
1
) ﻋﺪد اﻻوراق
11
(
ﻋﯿﻮن
27
/
10
/
2019
د. ﻋﺰام
Lec: 4
Conjunctiva
Out-lines
1 Anatomy.
2 signs of conjunctival diseases.
3 infectious and inflammatory conjunctivitis.
4 Conjunctival degenerations.
5 Pigmented conjunctival lesions.
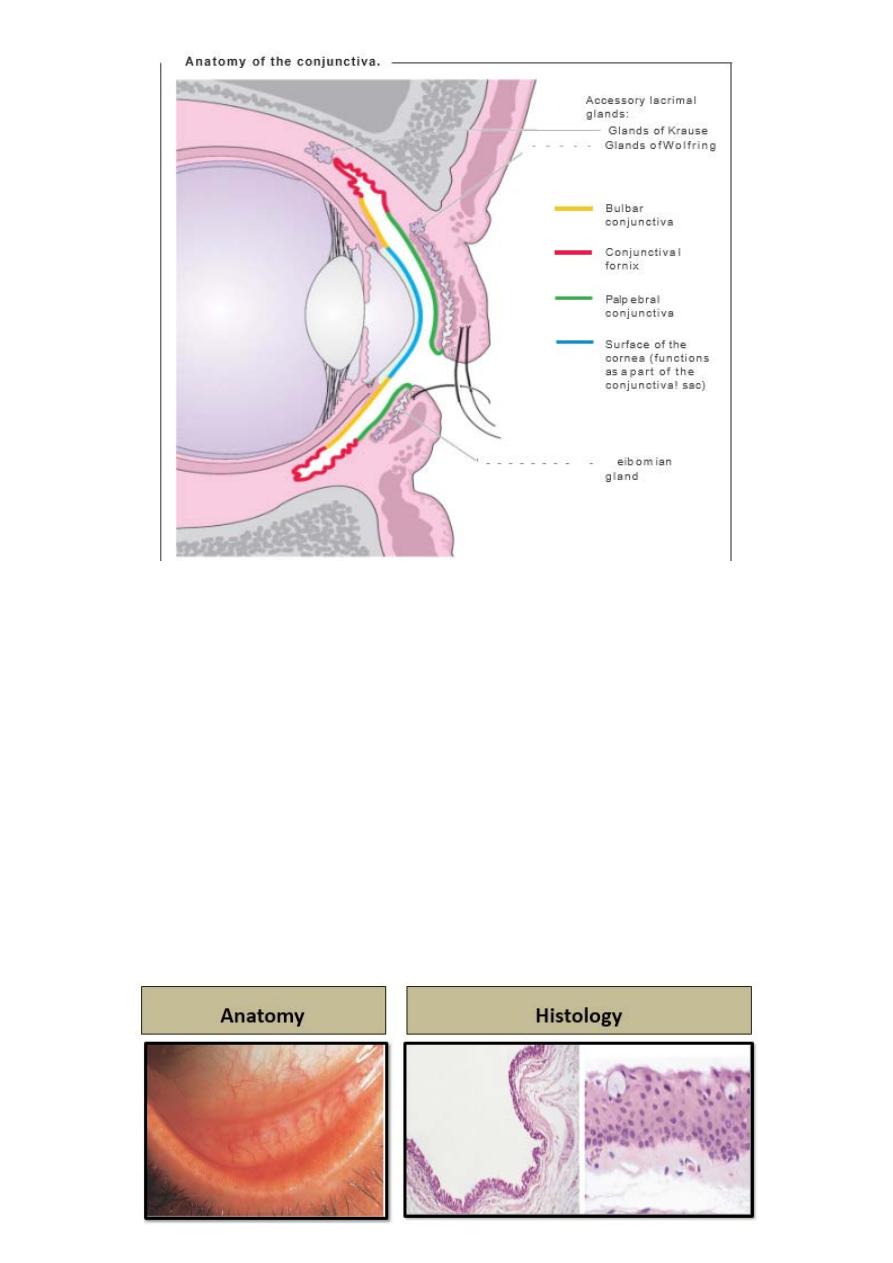
Anatomy:
The conjunctiva is a transparent mucous membrane lining the
inner surface of the eyelids and the surface of the globe as far as
the limbus.
It is richly vascular; there is a dense lymphatic network, with
drainage to pre-auricular and submandibular lymph nodes.
Anatomically, it is sub-divided into the following:
1- The palpebral conjunctiva:
Starts at the muco-cutaneous junction of the lid margin and it is
firmly adherent to the posterior tarsal plate.
2- The forniceal conjunctiva: is loose and redundant and may be
thrown into folds.
3- The bulbar conjunctiva:
Covers the anterior sclera and is continuous with corneal
epithelium at the limbus.
2
Normal conjunctiva
Histology:
1- The epithelium: is non-keratinized and around five cell layers
deep. Basal cuboidal cells evolve into flattened polyhedral cells
before they shed from the surface. Goblet cells are located
within the epithelium and densest inferonasally.
2- The stroma (substantia propria): consist of richly vascularized
loose connective tissue.
The accessory lacrimal glands of Krause and Wolfring are
located deep within the stroma, mucous from the goblet cells
and secretions from accessory lacrimal glands are essential
components of tear film.
3- conjunctiva-associated lymphoid tissue (CALT): is critical in
the initiation and regulation of ocular immune response.
3
Signs of conjunctival disease:
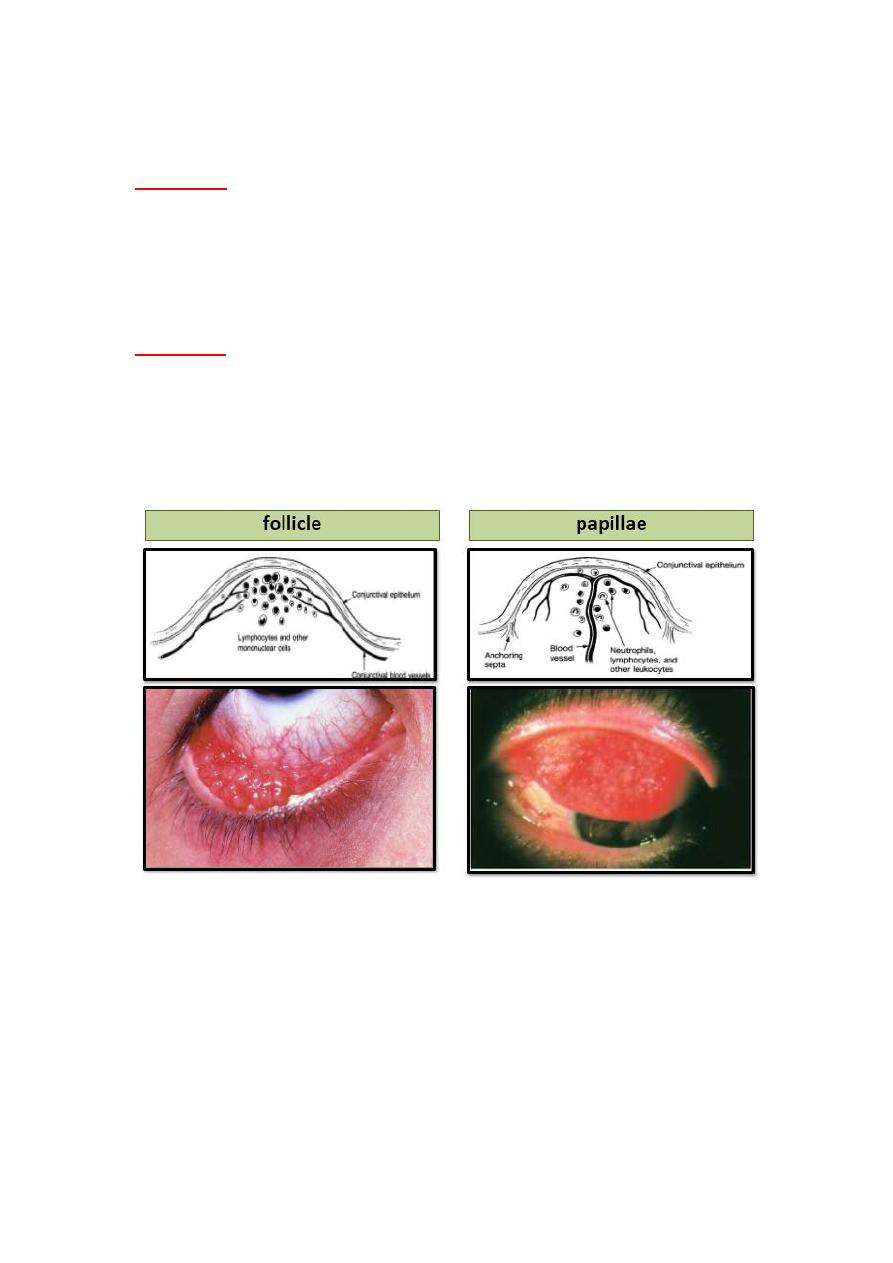
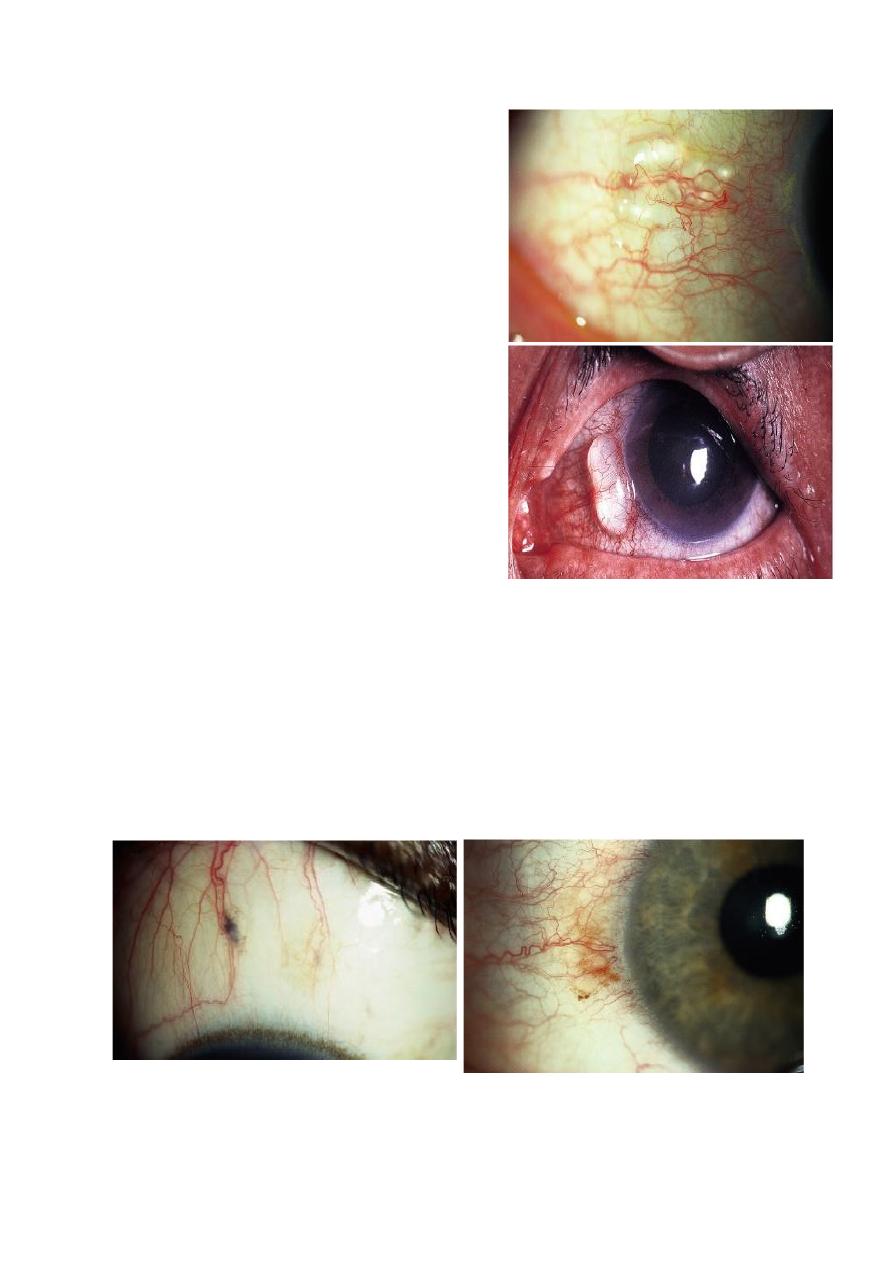
Follicle and papillae:
Follicles:
Signs:
multiple, discrete, slightly elevated lesions. Blood vessels
run around or across rather than within the lesion.
Histology: Subepithelial lymphoid germinal center with central
immature lymphocytes and mature cells peripherally.
Causes:
include viral and chlamydial conjunctivitis.
Papillae:
vascular core is present (unlike follicles).
Histology:
folds of hyper- plastic conjunctival epithelium with
fibro-vascular core and Subepithelial stromal infiltration .
Causes:
bacterial conjunctivitis, allergic conjunctivitis, chronic
marginal blepharitis, contact lens wear and floppy eyelid
syndrome.
Membranes:
Psedomembrane consist of coagulated exudates adherent to the
inflamed conjunctival epithelium. They can be peeled easily
leaving underlying epithelium intact.
True membrane: involve the superficial layers of the
conjunctival epithelium, attempt of removal leads to tearing.
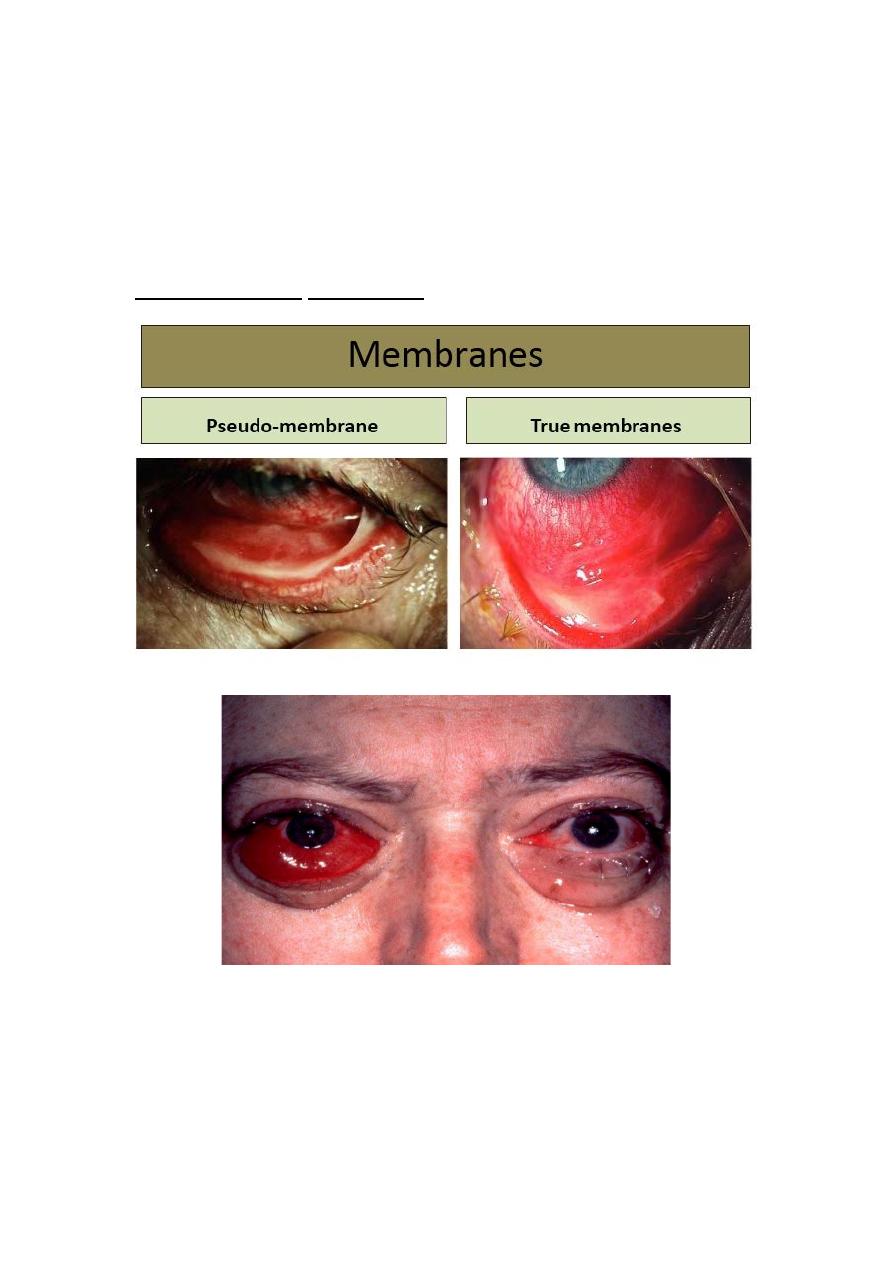
4
Causes:
1- Sever adenoviral conjunctivitis.
2- Gonococcal conjunctivitis.
3-Acute Steven-Johnson syndrome.
4- Bacterial infection (Streptococcus species and
Corynebacterium diphtheriae).
Conjunctival edema (chemosis):
Clinical features of conjunctival inflammation
• Discharge:
1 watery: viral and acute allergic conjunctivitis.
2 mucoid: chronic allergic conjunctivitis and dry eye.
3 mucopurulant: chlamydial and bacterial infection.
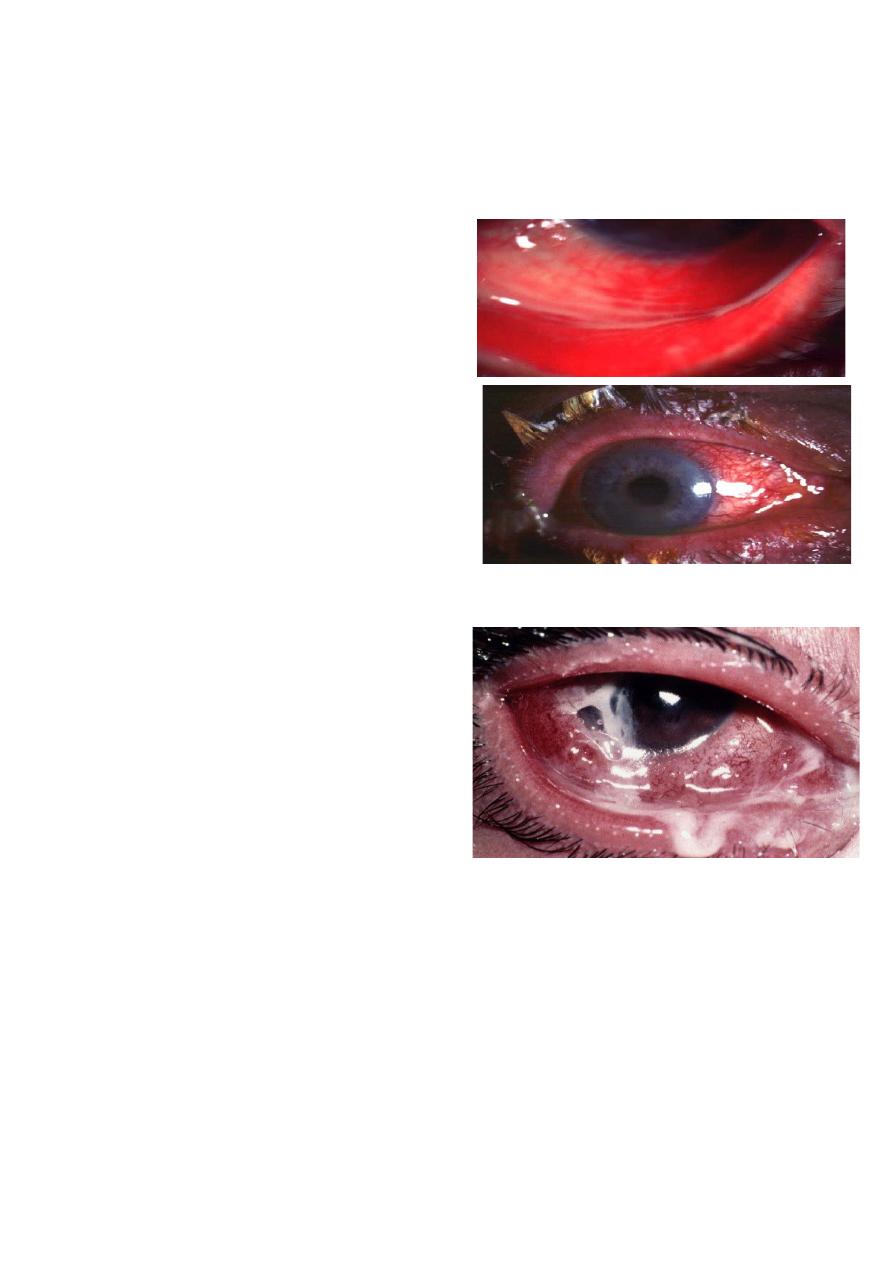
5
4 sever purulent: gonococcal infection.
Infectious and inflammatory conjunctivitis:
Bacterial conjunctivitis:
Acute bacterial conjunctivitis
Common, self-limiting caused by
direct eye contact with infected
secretions
Most common pathogens:
• S.pneumoniae.
• S.aureus.
• H.influenzae.
• Moraxella catarrhalis.
Minority caused by sexually
transmitted organism Nisseria
gonorrhoae.
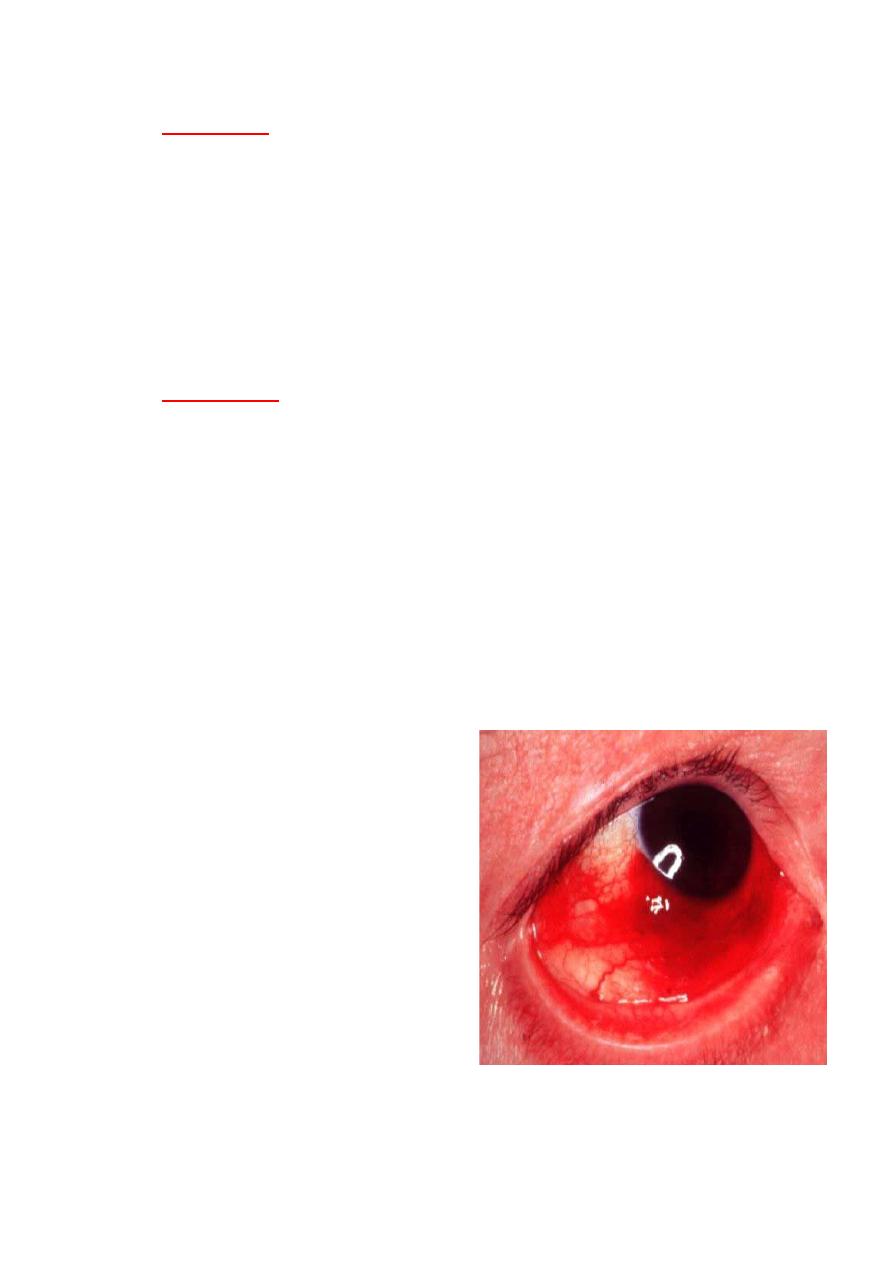
Gonococcal conjunctivitis:
• Needs systemic antibiotics
with frequent topical
antibiotics.
• Gonococci have an ability
to penetrate intact corneal
epithelium.
• Treatment of sexual
partner.
Viral conjunctivitis:
Adenoviral conjunctivitis:
Adenovirus is non-enveloped double-stranded DNA virus,
transmission by contact with respiratory or ocular secretions,
including via fomites such as contaminated towels.
Presentation:
1- Non-specific acute follicular conjunctivitis accompanied with
mild systemic symptoms like sore throat.
6
2- Pharyngo-conjunctival fever (PCF) caused by adenovirus 3, 4
and 7 spread by droplets within families with upper respiratory
tract infection.
3- Epidemic keratoconjunctivitis (EKC) caused by adenovirus 8,
19 and 37; are the most sever type and they are associated with
keratitis in 80% of cases.
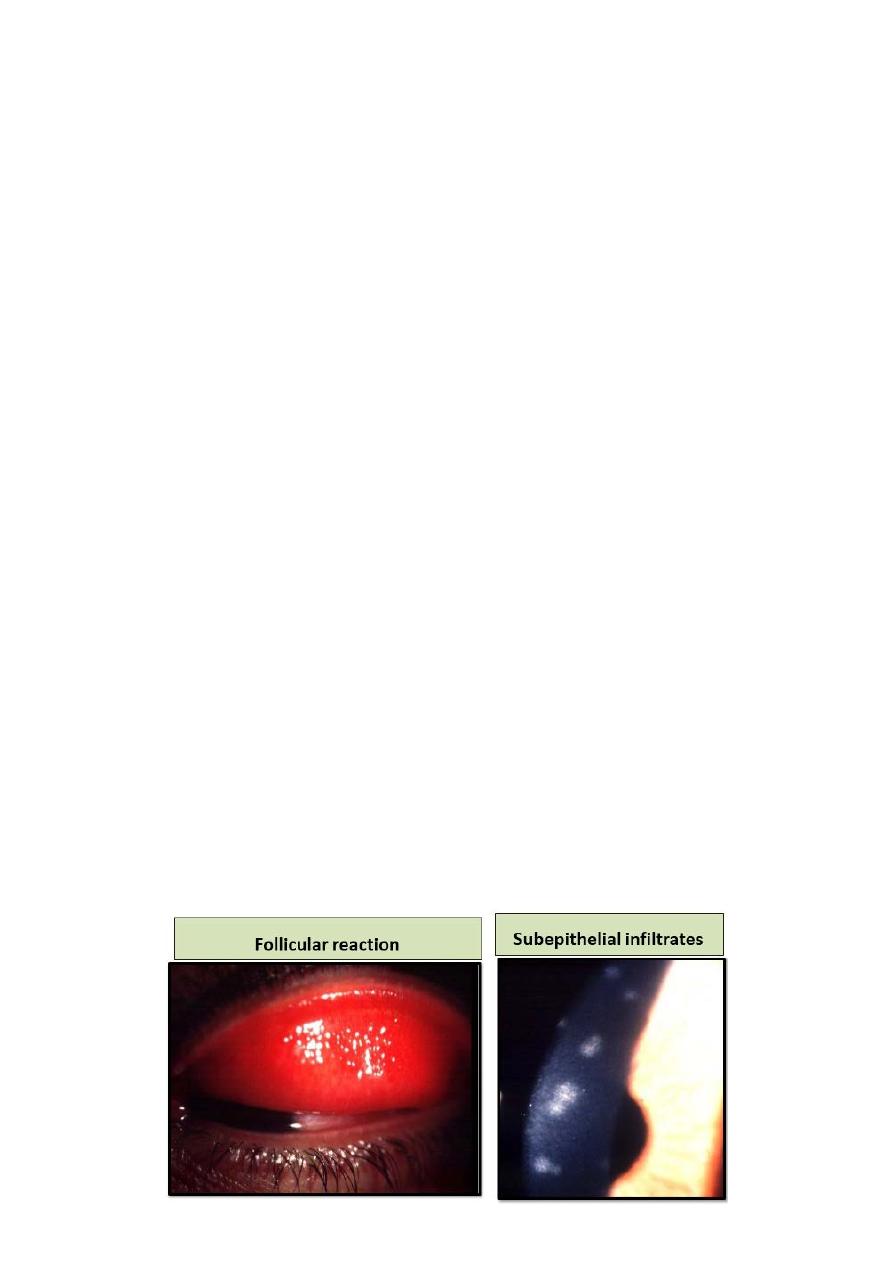
Signs:
1- Eyelid edema and tender preauricular Lymphadenopathy.
2- Prominent conjunctival hyperemia and follicles.
There may be chemosis, conjunctival hemorrhages and pseudo
membrane.
Keratitis:
punctate epithelial keratitis may develop within 7-10 days of
onset of symptoms and resolve within 2 weeks, focal white
Subepithelial infiltrates may develop as immune response to
virus and may persist or recur over months or years.
Investigation: generally unnecessary, but if in doubt or not
resolved Giemsa stain, viral culture may be required.
Treatment:
1- Reduction of transmission risk: by meticulous hand hygiene,
avoiding eye rubbing and towel sharing
Disinfection of instruments and clinical surfaces after examining
infected patients by povidone iodine
Topical steroids: such as prednisolone may be required for
membranous conjunctivitis
Artificial tears
Discontinue contact lens wear until symptom resolution.
Removal of pseudomemrane.
Topical antibiotics if secondary bacterial infection is suspected.
7
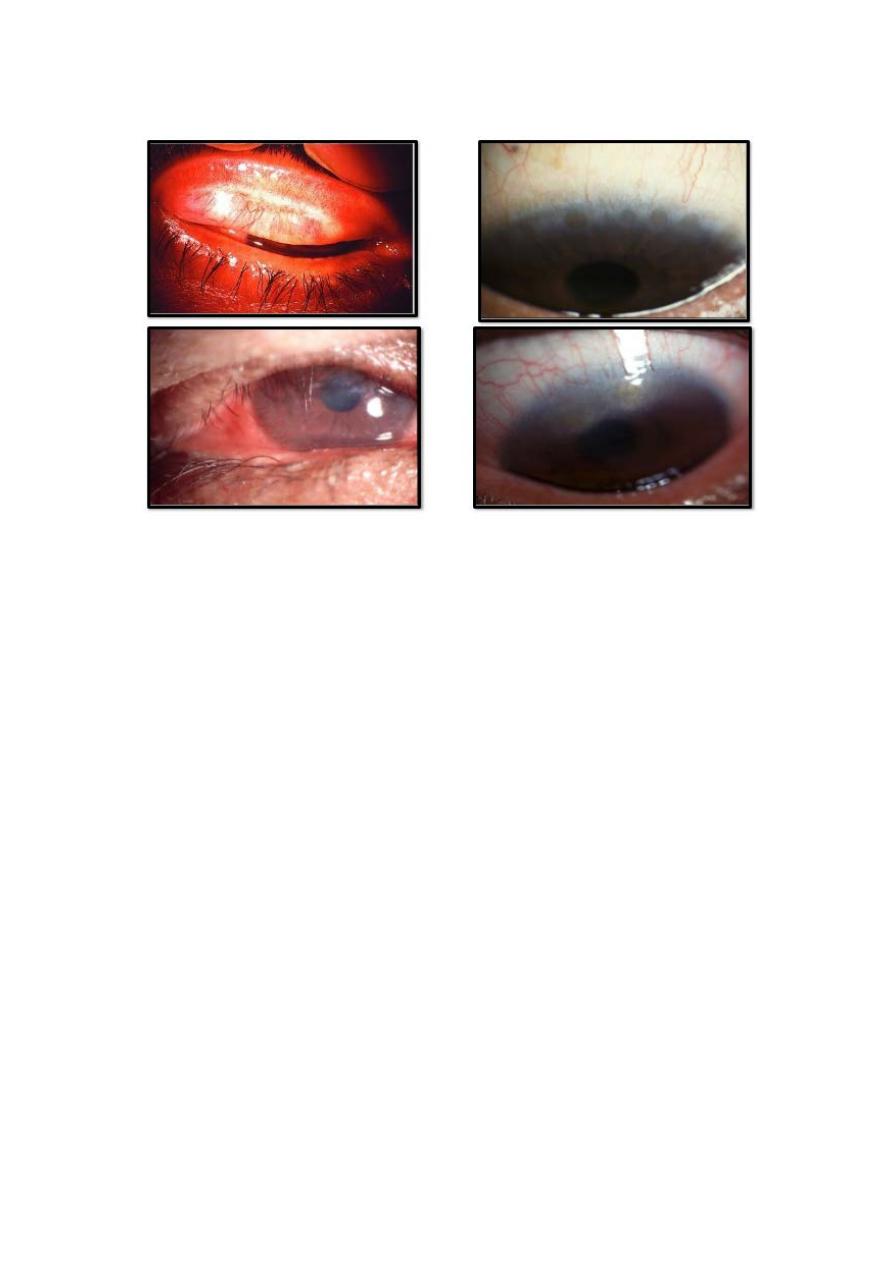
Molluscum contagiosum conjunctivitis:
Pathogenesis:
Molluscum contagiosum is a skin infection caused by human
specific double-stranded DNA poxvirus, which typically affect
healthy children between 2-4 years. Transmission is by contact.
The eyelash line should be examined carefully in patients with
chronic conjunctivitis.
Diagnosis:
Presentation: unilateral chronic ocular irritation.
Signs:
A pale, waxy, umbilicated nodule on the lid margin associated
with follicular conjunctivitis. With mild mucoid discharge.
Treatment:
The lesions are self-limiting in immunocompetant patient.
Removal is often necessary to address secondary conjunctivitis
or for cosmetic reason.
8
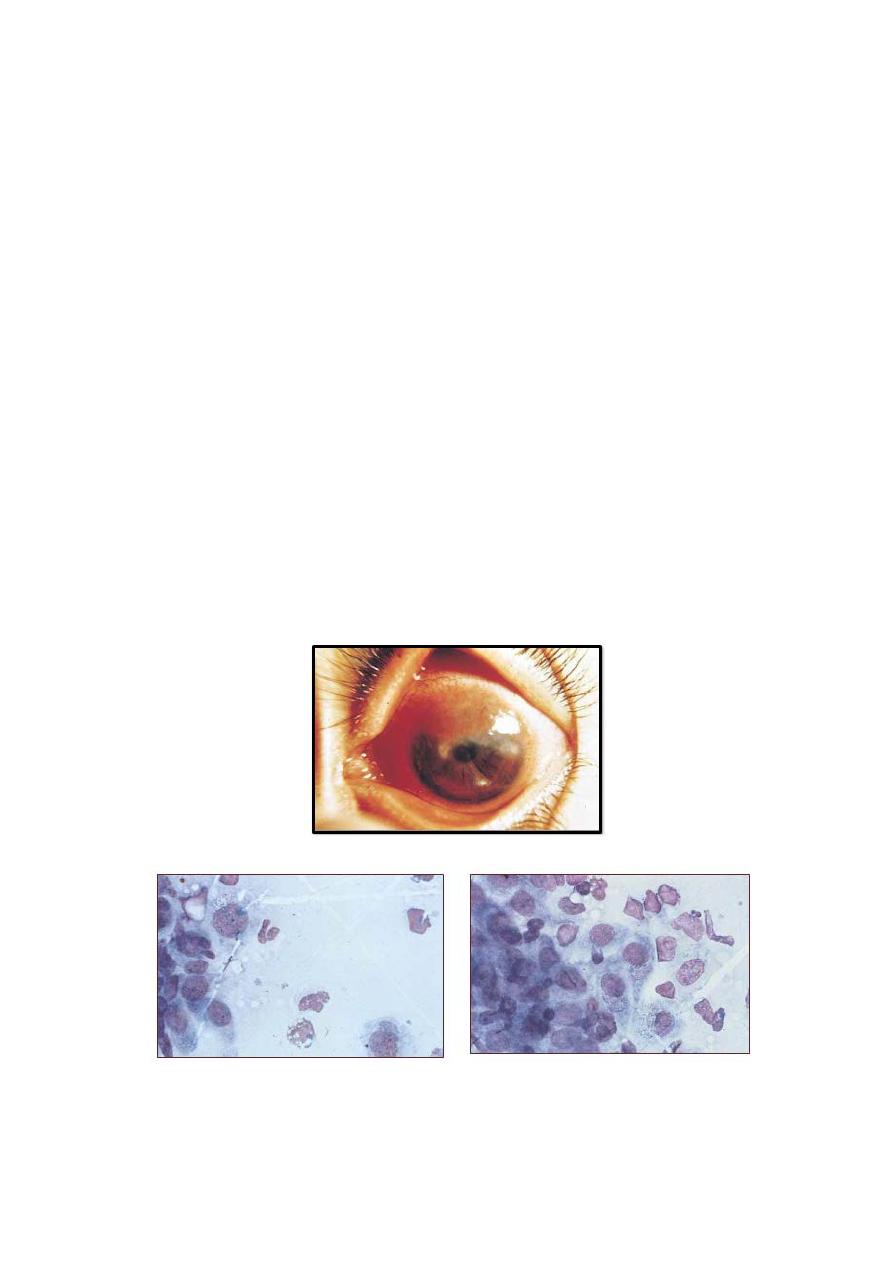
Trachoma:
Pathogenesis:
Trachoma is the leading cause of preventable irreversible
blindness in the world; it is related to the poverty, overcrowding
and poor hygiene.
A family is the most important re-infection reservoir and
consequently young children are mostly vulnerable.
A fly is most important vector, but may be direct transmission
from eye or nasal discharges.
Trachoma is associated principally with infection with sero
types A, B, Ba and C of Chlamydia trachomatis, but the sero
types D-K conventionally associated with adult inclusion
conjunctivitis.
Diagnosis:
1- Active trachoma: most common in pre-school children,
characterized by:
A- Mixed follicular/papillary conjunctivitis associated with
mucopurulant discharge.
B- Superior epithelial keratitis and pannus formation.
2- Cicatricial trachoma: most prevalent in middle age.
A- Linear or satellite scar in mild case, or confluent (Arlt line)
scar in sever case.
Upper tarsal conjunctiva mostly affected.
9
Superior limbal follicles may resolve to leave a raw of shallow
depression (Herbert pits).Trichiasis, Distichiasis, corneal
vascularization and cicatricial entropion.
Sever corneal opacification, dry eye caused by destruction of
goblet cells.
Diagnosis:
made on clinical ground.
Management:
SAFE strategy adopted by WHO:
Antibiotics for active disease (single dose of azithromycin 20
mg/kg up to 1g) is the treatment of choice.
Facial cleanliness is critical preventive measure.
Environmental improvement such as access to adequate water
and sanitation and flies control.
Surgery for entropion and Trichiasis.
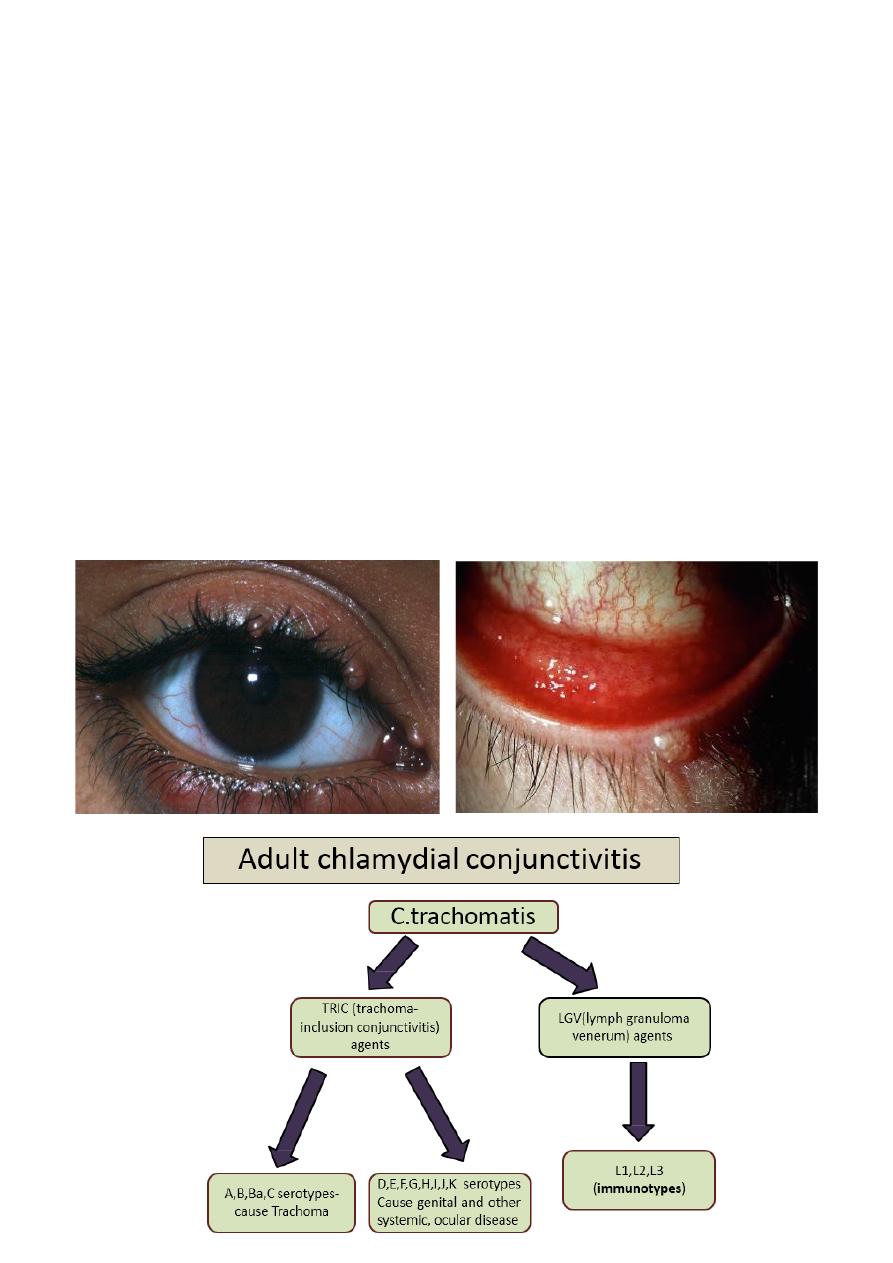
Adult chlamydial conjunctivitis:
Chlamydia trachomatis cannot replicate extracellularly and
depend on host cells. Adult chlamydial (inclusion) conjunctivitis
is an oculogenital infection usually caused by sero types D-k of
C. trachomatis, and affects 5-20% of sexually active young
adults in western countries.
Diagnosis:
Symptoms are consisting of subacute onset of unilateral or
bilateral redness, watering and discharge, untreated, the
conjunctivitis becomes chronic,
Signs:
1- Mucopurulant discharge.
2- Large follicles in inferior fornix.
10
3- Tender preauricular Lymphadenopathy.
4- Superficial punctate keratitis is common.
5- Chronic cases have less prominent follicles and may develop
mild conjunctival scarring and superficial corneal pannus.
Investigations:
1- Tarsal conjunctival scraping for:
A- Nucleic acid amplification using PCR.
B- Giemsa staining for basophilic intra-cytoplasmic bodies
C- Direct immunofluorescence
D- McCoy cell culture is highly specific
Treatment:
1- Referral to genitourinary specialist
2- Systemic: azithromycin 1g repeated after 1 week
(erythromycin, amoxicillin, and ciprofloxacin) are alternatives.
3- Topical antibiotics such as erythromycin or tetracycline
ointment.
4- Reduction of transmission risk by abstinence of sexual
contact
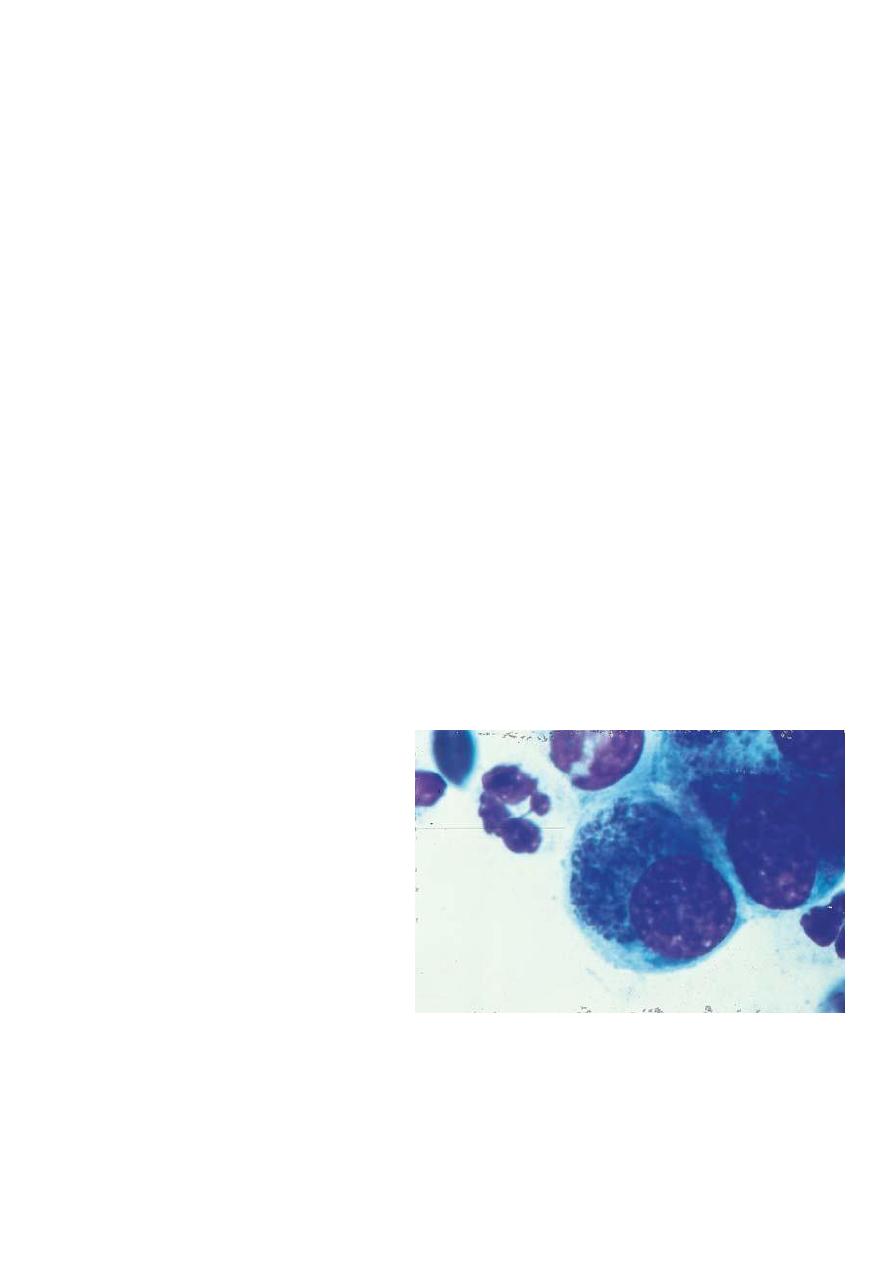
Chlamydial conjunctivitis typical basophilic
intracytoplasmic inclusion bodies:
Definition:
conjunctival
inflammation developing
within the first month of
life.
Causes according timing
of onset:
1- Chemical irritation: first
few days.
2-gonococcal: first week.
3- Staphylococcal and
other bacteria: end of first week.
Herpes simplex: 1-2 weeks.
Chlamydial 1-3 weeks.
11
Investigation:
conjunctival scraping applied to a glass slide for Gram and
Giemsa staining: multinucleated giant cells may be present on
gram stain in HSV infection.
Treatment:
A single instillation of povidone iodine 2.5% solution is
effective against common pathogens.
Erythromycin or tetracycline is also used.
Silver nitrate 1% solution still utilized were gonococcal
infection common.
Chemical conjunctivitis does not require treatment
Mild-moderate conjunctivitis needs broad-spectrum antibiotics.
Sever conjunctivitis (like gonococcal) requires hospital
admission and treated systemically with a third generation
cephalosporin. Co-treatment for Chlamydia is prudent.
Herpes simplex infection should always be regarded as systemic
condition and treated with high dose intravenous acyclovir,
early diagnosis and treatment of encephalitis may be lifesaving
or prevent serious neurological disability.
12
Neonatal conjunctivitis:
(ophthalmia neonatorum)
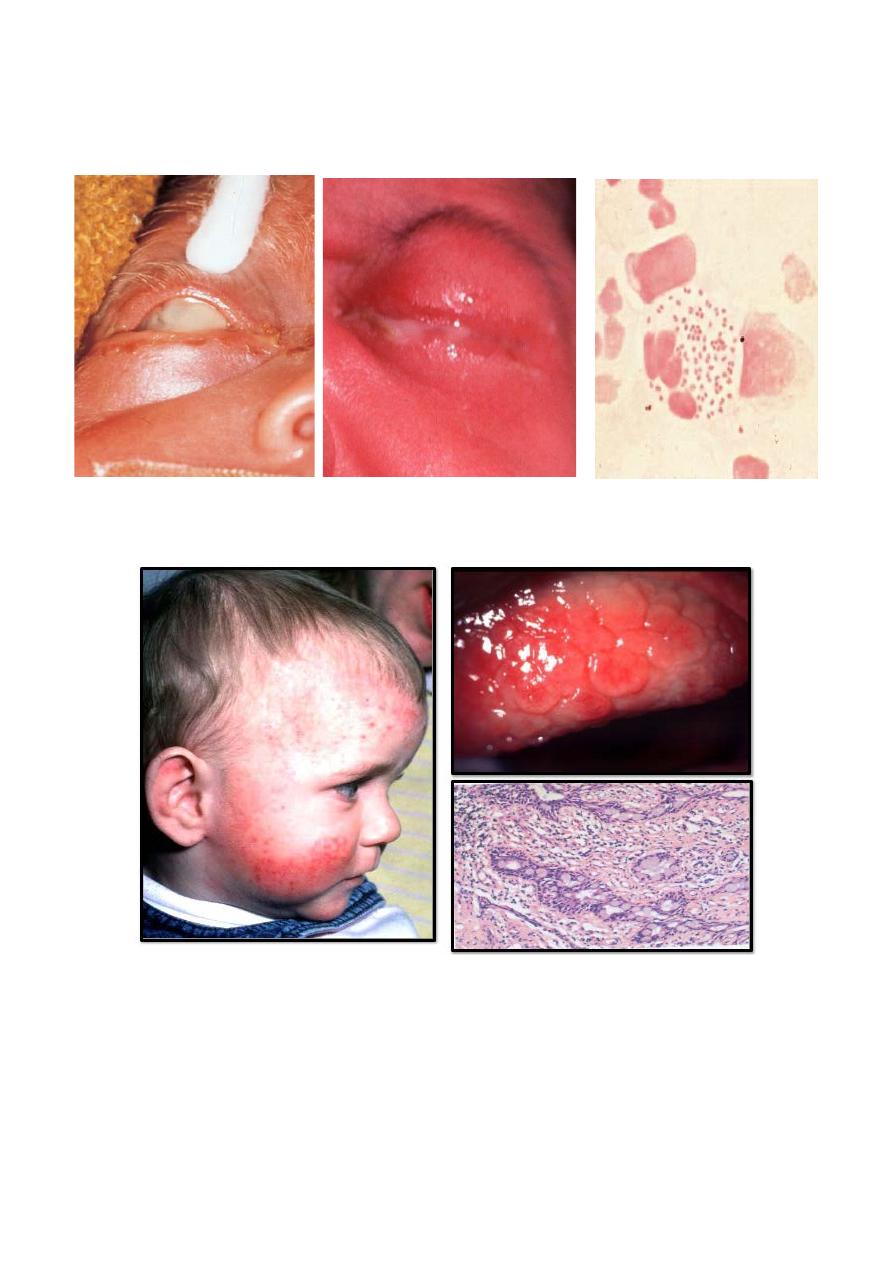
Vernal keratoconjunctivitis (VKC):
Pathogenesis:
Recurrent bilateral disorder, IgE and cell-mediated immunity
play a role.
Affects mainly boys from age 5 years onwards.
Common in warm dry climate (especially Middle East).
Two third of cases have family history of atopy.
13
VCK often occurs on seasonal basis with peak incidence over
late spring and summer.
Diagnosis:
Intense itching, lacrimation, photophobia, foreign body
sensation, burning and thick mucoid discharge.
Vernal keratoconjunctivitis typically affects children in their
first 2 decades and the majority have a good prognosis, because
the disease usually resolves spontaneously after puberty.
However, potentially sight-threatening corneal changes can
occur (i.e., corneal plaques and ulcers, corneal stem cell
deficiency, keratoconus).
Atopic keratoconjunctivitis (AKC):
AKC is a rare, developed in adulthood (between 30-50 years)
following long a long history of eczema. Asthma is common in
these patients. It is chronic unremitting unlike seasonal variation
in VKC it tends to be perennial.
Symptoms:
similar to AKC together with skin changes of
erythema, dryness fissuring and scratches due to intense itching
associated with chronic staph. Blepharitis and madarosis.
Herltoghe sign is characterized by absence of lateral portion of
eyebrows
Conjunctival involvement tends to be inferior while in VKC
more superior involvement, together with Cicatricial changes
and possible symblepharon formation.
14
There is keratopathy manifested as punctate epithelial erosions,
plaque formation and peripheral vascularization
There is associated shield- like anterior or posterior subscapular
cataracts.
Retinal detachment is more common than general population.
Treatment of VKC and AKC:
• A- local treatment:
1 mast cell stabilizers:
2 antihistamines.
3 combined preparation
4 steroids (flurometholone, rimexolone, prednisolone).
5 immune modulation: cyclosporine. 6- tacrolimus.
• Systemic treatment:
1 antihistamine.
2 antibiotics( doxcycycline). 3-imunosuppressive agents.
Conjunctival degenerations:
1 Pingueculum.
2 Pterygium.
3 Concretions.
4 Conjunctivochalasis.
5 Retention (epithelial inclusion) cyst.
Pingueculum:
• Common, innocuous ,
bilateral asymmetrical
‘elastotic’ degeneration
of collagen fibers of
conjunctival stroma.
•
Etiology:
actinic
damage
•
Signs:
Yellow-white
mound on bulbar
conjunctiva adjacent to limbus located at the nasal than
temporal limbus.
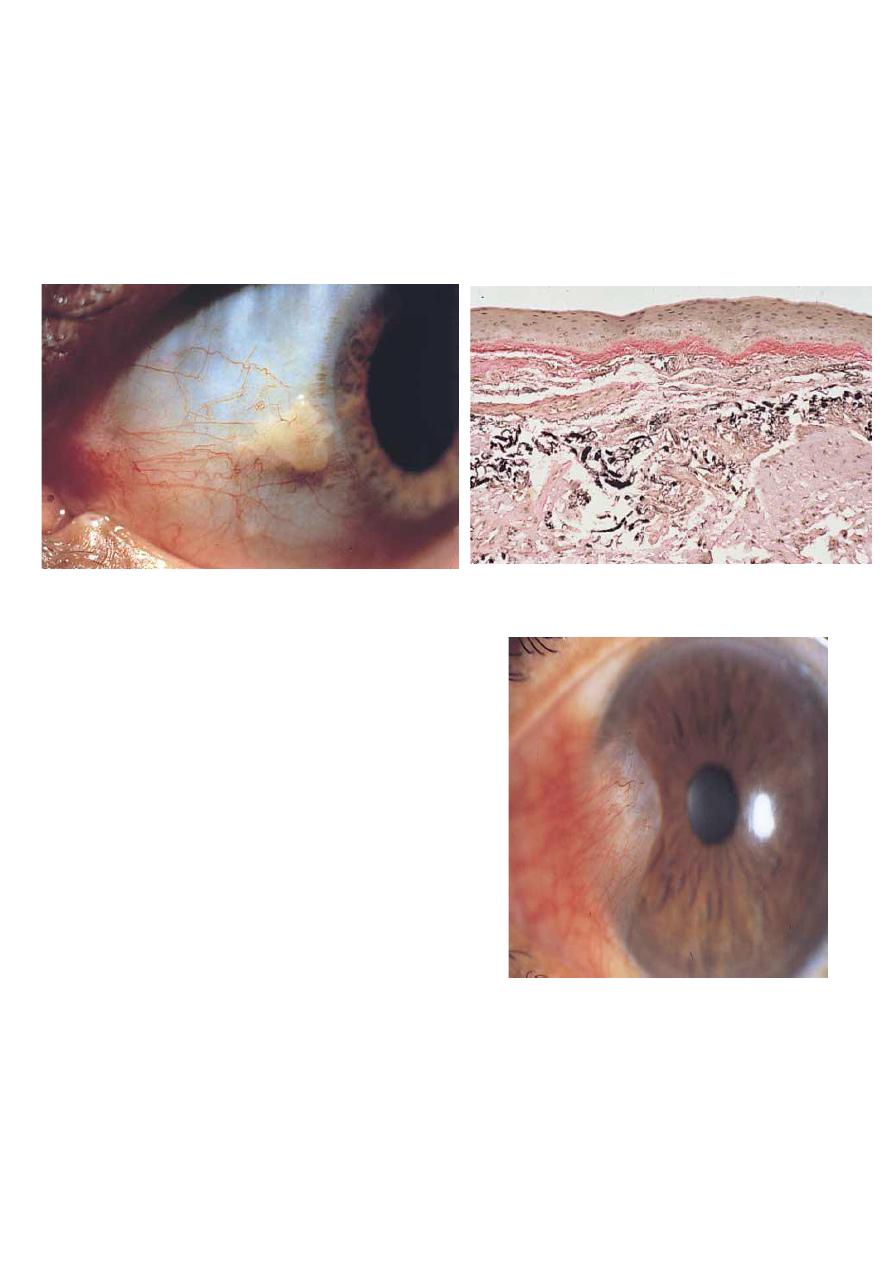
15
•
Treatment:
usually unnecessary because growth is very
slow or absent, occasionally, a pingueculum may become
inflamed (pingueculitis) and require a short course of a
weak steroid such as flurometholone.
Histopathology:
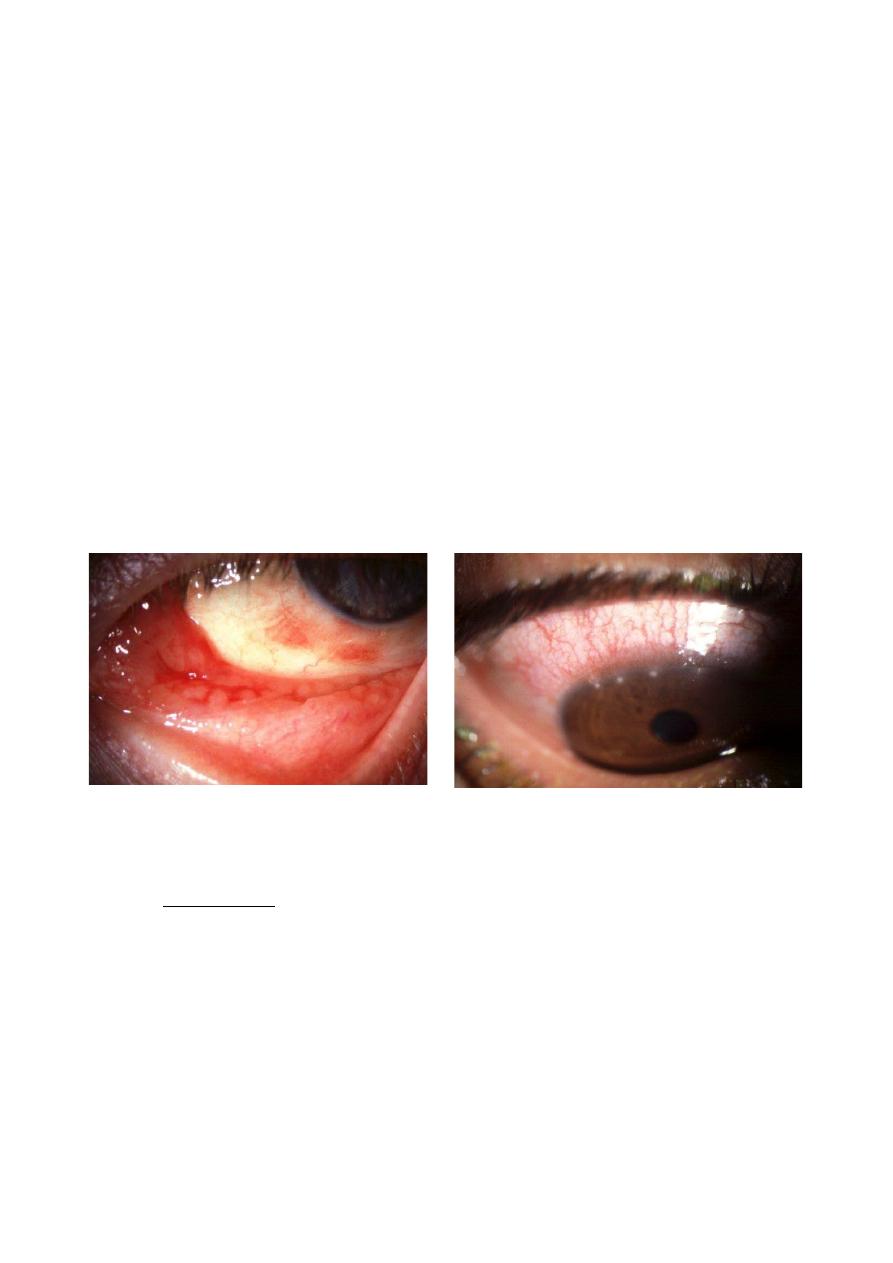
Pterygium:
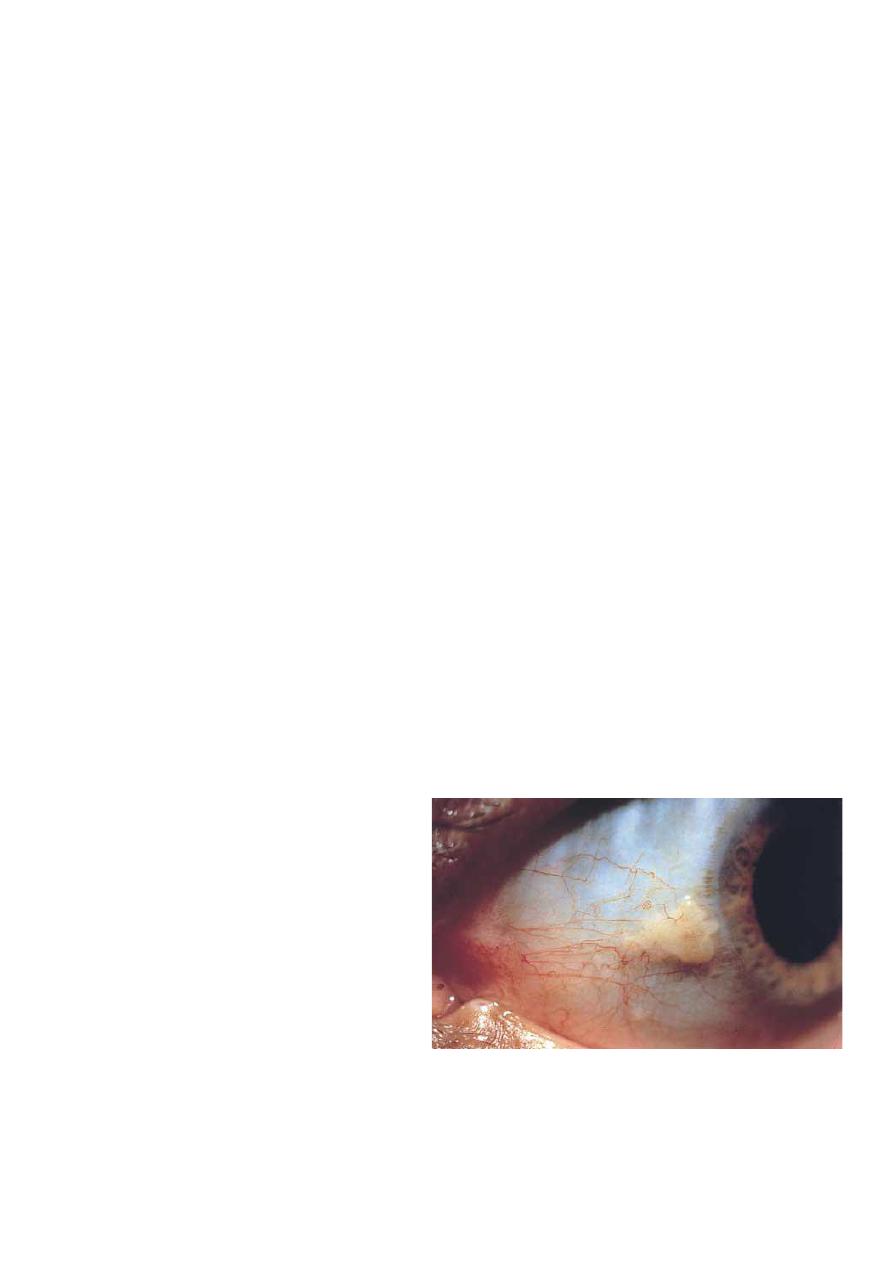
Definition:
• Triangular fibrovascular
Subepithelial ingrowth of
degenerative bulbar
conjunctival tissue over the
limbus onto the cornea.
• It develops in patients who
have been living in hot
climates and represent a
response to UV exposure .
•
Histology:
elastotic
degeneration.
Clinical features:
Symptoms:
Many small lesions are asymptomatic.
Irritation and grittiness caused by dellen effect at the advancing
edge due to interference with pre-corneal tear film.
16
Interference with vision by obscuring the visual axis or inducing
astigmatism.
Intermittent inflammation similar to pingueculitis
Cosmesis may be a significant problem.
Treatment:
1- Medical treatment: tear substitutes, topical steroids for
inflammation, wearing sunglasses to reduce ultraviolet
exposure.
Surgical techniques:
Simple excision.
Simple conjunctival flap.
Conjunctival auto-grafting with or without adjunctive treatment
with mitomycin C.
Amniotic membrane patch grafting reserved for aggressive
lesions Occasionally peripheral lamellar keratoplasty is required
for deep lesions.
Histopathology:
17
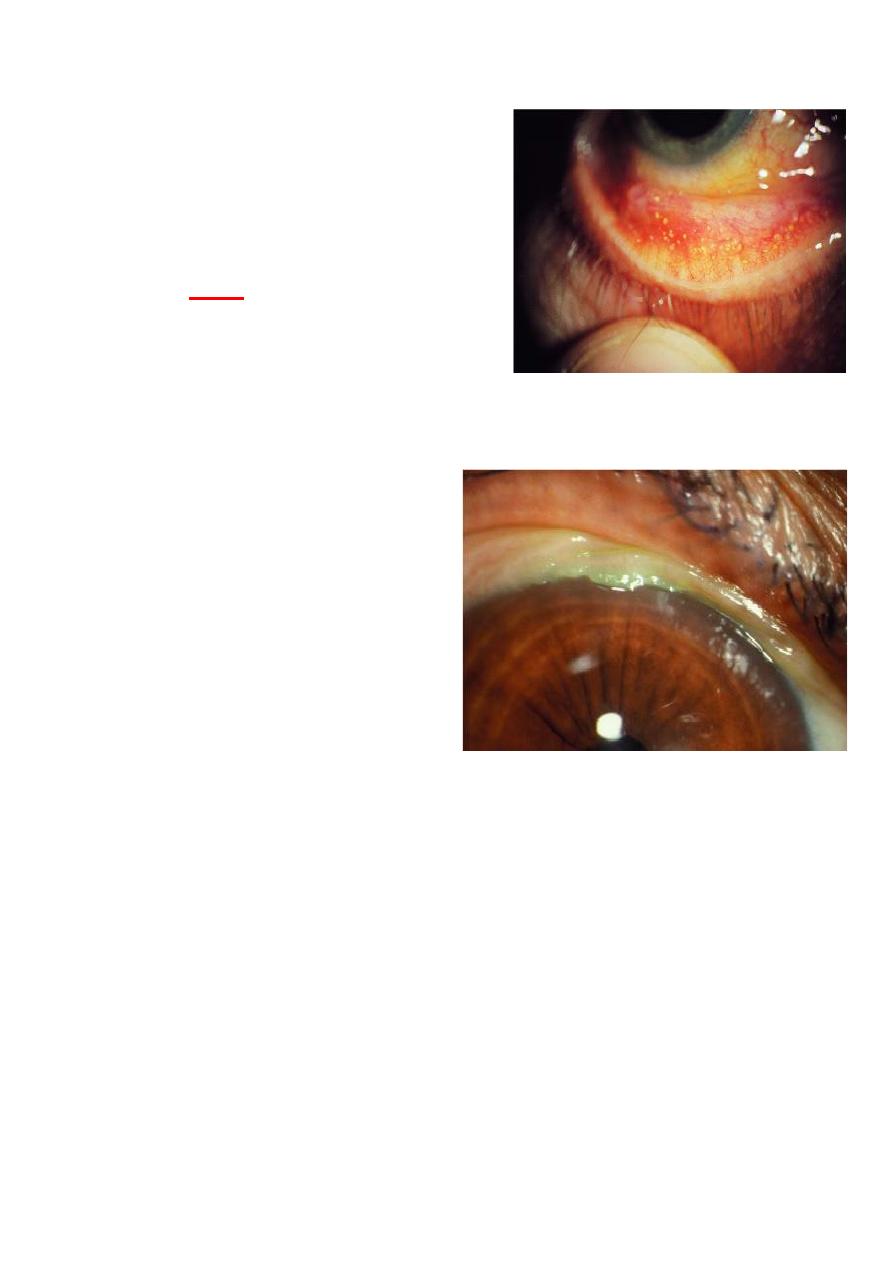
Concretions:
Common, associated with
aging.
Associated with chronic
conjunctival inflammation, e.g.
trachoma.
Signs:
multiple, tiny cysts
containing yellowish-white
deposits of epithelial debris
including keratin, located
suepithelially in inferior tarsal conjunctiva.
Conjunctivochalasis:
• Normal aging changes,
exacerbated by posterior
lid margin disease.
•
Symptoms:
watering of
the eye by mechanical
obstruction of inferior
punctum.
•
Signs:
a fold of redundant
conjunctiva interposed
between lower lid and
globe.
• Treatment:
1- Topical lubricants and treatment of blepharitis.
2- Short course of topical steroids.
3- Conjunctival excision in severe cases.
18
Retention (epithelial inclusion)
cyst:
•
Signs:
thin-walled lesion
containing clear and
occasionally turbid fluid.
• The cyst dose not usually
cause discomfort but may be a
mid cosmetic blemish
•
Treatment:
simple puncture
with a needle
Pigmented conjunctival lesions:
Epithelial melanosis:
Presentation:
• During the first few years of life.
•
Signs:
flat, patchy, brownish pigmentation scattered
throughout the conjunctiva.
• The lesions may become more intense around perforating
branches of anterior ciliary vessels.
19
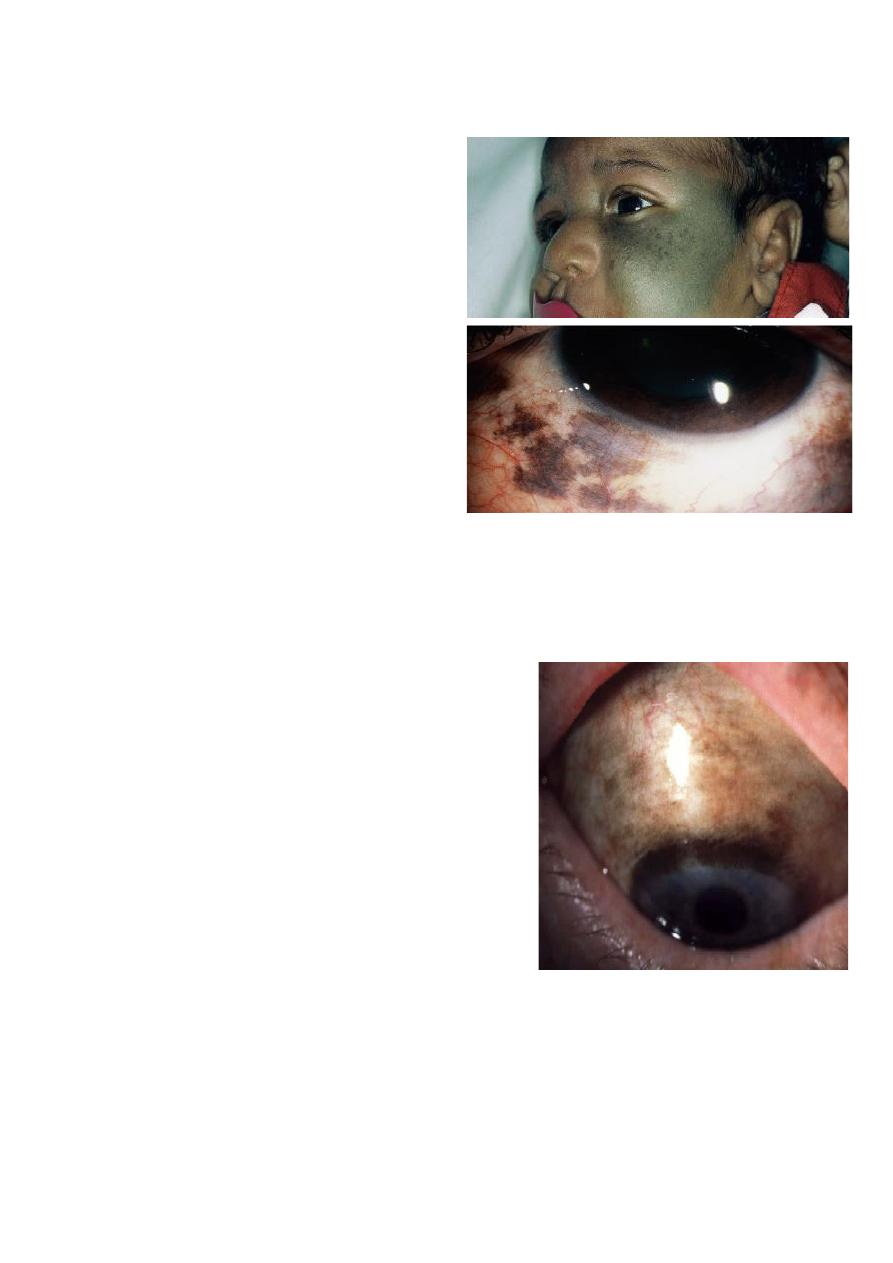
Congenital ocular melanosis:
Classification:
1- ocular melanocytosis:
involves only the eye.
2-
dermal melanocytosis:
involves only the skin .
3-
oculodermal melanocytosis:
(nevus of Ota) which involves
both skin and eye.
Signs:
multifocal slate-gray
pigmentation in the episclera.
Nevus of Ota: deep bluish
hyperpigmentation of facial
skin, most frequently in the
distribution of trigeminal nerve.
Associations:
iris hyperchromia, iris mammilliations, fundus
and trabecular hyperpigmentation.
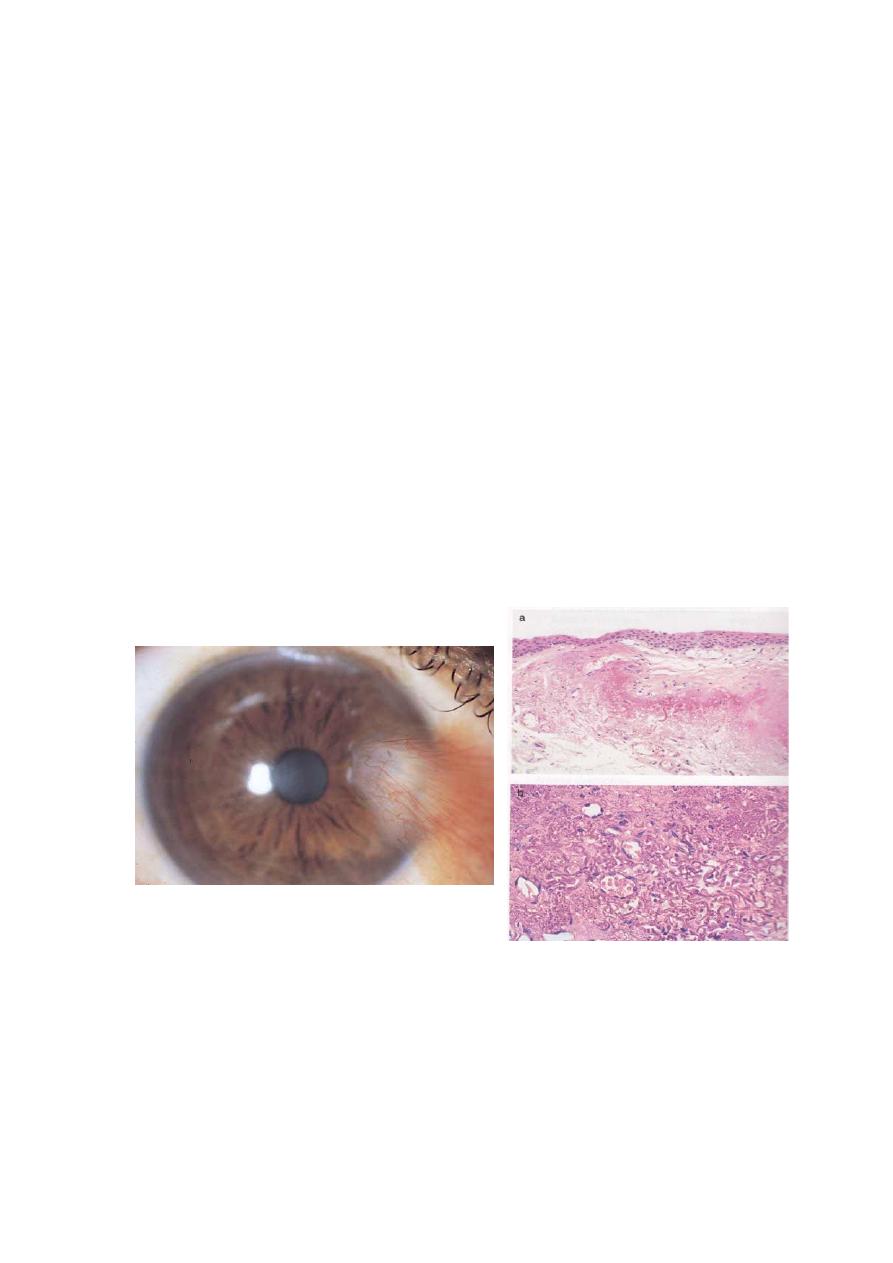
Primary acquired melanosis (PAM):
• A rare condition presenting in old
age with unilateral or multifocal
slowly growing patches of
intraepithelial pigmentation.
• Flat, brown pigmentation which
involves any part of the
conjunctiva.
Classification:
1.
PAM without melanocytic
atypia:
benign and require no
treatment.
2.
PAM with melanocytic atypia:
has potential of
developing infiltrating malignancy within 5 years, if
small can be treated with excision, but if large and
cannot be excised treated with cryotherapy or topical
application of mitomycin c.
20
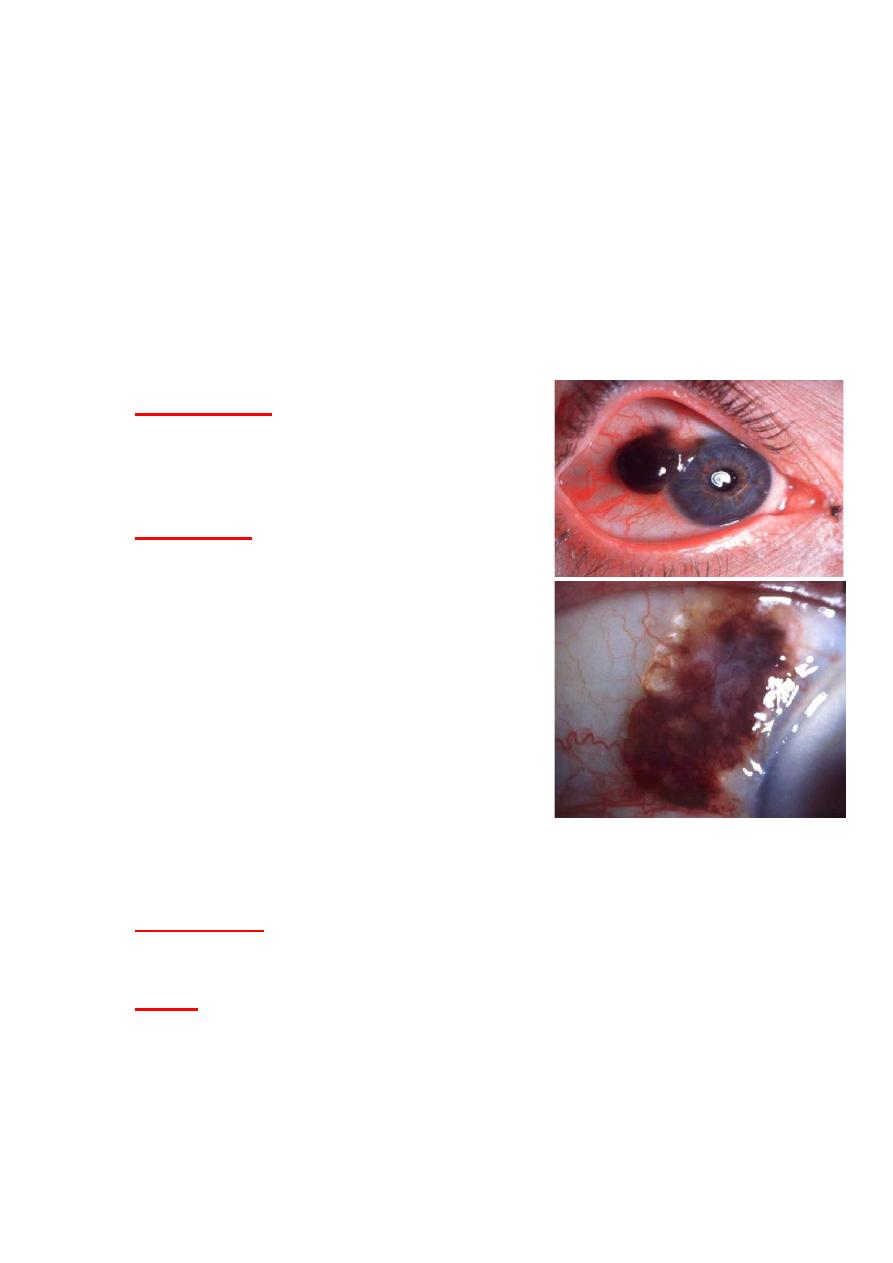
Melanoma:
A rare tumor accounting for 2% of all ocular malignancies.
Most frequently arises
1- within PAM with atypia, as a nodular lesion.
2- May arise from pre-existing nevus
3- Rarely, de novo, usually at the limbus.
Presentation:
in 6
th
decade of life.
A black, gray nodule containing
dilated feeder vessels.
Treatment:
1 circumscribed melanoma: excision
with safe
ty margin and cryotherapy
application+ adjunctive
radiotherapy
2 diffuse melanoma: excision of
localized lesion and cryotherapy or
mitomycin for diffuse component.
Conjunctival nevus:
Presentation:
during first 2 decades of life with irritation orb
pigmentation.
Signs:
Solitary, sharply demarcated, flat or slightly raised
pigmented bulbar lesion.
Cystic spaces within the nevus are frequent.
21
Around puberty the nevus
enlarged and more pigmented.
In children and adolescents,
nevus may appears more
inflamed, with dilated feeder
vessels.
Treatment:
Excision for
cosmetic reason.
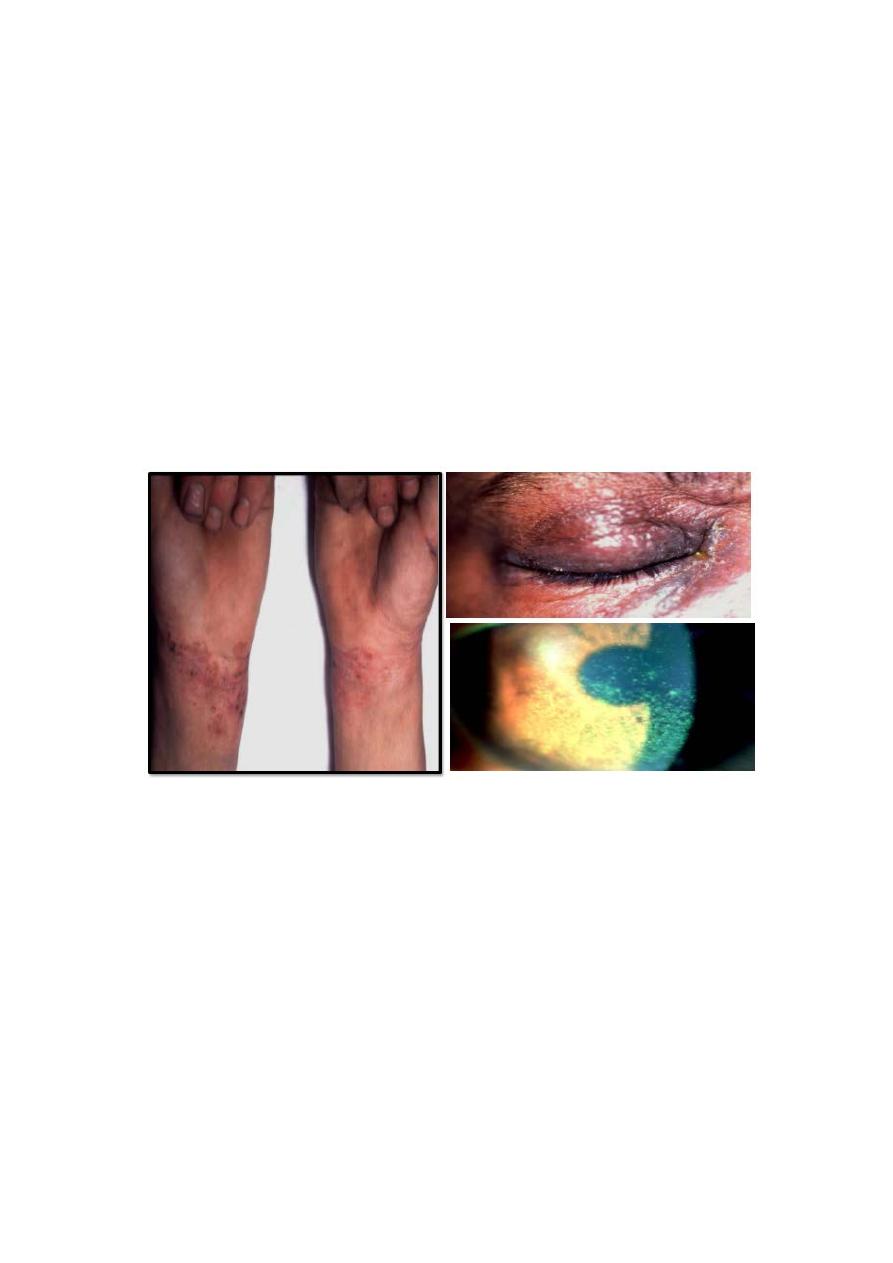
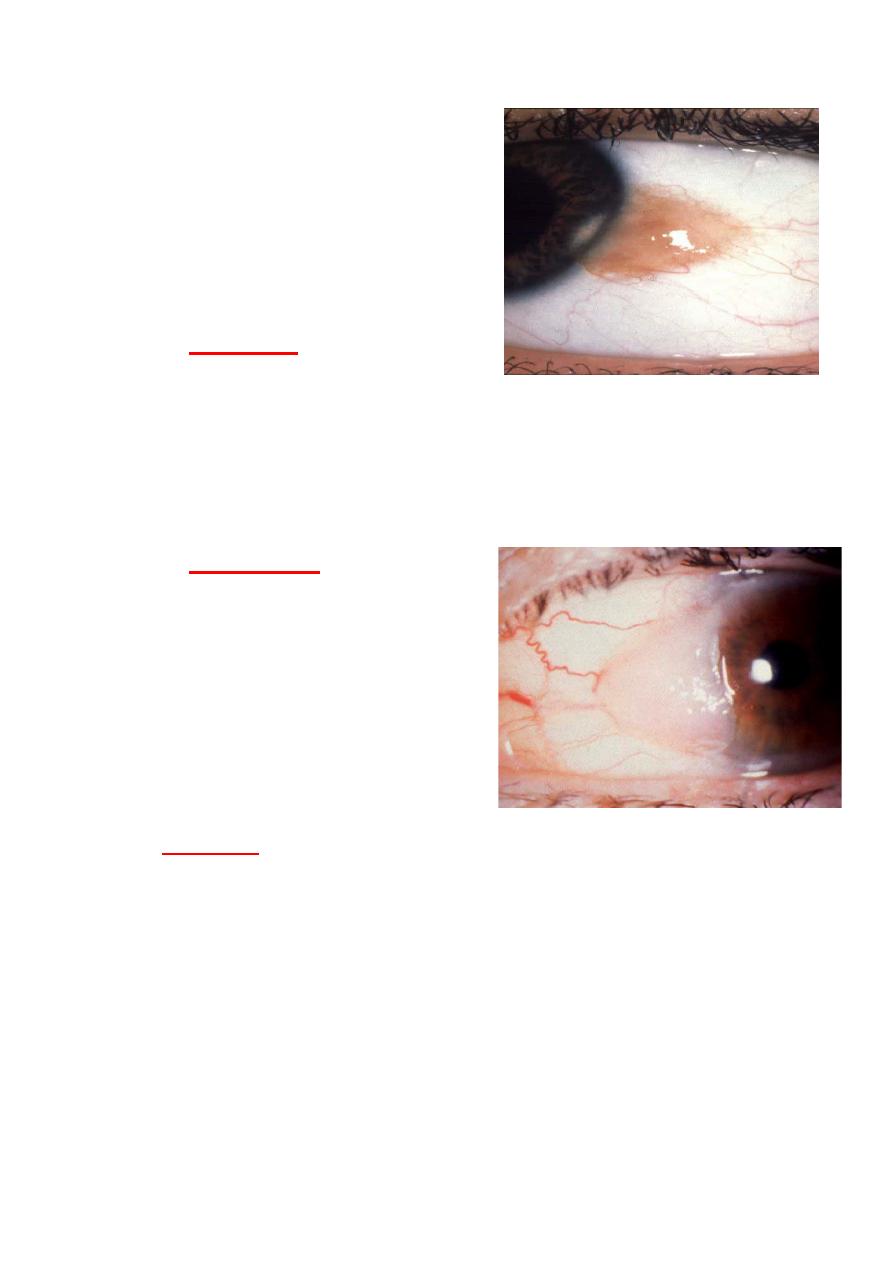
Conjunctival Intraepithelial Neoplasia (CIN):
• Uncommon, slowly progressive, unilateral disease.
• Risk factors:
1 UV light exposure
2 HPV16 infection.
3 AIDS.
4 Xeroderma pigmentosum.
Histology:
the spectrum includes:
1- Conjunctival epithelial dysplasia with dysplastic cells in
the basal layers of epithelium.
2- Carcinoma in situ with dysplastic cells involving the full
thickness of the epithelium.
3- Squamous cell carcinoma: is rare and characterized by
invasion of the underlying stroma.
22
Diagnosis:
usually late in adult life with irritation or mass.
1- Papillomatas lesion, which is discrete and have corkscrew
like blood vessels.
2- Nodular Squamous cell carcinoma a fleshy mass with
feeder vessels often at the limbus. Well-differentiated lesion
grow slowly and have a leukoplakia appearance with corneal
involvement.
Treatment:
1- Localized lesion by excision assessment of safety margin
by frozen section as well as adjunctive cryotherapy, or topical
chemotherapy.
2- Diffuse lesion topical mitomycin c, 5-fluorouracil and
interferon.
3- Enucleation or exenteration.
Kaposi sarcoma:
Affects patients with AIDS.
Vascular, slow-growing
tumour of
low malignancy.
Very sensitive to
radiotherapy.
Most frequently in inferior
fornix.
