Treatment
Benign intracranial hypertension is usually a self-limiting disease and most cases respond to simple conservative treatment. The usual measures undertaken are:Conservative Treatment:
Weight loss (the patients are usually obese).
Stopping any medication that may have led to the disease, e.g. oral contraceptives, tetracycline.
Diuretic therapy.
Acetazolamide (reduces CSF production).
If there is no improvement with the above measures, treatment with glycerol or steroids may be tried.
Surgical Treatment
The major indications for surgical treatment are:Persistent severe papilloedema despite conservative measures
Failing vision.
Intractable headaches despite conservative measures.
The surgical procedures that can be performed are:
• Optic nerve sheath decompression
• Lumboperitoneal shunt.
THANKYOU