
1
) ﻋﺪد اﻻوراق
10
(
ﻋﯿﻮن
3
/
11
/
2019
د. ﻋﺰام
Lec: 5
Cornea- I
Objectives:
1 To describe anatomical and physiological corneal concepts
in relevance to the clinical practice.
2 To define bacterial corneal ulcer, causes, presentation and
diagnosis.
3 To demonstrate procedure of corneal sampling.
4 To make algorithmic approach to deal with corneal ulcer.
5 Develop a plan of management of a corneal ulcer.
6 Analyze causes of non healing of corneal ulcer.
Anatomy and physiology:
The cornea consists of the following layers:
1 Epithelium: is stratified,
squamous, non-
keratinized.
2 Bowman layer: is the
acellular superficial layer
of the stroma.
3 The stroma: makes up 90%
of corneal
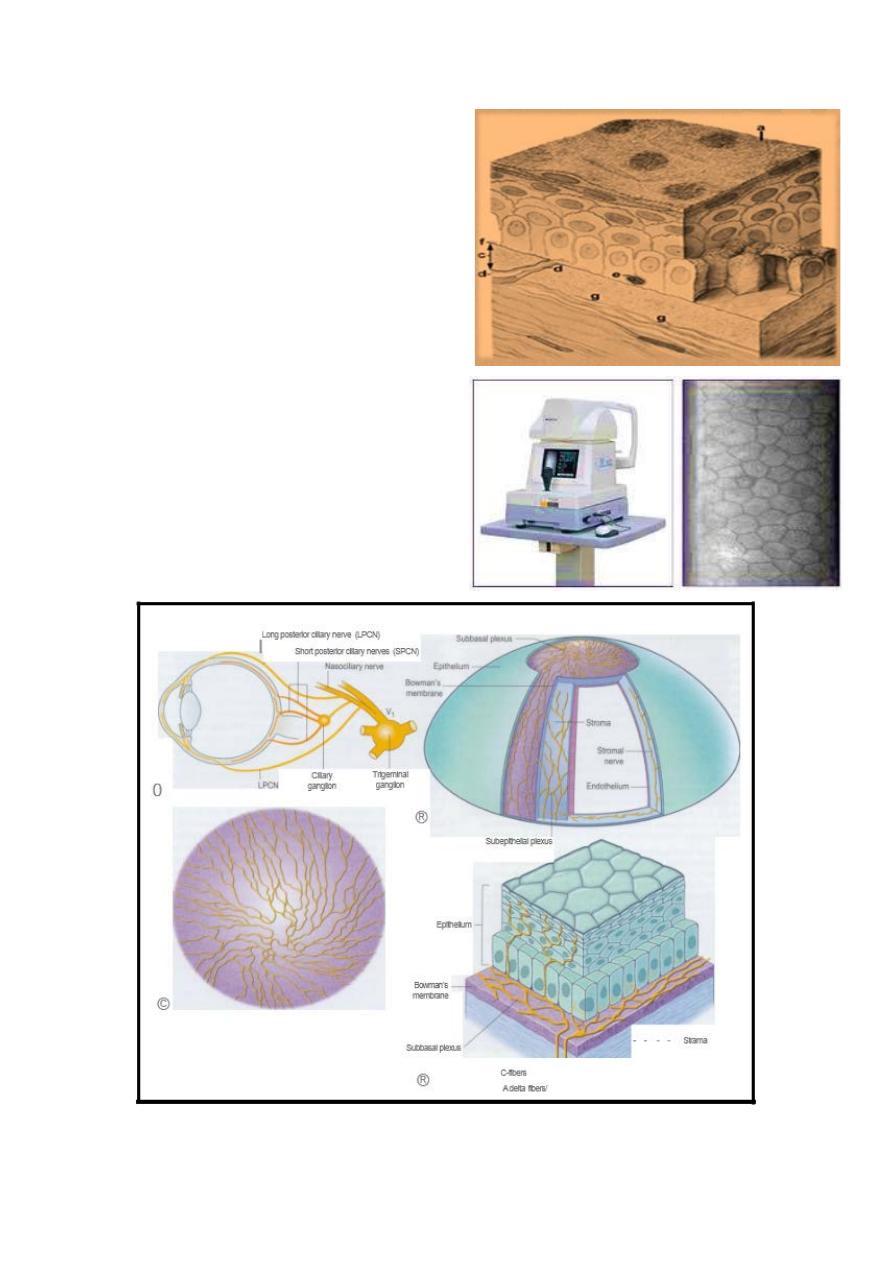
2
thickness.
4 Descemet‘s membrane : is
composed of a fine
latticework of collagen
fibrils.
5 The endothelium: consists
of single layer of
hexagonal cells that can not
regenerates. It plays a vital
role in maintaining corneal
deturgescence.
3
Why the cornea is transparent ?:
1 Regularly oriented and
arrenged collagen fibers.
2 Avascular tissue.
3 Unmylinated nerve fibers.
4 Non-keratinized epithelium.
5 Lack of pigments.
6 Role of the endothelium to
create a state of relative
corneal dehydration.
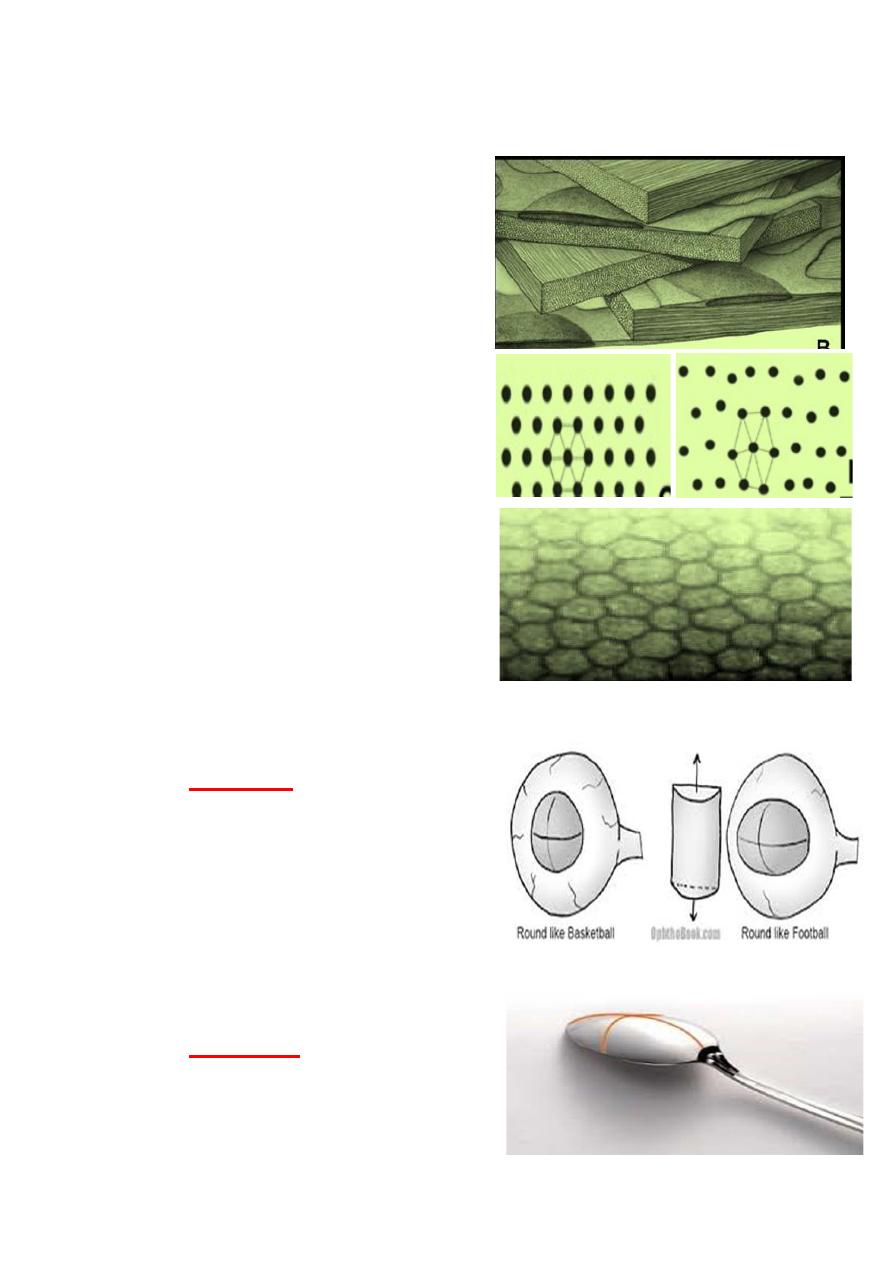
Cornea, Average measurement:
Diameter:
Vertical
1a1.5mm
horizontal 12.5mm
At birth :horizontal diam. 9.5-
10.5mm
reach adult size by age 2.
Thickness:
central
550 microns
peripheral 1.00 mm
4
The cornea is the main
refractive elements of the eye
accounting for about two-thirds
of the total refractive power (
which is about 43 Diopters),
the remaining one- third
(which is about 15 D) element
from the lens, thus the total
refractive power of the eye
equal to about 58 D.
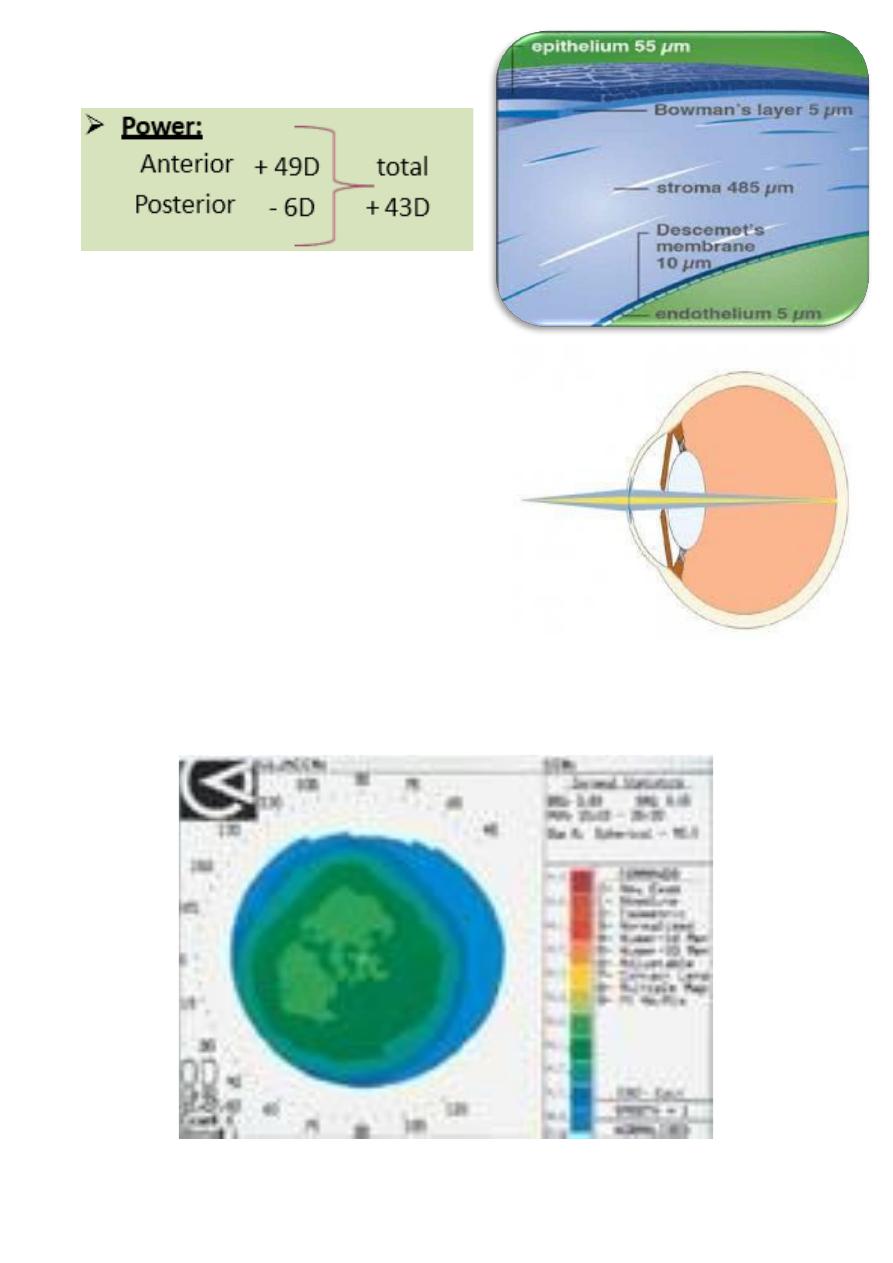
Corneal topography:

5
Fuchs’ dystrophy:
Corneal guttata appears in the central cornea bilaterally as dark
spots on endothelial surface. As the condition progress,
Descemet’s membrane/endothelium complex takes on beaten
metal appearance. Patient being warned that they are at
increased risk for corneal edema because of aging or ant trauma
to the corneal endothelial cells, such as from intraocular surgery
or inflammation. Symptomatic corneal edema develops in only a
small percentage of patients with endothelial dystrophy.
Histopathologically,
the endothelial cells lay down new
collagenous tissue over Descemet’s membrane, leading to
abnormally thickened Descemet's layer, usually this thickened
layer appear as discrete excrescences that protrude into the
anterior chamber (corneal guttata).The excrescences and the
thickened Descemet's membrane affect the over lying
endothelial cells and their function. They cause the cells to thin
and loose the hexagonal character.
Specular microscopy reveals small to large dark areas of ovoid
cells, demonstrating the guttata excrescence, and adjacent
endothelial cells. The cells being more varied in size
(polymegethism) and shape (polymorphism). Endothelial cell
density tend to decrease. The endothelial cells lose their Na-K
ATPase pump function.
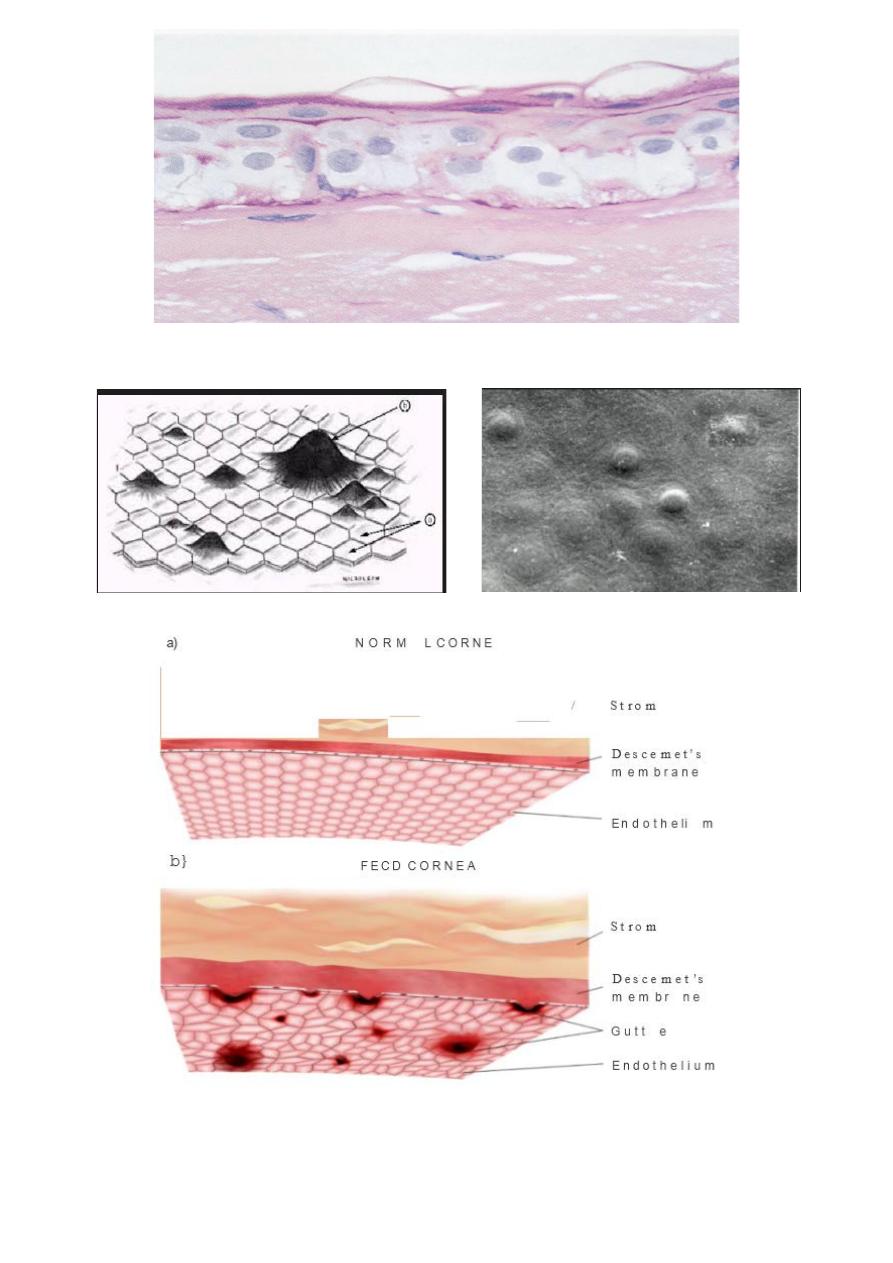
6
Croneal guttata:
7
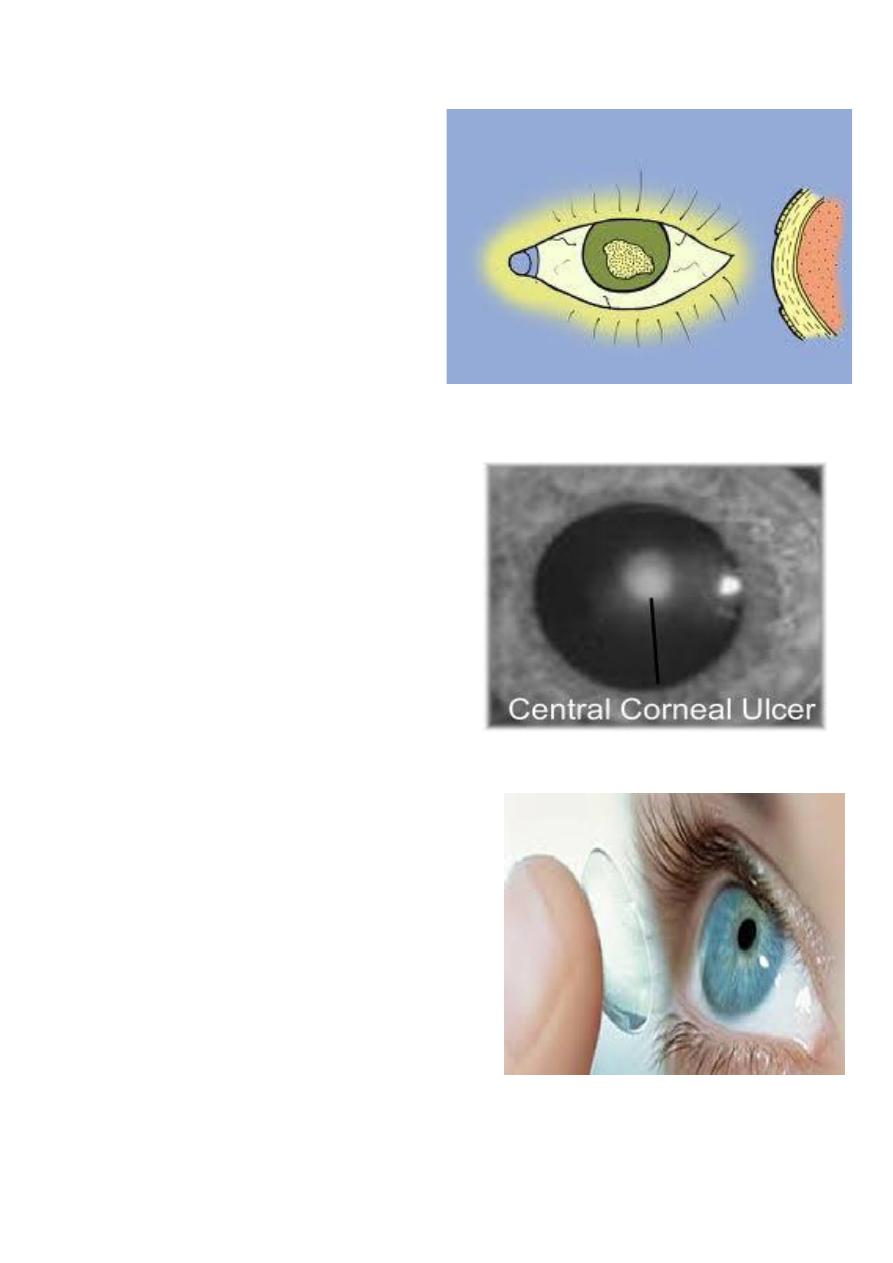
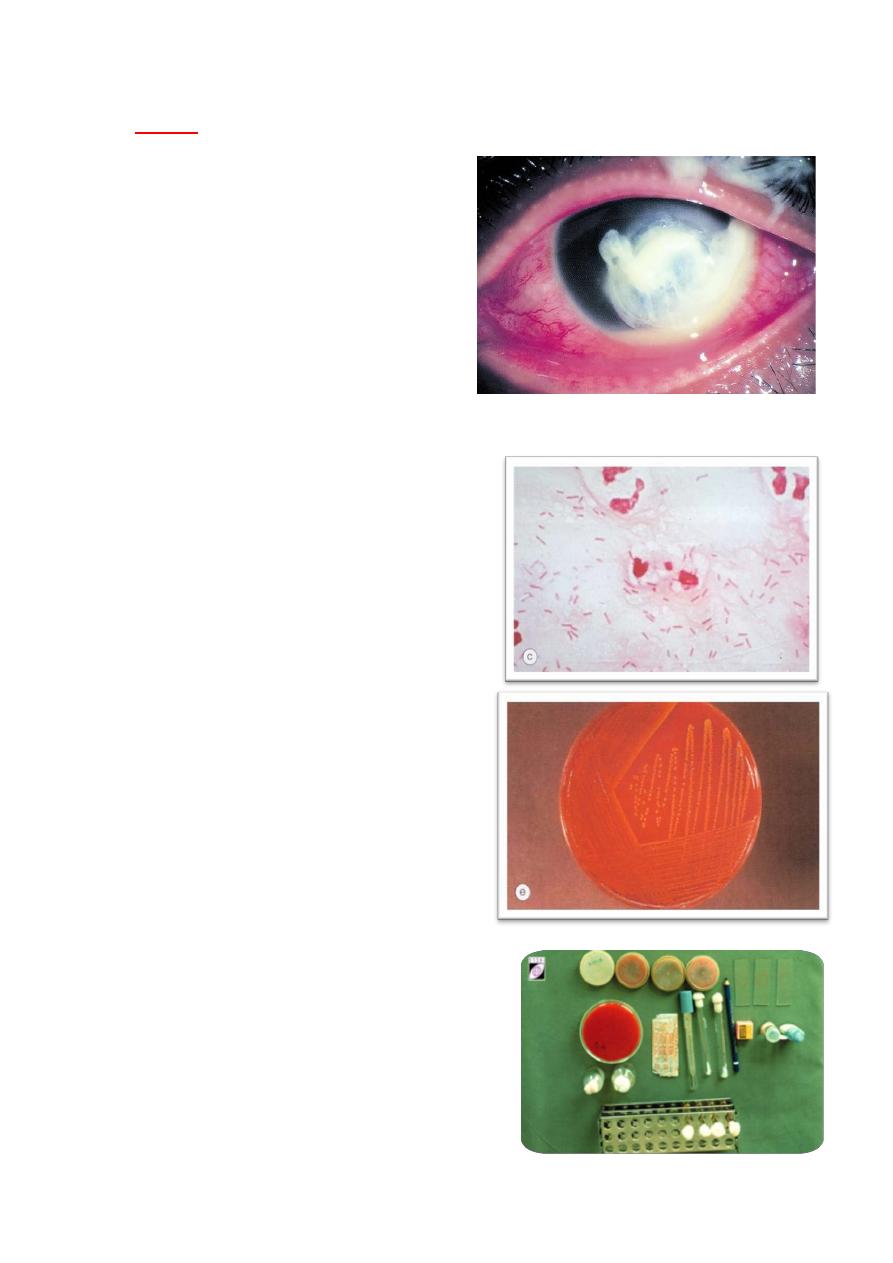
Corneal ulcer:
Bacterial keratitis is very
uncommon in normal
eye and usually only
develops when ocular
defenses have been
compromised,
considered as ocular
emergency.
• Prompt recognition and
initiation of appropriate
therapy are crucial to limit
tissue damage and improve
visual prognosis particularly
if the ulcer involve the
central cornea.
Facts:
• Epidemiologic studies have
estimated that the annual
incidence of cosmetic contact
– lens related ulcerative
keratitis at 0.21% For
individuals using extended-
wear soft contact lenses and
0.04%for patients using daily
–wear soft lenses.
• The risk of developing microbial keratitis increases
significantly (approximately 15 times) in patients who

8
wear their contact lenses overnight and is positively
correlated with number of consecutive day lenses are
worn without removal.
Risk factors:
1
contact lens wear:
particularly soft
contact lens worn overnight ,is the most
important risk factor for bacterial
keratitis.
Infection is more likely if there is poor
lens hygiene, bacteria may multiply in
the contact lens case.
2
Trauma:
such as accidental
injury, surgical(refractive
surgery) and loose sutures. In
developing countries agricultural
injury is the major risk factor for
developing corneal infection.
3
Ocular surface disease:
such as
Herpetic keratitis, Bullous
keratopathy, dry eye, chronic
blepharitis, Trichiasis, exposure,
sever allergic eye disease and
corneal anesthesia.
4
Other factors:
include topical
and systemic immunosuppression, diabetes, vitamin A
deficiency and measles.
9
Microbiology:
• Bacteria divided into two categories:
1 Bacteria that penetrate intact
epithelium.
2 Bacteria that penetrate through
epithelial defect.
Bacteria that penetrate through epithelial defect
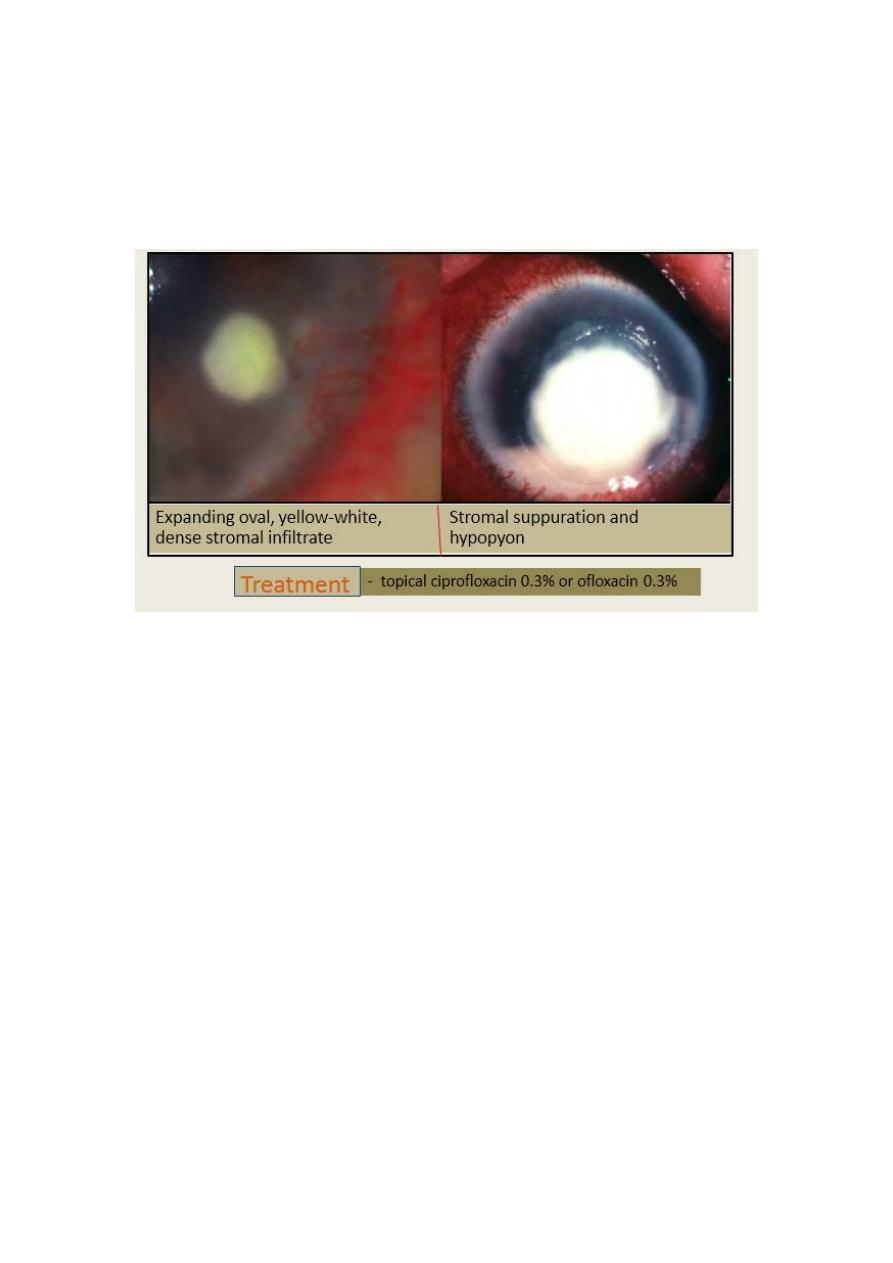
1-Pseudomonas aeruginosa:
Gram negative bacillus (rod ) that flourishes in soil, vegetation,
and moist situations in the hospital environment. Its also a
commensal of gastrointestinal tract .
2. Staphylococcus aureus
a common Gram positive and coagulase positive commensal of
nares, skin and conjunctive.
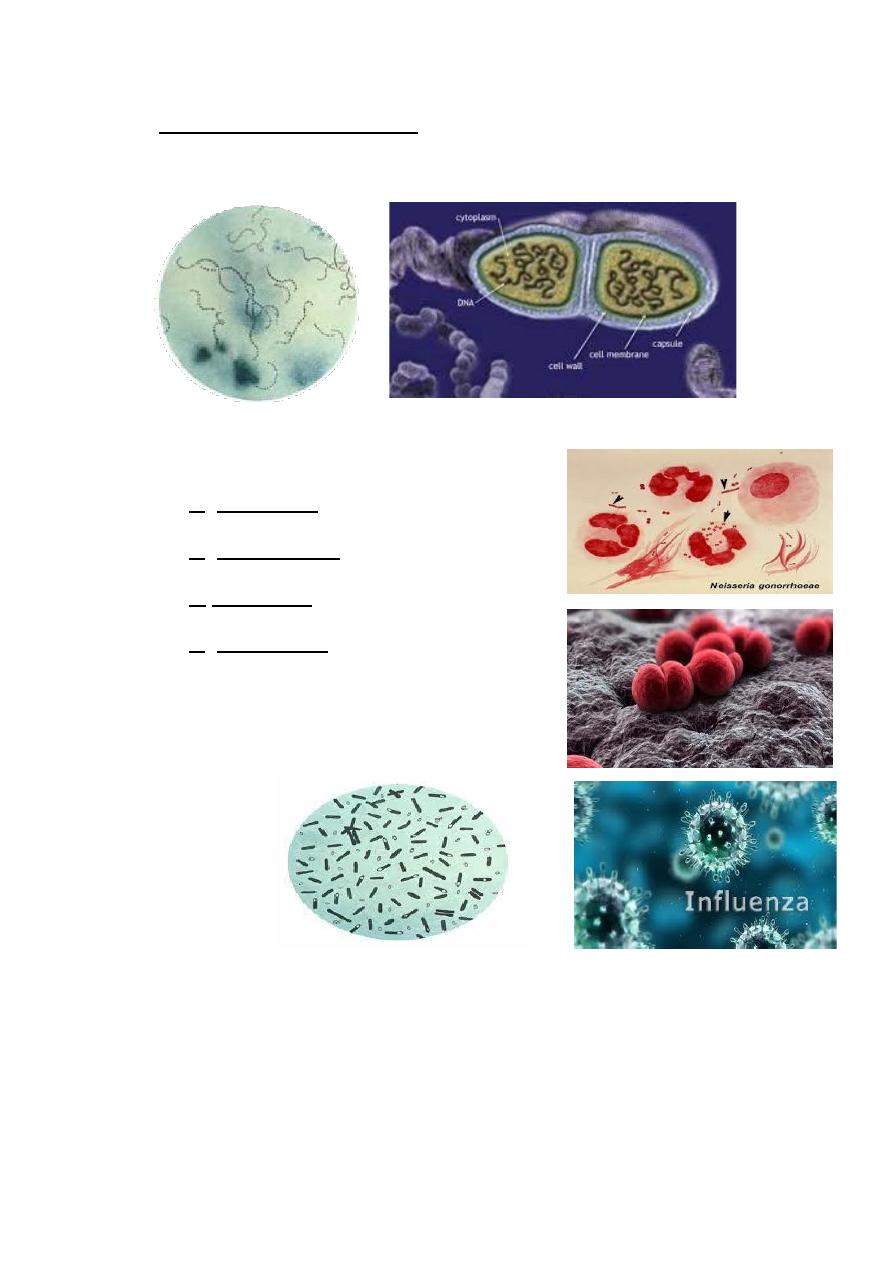
10
3. Streptococcus pneumonia Gram positive commensal of
upper respiratory tract, and infection with it is usually very
aggressive .
Bacteria that penetrate an apparently normal corneal
epithelium are:
1 N. gonorrhea
2 N. meningitides
3 H.influanzae
4 C. diphtheriae
11
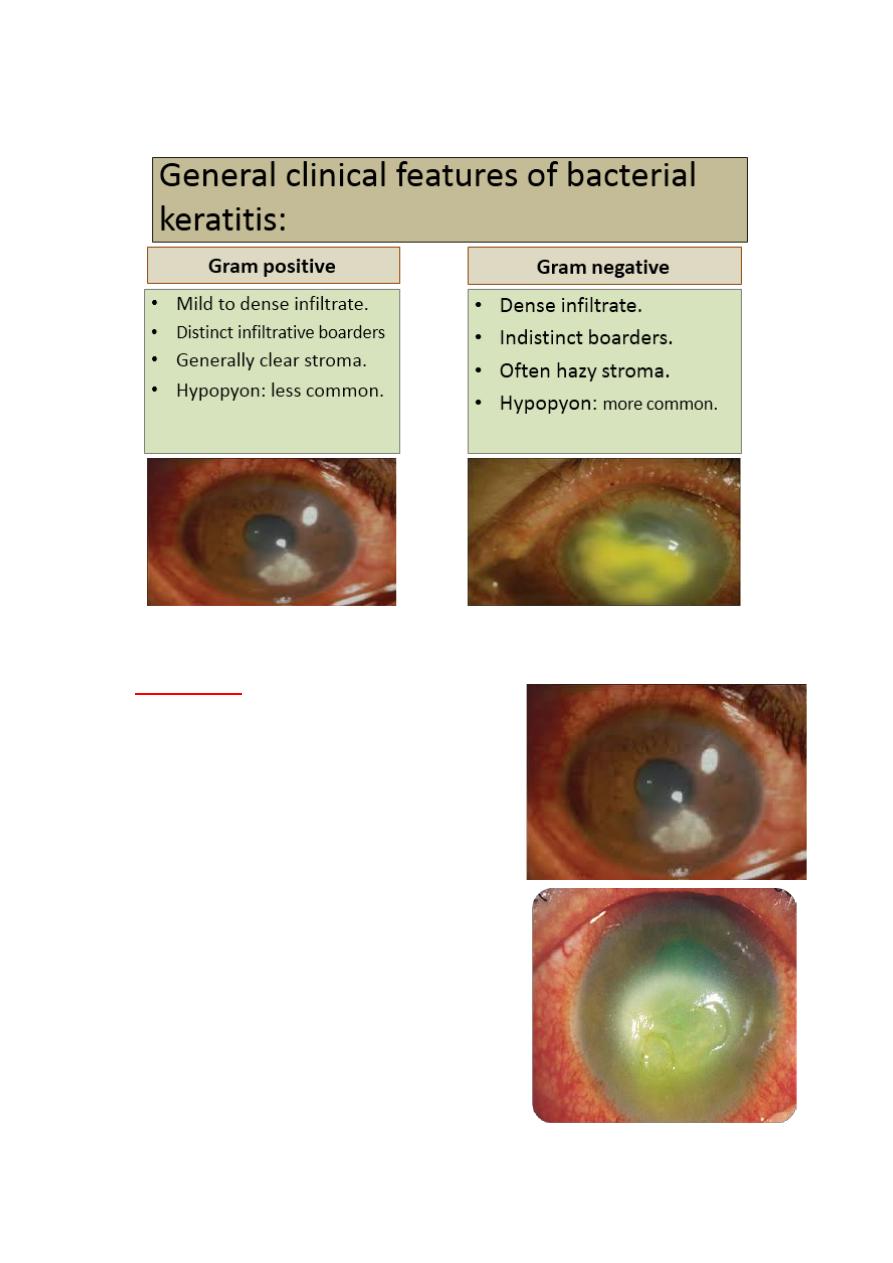
Clinical presentation:
Diagnosis:
• History: pay attention to risk
factors.
Presenting symptoms:
pain.
photophobia.
blurred vision.
discharge.
12
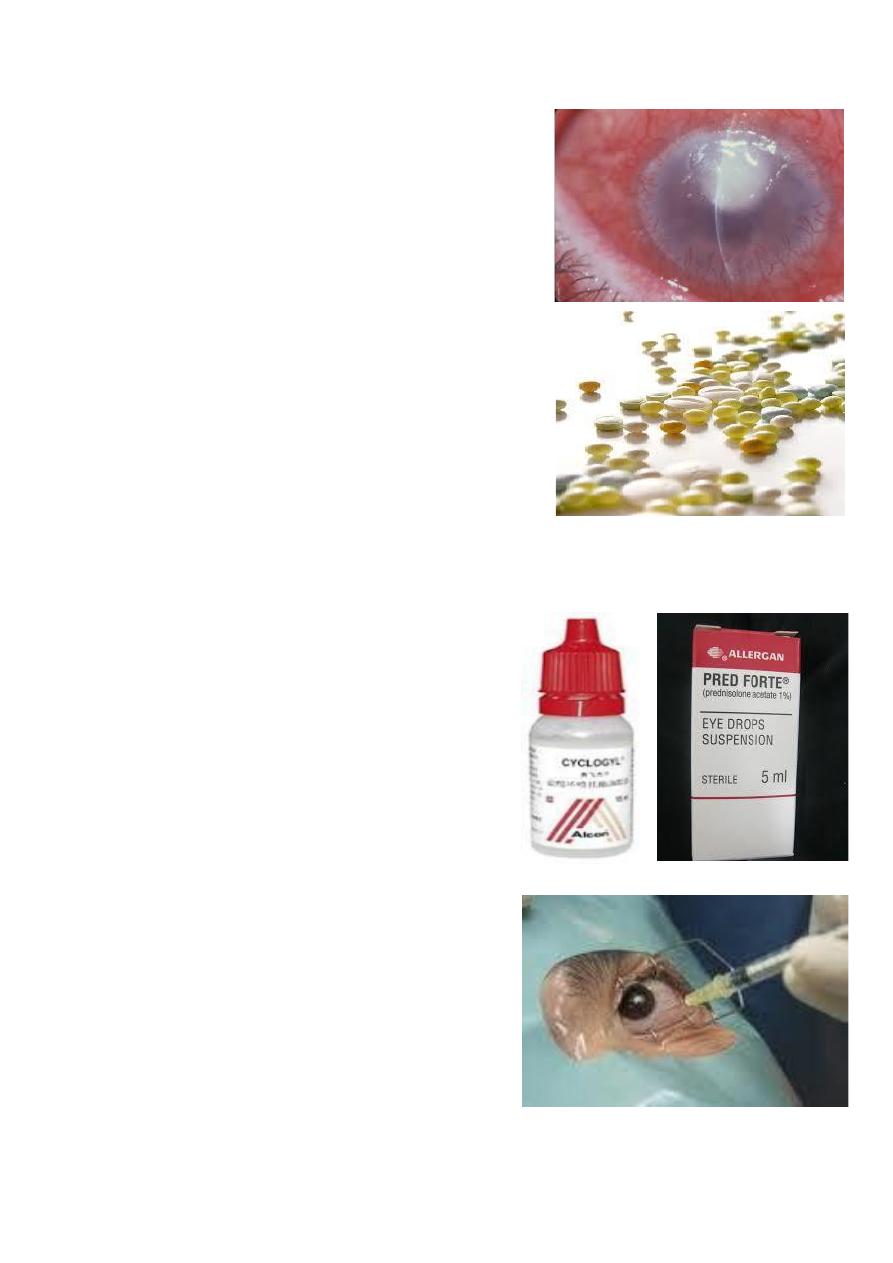
Signs:
❶Epithelial defect (pain).
❷ Enlarging infiltrate with
stromal edema and hypopyon.
❸Redness.
❹ Progressive ulceration may
lead to corneal perforation and
endophthalmitis (loss of function).
Work-up:
1 history and examination.
2 take cornea scraping.
3 Gram staining.
4 culture.
5 sensitivity report.
procedure:
1-Anaesthsthetize cornea with
0.5% propacaine.
2- obtain corneal scraping from
advancing ulcer boarders.
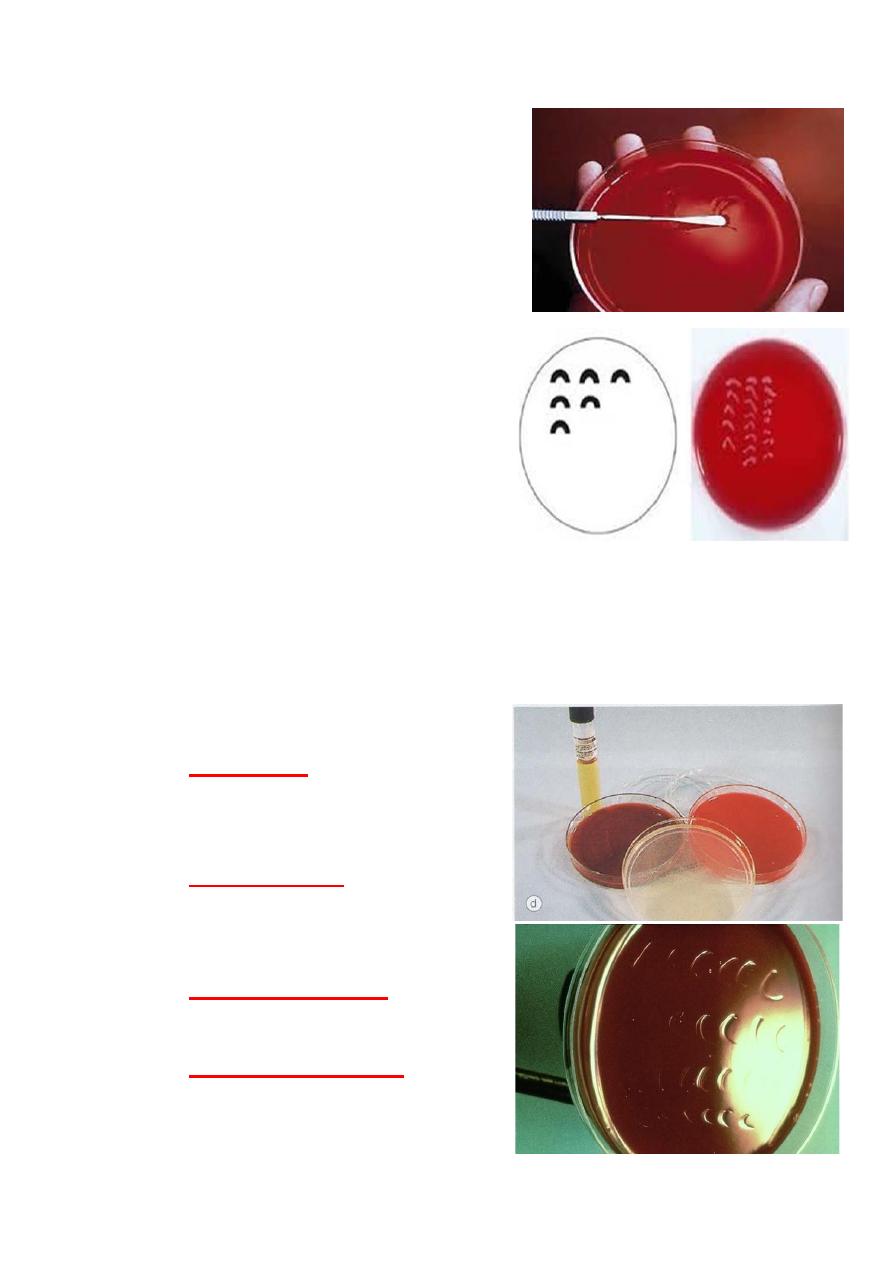
13
3- stain 2 slides with gram
and giemsa stains, reserve two
slides for special stain as needed.
4-Use flame sterilized kimura
spatula.
5- place the inoculum on
surface of media, in c-shaped
rows not penetrating the agar
surface.
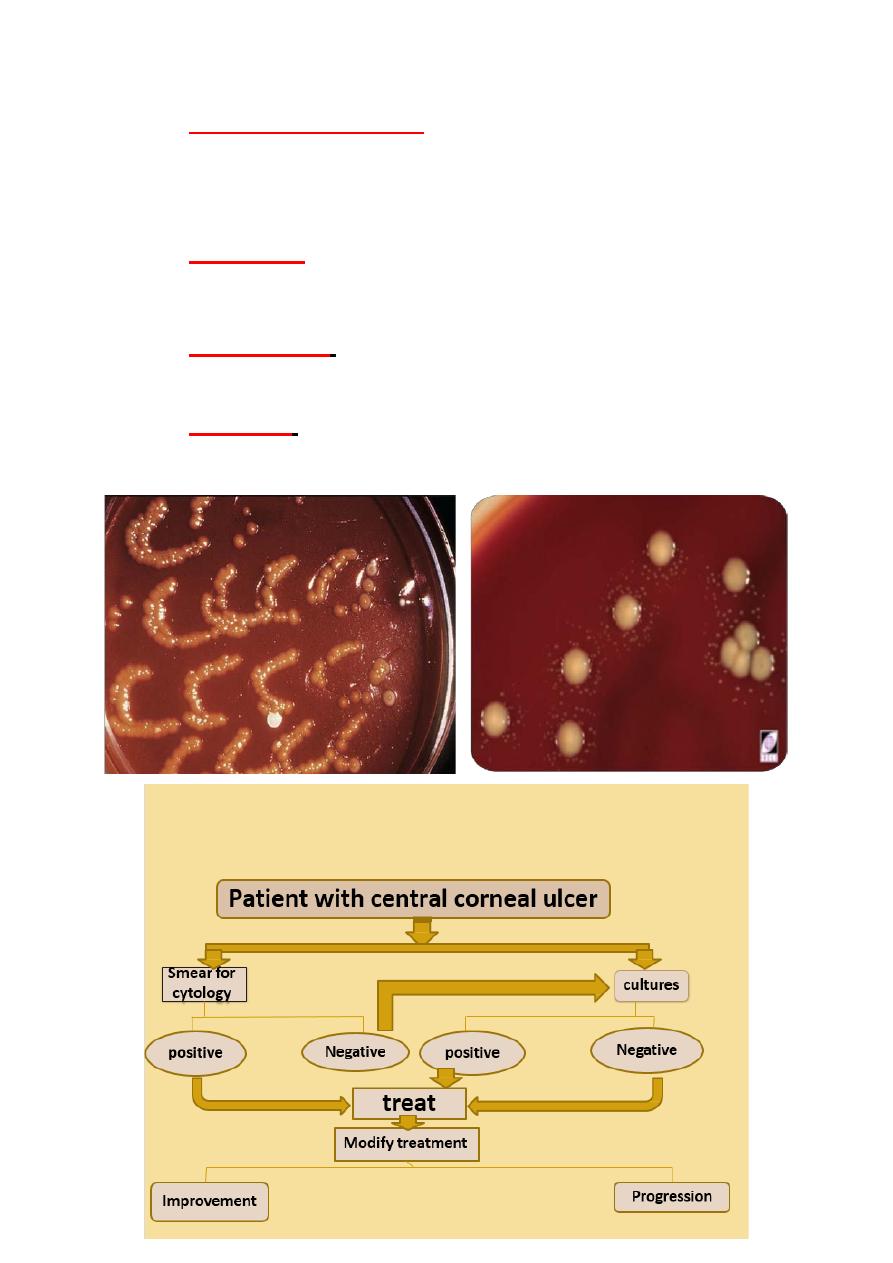
6- If smear and culture are
negative, consider
the possibilities of fungal, herpetic or non- infectious cause.
7- Judge improvement by daily slit-lamp examination and
corneal drawing, noting the size of the epithelial defect,
stromal infiltrates, anterior chamber reaction.
Cultures
Blood agar :
is suitable for
most bacteria and fungi except
Nisseria and Haemophilus.
Chocolate agar:
used to isolate
Nisseria, Haemophilus and
Maraxella spp.
Cooked meat broth:
for
anaerobics.
Brain-Heart infusion:
for most
aerobic bacteria and fungi.
14
Additional examination
should include Ziehl-Nielson
stain and Lowestain-Jensen media.
Sensitivity report:
Susceptible:
the organism is sensitive to normal dose of
antimicrobial agent.
Intermediate:
the organism is likely to be sensitive to
high dose of antimicrobial agent.
Resistant:
the organism not sensitive to the antimicrobial
agent at the tested dose.
15
Treatment and complications:
Bacterial keratitis has the potential to progress rapidly to
corneal perforation, even small axial lesion can cause
surface irregularity that can lead to significant visual loss.
Topical therapy can achieve high tissue concentration and
initially should involve broad spectrum antibiotics to
cover most common pathogens.
Out-lines:
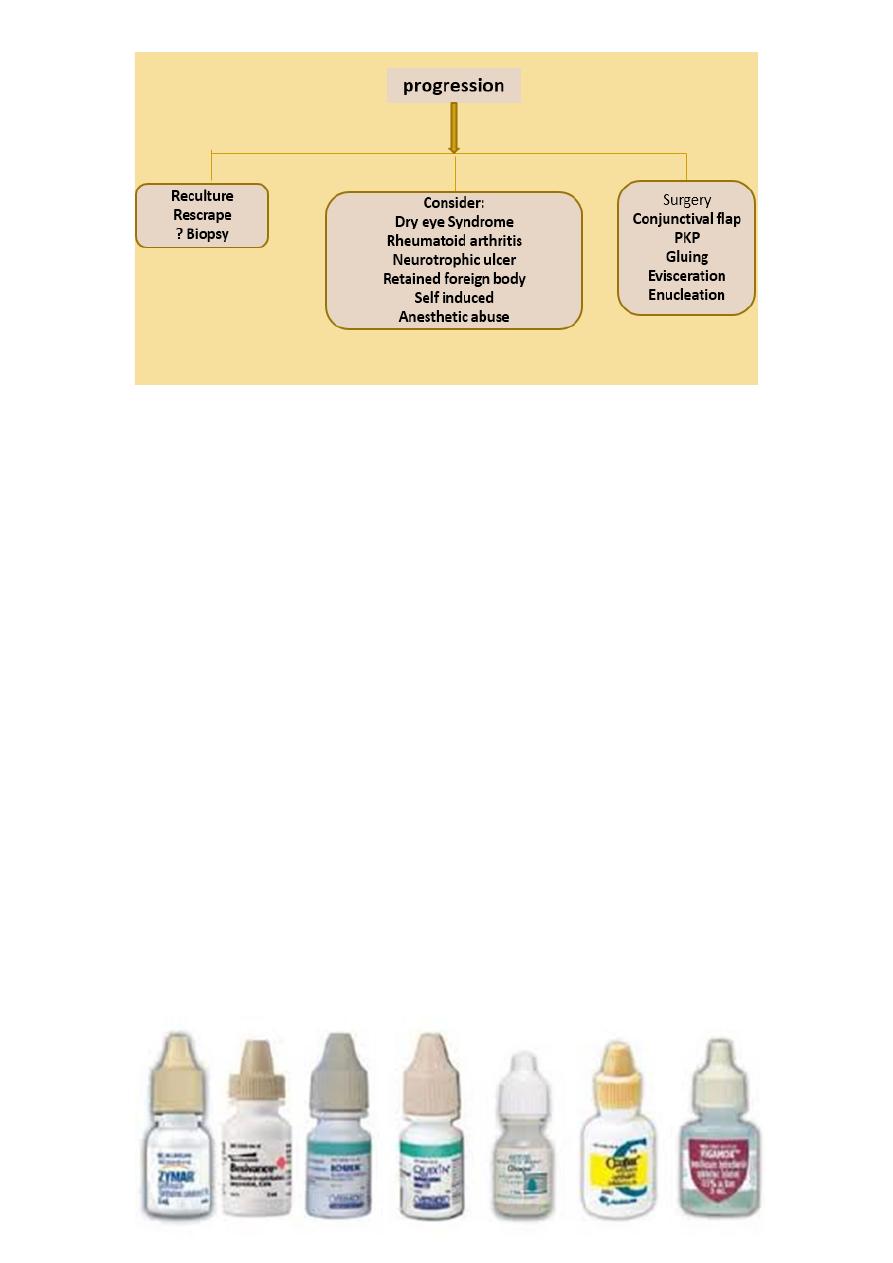
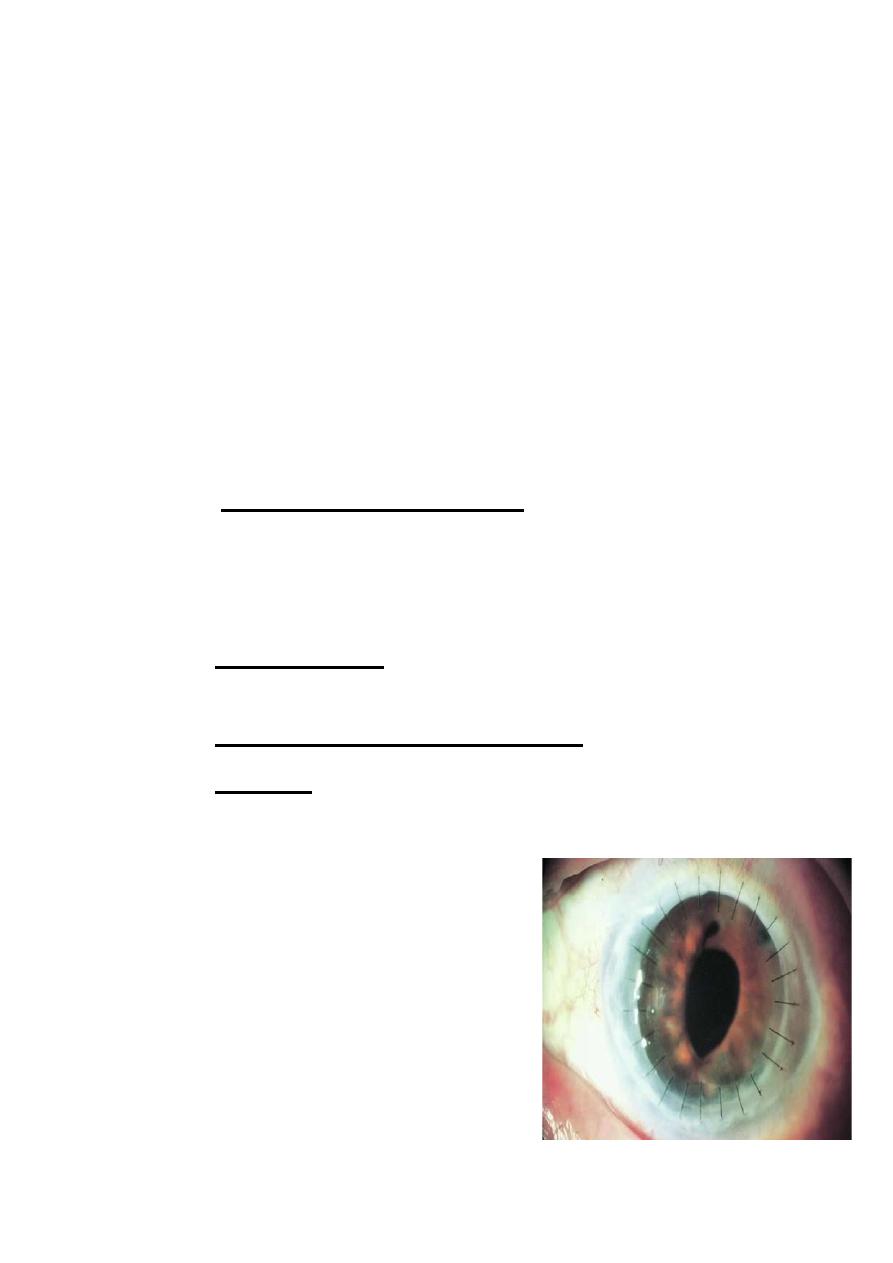
①Dual therapy vs. monotherapy vs systemic antibiotics.
②Topical corticosteroid.
③Cycloplegia.
Dual therapy:
Fortified topical antibiotics:
Therapeutic stromal concentrations may be achieved more
rapidly by initially administering the antibiotic drop every 5
minutes for 30 minutes as a loading dose.

16
• Fortified antibiotics should generally be
continued until substantial infection control, then after, a broad-
spectrum, non-fortified antibiotic may be given 3-8 times daily
according to patient´s clinical status.
• combination therapy
provide
good initial broad-
spectrum antibiotic coverage
→ Agent active against gram-
positive bacteria (e.g.
vancomycin, bacitracin,
cefuroxime).
→ Agent active against gram-
negative bacteria (e.g.
tobramycin, gentamycin,
ciprofloxacin).
Monotherapy:
•
Fluroquinolone monotherapy
is the
most appropriate in compliant
patients with less severe ulcers (e.g.>
3 mm in diameter, mid-peripheral,
and not associated with significant
thinning.
17
Oral antibiotics:
• Ciprofloxacin 750 mg twice daily
for 7-10 days indicated for:
❶ threatened or acute corneal
perforation.
❷peripheral ulceration in which
there is scleral extension.
❸ Isolates for which there are
potential systemic complication (N.
meningitides).
• Topical Cycloplegia.
•
Topical steroid
{ should be
avoided until improvement is
noted (usually after 48-72
hours) , then dosed at lower
frequency than topical
antibiotic}.
• Subconjunctivial antibiotics are
indicated only if there´s poor
compliance with topical
medications.
18
If no response to empiric therapy, consider:
1 antibiotic resistance (change regimen based on culture
results).
2 poor compliance (admit to hospital).
3 Anesthetic abuse.
Causes of failure:
Incorrect diagnosis.
Inappropriate choice of antibiotics.
Drug toxicity.
Complications:
1- Spread to adjacent structures: like sclera in
Pseudomonas, or to intraocular (which is rare in absence of
corneal perforation); filamentous fungi may penetrate intact
Descemet‘s membrane.
2- Corneal damage: scarring, neovascularization, corneal
edema, descematocele and perforation.
3- Synechiae and secondary glaucoma.
4- Cataract.
•
Penetrating keratoplasty (PK) is
indicated in:
❶progression despite therapy.
❷Descematocele formation.
❸Perforation.
Interrupted sutures are recommended.
19
Summery slide: Bacterial keratitis:
Predisposing factors: 1- Contact lens wear.
2- Chronic ocular surface disease. 3- Corneal hypoesthesia.
Summery:
Infectious keratitis can be caused by viruses, bacteria,
fungi and parasites.
In developed nations, herpes simplex virus is the most
common
causative organism.
Numerous bacteria have been reported like staph., Strep.
And Psudomonas.
Contact lens wear is the most common cause.
Prompt diagnosis is crucial to save vision.
Delayed treatment lead to tissue destruction and eventually
visual loss.
