Benign and malignant skin tumors
Mohamed Enaam AldewachiPlastic and reconstructive surgeon
F.I.B.M.S.
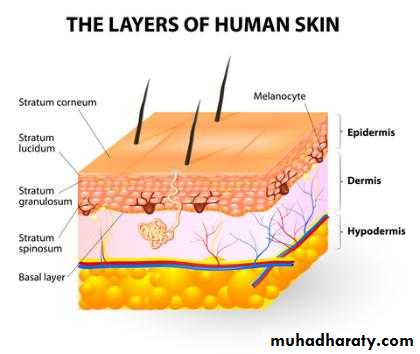
Skin anatomy
A. Epidermis—outer layer1. Cell types: Keratinocytes, melanocytes, Langerhans cells, Merkel cells
2. Superficial to deep: Stratum corneum, lucidum, granulosum, spinosum, basale
B. Dermis
1. Cell types: Collagen, elastin, ground substance2. Nerves, blood vessels, lymphatics, muscle fibers, pilosebaceous/apocrine/ eccrine
glands
3. Two layers superficial to deep
a. Papillary—fibroblasts, mast cells, histiocytes, Langerhans cells, lymphocytes
b. Reticular—thicker than papillary dermis
i. Extends to underlying fat
ii. Contains elastin with interspersed large collagen fibers.
Skin anatomy
Benign lesions
Epidermal nevus (linear nevus)1-Present at birth or early childhood.
2-Clinical presentation: Tan or brown
warty papules.
3-May be associated with
Ocular or central nervous abnormalities.
Treatment: Excision, laser therapy(CO2), dermabrasion, or cryotherapy.
Benign lesions
Seborrheic keratosis: Cystic inclusions of keratinous material.1-Clinical presentation: Waxy, stuck-on appearance; warty papule or plaque.
2-May be yellow, light brown, dark brown, or black in color.
3-Treatment: Dermabrasion, cryotherapy, shaving, and excision.
Seborrheic keratosis
Cutaneous horn
1-Clinical presentation: Well-circumscribed cone with hyperkeratotic features.2-Cutaneous horn can harbor malignancy.
3-Treatment: Excisional biopsy with careful evaluation of lesion base.
Keratoacanthoma
Clinical presentation: Firm, dome-shaped nodulei. Prominent horn-filled central depression
ii. Keratin with thick epidermis.
Treatment: Simple excision.
Sebaceous nevus of Jadassohn
1-Appears at birth2-After puberty, 10% to 15% degenerate into BCC.
May also develop SCC or keratoacanthoma.
3- Clinical presentation: Appears as yellow/orange, waxy, smooth plaques prior to puberty.
4- Appear as rough, verrucous, orange plaques after puberty.
5-Anatomic location: Most commonly found on scalp.
6- Treatment: Excision.
Sebaceous nevus of Jadassohn
PYOGENIC GRANULOMA
Pyogenic granulomas are vascular nodules composed of proliferating capillaries in a loose stroma.They often follow trauma with rapid growth and the tendency to bleed easily.
Most common on hands and around mouth.
Treatment : surgical excision.
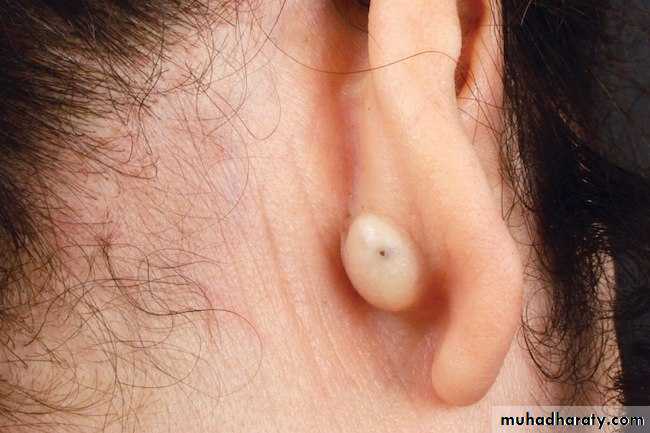
Cysts
1. Epidermal inclusion cyst (epidermoid cyst)#Occurs due to implantation of epidermis into the dermis.
#Appears in adulthood.
Clinical presentation: Fluctuant, flesh-colored, well-circumscribed nodules.
i. Punctum may be visible.
ii. Contains foul-smelling keratinous debris.
Treatment: Simple excision if uninfected; if infected, perform incision and drainage with interval excision.
Epidermal inclusion cyst (epidermoid cyst)
May be incorrectly called a sebaceous cyst; however, not sebaceous in origin.
Dermoid cystAppears at birth or early childhood.
Anatomic location: Most commonly found along supraorbital ridge, lateral brow,
or nasal midline(CT or MRI prior to excision to determine intracranial extension).
Treatment: Excision.
Dermoid cyst
SKIN MALIGNANCIES
Generally grouped into three types (listed from most common to least)a. Basal cell carcinoma (BCC)
b. Squamous cell carcinoma (SCC)
c. Melanoma
BASAL CELL CARCINOMA (BCC)
BCC is the most common skin cancer, accounting for ≈80% of all skin cancers.#Derived from the pluripotential cells of the epidermis or outer root sheath of the hair follicle.
Risk factors:
1- Sun exposure(especially repeated sunburn in childhood).
2- Advanced age
3-Immunosuppression, most commonly seen in transplant patients.
BCC (CONTINUED)
4-Fair complexion5-Nevus sebaceus of Jadassohn
6-Arsenic exposure
7. Syndromes associated with BCC
a. Basal cell nevus syndrome (Gorlin’s syndrome)
i. Autosomal dominant inheritance
ii. Multiple nevi/lesions often seen early in childhood with malignant degeneration more likely by the age of puberty.
iii. Skin pits on palms and soles, jaw cysts (odontogenic keratocysts), rib abnormalities, mental retardation.
BCC (CONTINUED)
b. Xeroderma pigmentosum (XP): Patients have increased incidence of BCC, SCC, and malignant melanoma.
c. Albinism
Basal cell nevus syndrome (Gorlin’s syndrome)
SUBTYPES of BCC
1. Nodular BCC: a. The most common type, usually presenting as a single lesion consisting of pearly papules with telangiectasias, pruritus, and occasional bleeding.b. Lesion breakdown over time leads to nodulo-ulcerative BCC (“Rodent ulcer”).
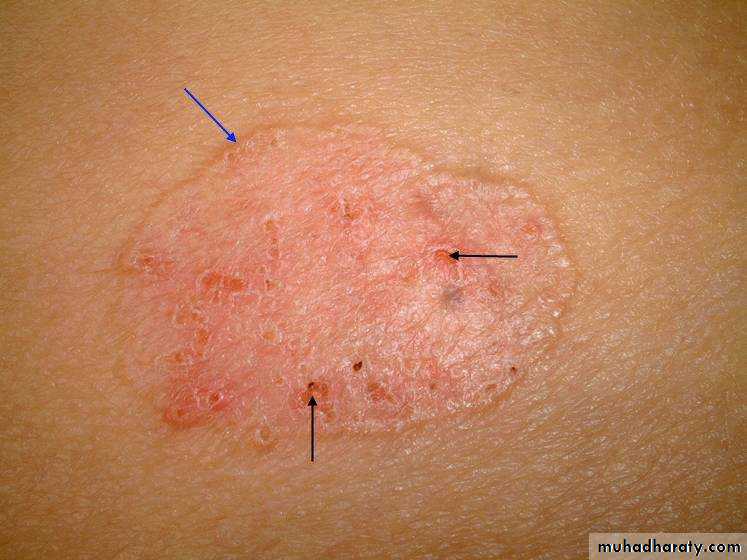
SUBTYPES of BCC
2. Superficial spreading BCCa. Slow-growing, erythematous, with minimal induration, and located primarily on the
trunk.
b. It is easily confused with other scaly, eczematous dermatoses.
SUBTYPES of BCC
3. Morpheaform (sclerosing, fibrosing) BCCa. Flat, often yellowish or hypopigmented, sometimes resembling scars or normal skin.
b. The true extent of the lesion is usually greater than the clinical appearance.
c. There is a high incidence of recurrence or incomplete excision due to “finger-like”
extensions.
3. Morpheaform (sclerosing, fibrosing) BCC
4. Pigmented BCC:
Similar to nodular BCC; easily confused with melanoma due to its deep pigmentation and nodularity.TREATMENT OF BCC
Wide local excision of BCC: 3- to 5-mm safe margins for nonaggressive types and 7-mm safe margins for morpheaform type.Curettage and electrodessication can be used for BCC <1 cm that is NOT a recurrent
disease or morpheaform type.
Cryotherapy is effective for small BCC
TREATMENT OF BCC
Imiquimod: Immune stimulant,only for superficial BCCs, with cure rates
between 80% and 90%. The 5% cream is applied 5 times per week for 6 weeks or longer.
Fluorouracil (5-FU): Chemotherapy,only superficial BCCs, with similar cure rates to imiquimod.
Radiotherapy in the older age group with a cure rate of 92%.
FOLLOW-UP
There is a 35% risk of developing another skin cancer in 3 years, 50% in 5 years. Recurrence may take up to 5 years.Patients treated for BCC should be observed every 6-12 months.
Cutaneous SCCSCC is second most common skin cancer after BCC. Occurs in sun-exposed regions.
Risk Factors:
1-Fitzpatrick skin type: Types I and II have increased risk
2-Sun exposure: Cumulative exposure strongly correlated to SCC
3- Carcinogen exposure: Pesticides, arsenic, organic hydrocarbons
4- Viral infection: HPV and herpes simplex
5- Radiation: Long-term latency between exposure and disease
6-Immunosuppression: like HIV patients
Risk Factors(Continued)
7-Marjolin’s ulcer: SCC arising in a chronic wound (i.e., chronic burn scars and pressure sores) secondary to genetic changes caused by chronic inflammation.
8- Premalignant lesions
A-Actinic keratoses:
Erythematous macules and
with coarse, adherent scale
Risk Factors(Continued)
B-Bowen’s disease: Erythematous plaque with sharp borders and slight scaling.#Erythroplasia of Queyrat is SCC in situ of the glans penis.
Risk Factors(Continued)
C. Leukoplakia:Presents as a white patch on oral
Or other mucosa.
D-Keratoacanthoma
Types of SCC
1. Verrucous SCC: Slow-growing, exophytic, and less likely to metastasize.2. Ulcerative SCC: Grows rapidly and is locally invasive with very aggressive growth characteristics.
3. Majorlin’s ulcer
a. Arise from chronic wounds (burn, pressure ulcer, fistula, osteomyelitis tracks)
b. Commonly metastasize to lymph nodes.
SCC TREATMENT
1. Wide local excision of SCC: 5- to 10-mm safe margins are usually sufficient.2-Curettage, electrodessication, and cryotherapy are used much less in SCC treatment than in BCC treatment, because of higher risk associated with missed deep tumor portions,and the risk of scarring obscuring SCC recurrences
3-Radiation is reserved for unresectable lesions or for the very elderly.
Follow-Up:
skin and nodal examinations every 3-6 months for 2 years, then every 6-12 months for 3 years, then yearly.
Example of SCC
Melanoma
Less than 3% of all skin cancers, but cause of 75% of skin cancer-related deaths.Risk Factors:
1- UV exposure:Australia, New Zealand
2-Prior melanoma
3- Family history of MM
4-Age
5-Fitzpatrick types I, II,Lighter hair color.
6-male gender
Risk factors(continued)
7- Xeroderma pigmentosum (XP)8-Precursor lesions:
a-Dysplastic nevus
b-Congenital nevus: 6% lifetime risk depending on size.
c-Melanoma in situ: Lesions have intraepidermal proliferation with fully developed cellular atypia.
d-Lentigo maligna
Classification of melanoma types
1. Superficial spreading melanomaa. Most common type, ≈70% cases
b-Usually arises from preexisting nevus
c-Long horizontal growth phase before vertical growth.
d-Irregular, asymmetric borders with color variegation.
Melanoma types
2. Nodular melanomaa-Second most common: 15% to 30% cases
b. Most aggressive type
c. Typically do not arise from preexisting nevi
d-No clear association with sunlight exposure
e- Typically bluish-black, with uniform, smooth borders
f-5% are amelanotic
Vertical growth phase is
a hallmark feature;
no radial growth.
Melanoma types
3. Lentigo maligna melanoma (LMM)a-Least aggressive type
b- Most clearly associated with sunlight/UV exposure
c. Head, neck, and arms of elderly (sun-exposed areas) typically affected
d-Usually greater than 3 cm in diameter; irregular, asymmetric with color variegation.
Lentigo maligna melanoma
Acral lentiginous melanoma
a-2% to 8% of melanomas in Caucasians, 35% to 60% of melanomas in African-Americans, Hispanics, and Asians.b. Presents in palms, soles, and beneath nail plate (subungual).
c- Long radial growth phase.
Diagnosis
Common clinical features of melanoma lesions: (ABCDE)1. Asymmetry
2. Border irregularity
3. Color variation
4. Diameter >6 mm
5. Enlarging/evolving lesion
Diagnosis
Excisional biopsy is preferred for lesions <1.5 cm in diameter. If possible, excise lesionwith 1- to 2-mm margins.
Breslow thickness is reported in millimeters; thus, it is more accurate and reproducible
than Clark level (level of invasion) and is a better prognostic indicator.
MELANOMA TREATMENT
#Wide local excision is the treatment of choice.#safe margin depends on tumor thickness.# Subungual melanoma requires amputation proximal to the DIPJ for fingers and proximal
to IP joint for the thumb.
#Management of regional lymph nodes
#follow up