
Specific: T.B. and syphilis.
Non-specific
Chronic irreversible inflammation of the
mucous membrane of the pharynx with
hyperplasia of it's various elements. Not
infrequently the normal lymphoid tissue on
the posterior pharyngeal wall undergo
hypertrophy so called granular pharyngitis.
Likewise the strip of lymphoid tissue in the
posterior tonsillar pillar may undergo an
overgrowth forming the lateral pharyngeal
band.
Aetiology
The aetiology is usually obscure:
-Recurrent attacks of acute pharyngitis.
-Persistant neighbourhood infection as chronic
sepsis in the teeth, gums and sinuses.
Bronchiactasis is said to be associated with
chronic pharyngitis.
-Exogenous irritants such as tobacco, alcohol
and industrial fumes.
-Endogenous irritants as gastroesophageal reflux.
-Allergic factors.
Clinical picture
1. Discomfort and painful throat without fever.
There is none of the malaise of tonsillitis and
the condition persists for weeks or months.
2. Foreign body sensation in the throat.
3. Tendency to clear the throat, which results
from postnasal drip bathing the posterior
pharyngeal wall.
Clinical picture
4. Tiring of voice (not hoarseness).
5. Fear of cancer may be dominant in patient’s
mind.
Examination
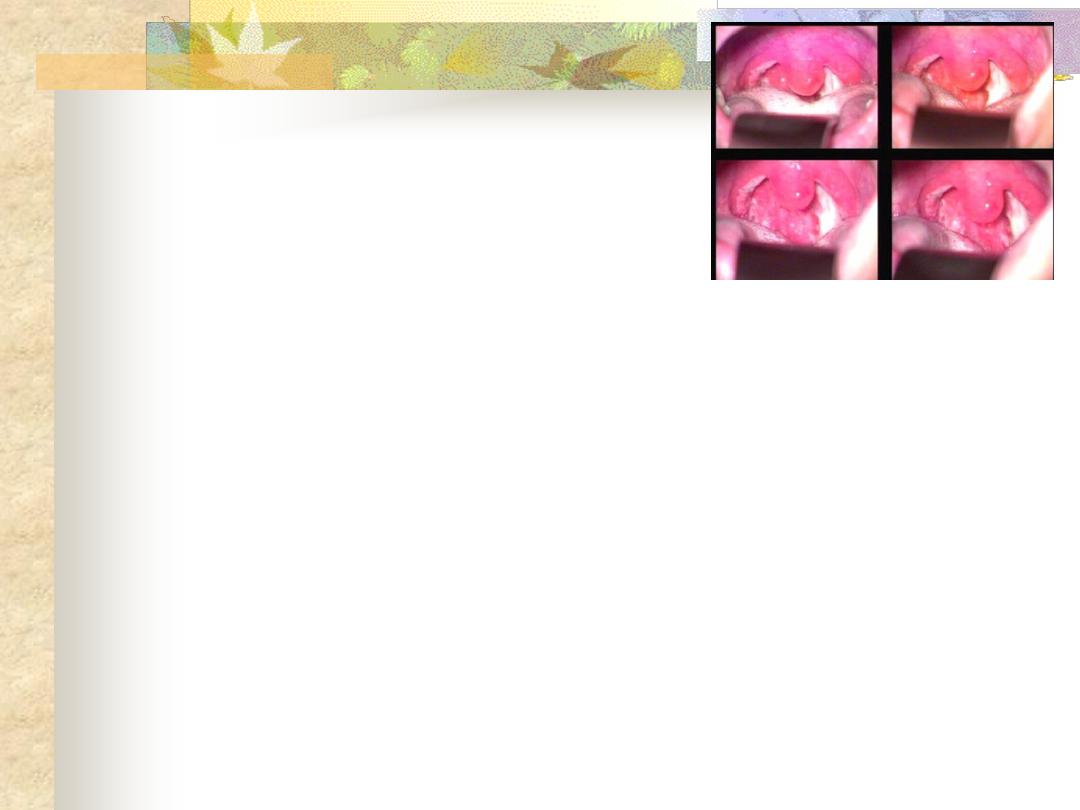
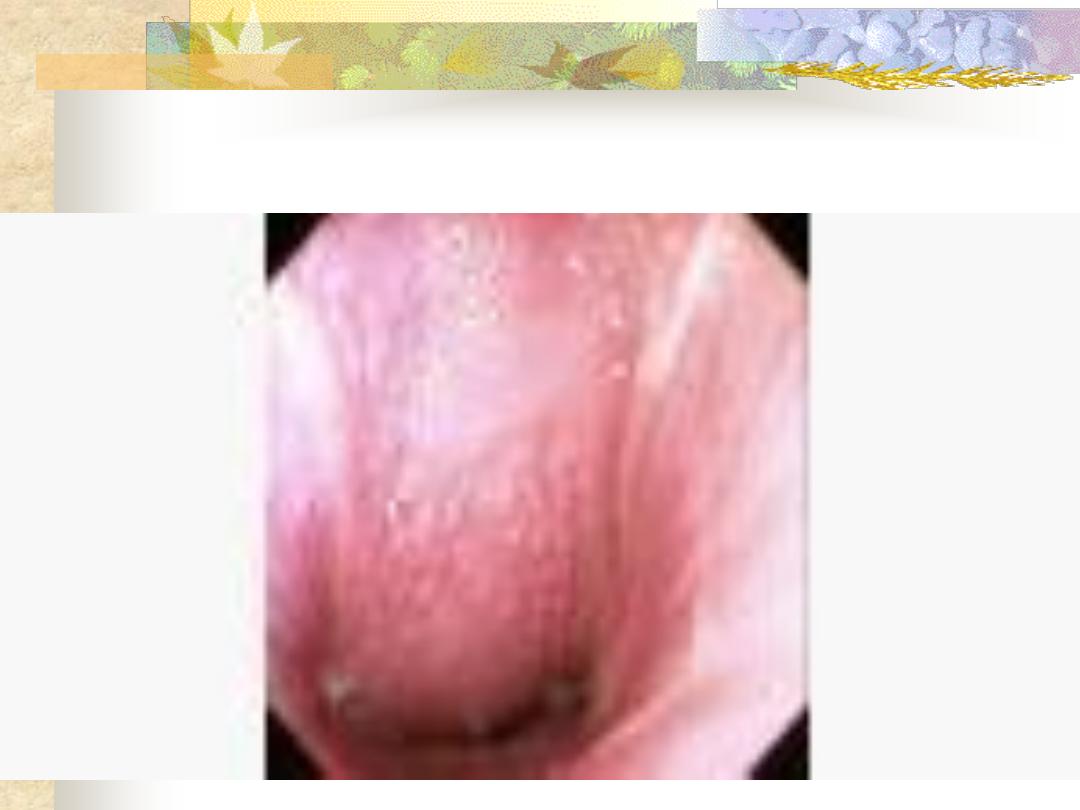
Simple (catarrhal) type: redness and congestion
of the pharyngeal mucosa. The uvula may
appear enlarged or elongated.
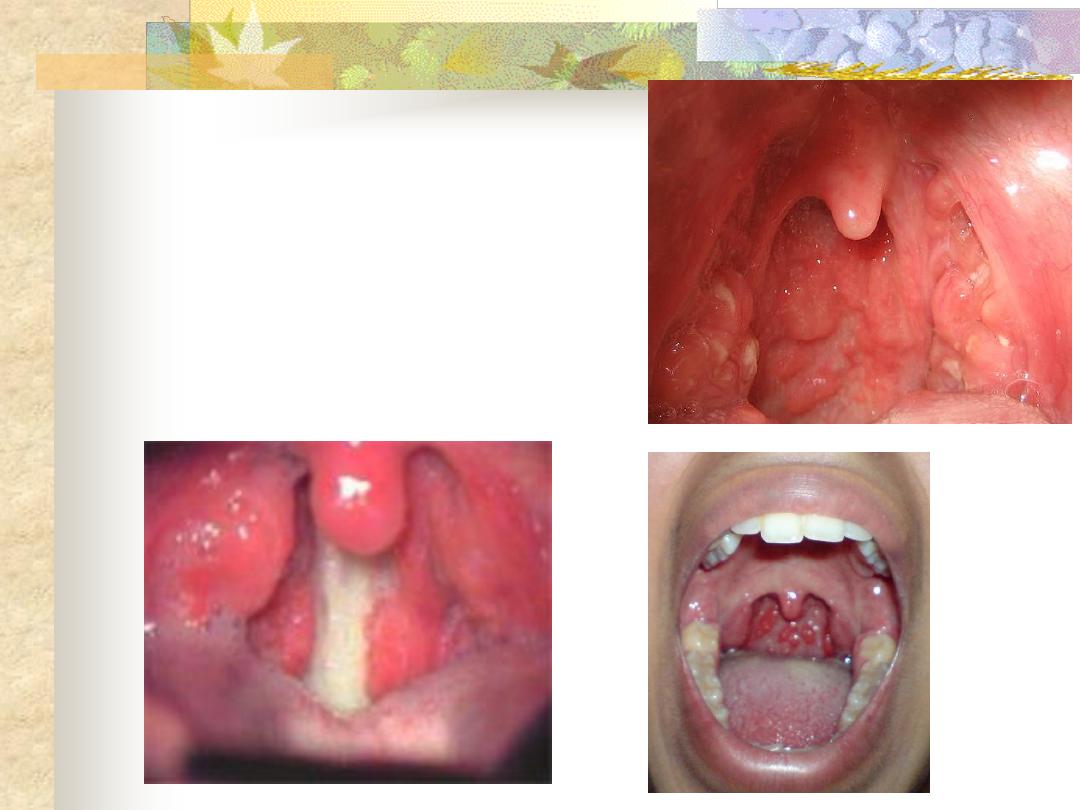
Hypertrophic (granular) type: small nodules are
scattered on the posterior pharyngeal wall
giving a granular appearance. The lateral
pharyngeal bands may be prominent.
Chronic Pharyngitis
Treatment
1.Treat the cause: Appropriate treatment of
postnasal drip –if present- ( by intranasal
steroid), and acid reflux (by proton pump
inhibitor).
2. Altering the patient habit in regard to
smoking, alcoholism and food.
3. Reassurance by the exclusion of malignancy.
Treatment
4. Soothing gargles such as crushed soluble
aspirin.
5. Antibiotics if there is fever.
A chronic atrophic type of inflammation of
the mucous membrane of the pharynx. The
major changes occur in the postcricoid region
initially started by fissuring and hyperkeratosis
followed by fibrosis, web formation of
stricture.
A small proportion of patients (3%)
with this condition progress to the stage of
postcricoid cancer.
Aetiology
It’s unknown but autoimmune and metabolic basis
may be presumed.
Clinical picture
The disease is more common in females usually over
40 years.
-Dysphagia and feeling of a lump in the throat.
-Pallor due to iron deficiency anaemia.
-Fissures at the angles of the mouth result from
angular stomatitis.
-Dryness of the tongue because of glossitis
-Koilonychia
-Loss of weight
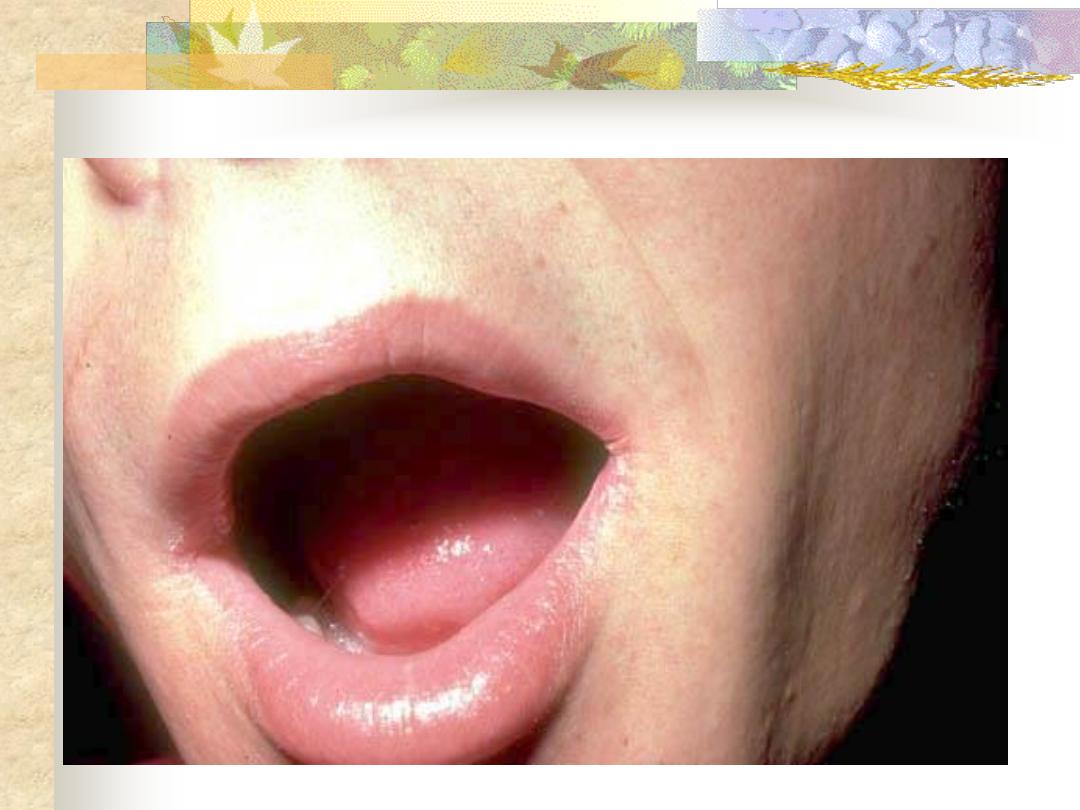
Angular stomatitis
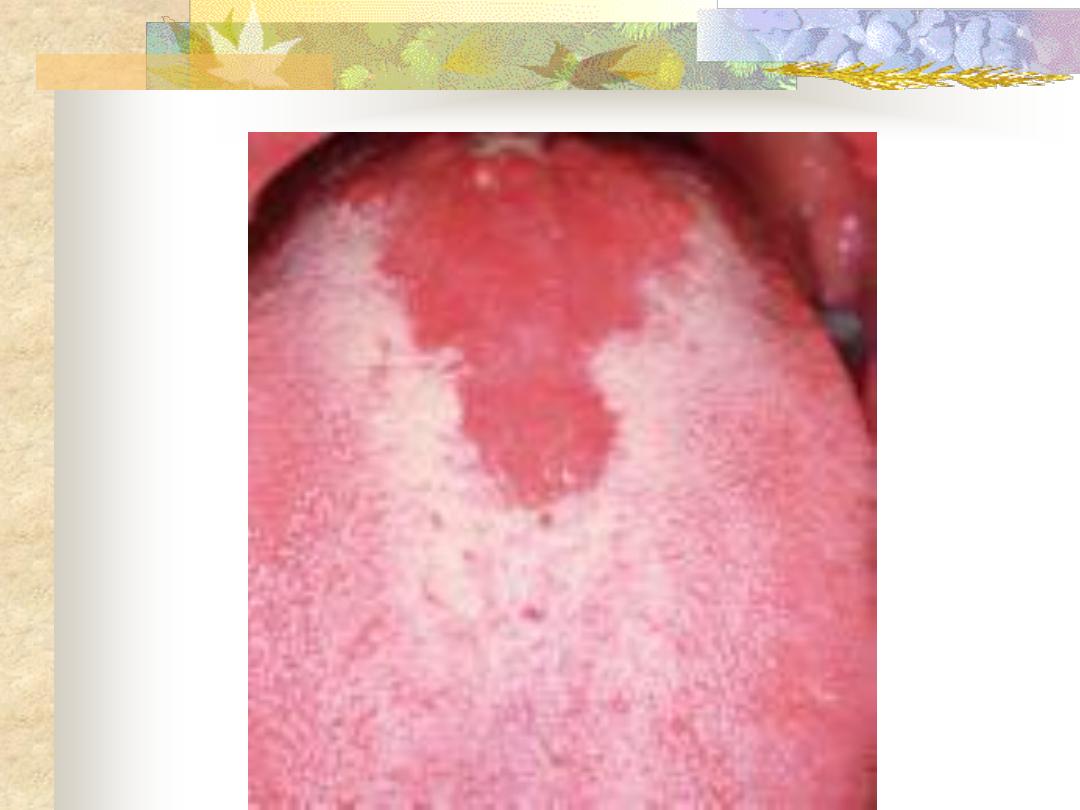
Glossitis
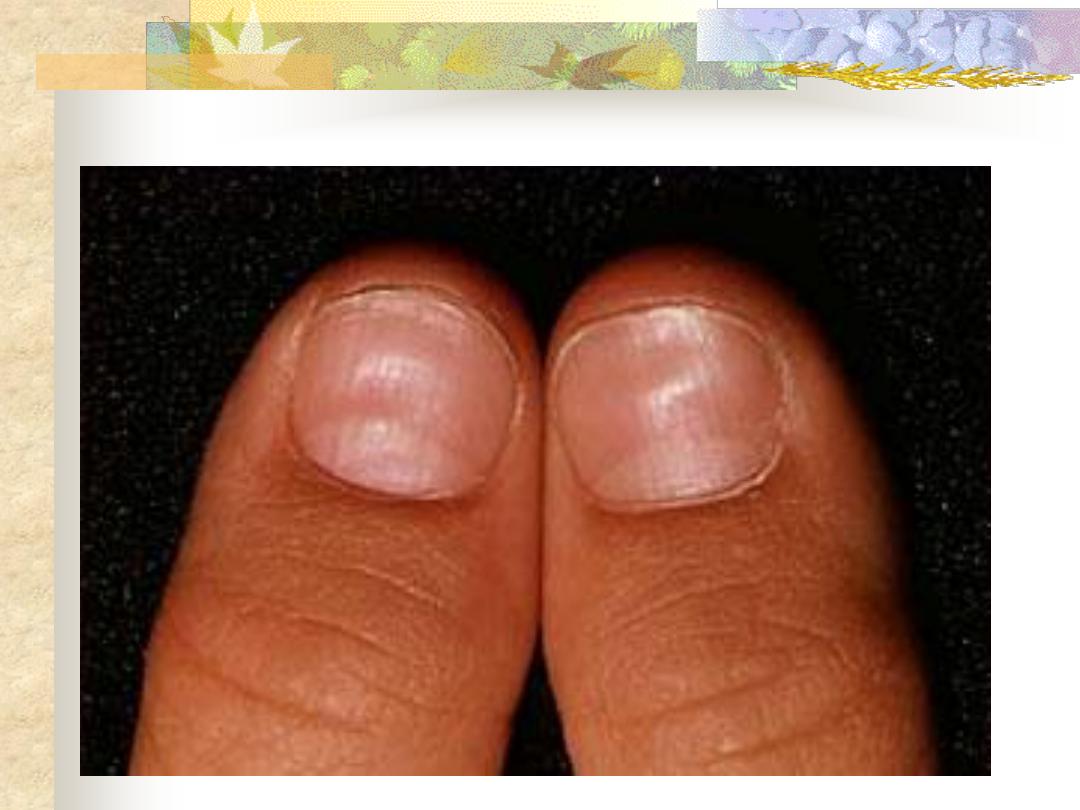
Koilonychia
Investigations
-Haematological: CBP---- hypochromic microcytic
anaemia, low serum iron and high iron binding
capacity.
-Ba -swallow: web at the postcricoid region.
-Endoscopy: changes of the postcroid region
.
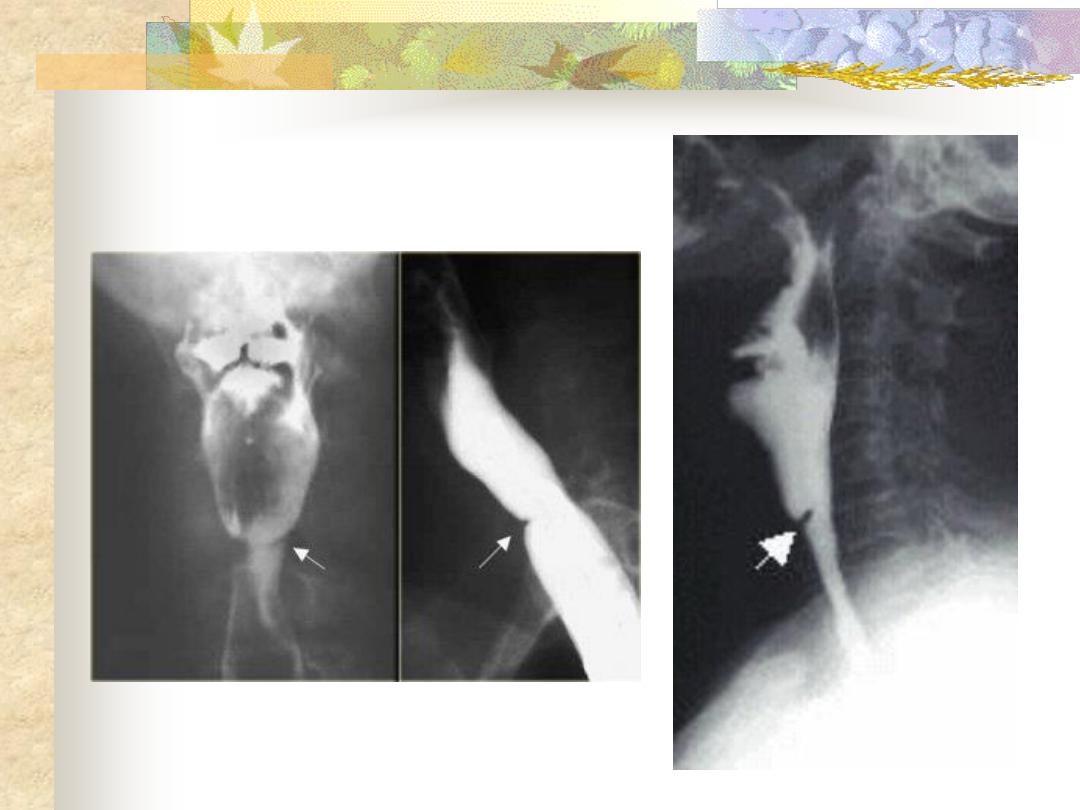
Oesophageal web
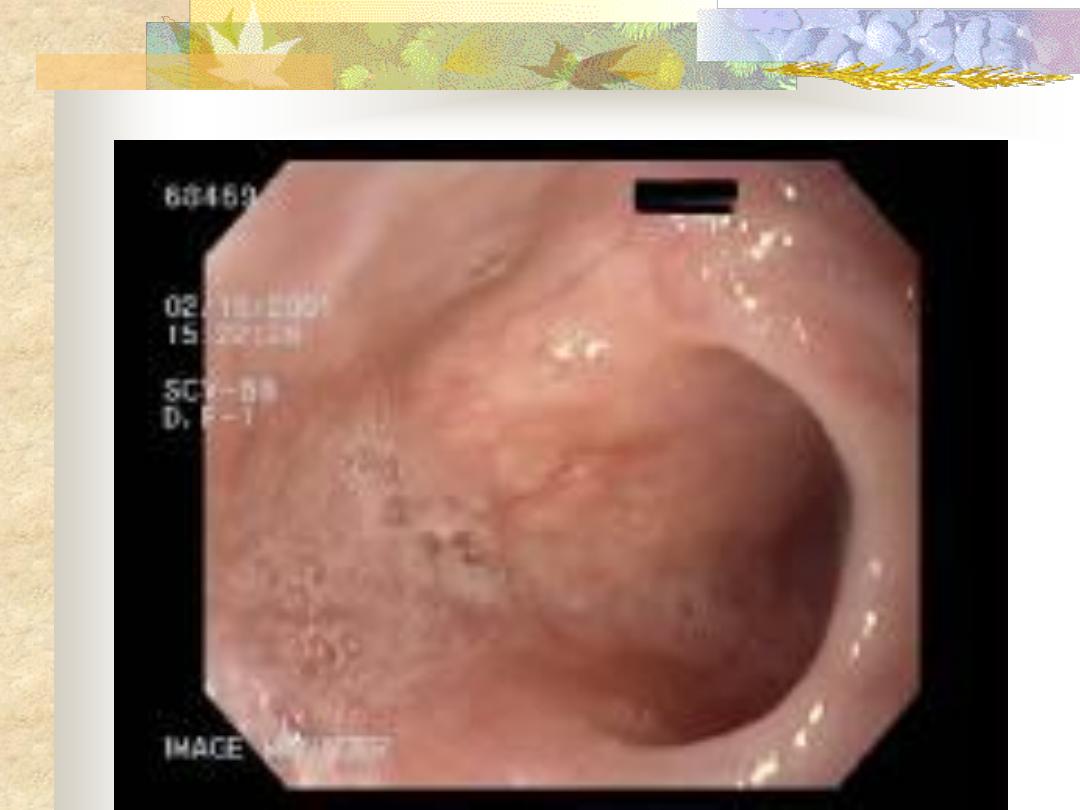
Endoscopic Findings
Treatment
-Iron and vitamin B complex in high doses.
-Endoscopic dilation in resistant cases to medical
treatment to relieve dysphagia and exclude
malignancy
(
by
histopathological
examination).
-Keep the patient under observation, because
malignant changes can still occur.

Sensation of a lump in the throat
affecting mainly females, which is brought
on or made worse by anxiety.
Aetiology
The condition is often regarded as
functional in which no other organic cause
can be found. Recently the most accepted
organic theory is gastroesophageal reflux.
Clinical Picture
Sensation of a lump in the throat, which is,
noticed when the patient is swallowing saliva
(i.e. between meals) and relieved by
swallowing solid food. There is no true
dysphagia
and
the
patient
often
has
psychological stress or cancer phobia.
Diagnosis
The condition should not be diagnosed until an
organic lesions has been excluded in order
not to miss an early carcinoma.
-Ba -Swallow ---- cricopharyngeal spasm
-Endoscopy to exclude any abnormality
-Full haematological investigations to exclude
Plummer-Vinson syndrome.
Treatment
1.
Reassurance that there is no organic
disease or cancer
2.
Antireflux
therapy:
Omeprazole
+
Domperidone
3.
Psychiatric consultation is required in
selected cases
Remember that : dysphagia +
weight loss
pain radiating to the ear
enlarged neck lymph node
Malignancy is the cause until proven
otherwise !!!

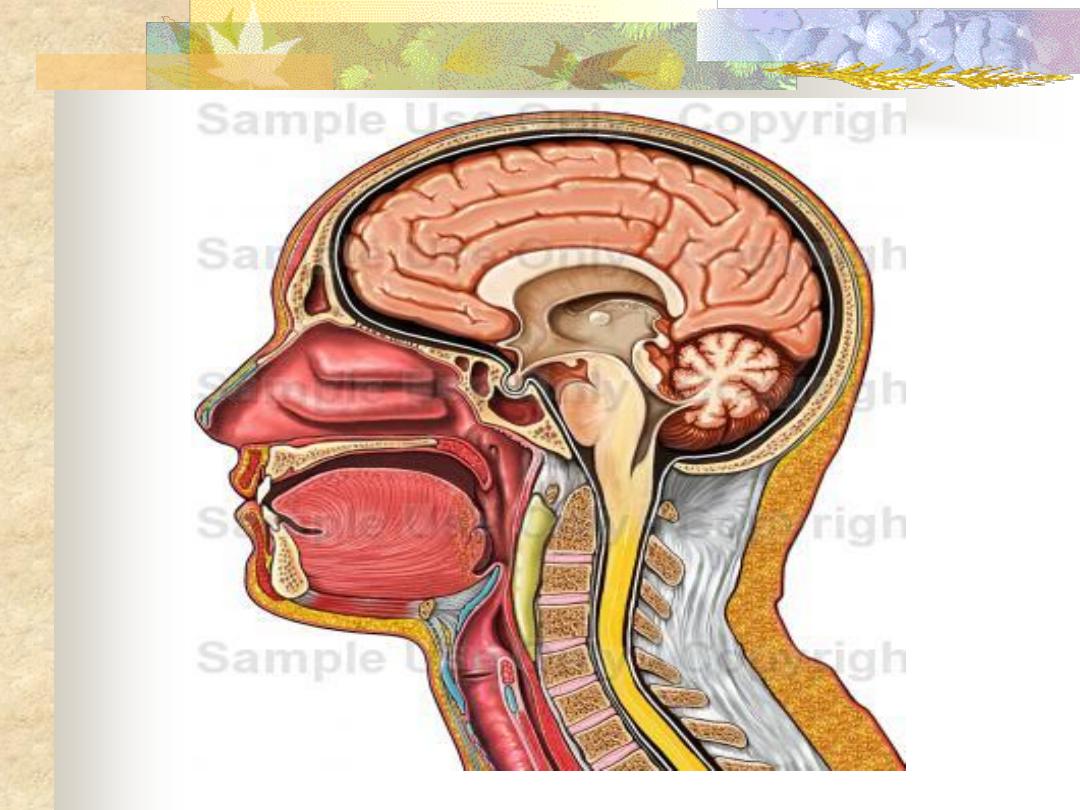
An abscess in the potential space between
the buccopharyngeal and prevertebral fascia.
There are two distinct types.
Collection of pus in the retropharyngeal
space due to infection in the retropharyngeal
lymph nodes (lymph nodes of Rouviere).
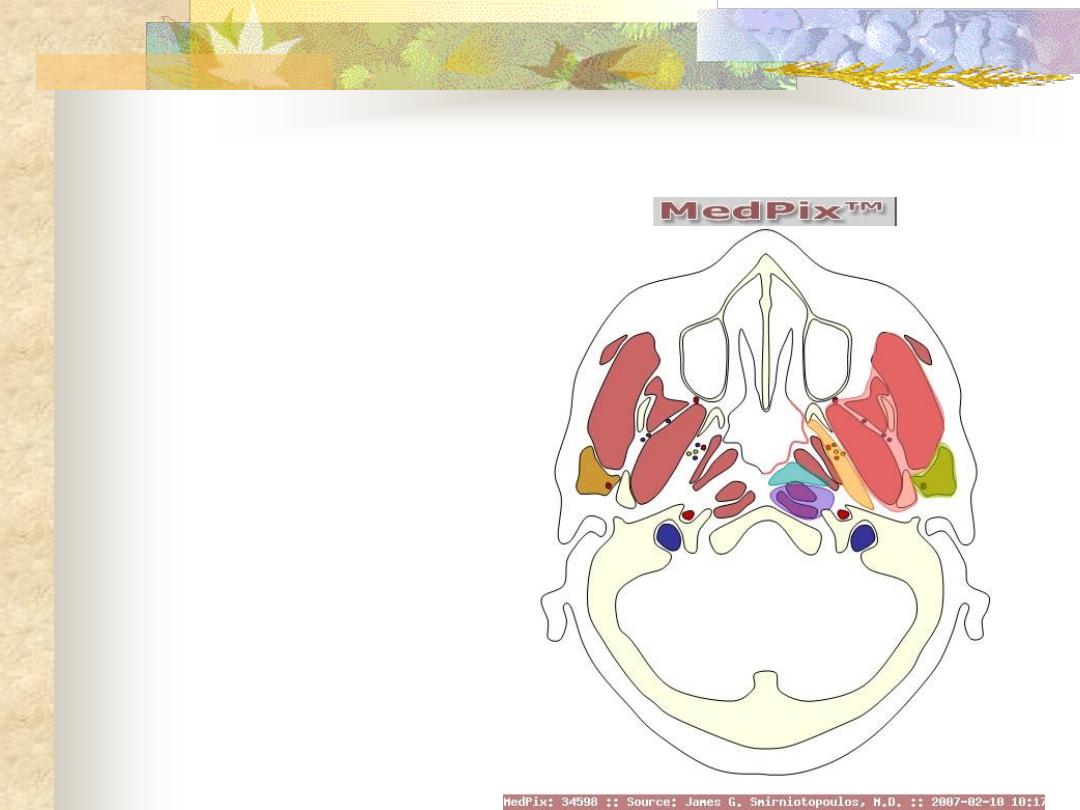
Parapharyngeal space:
orange
Retropharyngeal space:
blue
Aetiology
-Upper respiratory tract infection (Tonsillitis,
sinusitis)
-F.B penetrating the posterior pharyngeal
mucosa.
Clinical Picture
Mostly affects infants and it's of acute onset
1. The patient is ill, toxic and feverish.
2. Sore throat with pain and discomfort on
swallowing and the patient may drool saliva.
3. Nasal obstruction in upward situated abscess
and laryngeal obstruction (stridor) in those
situated downward.
Examination
-Swelling on one side of the posterior pharyngeal
wall.
-Cervical lymphadenopathy.
Investigations
Lateral X-ray of the neck, which shows
increase in prevertebral soft tissue shadow or
an air-fluid level.
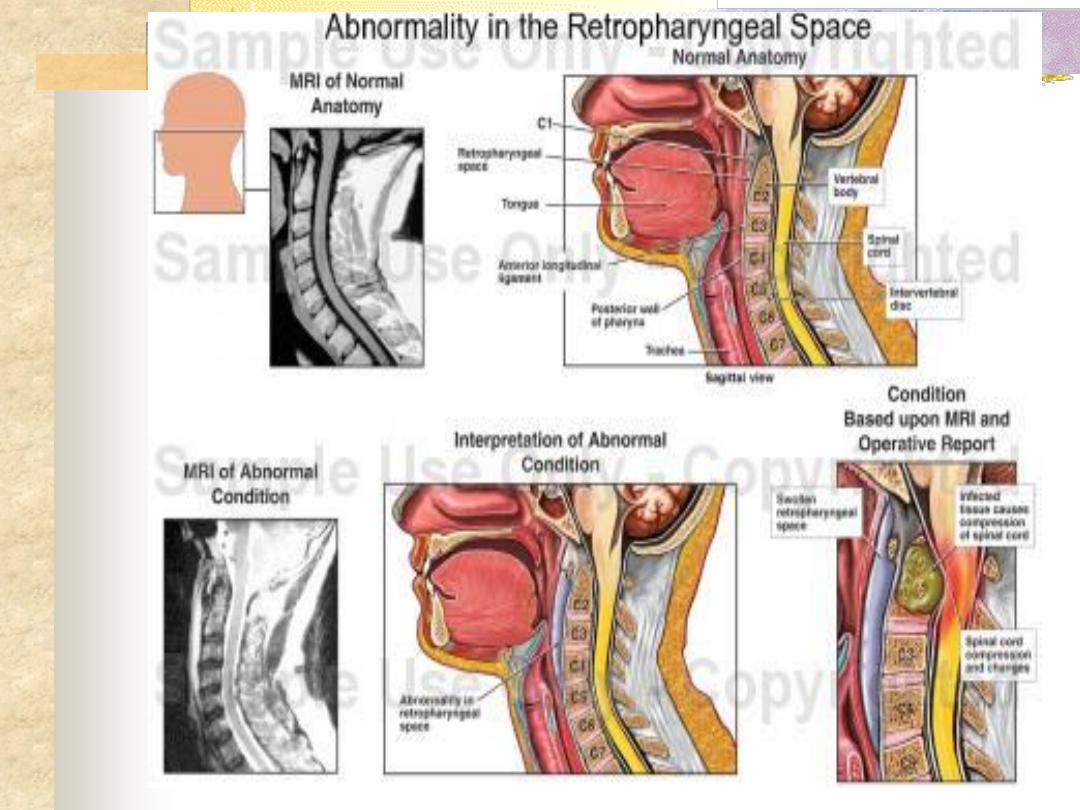
Retropharyngeal space
Acute retropharyngeal abscess
Retropharyngeal abscess
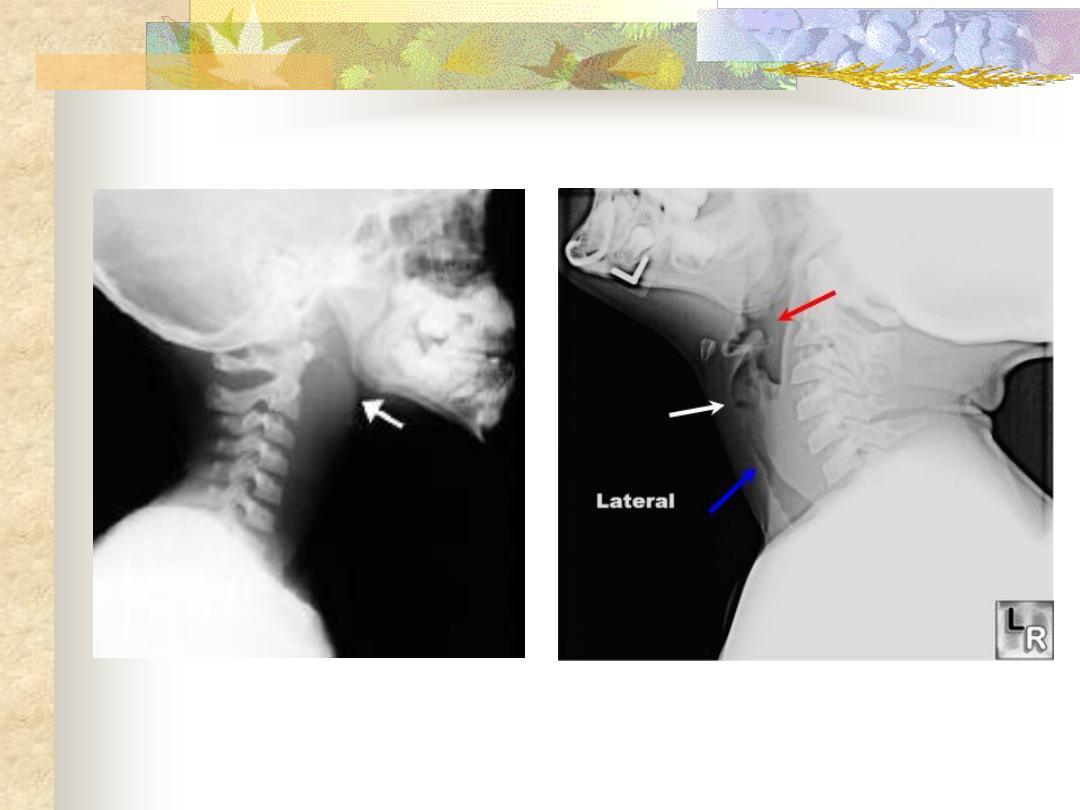
Acute retropharyngeal abscess
Treatment
Under the cover of intravenous antibiotics,
the abscess should be drained vertically
through the posterior pharyngeal wall.
1. Drainage under G.A. with endotracheal tube.
2. If no facility for G.A. an assistant should be
ready to turn the patient over quickly after
drainage to avoid inhalation of pus. A sucker
should be present to aspirate the pus.
This is caused by TB of the cervical spine.
Clinical Picture
Occurs in older children, adolescents and
adults. It’s of slow onset and presents as:
-Pharyngeal discomfort rather than pain.
-Mild dysphagia.
Examination
1. Painless swelling on the posterior pharyngeal
wall.
2.
Enlarged
and
painless
cervical
lymphadenopathy.
Investigations
Lateral X-ray of the neck shows evidence of
bone destruction and loss of the normal
curvature of the cervical spine.
Treatment
1. Drainage through the neck and never
through the mouth to avoid secondary
infection.
2. Full anti T.B. therapy must be ordered.

Chronic retropharyngeal abscess

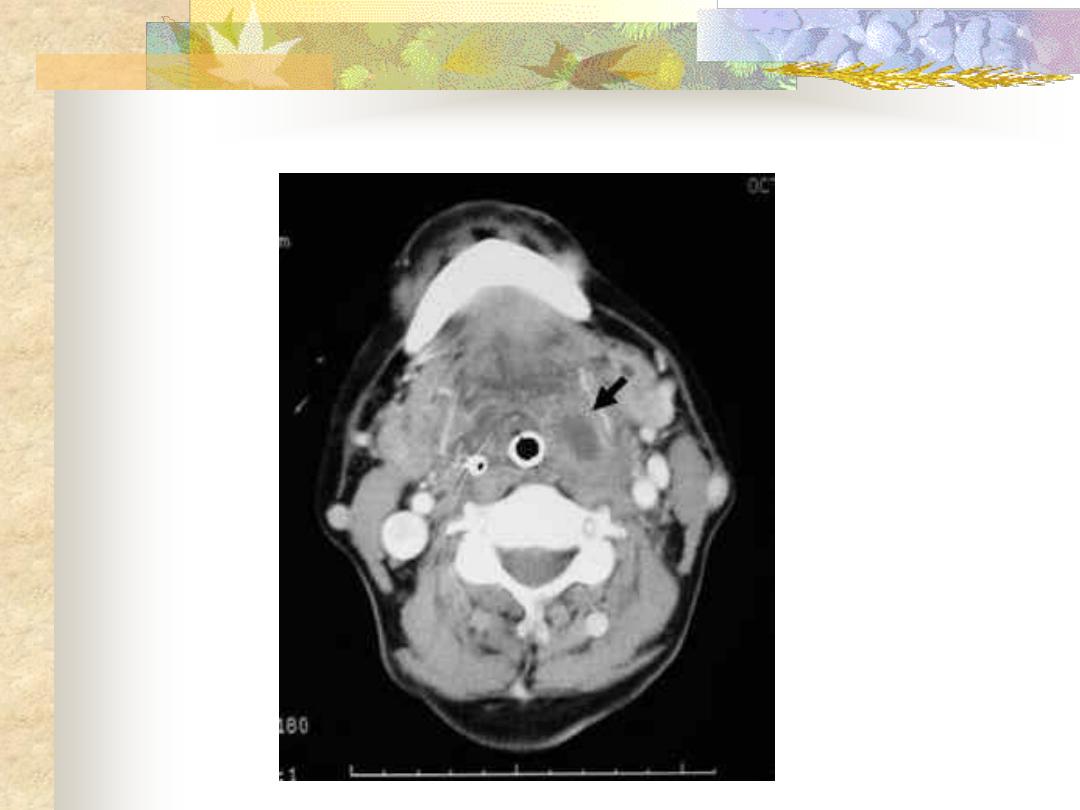
A suppurative infection of the parapharyageal
space.
Aetiology
-Complication of tonsillitis or tonsillectomy.
-Infection or extraction of the lower third molar
tooth.
-Extension of mastoid infection
Clinical Picture
Occurs mostly in adolescents and adults
-The patient is feverish , ill and toxic.
-Acute
sore
throat
with
dysphagia
and
odynophagia.
-trismus because of spasm of the medial
pterygoid muscle
.
Examination
-Tender and firm swelling in the upper part of
the neck.
-The pharyngeal wall and tonsil are pushed
medially.
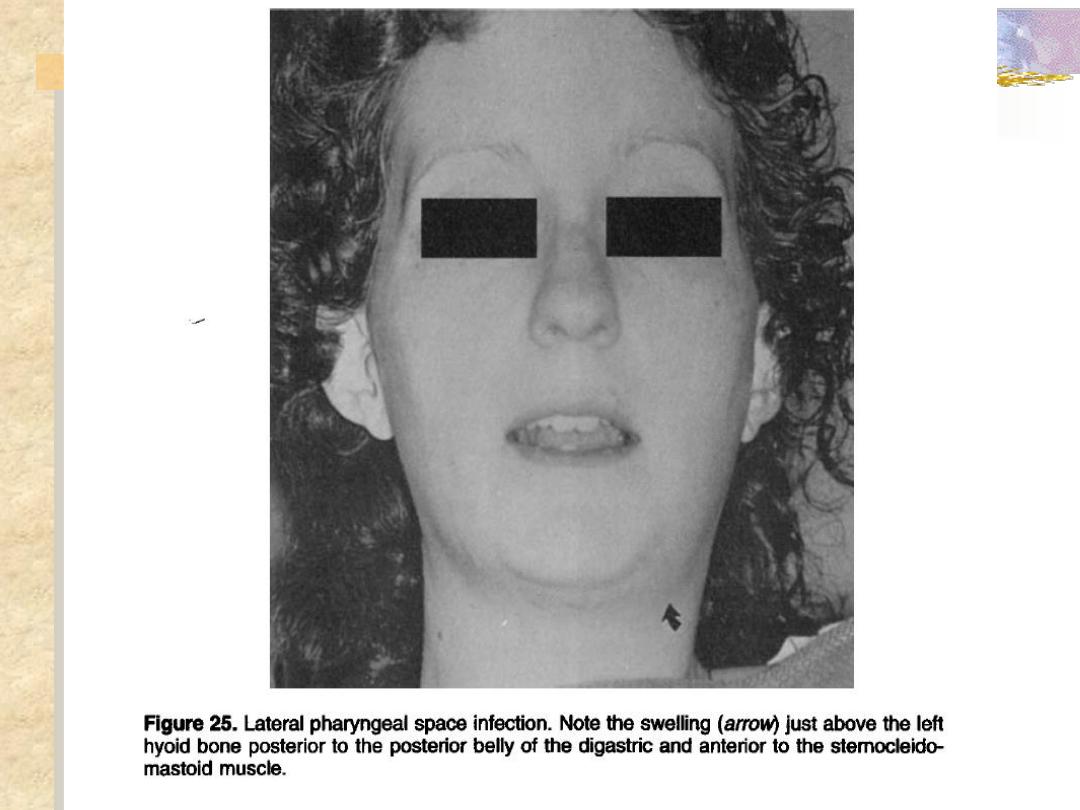
Parapharyngeal Abscess
Complications
1- Acute oedema of the larynx tracheostomy.
2. Thrombophlebitis of the IJV with septicaemia.
3. Carotid artery erosion.
4. Cranial nerves and sympathetic chain
involvement leading to Horner
,
s syndrome.
5. Spread of infection into the mediastinum.
Treatment
Antibiotics should be commenced before
culture and sensitivities are available:
I.V. penicillin + Metronidazole
If the general condition is stable and airway is
patent investigations can be done:
1. WBC ↑, ESR ↑
2. Needle aspiration will prove the diagnosis(
if doubtful) and pus is send for culture.
3. Orthopantomogram ( OPG) may shows root
abscess.
4. Ultrasound of the neck can differentiate
between cellulites and abscess collection.
If there is no improvement within 24
hours abscess must be drained:
Under GA and ETT collar incision is done
in the neck at the level of hyoid bone at the
anterior border of sternomastoid muscle,
pus is evacuated and drain is inserted.
Aetiology
-Idiopathic.
-Infection: diphtheria and poliomyelitis.
-Neurological: paralysis of the lower 4 cranial
nerves by lesions of the brainstem jugular
foramen and upper part of the neck.
-Malignancy: nasopharyngeal malignancy.
-Surgical
trauma:
tonsillectomy
and
adenoidectomy
Clinical picture
1.Unilateral: the condition may be asymptomatic
although the palate is pulled to the healthy
side.
2.Bilateral: hypernasality (rhinolalia aperta) and
regurgitation of food.
On examination
1- Unilateral: the palate rises up to the healthy
side.
2- Bilateral: the palate is immobile in speech and
not retract by touching with a probe
Treatment
-Treat the cause.
-In severe cases with regurgitation------NGT
feeding.

. All are true regarding globus pharyngeus
:
EXCEPT
a. It is associated with tumour of the upper
oesophagus.
b. Sensation of lump in the throat affecting
mainly females.
c. The condition is regarded functional with
no organic cause.
d. Reassurance is the treatment of
choice.
. All are true regarding chronic non specific
:
EXCEPT
pharyngitis
a. This is associated with smoking.
b. Its exacerbated by chronic bronchitis and
sepsis in teeth, gums and sinuses.
c. Lymphoid hypertrophy of the posterior
pharyngeal wall is seen in some cases.
d. Tonsillectomy is the treatment of choice.
. Plummer Vinson syndrome is common in:
a. Males.
b. Females.
c. Diabetics.
d. Children.
Acute retropharyngeal abscess is
commonly seen in:
a. Infants.
b. Adults.
c. Middle aged females.
d. Elderly.
e. Diabetics.


