Pleural Disease
Dr. Ziad T. MahmoodCollege of Medicine
University of Mosul
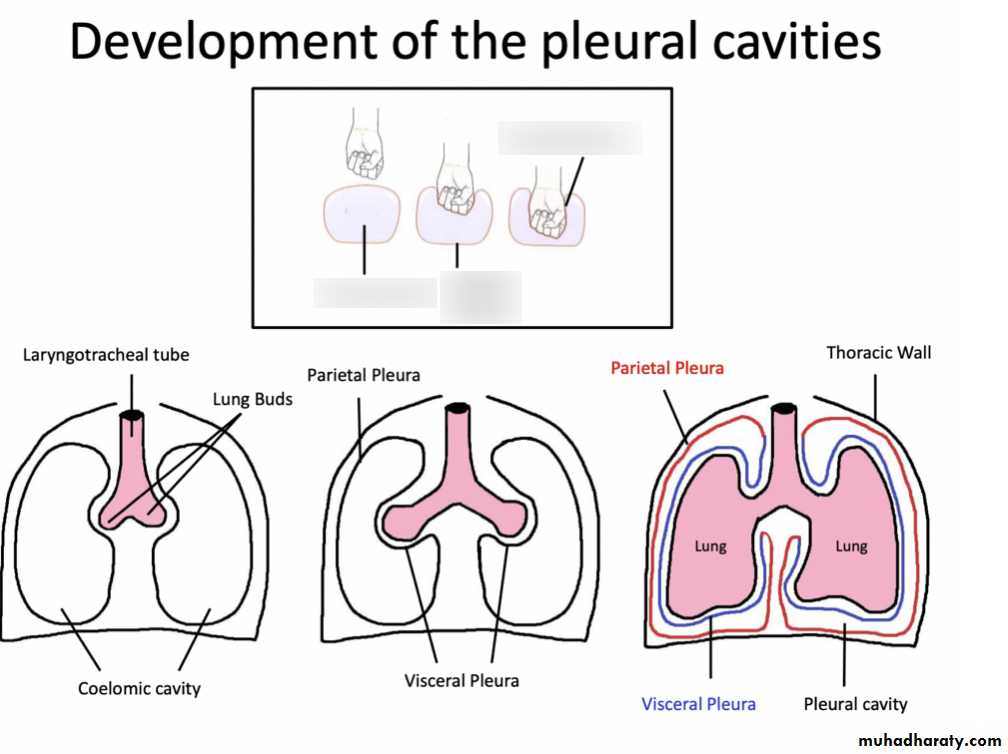
Introduction
What is the pleura??What is the pleural space??
What does the pleura do??Pneumothorax
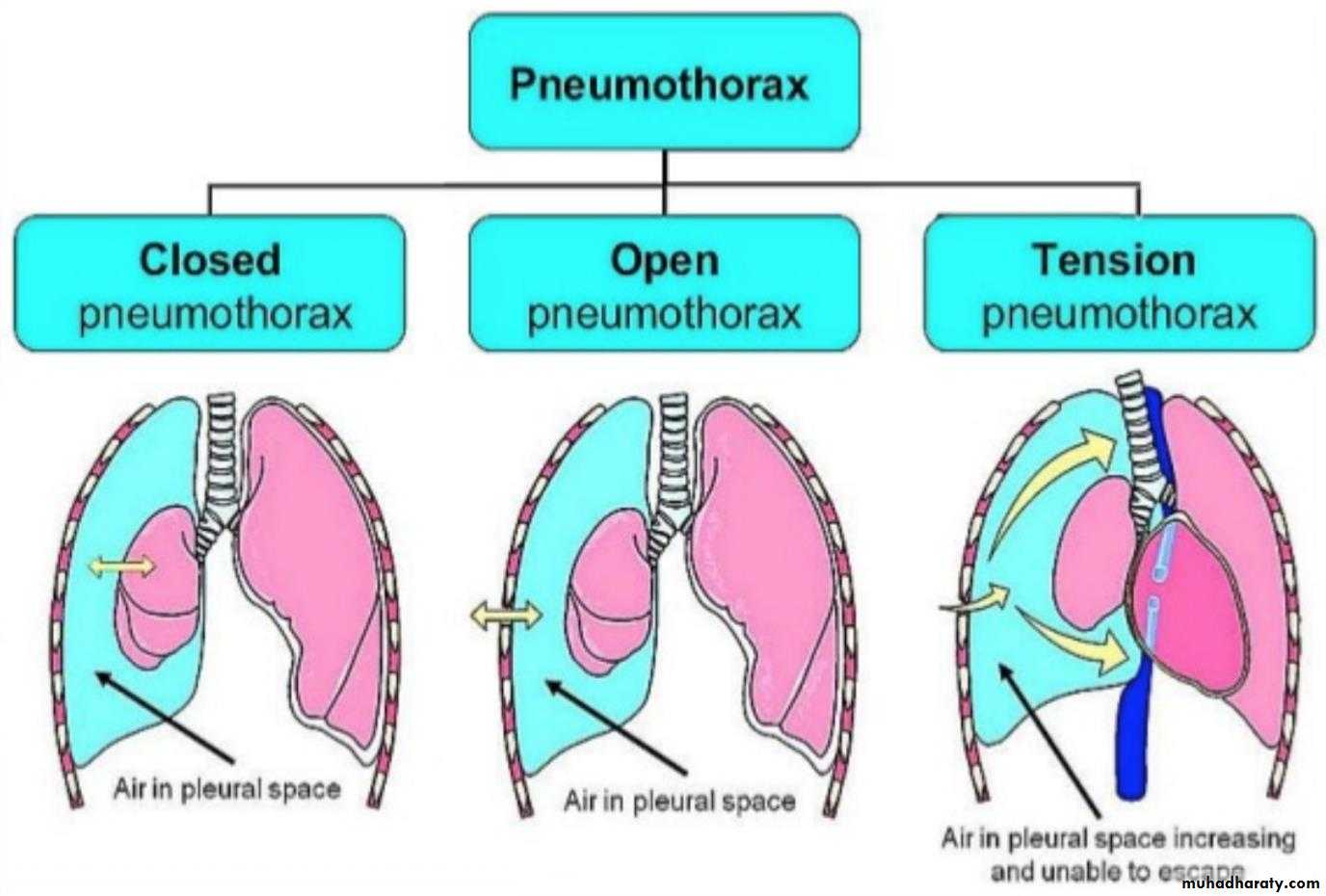
Classification• Spontaneous
• PSP
• SSP
• Acquired
• Blunt trauma
• Penetrating trauma
• Barotrauma
• Iatragenic injury
Pathophysiology
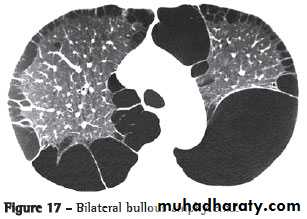
Alveoli ruptureAir in the interstitium
Air dissects superiorly
Sub-pleural bleb or bullae
Rupture to the pleura
Pneumothorax
• Primary Spontaneous Pneumothorax (PSP)
• Young men (teens – mid 20s)• Tall and thin
• Families
• Smokers
• Secondary Spontaneous Pneumothorax (SSP)
• Older people (45 – 64 years)
• Pre-existing lung disease
• Higher incidence of respiratory failure
• Higher mortality rate
Recurrence:
1st attack : 33% risk of recurrence2nd attack : 50% risk of recurrence
More than 2 attacks : 100% risk of recurrence
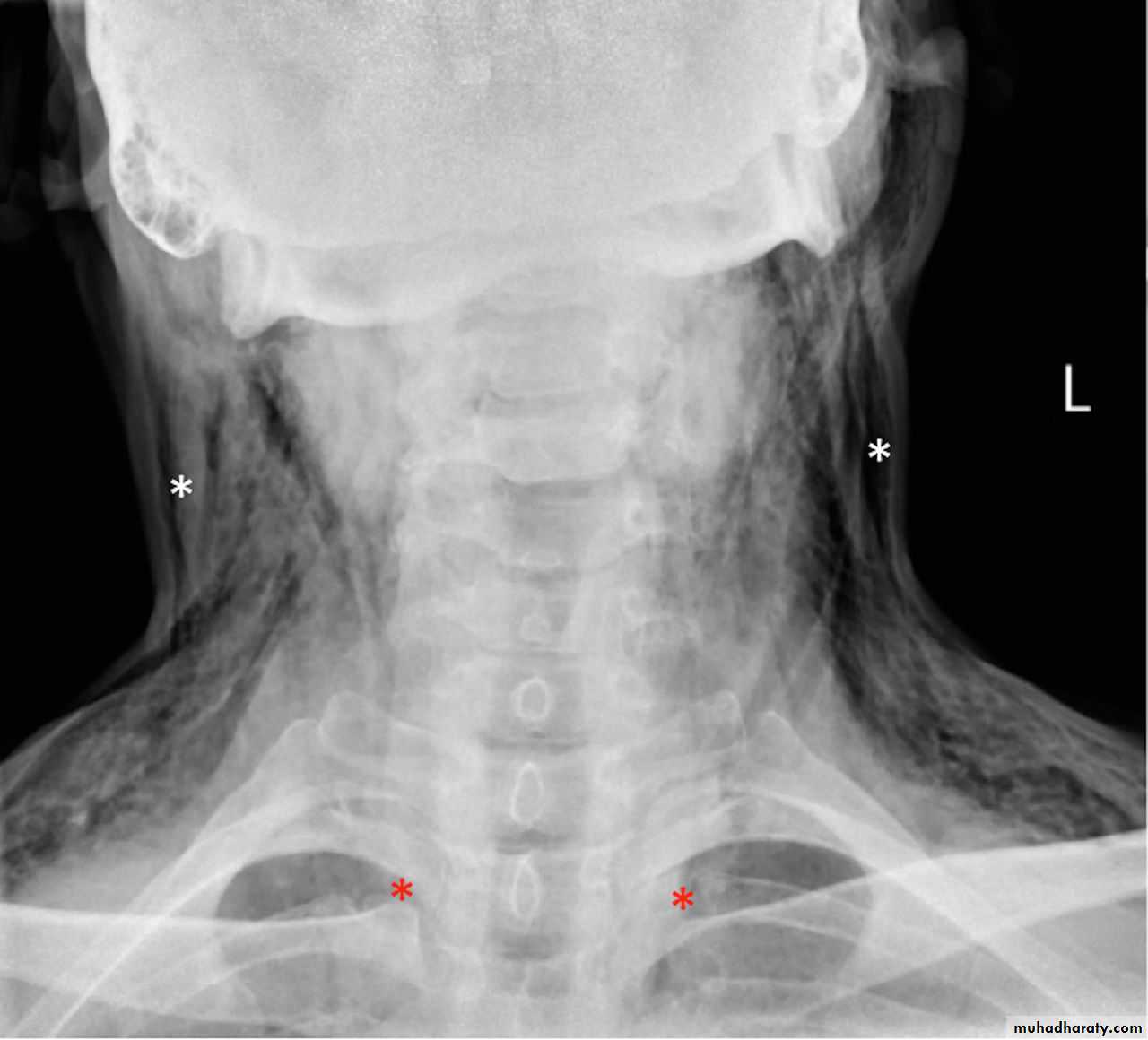
What is a surgical or subcutaneous emphysema?
Surgical emphysema
Surgical emphysema
Clinical presentationAsymptomatic
Symptomatic:
Chest painDyspnea
Orthopnea, cough and hemoptysis
On examination
Inspection: Dyspnea ± cyanosis ?• Decrease or absence chest wall movement
Palpation: Apex shifted to the other side
• Trachea shifted to the other side
• Decreased chest wall expansion
• Decreased or absent tactile vocal fremitus
Percussion: Hyper-resonance (tympanic)
Auscultation: Decrease or absent breath sounds
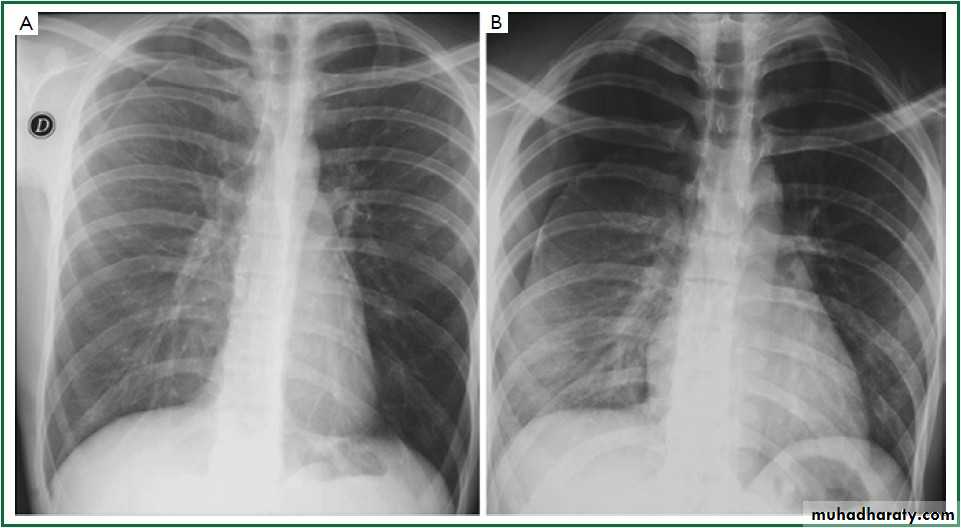
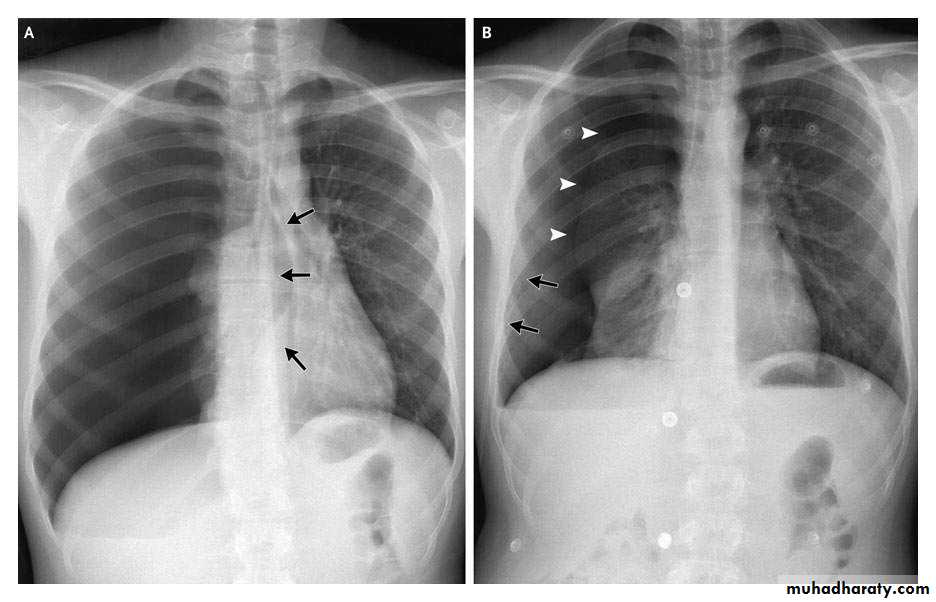
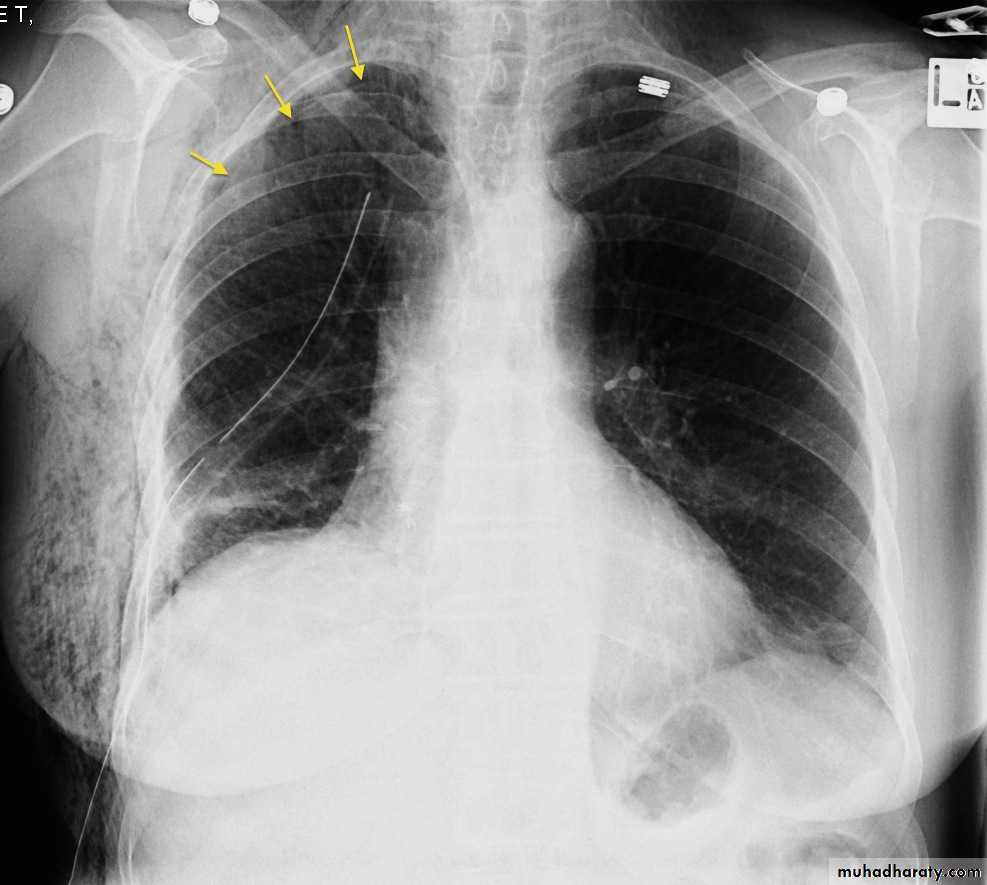
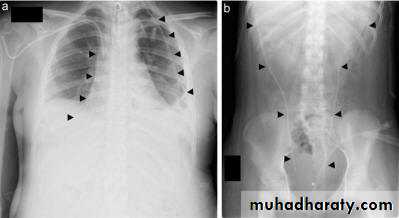
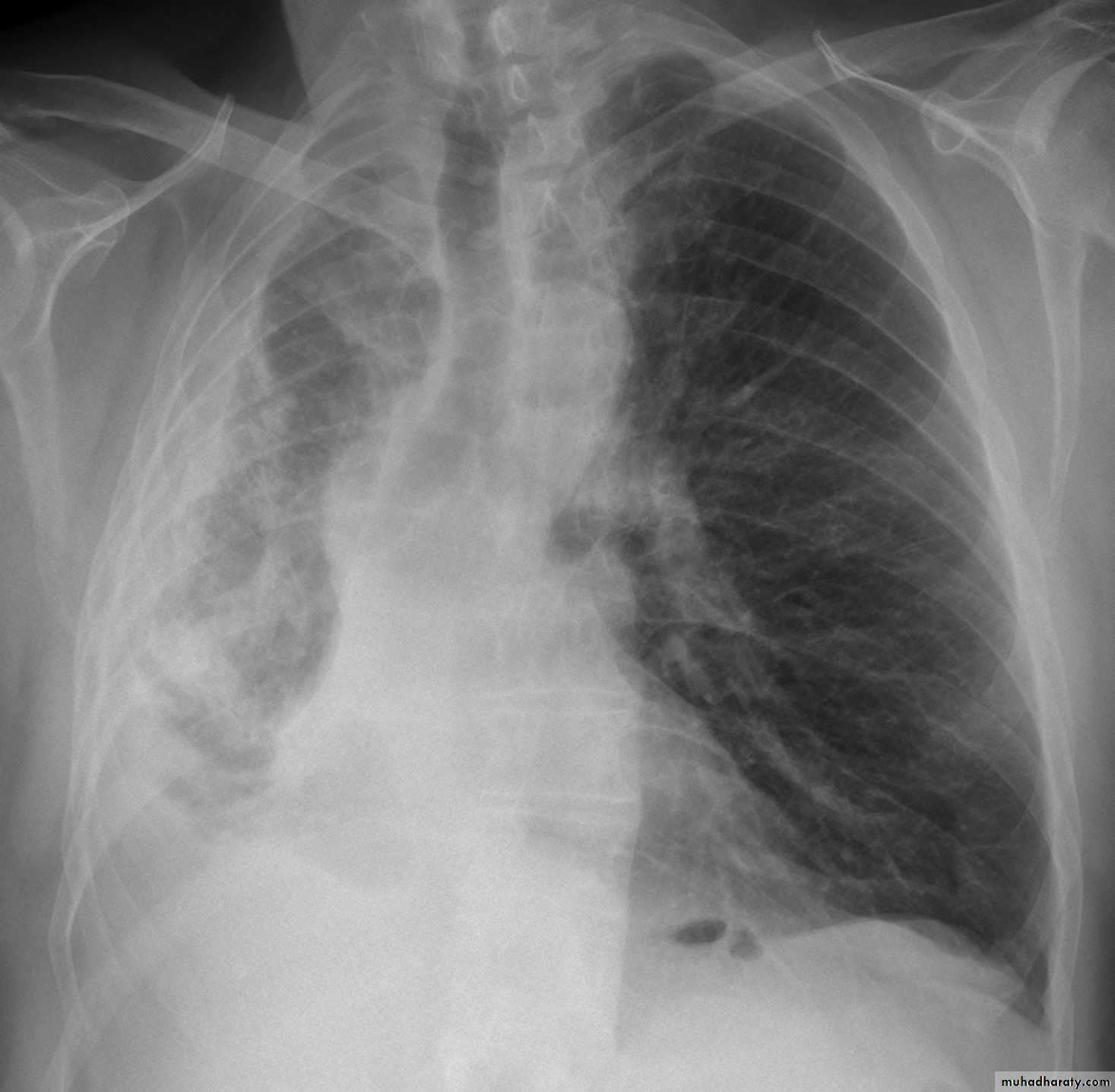
CXR:
Tension Pnenmothorax
What is the difference??Surgical Emphysema
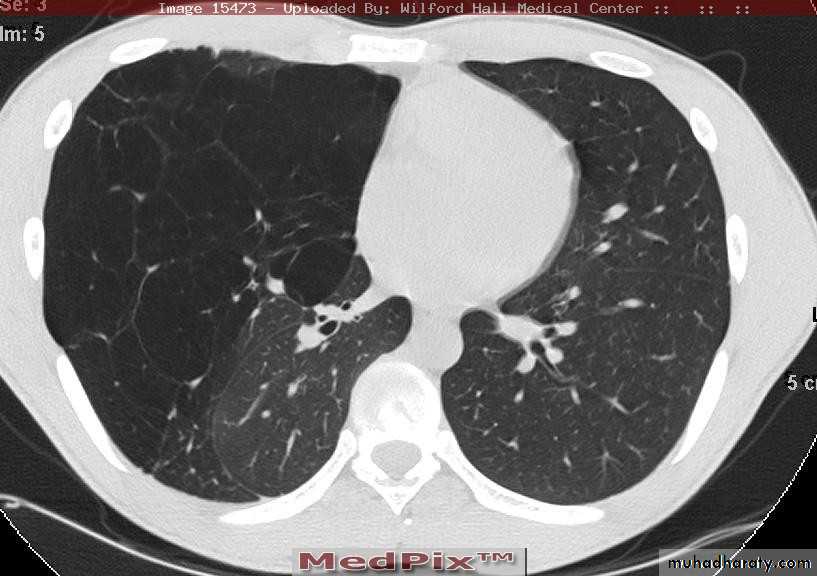
CT scan
BronchoscopyPneumothorax
Emphysema
Complications
• Pleural effusion• Hemothorax due to torn pleural adhesions
• Empyema
• Trapped lung (fibrothorax) due to failure of re-expansion
• Tension pneumothorax
Treatment
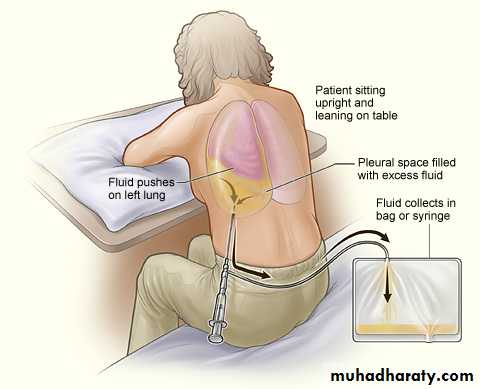
• Observation• Pleurocenthesis
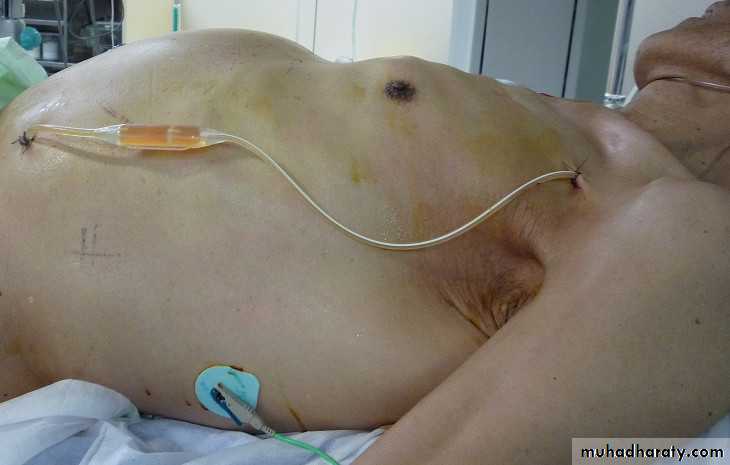
• Chest tube thoracostomy
• Surgery
• Massive air leak
• Persistent air leak
• Recurrent pneumothorax
• Bilateral pneumothorax
• Previous pneumonectomy
• Occupational hazard
• Pleurodesis
asymptomatic
small pneumothorax
1st 24h in hospital
Malignant Pleural effusion
Treatment of pleural effusion due to whatever cause?Treat underlying cause
Drainage if symptomatic
Causes of malignant pleural effusion?
• Lung cancer• Pleural malignancy
• Mediastinal LN malignancy
Treatment of pleural effusion → physician or oncologist
• When to reffer to a surgeon → recurrent &/or a suspicion of being a malignant effusionWhy reffer →biopsy + prevent reccurence of effusion
Biopsy:• Cytology of pleural effusion
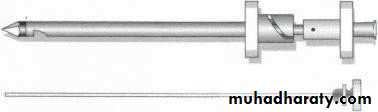
• Abram's needle of fine needle
• CT or U/S guided needle biopsy
• VATS biopsy
• Open biopsy
Prevent recurrence
• Repeated thoracocenthesis
• Chemical pleurodesis
• Surgical pleurodesis/pleurectomy
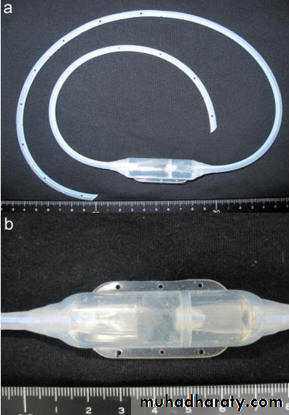
• Pleuro-peritoneal shunt (Denver's shunt)
Pleuro-peritoneal shunt
Empyema
Causes:• Complication of pulmonary infection
• Following chest trauma
• Extrapulmonary spread
• Complication of pneumothorax
• Non sterile aspiration of pleural fluid
Pathogenesis
1. Acute or exudative phase
Thin pus, Thin pleura, Expandable lungs
Antibiotics and drainage (needle)
2. Transitional or fibrinopurulent phase
Pus thicker, fibrin deposition, lung less expandable
Antibiotics and drainage (chest tube)
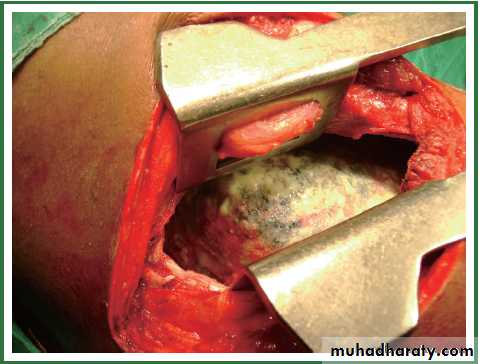
3. Chronic or organization phase
Thick pus, thick pleura with fibrous coat, non expandable lungs (fibrothorax)
Surgery (decortication)
Clinical presentation
• Fever, maliase, anorexia, weight loss• Pleuretic chest pain
• Dyspnea, cough, purulent sputum
O/E: Signs of infection: fever, fatigue, anemia, ….etc.
• Signs of pleural effusion:
• Inspection: Dyspnea ± cyanosis ?
• Decrease or absence chest wall movement
• Palpation: Apex shifted to the other side
• Trachea shifted to the other side
• Decreased chest wall expansion
• Decreased or absent tactile vocal fremitus
• Percussion: Dullness over the area of empyema
• Auscultation: Decrease or absent breath sounds
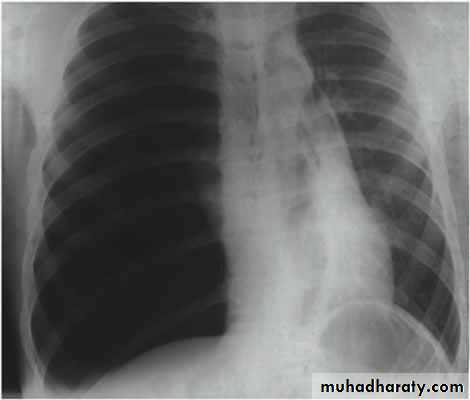
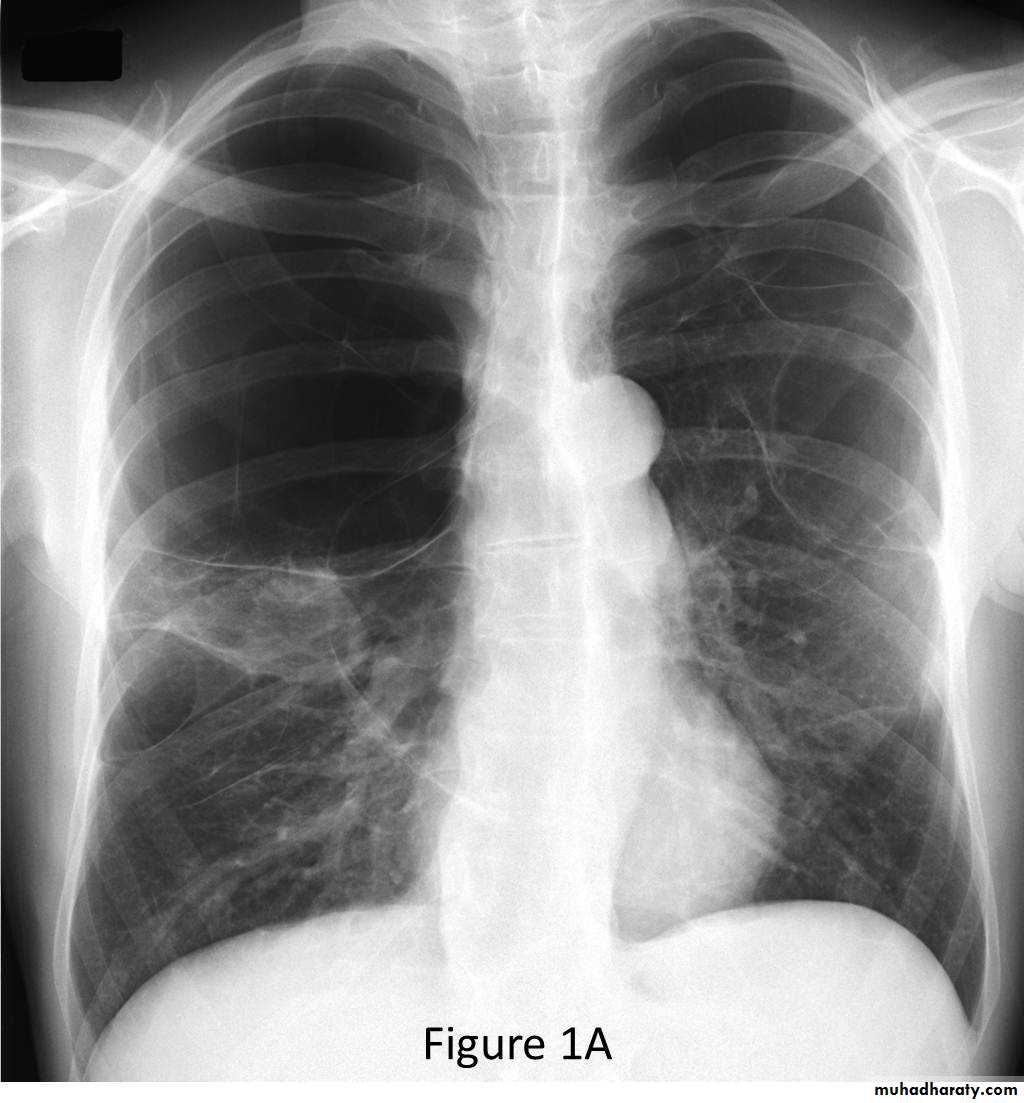
CXR:
Treatment
Objectives:• Control infection
• Drain purulent material
• Restore lung function
Exudative phase
Needle drainageTransitional or organization
Wide bore
Chest tube
Surgery
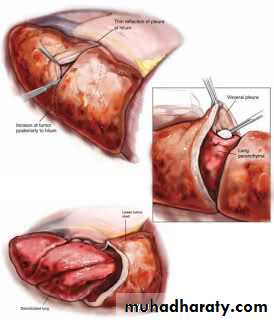
Decortication
pleurectomy
Open drainage
Decortication ± pleurectomy
Decortication
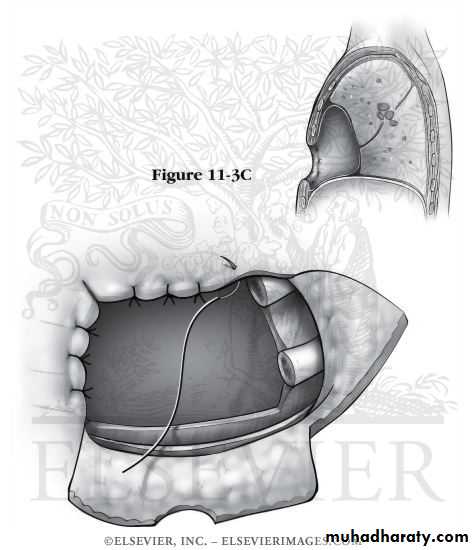
• Eloesser’s flap
ChylothoraxEtiology:
Disruption or tear in the thoracic duct during its coarse in the chest.
• Trauma including penetrating, blunt or iatrogenic injury
• Neoplasm with invasion of the thoracic duct• Infection
Clinical presentation:
• Dyspnea, orthopnea, and cough• Malnutrition why?
• Dehydration why?
• Decreased immunity why?
Investigations:
• 1. Pleural fluid analysis: odorless milky white appearance with a creamy layer on standing.
• 2. Lymphangiography
Treatment
• Conservative treatment• Chest tube drainage
• Correct dehydration
• Correct electrolyte imbalance
• Nutritional support by TPN or fat free oral diet
2. Surgical repair or ligation of thoracic duct
3. Denver's shunt (pleuro-peritoneal shunt)Pleural malignancy
• Primary pleural tumors are rare• The most common primary tumor malignant mesothelioma (usually as a consequence of asbestos exposure).
• Poor prognosis. Why?
• Respiratory failure or symptoms of invasion of nearby organ.
• CXR: lung surrounded by thick irregular pleura with multiple nodules with extension to nearby structures.
• Curative treatment is surgery (extrapleural pneumonectomy).
• Both radiotherapy and chemotherapy are weakly effective.