1
) ﻋﺪد اﻻوراق
11
(
ﻋﯿﻮن
20
/
10
/
2019
د. ﻋﺰام
Lec: 3
1- To identify anatomy of the orbital structures.
2- To discuss causes of proptosis and recall its
examination techniques.
3- To Define enophthalmos and demonstrate
some examples.
4- To differentiate few cases of cystic lesion.
5- To report on some orbital tumours.
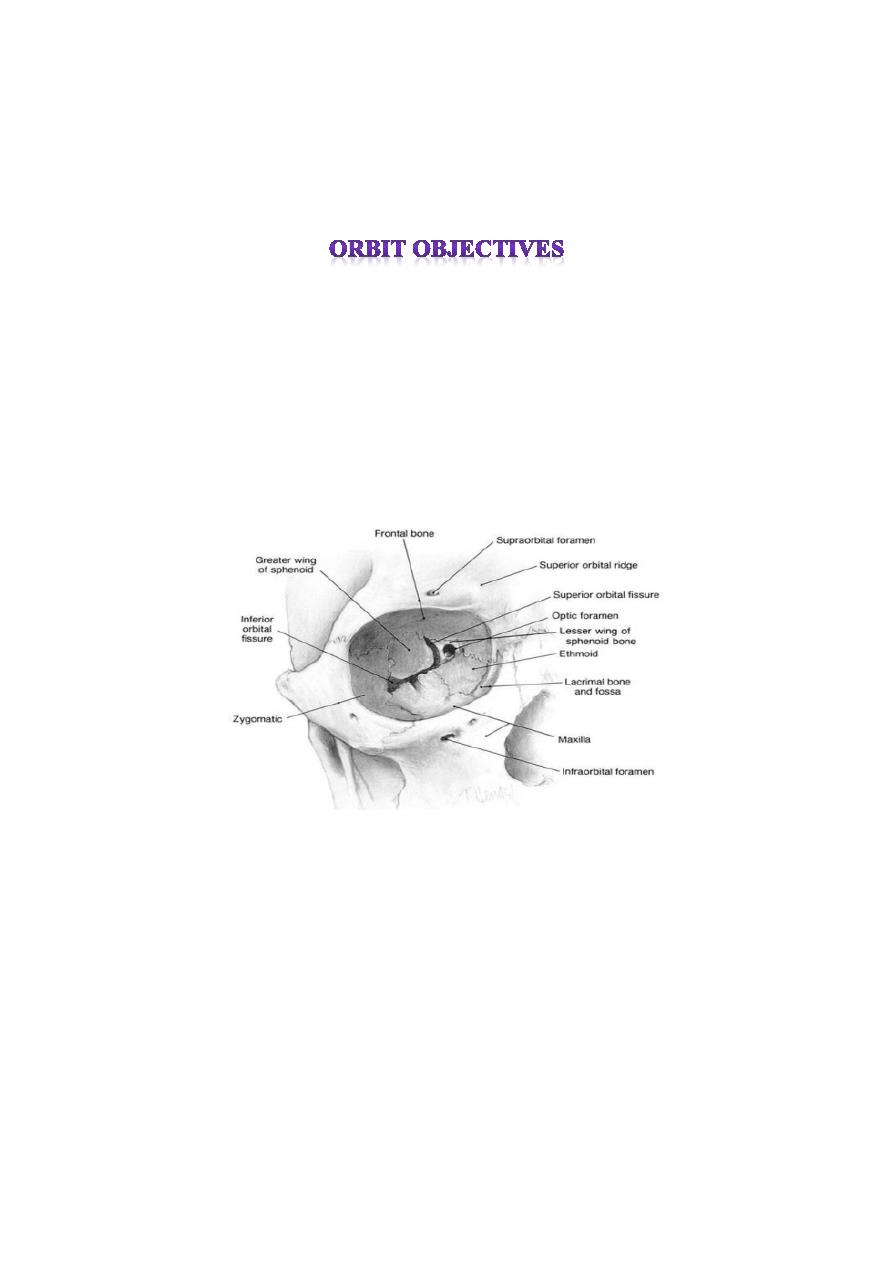
Anatomy of orbit
The orbit pear shaped cavity, the stalk of which is the optic
canal.
1- The roof; consist of two bones: lesser wing of sphenoid and
orbital plate of the frontal bone.
2- The lateral wall: consist of two bones: greater wing of
sphenoid and the zygoma
3- The floor: consist of three bones: zygoma, maxillary and
palatine bones, the posteromedial portion of maxillary bone is
relatively weak and may be involved in blowout fracture.
2
4- The medial wall: consist of four bones: maxillary, lacrimal,
ethmoid and sphenoid, the lamina papyracea, which forms part
of the medial wall, is paper-thin and perforated by numerous
foramina for nerves and blood vessels. Orbital cellulitis is
therefore frequently secondary to ethmoidal sinusitis.
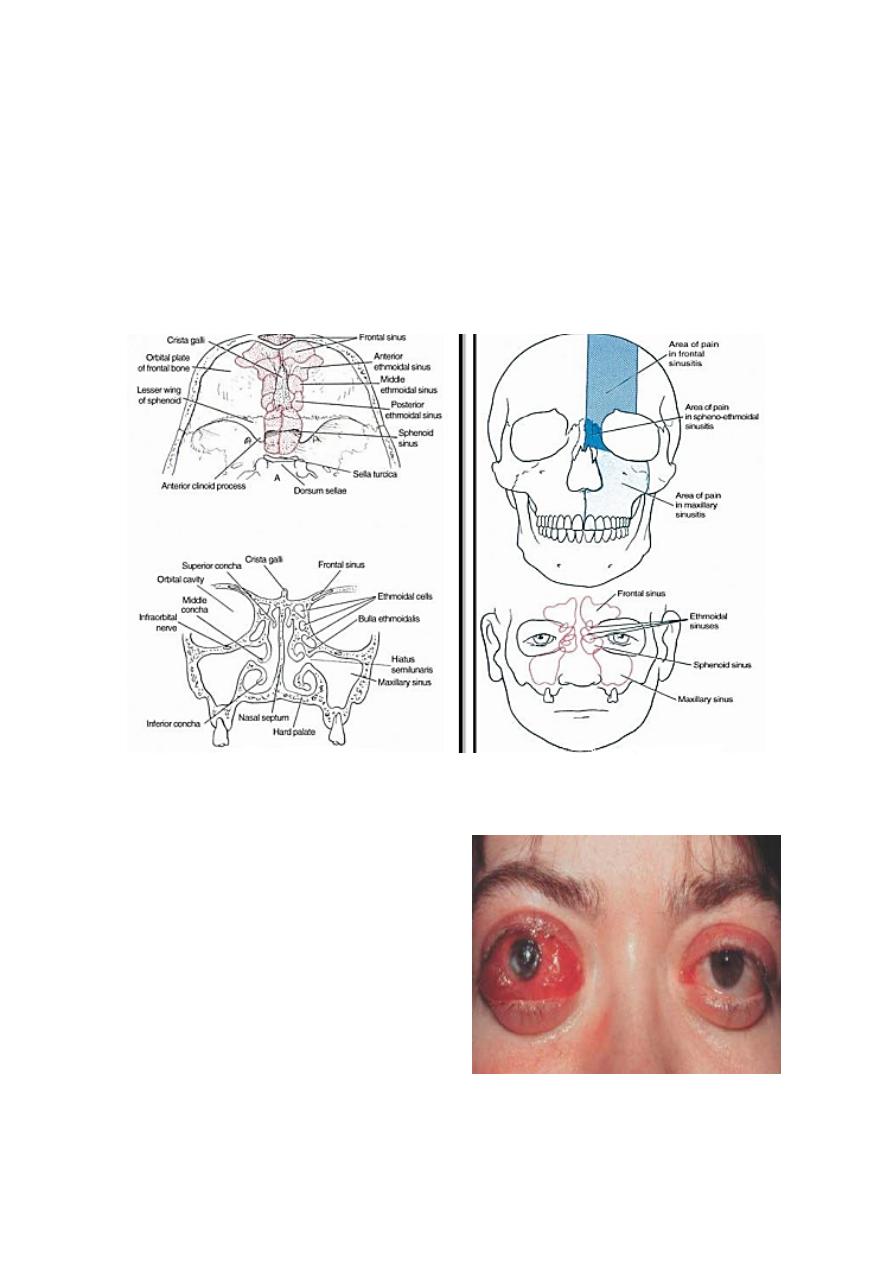
Para-nasal sinuses
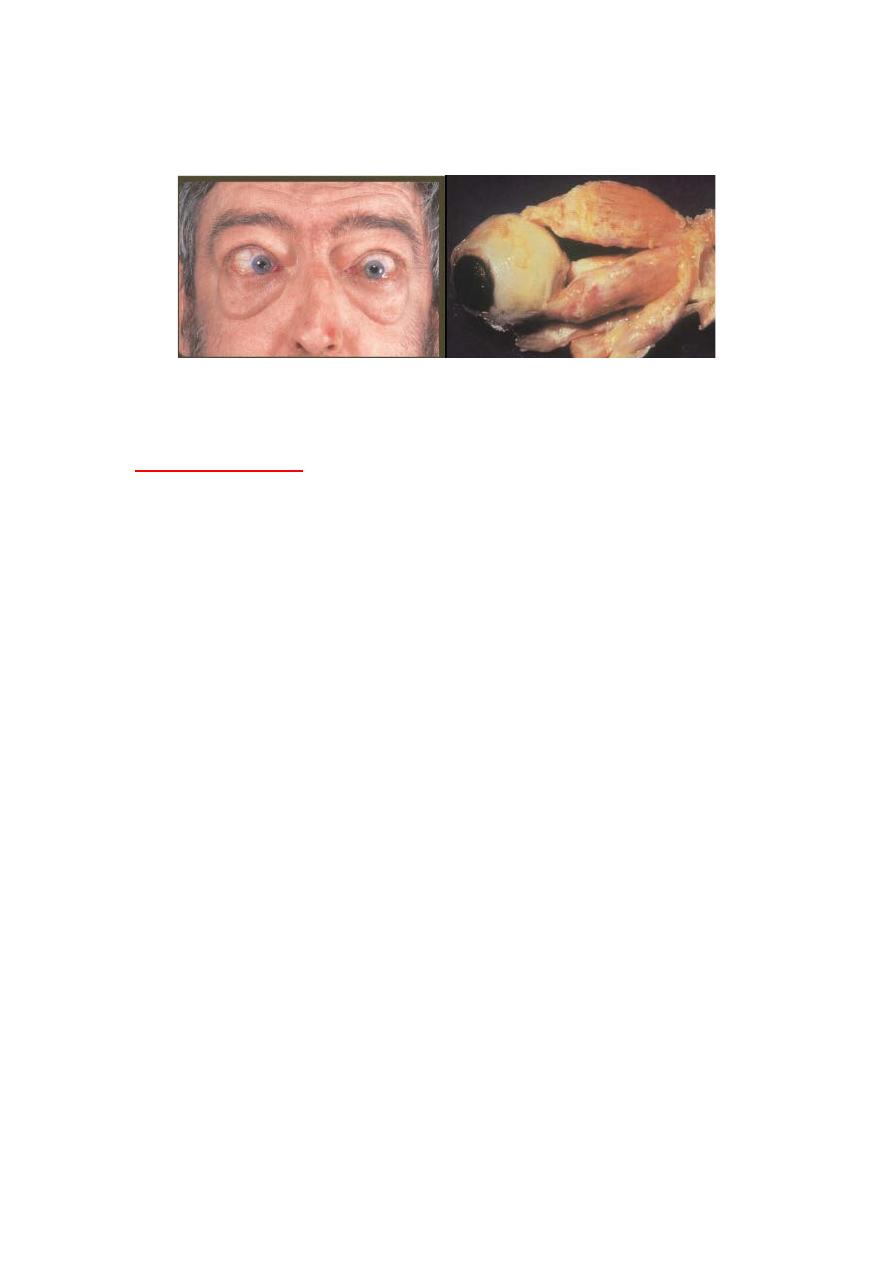
Proptosis
Definition:
• Abnormal protrusion of the
globe which may be caused
by retrobulber lesions or
less frequently, by a
shallow orbit.
• Asymmetrical proptosis is
best detected by looking
down at patient from above
and behind.
3
Thyroid eye disease
Autoantibodies to both thyroid and orbital tissue cause
inflammation; the extraocular muscle are particularly affected.
Clinical features;
The clinical course involves an active "congestive stage”,
usually lasting 2-3 years, followed by a “quiescent stage” in
which residual restriction of ocular movements may be the chief
features.
Symptoms:
1-redness
2- Irritation
3- Aching
4-wide-eyed; staring appearance
5- Double vision
6-decresed vision in severe cases.
Signs:
1- Fullness of eyelids
2-conjunctival hyperemia and chemosis
3- Proptosis (exophthalmos0); may be unilateral or bilateral. If
sever, may prevent adequate lid closure with resultant exposure
keratopathy.
4- Lid retraction in primary position, which compounds the
cosmetic effect of proptosis
5-lid lag in down gaze (von Grafe’s sign).
4
6- Ophthalmoplegia due to inflammation early in the disease
and subsequently to fibrosis. The inferior and medial recti are
most frequently affected.
7- Choroidal folds.
8-optic neuropathy; is a sight threatening complication caused
by compression of optic nerve or its blood supply by swollen
orbital tissue, particularly extraocular muscles. Useful tests
include color vision, visual acuity and visual fields. There may
be a relative afferent pupillary defect and optic disc edema.
Management:
1- Tear substitutes and topical steroids for conjunctival and
corneal involvement.
2- Systemic steroids usually reserved for optic neuropathy.
3- Surgery for proptosis (orbital decompression), diplopia
(muscle surgery) and eyelid retraction.
4- Radiotherapy may be appropriate for congestive phase, if
sever.
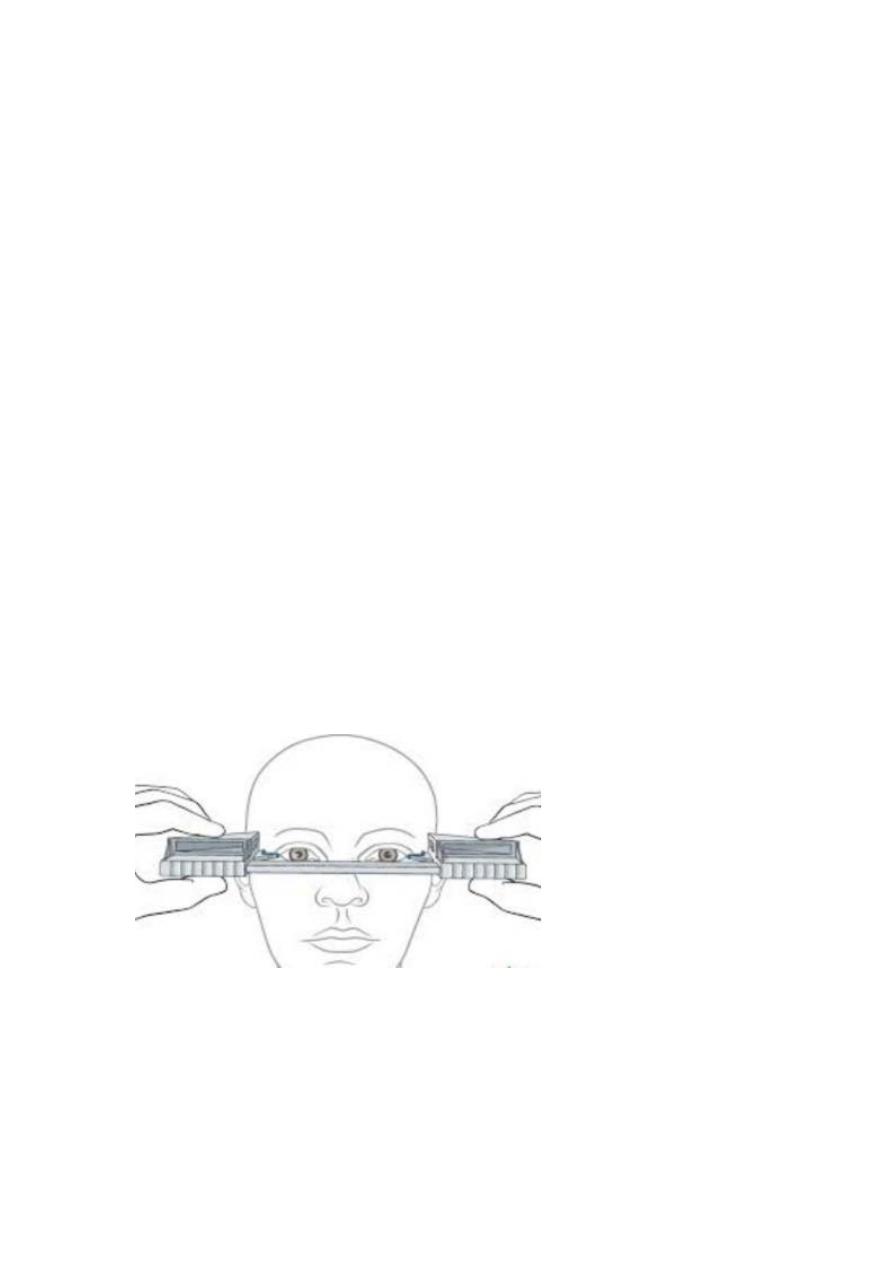
Hertel exophthalmometer:
Reading greater than 20 mm are indicative of proptosis and a
difference of 2 mm between the two eyes is suspicious
regardless of absolute value.
Proptosis is graded as mild (21-23 mm), moderate (24-27 mm),
and sever (28 mm or more).
5
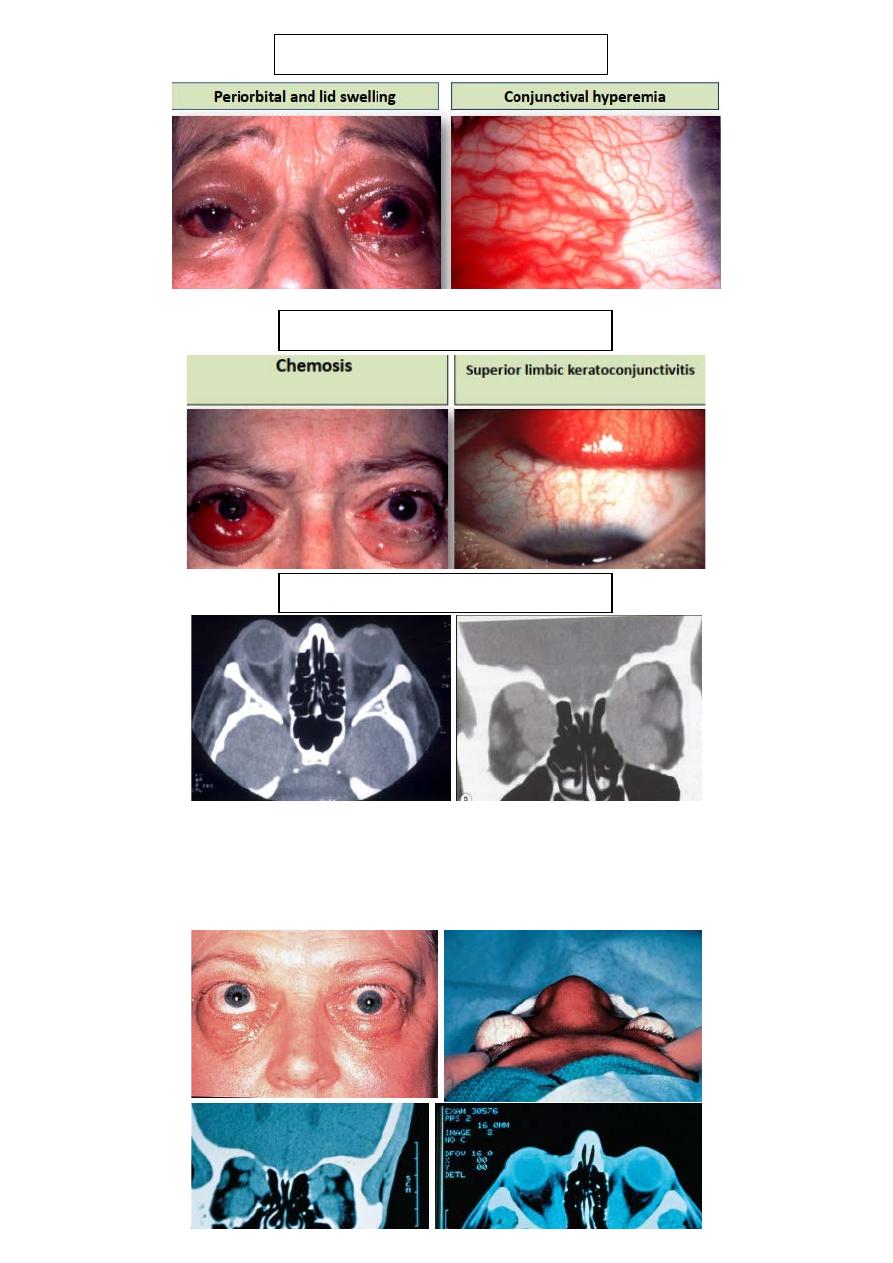
Soft tissue involvement
Soft tissue involvement
Optic neuropathy
Treatment:
Initial treatment is usually with systemic steroids. Orbital
decompression may considered if steroids are ineffective or
inappropriate.
6
Treatment of congestive phase
• Tear substitute.
• Corticosteroids.
• Orbital irradiation or surgical
• decompression.
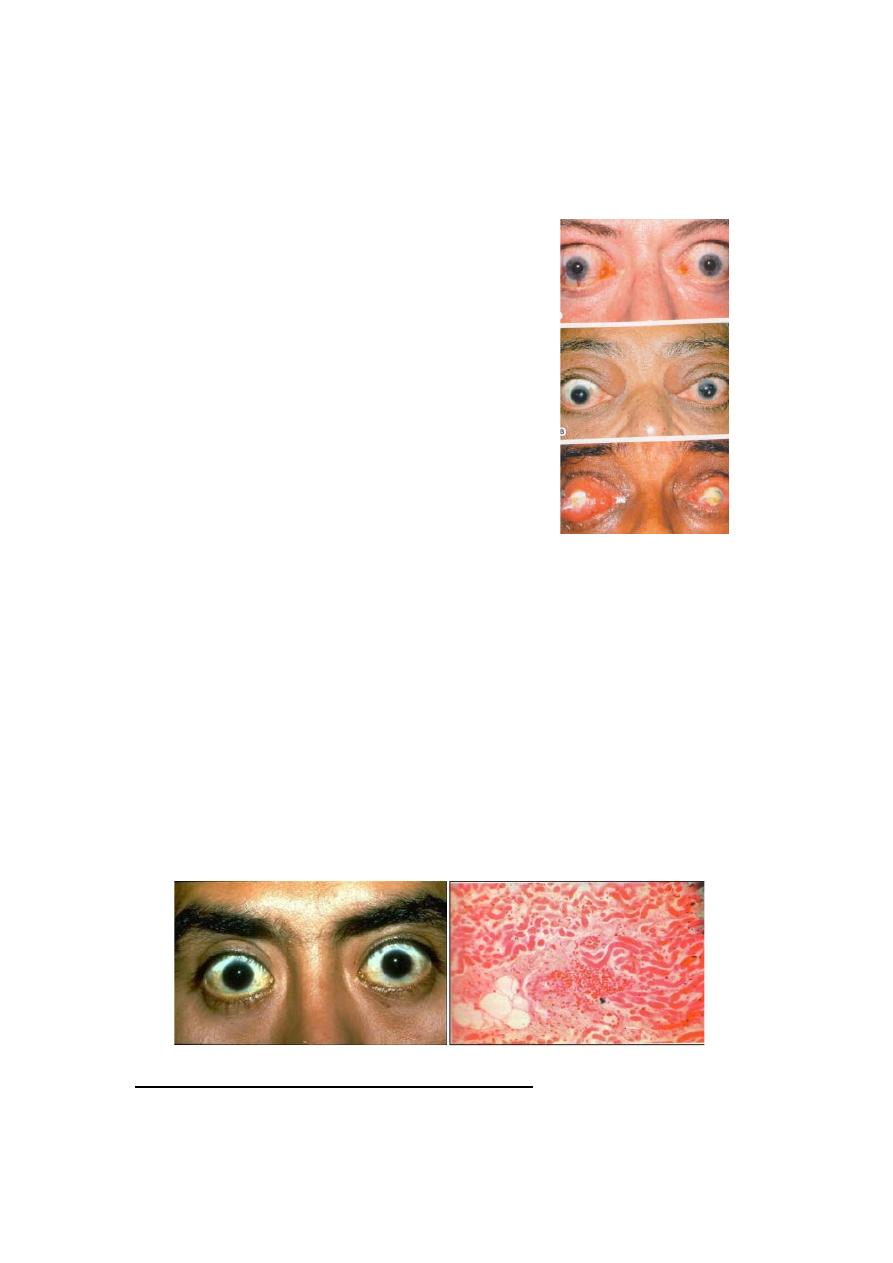
Thyroid Opthalmopathy
Not always correlated with
serum thyroid levels.
• Can progress after thyroid
function is normal.
Thyroid Opthalmopathy: classes
0
N
o sign or symptoms.
1
O
nly signs.
2
S
oft tissue involvement.
3
P
roptosis.
4
E
xtraocular muscle involvement.
5
C
orneal damage.
6
S
ight loss.
Thyroid eye disease histopathology:
1-Inflammation of extraocular muscles: characterized by
Pleomorphic cellular infiltration associated with increased
secretion of glycosaminoglycans and osmotic imbibition of
7
water. The muscles might enlarged and may compress the optic
nerve. Subsequent, degeneration of muscle fibers eventually
leads to fibrosis, which exert tethering effect on involved
muscle, resulting in restrictive myopathy and diplopia.
2- Inflammatory cellular infiltration: with lymphocytes,
plasma cells macrophages and mast cell of interstitial tissues,
orbital fat with accumulation of glycoaminoglycans and
retention of fluid.
Acute congestive phase:
Orbital cellulitis
• A potentially life-threatening
acute bacterial infection of
soft tissue of the orbit.
Etiology:
1- secondary to sinusitis.
2- spread from adjacent
structures(e.g. dacryocystitis).
3- following trauma and surgery.
Symptoms: acute lid swelling and redness, pain and malaise.
Signs: Reduced visual acuity, lid edema and erythema, chemosis
painful ophthalmoplegia, and optic disc swelling.
8
Complications:
Intracranial infection, cavernous sinus thrombosis, sub-
periosteal abscess and blindness
Management:
Intravenous antibiotics.
Orbital CT, principally to rule out an abscess.
Surgery for abscess drainage or sinus washout.
Orbital cellulitis histopathology
Idiopathic orbital inflammation(pseudotumor)
Definition: idiopathic inflammation of soft tissue of the orbit.
Clinical features:
Sub-acute onset of unilateral pain, lid edema, chemosis,
proptosis, decreased vision and ophthalmoplegia
Management:
Observation in relatively mild cases.
9
Biopsy required in persistent cases to confirm the diagnosis and
rule out neoplasia.
Systemic steroids, radiotherapy or cytotoxic agents
(methotrexate or mycophenolate mofetil).
Systemic infliximab: a tumor necrosis factor inhibitor.
Differential diagnosis:
1- Bacterial orbital cellulitis.
2-Sever acute thyroid eye disease.
3- Systemic disorders: like wegner granulomatosis, Polyarteritis
nodosa.
4- Malignant orbital tumors.
5- Ruptured dermoid cyst.
Idiopathic orbital inflammation histopathology:
Orbital myositis:
10
Orbital venous anomalies (varices)
• Congenital enlargements
of pre-existing
venous channels.
• Usually unilateral.
• May bleed or become thrombosed.
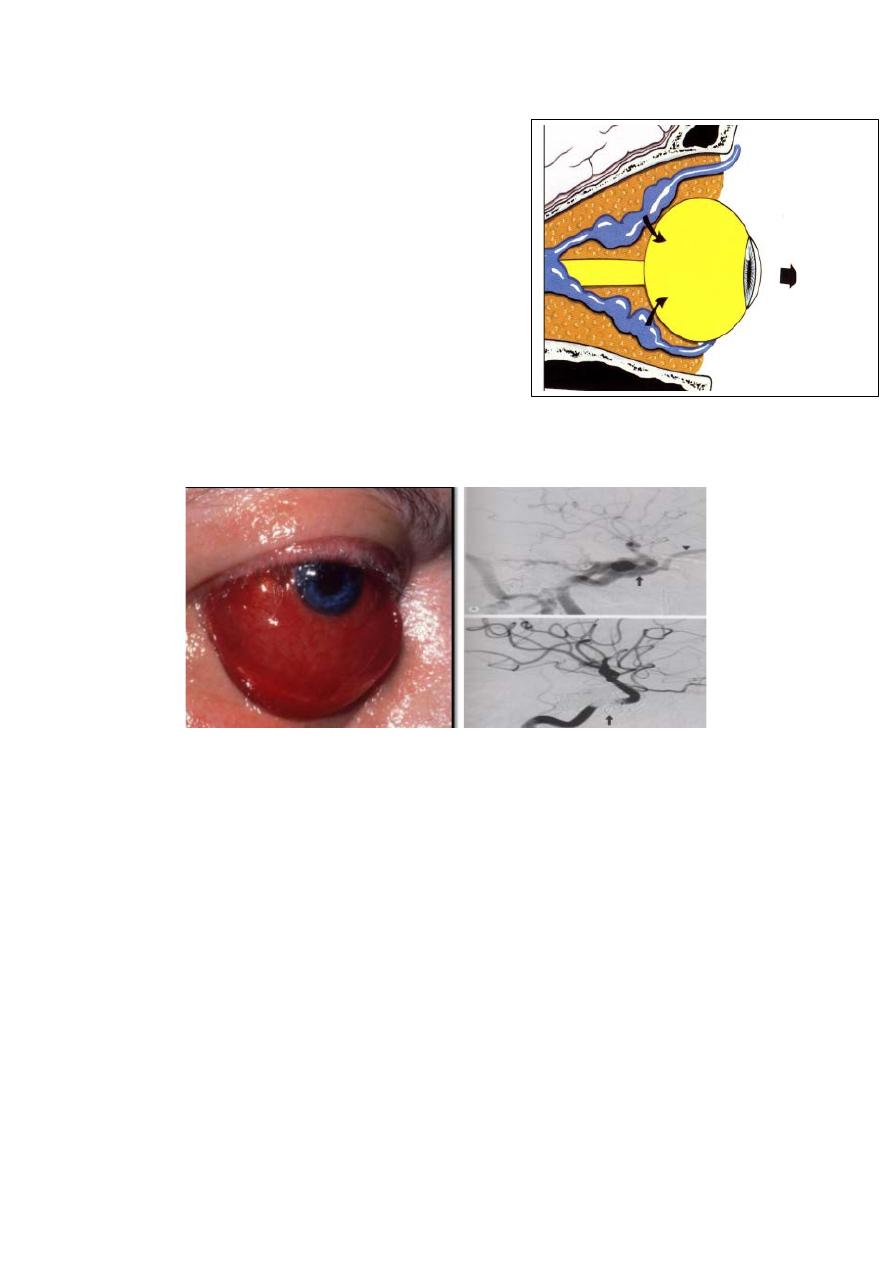
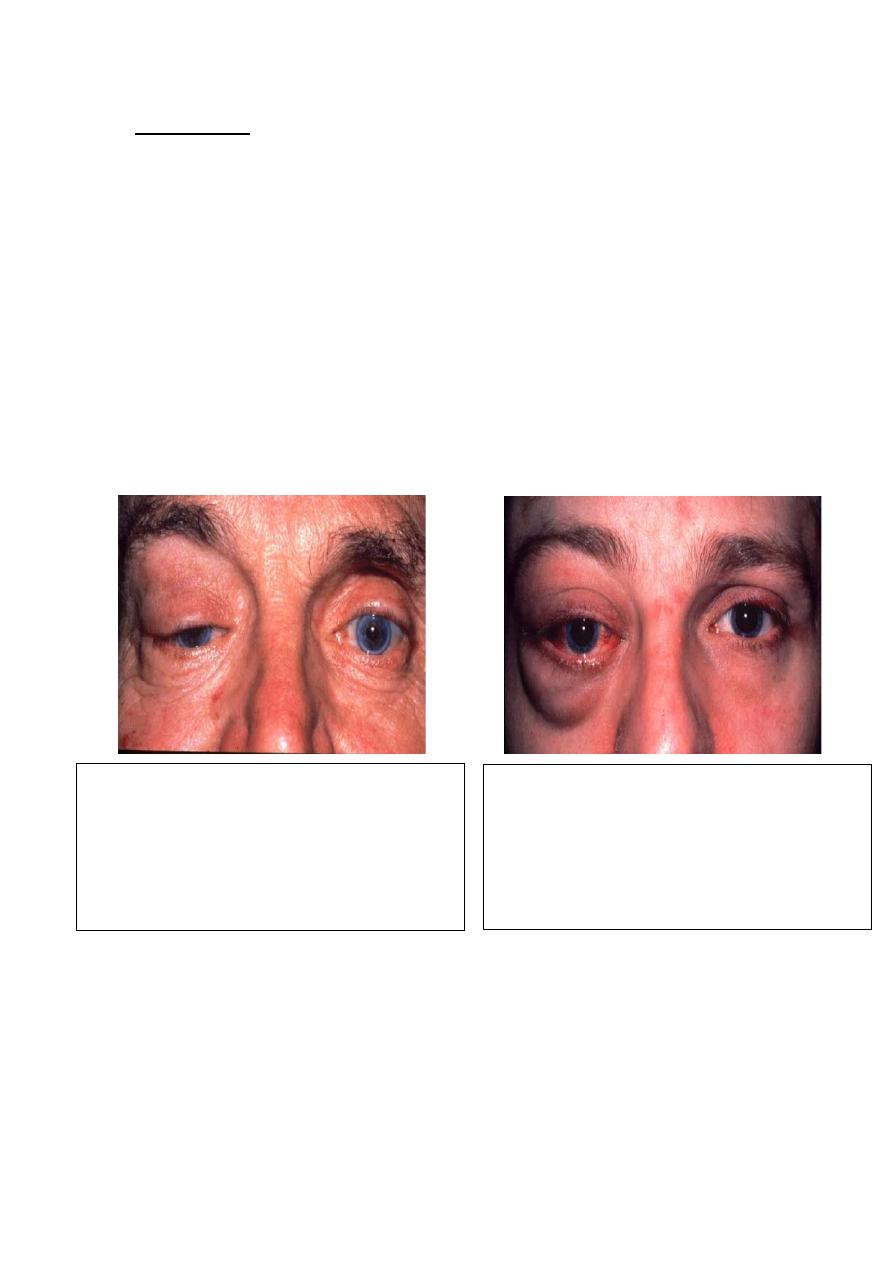
Carotid cavernous sinus fistula
Indirect or direct arterial communication with the cavernous
sinus. Usually due to trauma or spontaneous arterial rupture.
Clinical features:
Headache, chemosis, dilated episcleral vessels, pulsatile
proptosis with associated thrill and bruit, ophthalmoplegia,
raised intraocular pressure and retinal vascular congestion and
hemorrhages.
Management:
radiological intervention if appropriate.
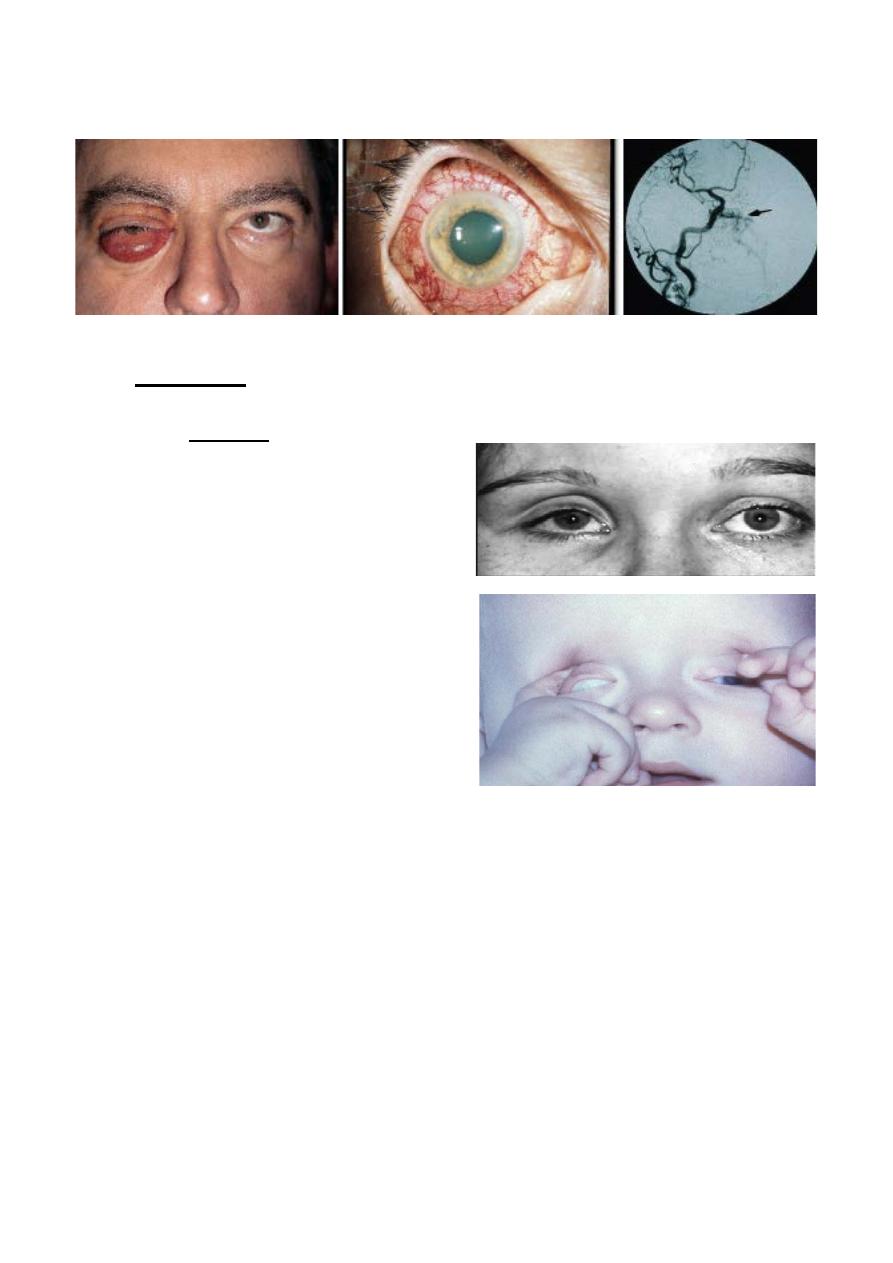
11
Arterializations of episcleral and conjunctival vessels:
Enophthalmos:
Definition;
recession of the globe within the orbit, often subtle.
• Causes:
1. structural abnormalities in
the orbital walls that may
be post- traumatic, such as
blow-out fractures of
orbital floor or congenital,
2. Atrophy of orbital contents
secondary to radiotherapy,
scleroderma or eye poking
(oculodigital sign) in blind
infants.
3. Sclerosing orbital lesions
such as metastatic schirrus
carcinoma.
Pseudo-enophthalmos may be caused by microphthalmos
or phthisis bulbi.
Leber congenital amaurosis:
Is a sever rod-cone dystrophy that is the commonest genetic
cause of visual impairment in infant and children. It carries very
poor prognosis.
Inheritance: Autosomal recessive.
Presentation: is with blindness at birth, or shortly thereafter;
associated with nystagmus.
Oculodigital syndrome: in which constant eye rubbing by the
child causing enophthalmos because of atrophy of orbital fat.
12
Ocular associations: Strabismus, hypermetropia and
keratoconus.
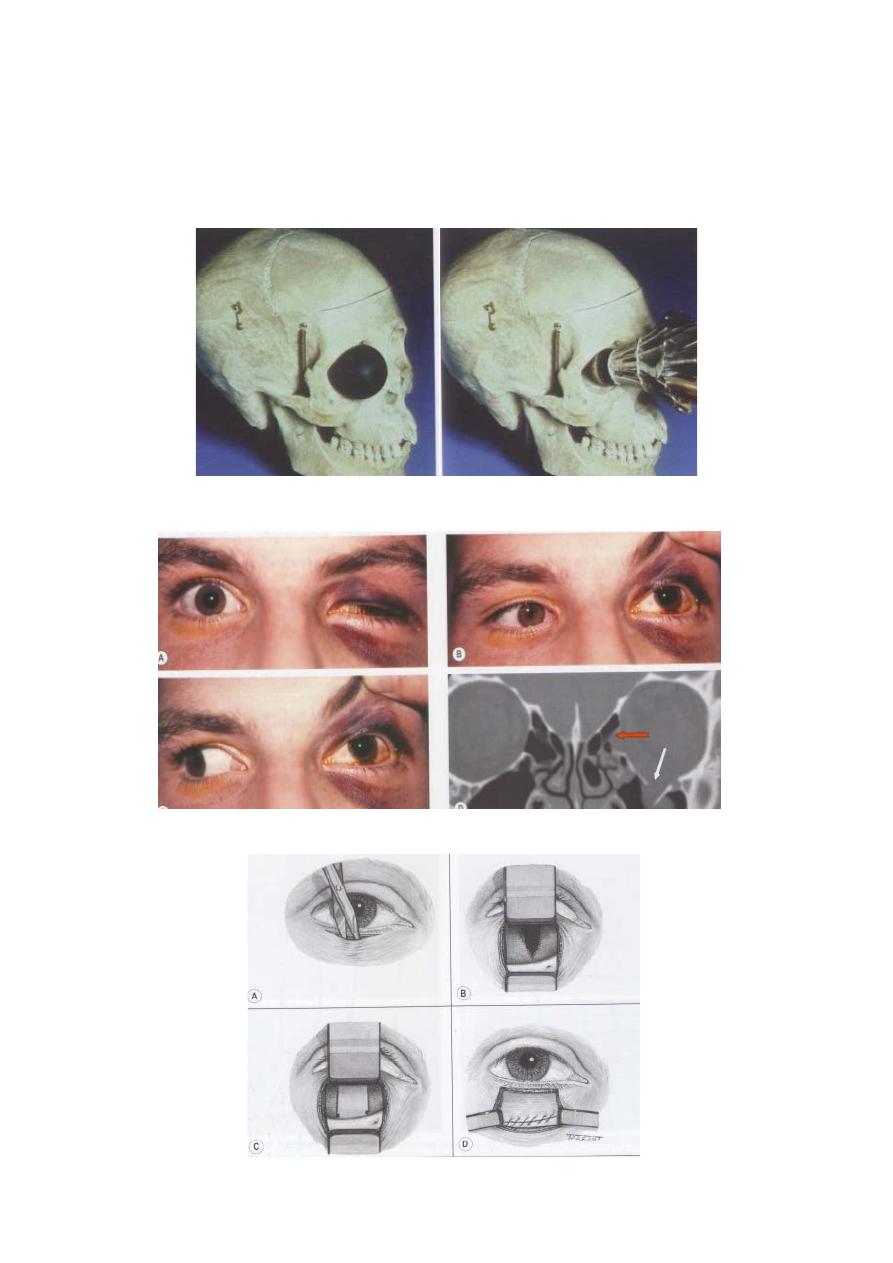
Orbital blow-out fracture:
Blow-out fracture of orbital floor:
Repair of blow-out fracture:
13
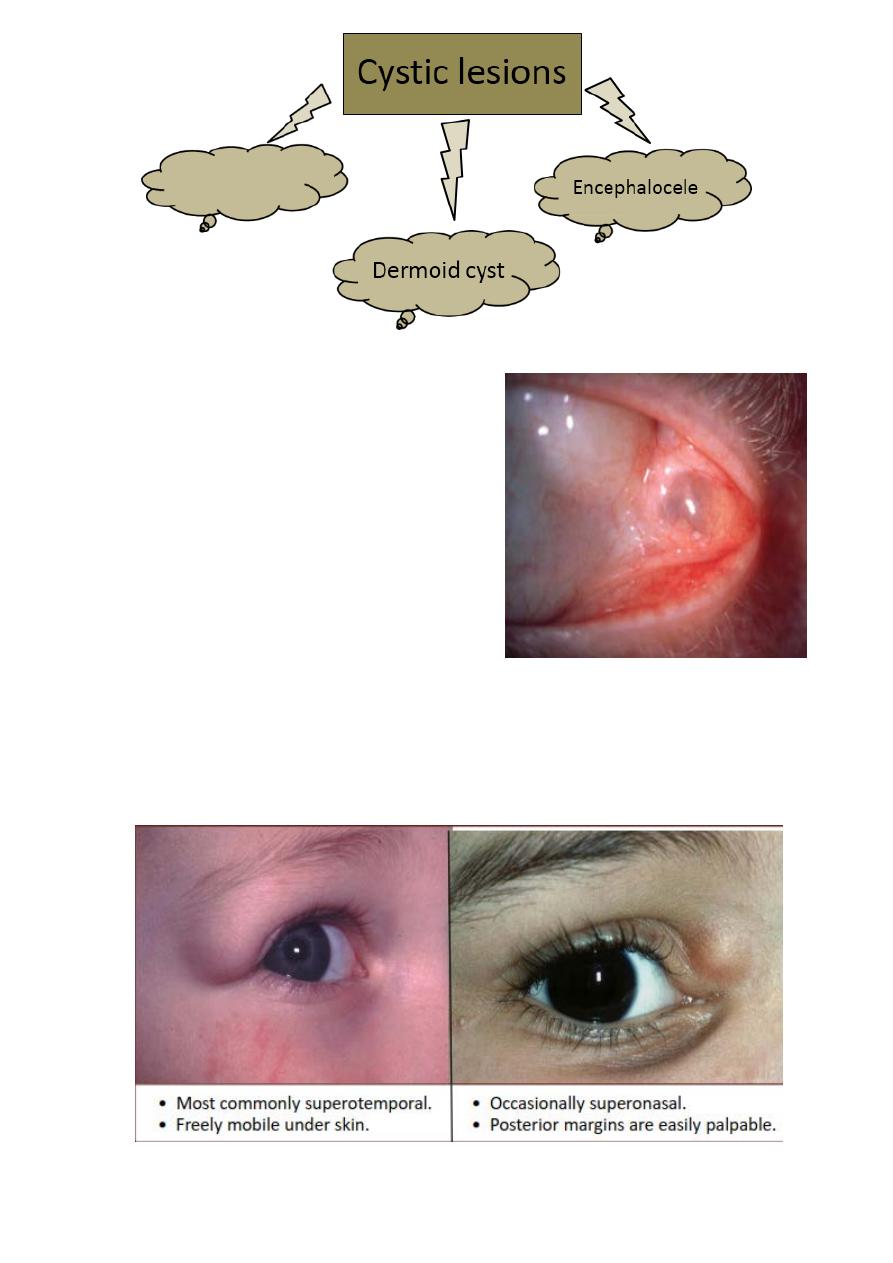
Dacryops:
Definition:
Ductal cyst of lacrimal gland,
uncommon frequently bilateral.
• Signs:
Round cystic lesion,
originating from the palpebral
portion of lacrimal gland,
which protrudes into the
superior fornix.
• Treatment:
Excision or marsupalization.
Superficial dermoid cyst:
• Presents in infancy.
• No displacement of globe.
14
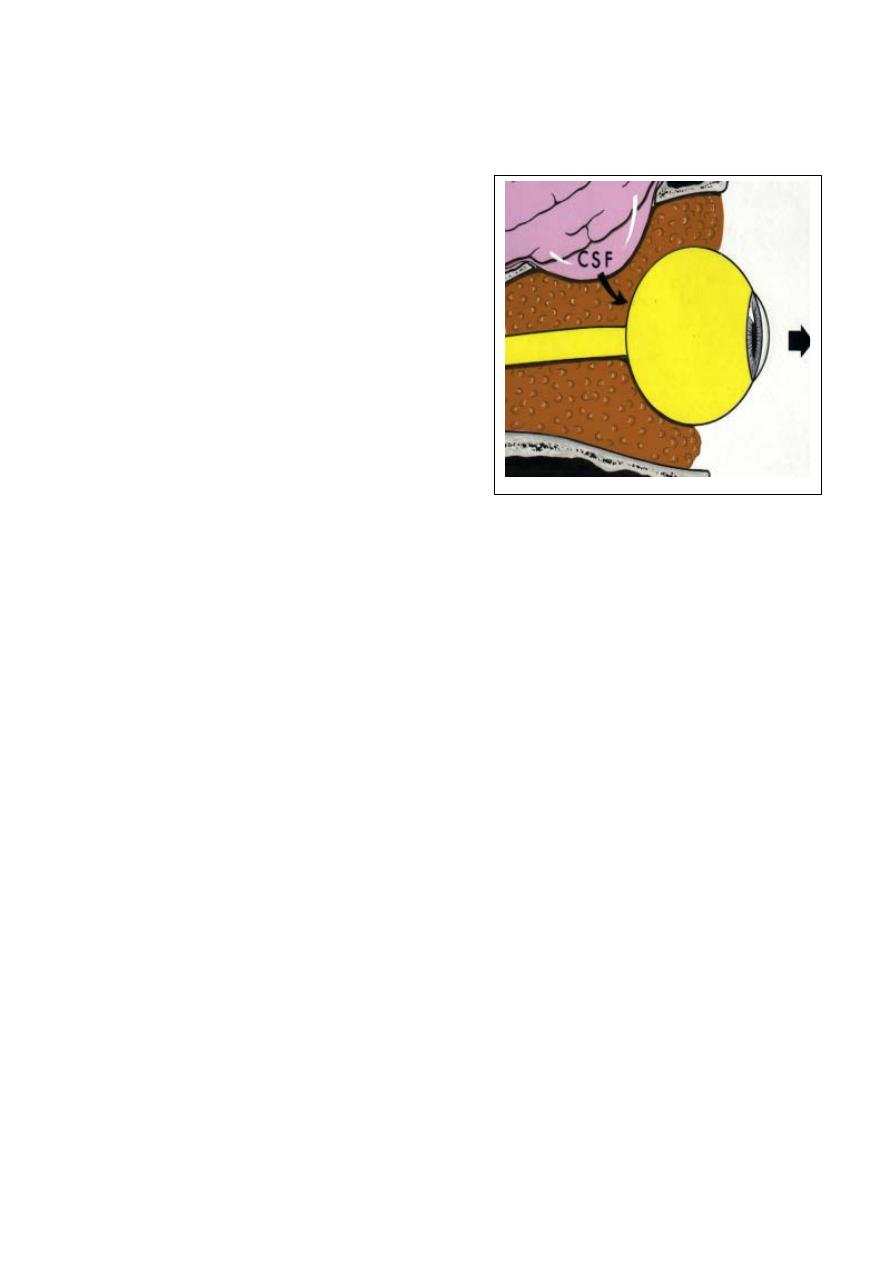
Encephalocele
:
Encephalocele
:
Herniation of
intracranial contents through
congenital skull defect.
Transmission of CSF pulsation
causes pulsating proptosis
without a bruit.
Meningocele
- contains only dura.
Meningoencephalocele
- contains
dura and brain tissue.
• Anterior (fronto-ethmoidal).
• Posterior (spheno-orbital).
CT scan shows the bony defect responsible for the herniation.
Association:
1- Other bony abnormalities, such as hypertelorism, broad nasal
bridge and cleft palate.
2- Ocular; include microphthalmos, orbital varieses and
coloboma.
3- Neurofibromatosis I (NF-I) frequently associated with
posterior encephalocele.
Tumors
1- Capillary haemangioma.
2- Cavernous haemangioma.
3- Optic nerve glioma.
4- Optic nerve sheath meningioma.
15
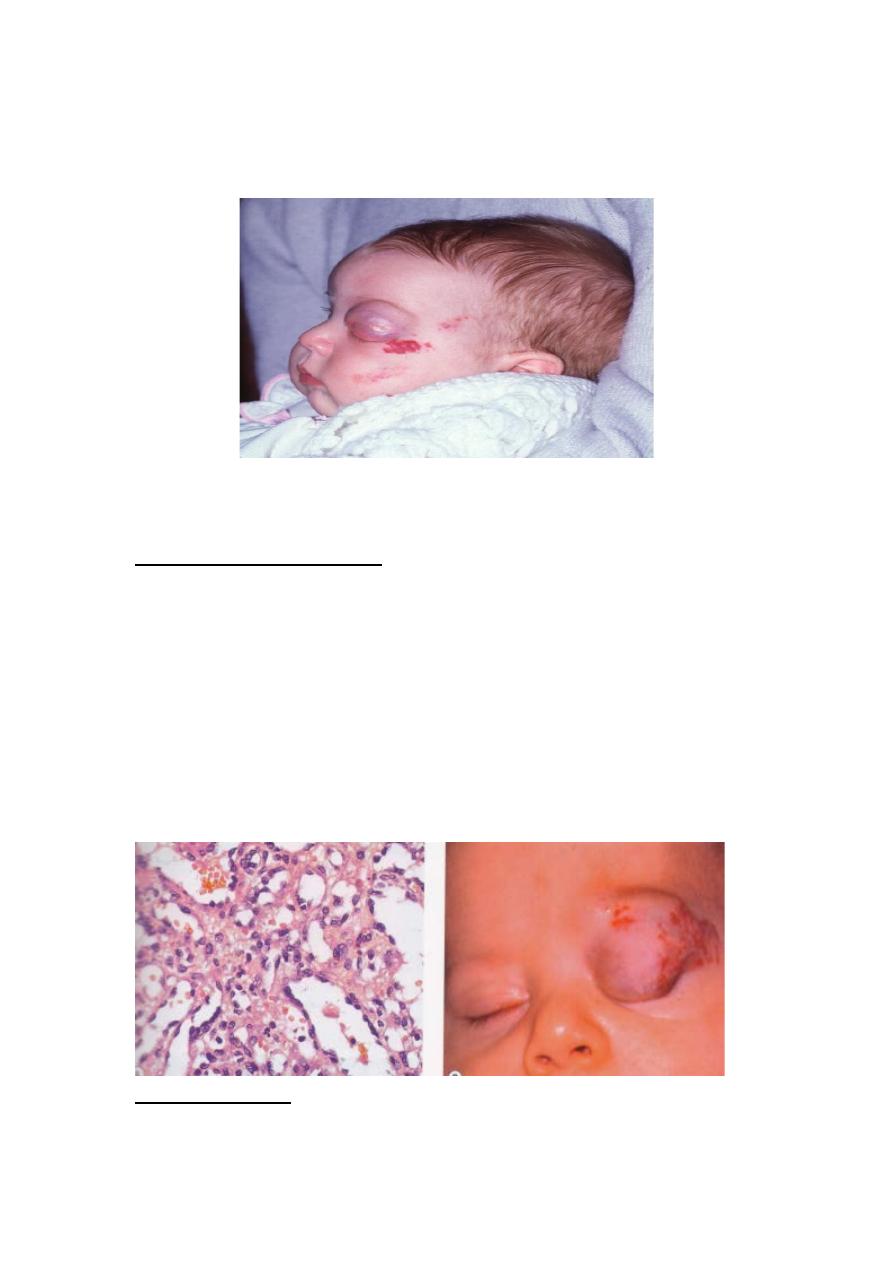
Capillary haemangioma
• Most common orbital tumour in children..
• Presents - 30% at birth and 100% at 6 months.
• Most commonly in superior anterior orbit.
• May enlarge on coughing or straining.
• Associated ‘strawberry’ nevus is common.
Capillary haemangioma
• Clinical features; presents in infancy with an anterior
orbital swelling. Which may increase in size when crying.
A similar eyelid skin lesion, a ‘strawberry’ nevus may also
be present.
• Management:
• Steroids injected into the lesion or given systemically are
effective but the tumor often involutes spontaneously.
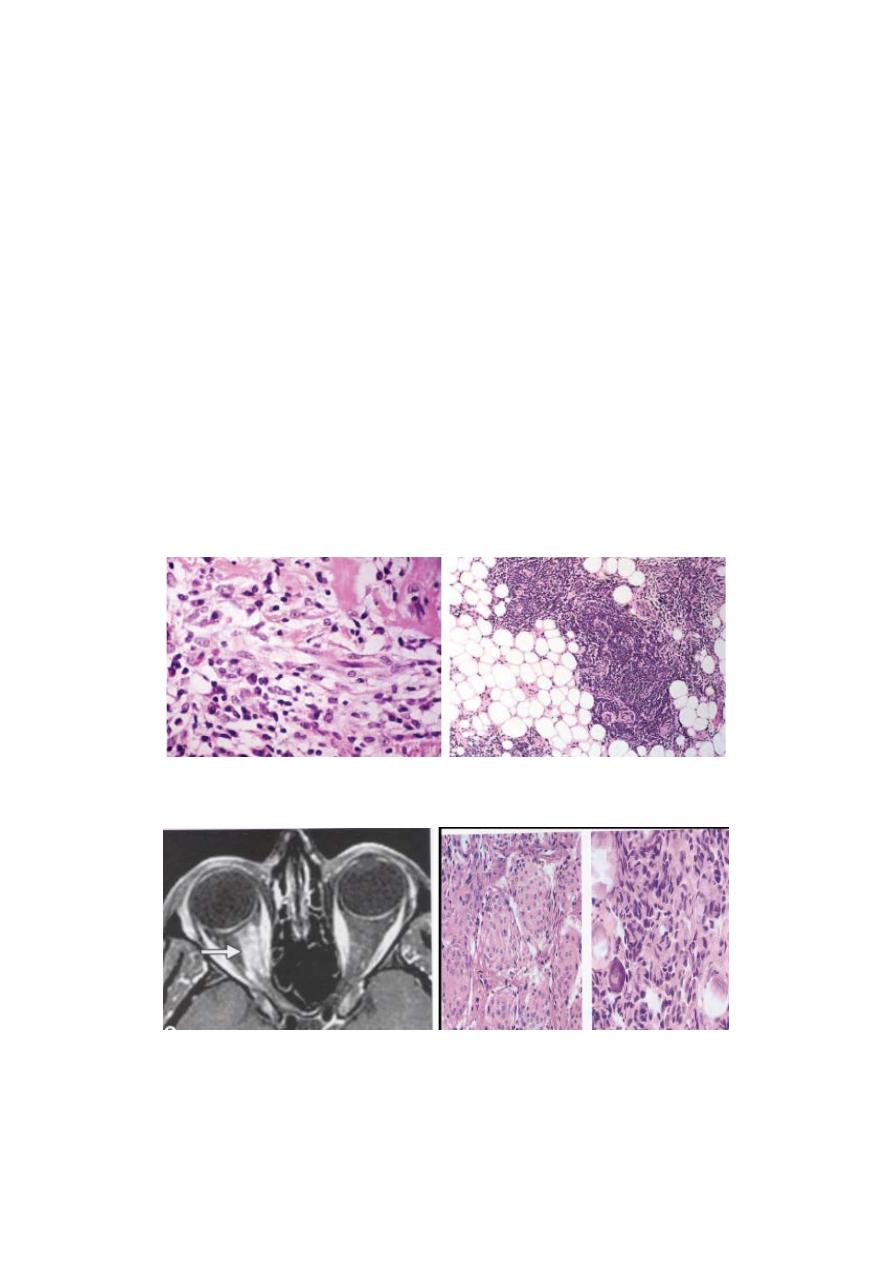
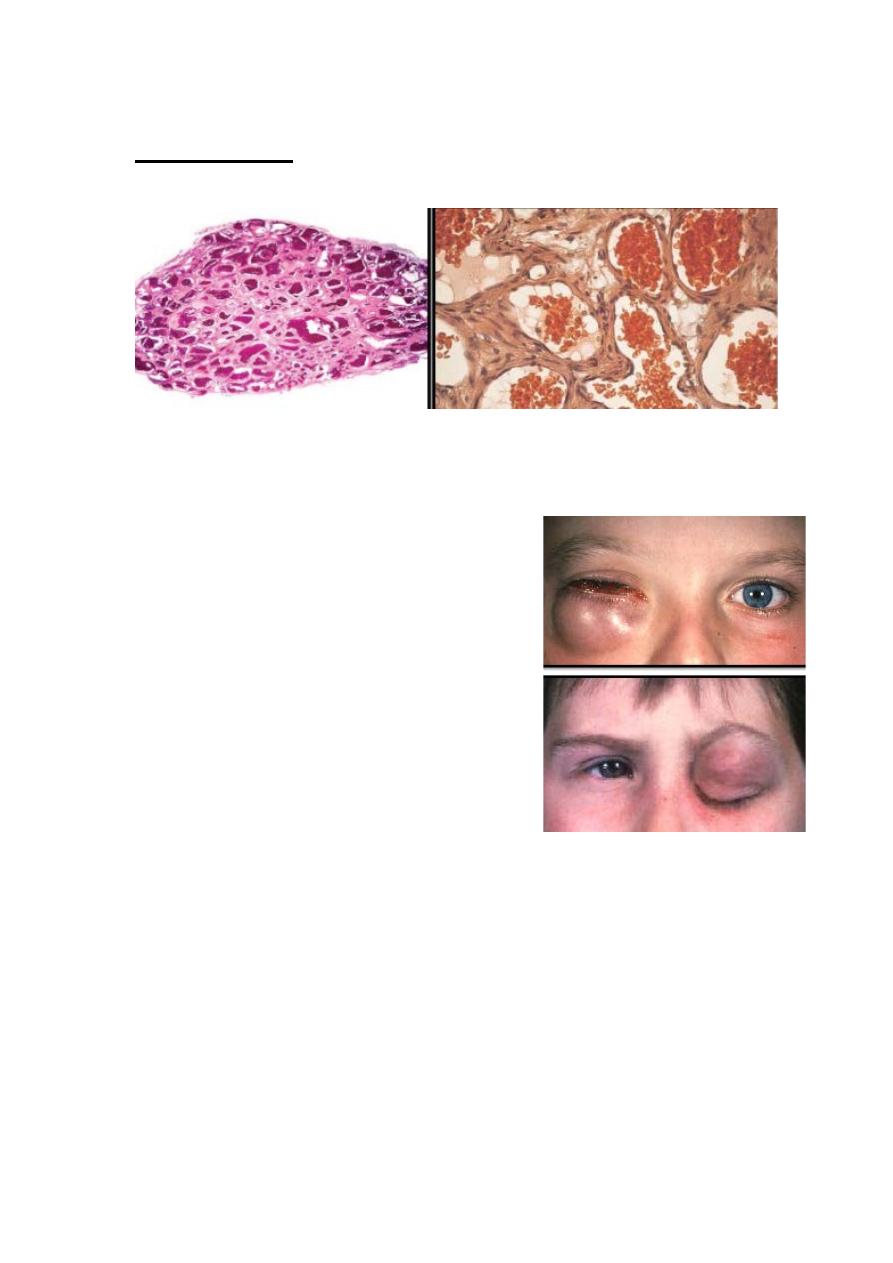
Capillary haemangioma histopathology
shows irregular capillary channels of varying
Histopathology
size.
16
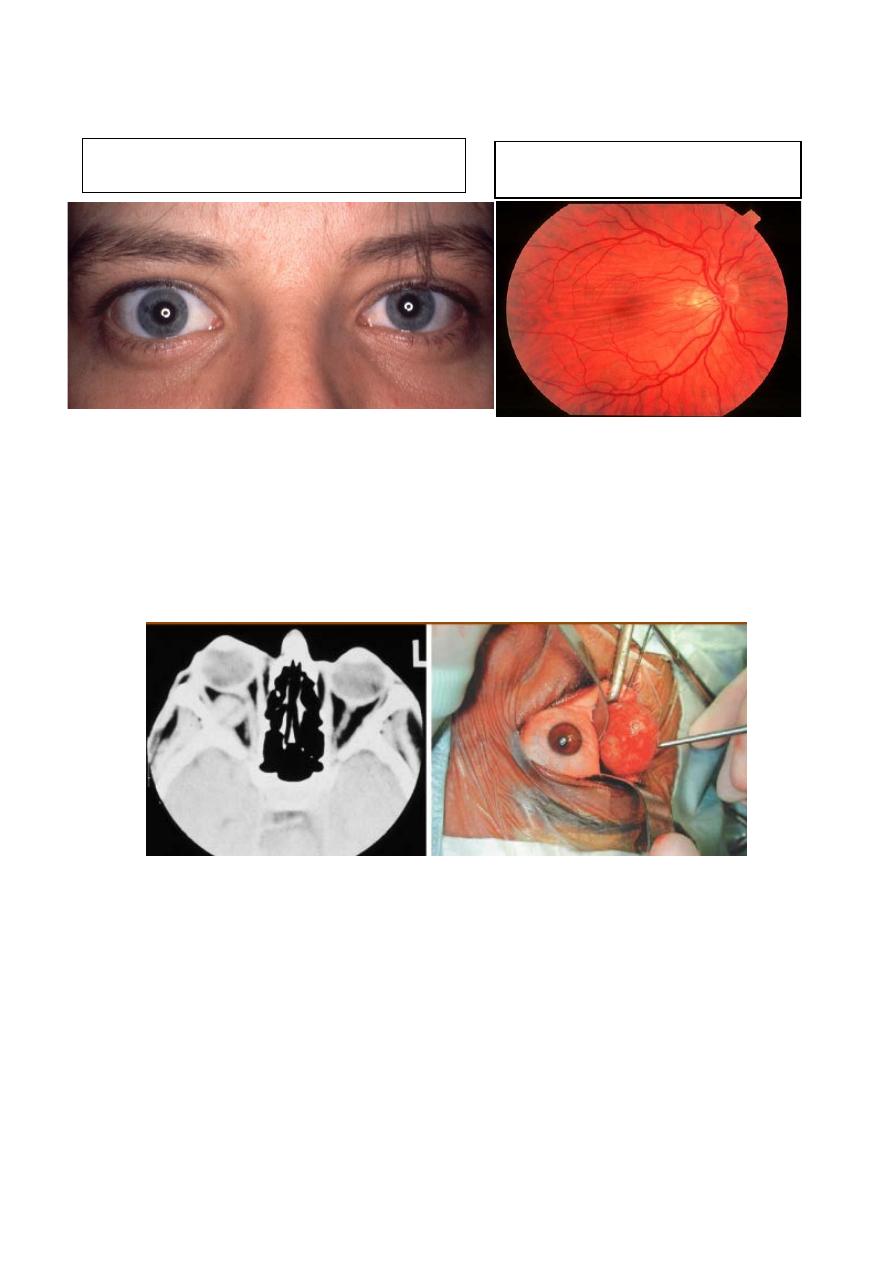
Slowly progressive axial proptosis
May cause choroidal folds.
Cavernous haemangioma:
• Most common benign orbital tumour in adults.
• Usually located just behind globe.
• Female preponderance - 70%.
• Presents - 4th to 5th decade.
Cavernous haemangioma
Clinical features:
The most common benign orbital tumor in adults. Presents in
young adults with painless axial proptosis of gradual onset
Management:
Surgical excision.
17
Capillary haemangioma histopathology
Histopathology: shows congested varying-sized endothelial-
lined vascular channels separated by fibrous septae.
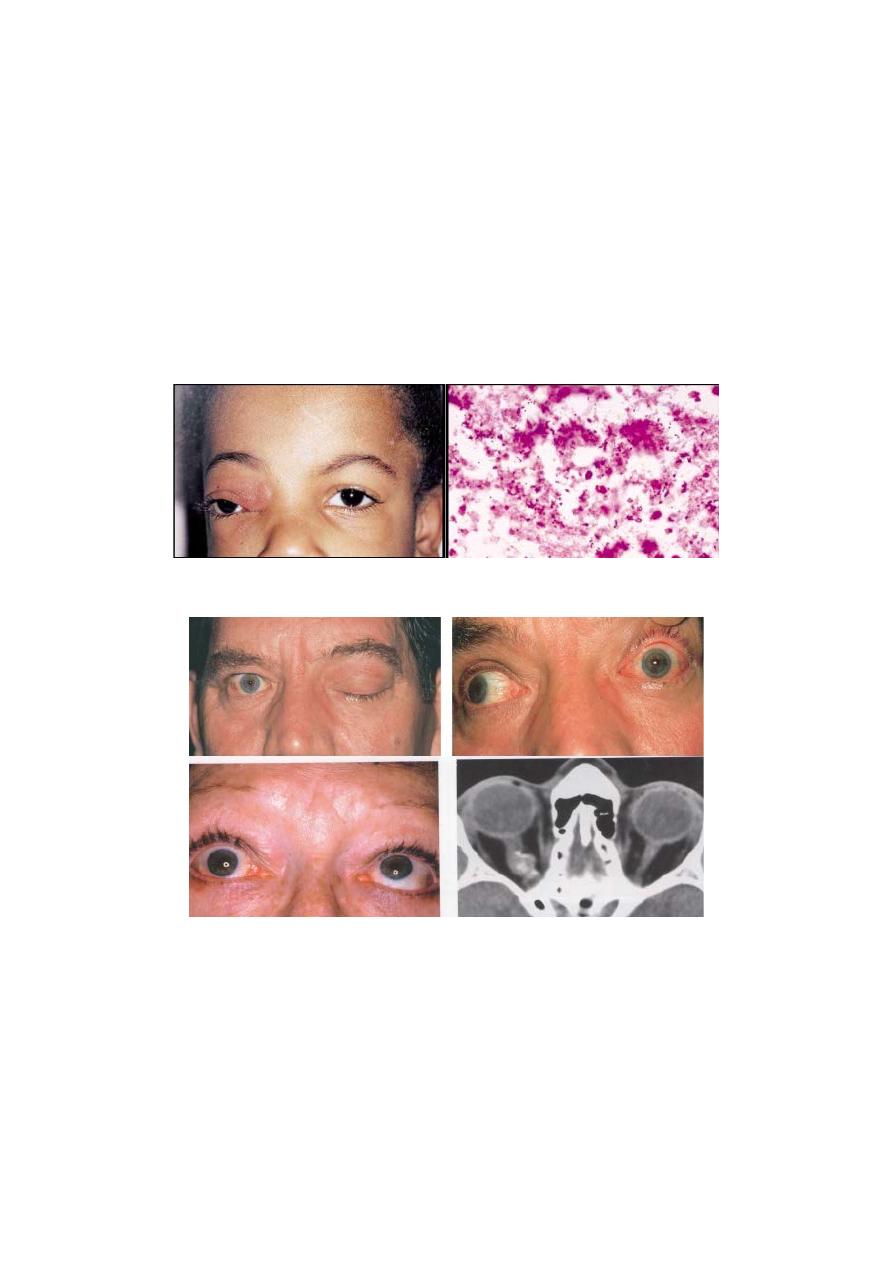
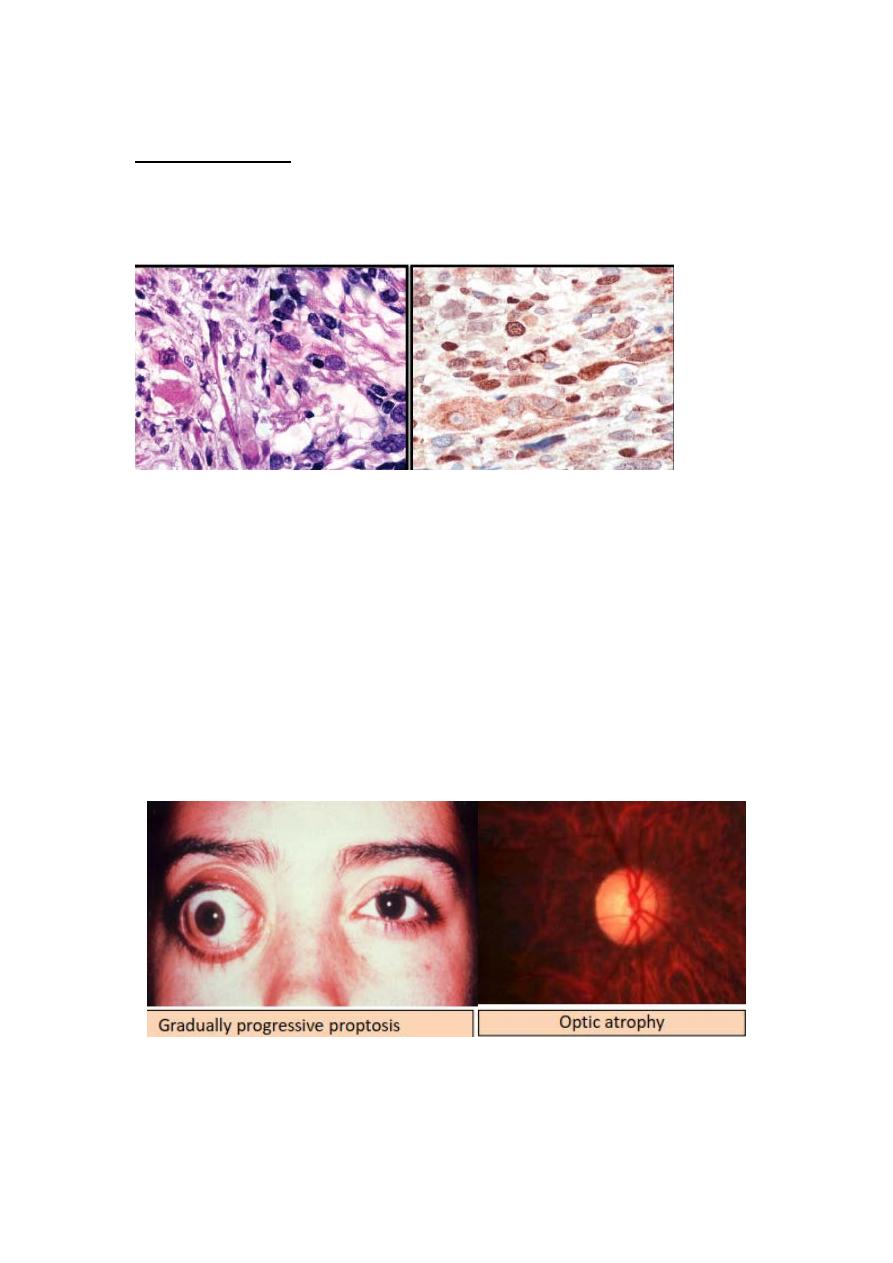
Rhabdomyosarcoma (Embryonal sarcoma):
• Most common primary
childhood orbital malignancy.
• Rapid onset in first decade
( average 7 years).
Treatment:
Radiotherapy and chemotherapy
Exenteration for radio-resistant or
recurrent tumors.
This is very rare (but the most common
primary orbital malignancy of childhood) but aggressive tumor
typically present at about the age of 7 years with progressive
proptosis and palpable mass may be present.
Management:
Incisional biopsy followed by radiotherapy and chemotherapy.
18
Rhabdomyosarcoma histopathology
: differentiated tumor shows many elongated
Histopathology
strap-like cells with eosinophilic cytoplasm (rhabdomyoblast).
Cells in the center of the field has cross-striations: Masson
trichrome stain.
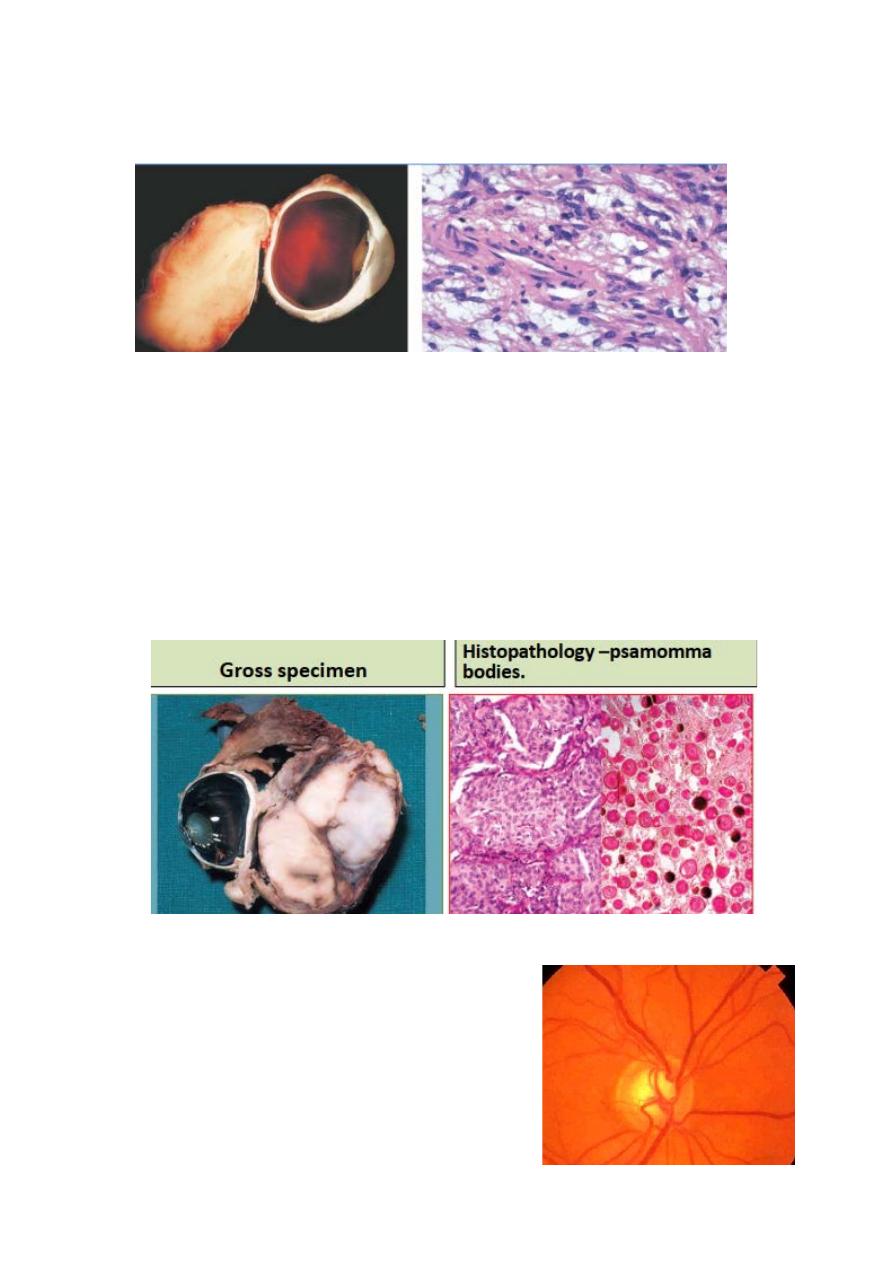
Optic nerve glioma:
Typically affects young girls.
Associated neurofibromatosis -1 is common.
Presents - end of first decade with gradual visual loss.
Treatment
Observation - no growth, good vision and good cosmesis.
Excision - poor vision and poor cosmesis.
Radiotherapy - intracranial extension.
19
Optic nerve glioma histopathology:
Histopathology: shows spindle-shaped pliocytic astrocytes and
glial filaments.
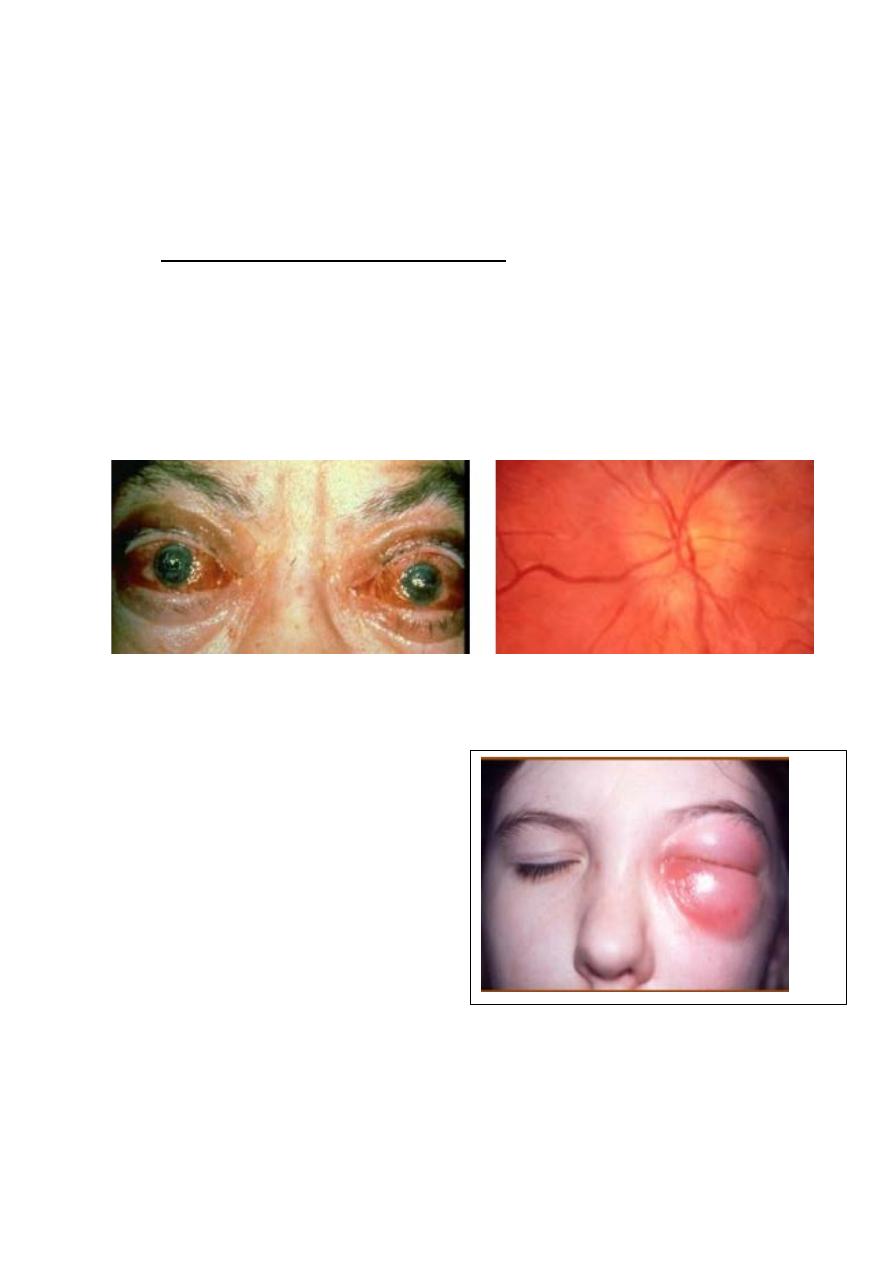
Optic nerve sheath meningioma:
Typically affects middle-aged females and causes slowly
progressive visual loss followed later by proptosis.
The optic disc frequently shows optociliary shunt vessels.
Management;
Options include observation, surgery and radiotherapy.
Optociliary shunt
Optociliary collaterals consist of
enlarged pre-existing peripapillary
capillaries, which divert blood from
central retinal venous circulation to the
peripapillary choroidal circulation when
20
there is obstruction of normal drainage channels.
On examination, the vessels appear as large tortuous channels
most frequently on temporal side, which disappear at the disc
margin.
The collateral may be associated with any orbital or optic nerve
tumor that compress the intra-orbital optic nerve and impair
blood flow through the central retinal vein.
Differential diagnosis:
1- Optic nerve sheath meningioma
2- Optic nerve glioma.
3- Central retinal vein occlusion.
4- Idiopathic intracranial hypertension.
5- Primary open angle glaucoma.
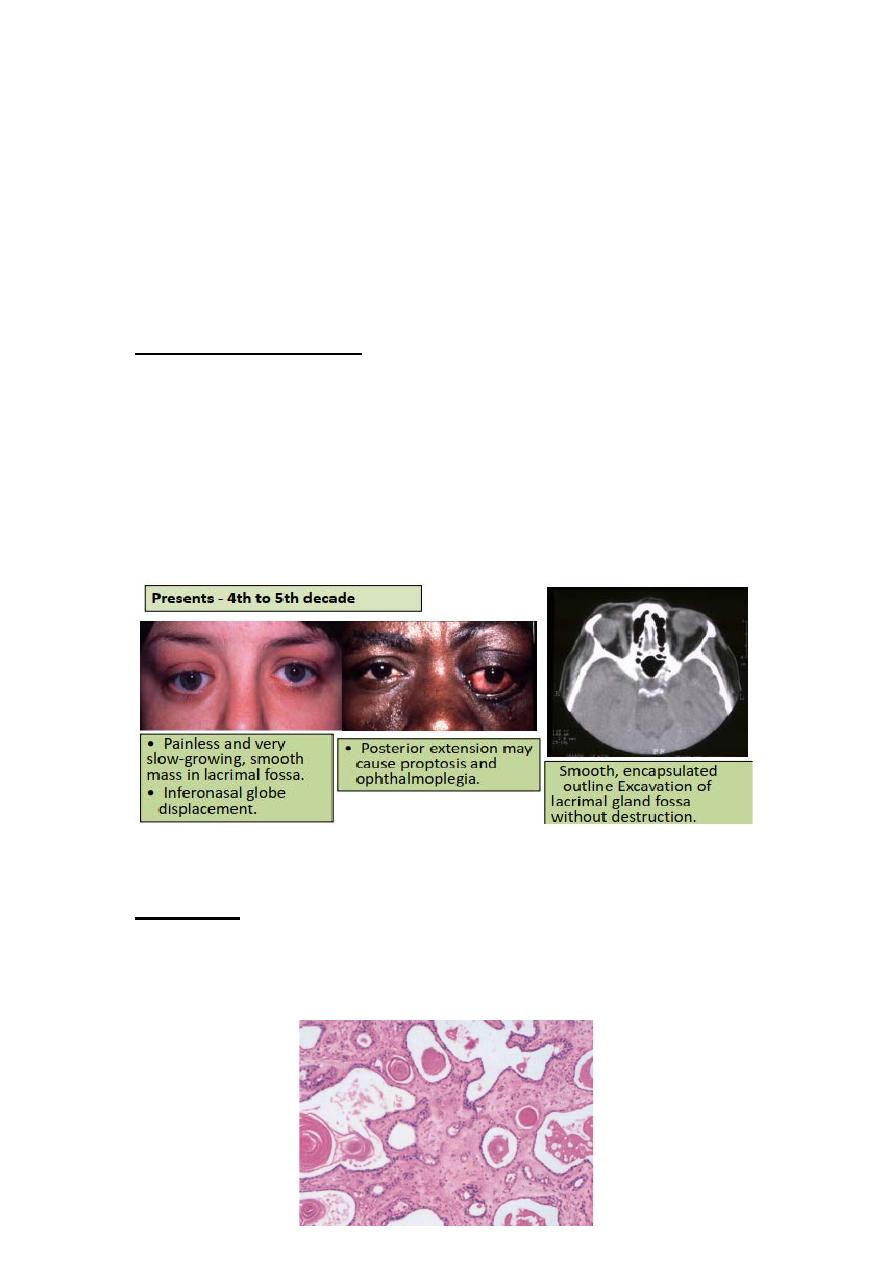
Pleomorphic Lacrimal Gland Adenoma
Pleomorphic adenoma of lacrimal gland histopathology
Histology: the inner layer of cells forms glandular tissue that
may be associated with squamous differentiation and keratin
production the outer cells undergo metaplastic changes leading
to formation of myxoid changes.
21
Treatment: surgical excision, it is wise to avoid prior biopsy to
avoid tumor seeding into adjacent orbital tissue.
Prognosis: excellent provided complete excision without
disruption of capsule.
Histology: the inner layer of cells forms glandular tissue that
may be associated with squamous differentiation and keratin
production; the outer cells undergo metaplastic change leading
to the formation of myxoid tissue.
Lacrimal gland carcinoma
• Presents - 4th to 6th decades.
• Very poor prognosis.
Management:
• Biopsy.
• Radical surgery and radiotherapy.
•
Painful, fast-growing mass in
lacrimal fossa.
•
Inferonasal globe displacement.
• Posterior extension may cause
proptosis, ophthalmoplegia and
episcleral congestion.
• Trigeminal hypoaesthesia in
25%.
