Bipolar disorder
Dr. Safeya AlchalabiBipolar disorder
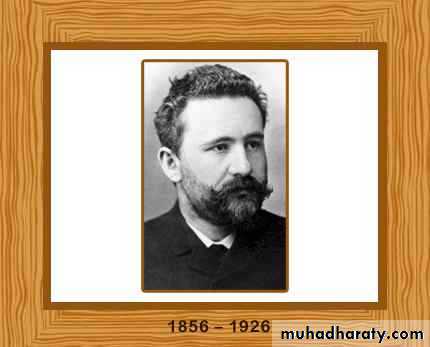
Kraepelin (1921)
brought maniaand depression
together as manic
depressive psychosis.
• Epidemiology of bipolar and unipolar (depressive) disorder
•• Bipolar disorder
• Unipolar disorder
• Lifetime risk
• About 1%
• About 15%
• Sex ratio (M:F)
• 1:1
• 1:2
• First-degree relatives
• Lifetime risk for bipolar disorder
• About 10%
• About 2%
• Lifetime risk for unipolar disorder
• 20–30%
• 20–30%
• Average age of onset
• 18 years
• 27 years
• Patients with recurrence
• 90%
• 80%
• Average number of episodes
• 10
• 4
Clinical features of a manic episode
Mood is elevated out of keeping with the individual’s circumstances, varying from carefree joviality to almost uncontrollable excitement.In some manic episodes the mood is irritable and suspicious rather than elated
Clinical features of a manic episode
● Increased energy results inoveractivity,
pressure of speech, and
a decreased need for sleep
Clinical features of a manic episode
Social inhibitions are lost,
attention cannot be sustained, and
there is often marked distractibility
Clinical features of a manic episode
● Self-esteem is inflated, and grandioseoveroptimistic ideas are freely expressed
Clinical features of a manic episode
● Perceptual disorders may occur; for example, the appreciation of colours can be especially vivid and beautifulClinical features of a manic episode
● The individual may embark on extravagant and impracticable schemes,spend money recklessly or
become aggressive, amorous, or facetious in inappropriate circumstances
Clinical features of a manic episode
For diagnosis,the episode should last for at least one week and should be severe enough to disrupt ordinary work and social activities more or less completely.
The mood change should be accompanied by increased energy and pressure of speech, decreased need for sleep, grandiosity, and excessive optimism.
Criteria for hypomanic episode in ICD-10 and DSM-5
Hypomania refers to a state of elevated mood that is of lesser extent than mania.
The criteria in ICD-10 and DSM-5 are similar:
● There is persistent mild elevation of mood for at least several days with increased energy and activity and feelings of wellbeing.
● There is increased sociability, talkativeness and overfamiliarity, increased sexual energy, and decreased need for sleep.
● not sufficiently severe to cause marked impairment in social or occupational activities, or to necessitate hospital admission.
● Psychotic features are absent.
Rapid cycling disorders ( folie circulaire) or (circular insanity)
Some bipolar disorders recur regularly, with intervals of only days or weeks between episodes.These recurrent episodes may be depressive, manic, or mixed.
The main features are that recurrence is frequent ( at least four distinct episodes a year), and that episodes are separated by a period of remission or a switch to an episode of opposite polarity.
Rapid cycling disorders ( folie circulaire) or (circular insanity)
• A number of clinical features of rapid cycling disorder are important in management and prevention.They occur more frequently in women.
Concomitant hypothyroidism is common.
They can be triggered by antidepressant drug treatment.
Rapid cycling disorders ( folie circulaire) or (circular insanity)
The lifetime risk of rapid cycling in bipolar populations is probably in the range 15–30%.Rapid cycling may be a temporary phenomenon, and in most patients it remits within about 2 years.
Cyclothymia
persistent instability of mood in which there are numerous periods of mild elation or mild depression that do not meet severity criteria for either major depression or hypomania.
It is seen as a milder variant of bipolar disorder.
Depression
Depressive episodes are common in the course of bipolar disorderMost patients with bipolar disorder present initially with an episode of major depression.
Depression
• Other clinical features associated with subsequent development of bipolar illness include:early age of onset.
clinical severity.
The presence of psychosis.
family history.
The presence of any hypomanic or mixed symptomatology at initial presentation.
Depression
• There is a high degree of overlap between the clinical symptomatology of unipolar and bipolar depression; however,psychomotor retardation,
early morning awakening,
morning worsening, and
psychotic features
• are reportedly more common in patients with bipolar disorder.
DSM-5 categorizes bipolar disorder as follows:
● Bipolar I, in which mania has occurred on at least one occasion.
● Bipolar II, in which hypomania has occurred, but mania has not. However, to make the diagnosis of bipolar II disorder an episode of major depression must also have occurred.
Differential diagnosis of bipolar disorder
● schizophrenia;● organic brain disease involving the frontal lobes (including brain tumour and HIV infection);
● states of brief excitement induced by amphetamines and other illegal drugs.
Epidemiology
The lifetime risk for bipolar disorder is in the range 0.3–1.5%.The prevalence in men and women is the same.
The mean age of onset is about 18 years in community studies (Late-onset bipolar disorder is rare, and may be precipitated by organic brain disease.
)
Bipolar disorder is highly comorbid with other disorders, particularly anxiety disorders and substance misuse, as well as general medical conditions such as cardiovascular disease.
Course and prognosis
Bipolar disorders● Bipolar disorder usually begins as depression, with the first manic episode manifesting about 5 years later.
Course and prognosis
Bipolar disorders● The average length of a manic episode (treated or untreated) is about 6 months.
Course and prognosis
Bipolar disorders
● At least 90% of patients with mania experience further episodes of major mood disturbance.
Course and prognosis
Bipolar disorders● Over a 25-year follow-up, on average bipolar patients experience about 10 further episodes of major mood disturbance.
Course and prognosis
Bipolar disorders● The interval between episodes becomes progressively shorter with both age and the number of episodes.
Course and prognosis
Bipolar disorders● Nearly all bipolar patients recover from acute episodes, but the long-term prognosis is rather poor. For example, less than 20% of bipolar patients achieve a period of 5 years of clinical stability with good social and occupational performance.
Course and prognosis
Bipolar disordersPatients with bipolar II disorder have a somewhat better outcome.
Course and prognosis
Bipolar disorders
Persistent cognitive deficits and mood instability predict a poorer outcome.
Mortality of bipolar disorder
Mortality is significantly increased in patients with bipolar disorders.Mortality of bipolar disorder
About 8% of men and 5% of women hospitalized for bipolar illness died by suicide.Mortality of bipolar disorder
The high mortality in bipolar disorder is caused not only by suicide but also general medical conditions such as cardiovascular disease and the secondary consequences of comorbid substance misuse, including smoking.Mortality of bipolar disorder
patients with bipolar disorder found a reduction in life expectancy of about 13 years in men and 9 years in women. About two-thirds of this reduction was accounted for by natural causes, with the remainder being due to suicide and accidents.Mortality of bipolar disorder
Cardiovascular disease is an important cause of increased mortality in bipolar patients, which highlights the importance of attending to the medical needs of this population.Mortality of bipolar disorder
The metabolic effects of extended treatment with psychotropic medication, particularly antipsychotic drugs, also need careful assessment.Treatment of mania
The aim of treatment:
reducing physical and mental overactivity,
improving features of psychosis,
preventing deterioration in health caused by exhaustion, sleep deprivation, and poor fluid intake.
Treatment of mania
It is worth noting that before the advent of modern drug treatment the mortality of mania in the hospital setting was over 20%;nearly 50% of these patients died from exhaustion.
Treatment of mania
MedicationTypical antipsychotic drugs (chlorpromazine and haloperidol ).
Atypical antipsychotic drugs
Lithium (poorer response with prominent depressive symptoms, rapid cycling disorder and psychotic features)
Carbamazepine
Valproate (dysphoric symptoms and rapid cycling.)
Benzodiazepines
Continuation treatment of mania
Since the average length of a manic episode is about 6 months, it seems prudent to continue some form of medication for at least this period.Treatment of bipolar depression
Antidepressant drugs
Depression in the context of a bipolar disorder can be problematic because standard antidepressant treatments have a number of disadvantages, which include:
● a possibly lower efficacy than in unipolar depression;
● a risk of inducing mania;
● a risk of inducing rapid cycling.
Treatment of bipolar depression
Lithiumlithium less efficacious than quetiapine for treatment of bipolar depression
Treatment of bipolar depression
Atypical antipsychotic drugsQuetiapine > olanzapine
Treatment of bipolar depression
Anticonvulsantslamotrigine and valproate.
coadministration of folic acid appeared to antagonize the therapeutic effect of lamotrigine.
Treatment of bipolar depression
Electroconvulsive therapyFor resistant depression in bipolar patients, ECT can be of benefit.
Longer-term treatment of bipolar disorder
Medication
Lithium
Valproate
Lamotrigine
Carbamazepine
Antipsychotic drugs
Longer-term treatment of bipolar disorder
Lithium50% of bipolar patients who are treated with lithium respond well.
use of lithium in patients with recurrent mood disorders is associated with a significant reduction in mortality from suicide.
Longer-term treatment of bipolar disorder
LithiumThe following are predictors of a relatively poorer response to lithium maintenance treatment:
rapid-cycling disorders
chronic depression;
mixed affective states;
alcohol and drug misuse;
mood-incongruent psychotic features.
Longer-term treatment of bipolar disorder
Lamotrigine
it may have some modest benefit in the prevention of mania, lamotrigine has a clearer prophylactic effect against depression.
Longer-term treatment of bipolar disorder
PsychotherapyCognitive behaviour therapy
Family focused approaches
Interpersonal and social rhythm therapy (maintain regular sleep-activity schedules with careful attention to sleep hygiene)
Group psychoeducation