Viral infection
Dr. Anfal laythArab board of dermatology
Objective
general informations about viral infectionViral infection types
Human papilloma virus types and presentation and mode of transmission and treatment
Herpes infection types and presentation and mode of transmission and treatment
Other viral infection
Viral infection
Viruses are obligatory intracellular parasites. They are capable of producing a wide variety of changes in the skin and mucosa.There are two main groups of virus:
DNA viruses: herpes virus, pox virus, adenovirus, ….
RNA viruses: picorna virus, retro virus, paramyxovirus,
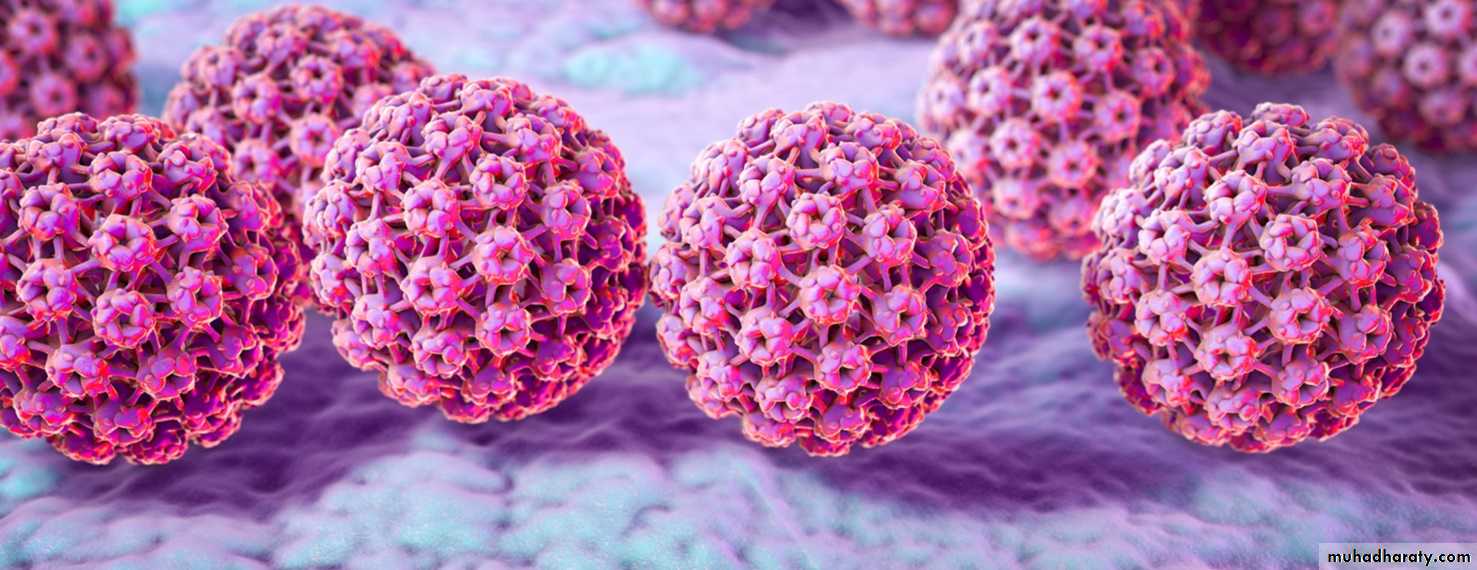
Human papillomaviruses (HPVs)
Papillomaviruses are a large group of double-stranded DNA viruses that are widely distributed in animals and humans, most commonly inducing benign papillomas or wartscomprise a large group of more than 150 genotypes that infect the epithelia of skin or mucosa
EPIDEMIOLOGY
Cutaneous warts are caused by a small group of specific HPV types,with a prevalence of up to 30% in primary schoolchildren
The majority of warts will regress spontaneously within 1–2 years.
After clearance occurs, reinfection with the same HPV type appears to be uncommon, suggesting that protective type-specific immunity may develop.
Genital infection with HPV occurs most commonly by intimate contact, while infection of non-genital skin may occur via direct skinto- skin contact or indirectly through contaminated surfaces and objects (e.g. swimming pool, gymnasium
Autoinoculation
Persistent infection with sexually transmitted high-risk mucosal types, mostly HPV-16 and -18, cause all cervical and most anal cancers, a subset of vaginal, vulvar
Types:
1. Common warts (verruca vulgaris).2. Plantar warts.
3. Plane warts.
4. Filliform or digitate warts.
5. Ano-genital warts.
6. oral warts.
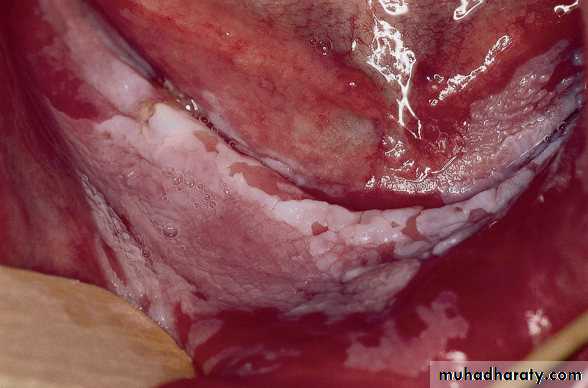
Common warts
are hyperkeratotic, exophytic, dome-shaped skin color papules or plaques that are typically associated with HPV-1, -2, -4These warts are most frequently located on the hands or in other sites prone to trauma
Characteristic features of common warts are punctate black dots representing hemorrhage into the stratum corneum
Palmar and plantar warts
Cause: HPV- 1, 2 & 4.appear as thick, endophytic papules on the palms, soles, and lateral aspects of the hands and feet.
On the soles, these are often painful from pressure when walking, due to their deep inward growth
Plantar warts that coalesce into large plaques are referred to as mosaic warts
Flat warts (Plane warts)
They are usually caused by HPV-3 or -10are skin-colored or pinkish to brown, relatively smooth surfaced, slightly elevated flat-topped papules
most commonly located on the dorsal hands, arms or face
with positive Koebner phenomenon.
Filliform or digitate warts:
Occur mostly on the face, in adults male and spread by shaving.Ano-genital warts
Condylomata acuminataare found on the external genitalia and the perineum, perianally,
Condylomata are typically discrete, sessile, smooth-surfaced exophytic papillomas or acuminate warts and may be skin-colored, brown or whitish (especially when macerated in
moist areas)
High-grade intraepithelial neoplasias are usually caused by high-risk types, mainly HPV-16, -18
whereas low-grade lesions may contain low-risk HPV type 6,11
Buschke–LِwensteinGiant condylomata acuminata
is a rare tumor of the anorectal area and external genitalia associated with the low-risk HPV types 6 or 11The histology of the Buschke–Lِwenstein tumor may appear remarkably benign and resemble that of condylomata acuminata
oral florid papillomatosis
multiple, confluent warty lesions associated with HPV-6 or -11 are found in the oral cavity or the nasal sinuses.The development of these lesions is believed to be promoted by smoking, X-irradiation, and chronic inflammation. Patients with oral papillomas
need frequent examinations and repeated biopsies for early diagnosis of progression to verrucous carcinoma
Differential Diagnoses:
1. Molluscum contagioseum.2. Corn:
* at pressure area.
* no capillary bleeding on paring.
* central keratotic core.
* painful.
3. Granuloma annulare.
4. Cnodylomata lata.
5. Amelanotic melanoma.
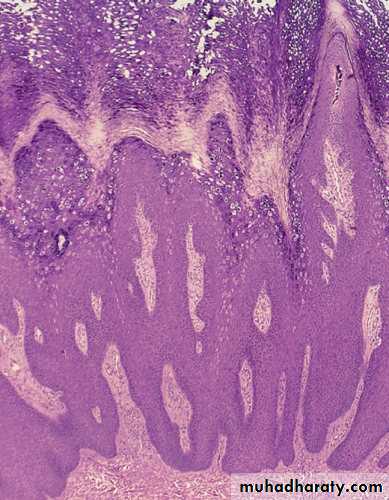
Pathology
Common warts are well circumscribed from the surrounding skincharacteristically have steeply sloping “church spire” papillomatosis
heaped with ortho- and parakeratosis
Treatment:
Spontaneous improvement is common.
* Conservative treatment:
1. Salicylic acid paint, 12-20% for 12 weeks.
(except in: face, anogenital, adjacent eczema.).
2. Formalin 4% solution (plantar warts).
3. lactic acid.
4. Trichloroacetic acid (TCA).
5. Podophyllin (local cytotoxic, genital warts).
6. Imiquimod (immunomodulatory).
7. Zinc sulphate: topical and systemic (immunomodulatory).
7. bleomycin.
8. Suggestion
* Destructive treatment:
1. Curette.2. Electrocautary +/- curette.
3. Cryotherapy: liquid nitrogen(-196), or CO2.
4. Laser.
5. Surgical excision.
HPV Vaccines
The HPV vaccines that have been introduced worldwide over the past decade are aimed at achieving universal vaccination of children and adolescents, ideally before 12 years of age. with CDC recommending “catch-up” shots for those ages 13–26 years.
a quadrivalent vaccine of HPV-6, -11, -16, -18 VLPs (Gardasil)and
a bivalent vaccine of HPV-16, -18 VLPs (Cervarix)
Human Herpesviruses
The human herpesvirus family is composed of eight distinct viruses that cause infections with a wide spectrum of clinical features, including characteristic cutaneous manifestationsThey are medium-sized, double stranded DNA viruses. They replicate inside the nucleus.
The human herpesviruses (HHVs) are categorized into three groups: alpha, beta, and gamma herpesvirinae.Human herpesvirus
ClassificationPredominant cell type infected
Lytic infection
Latent
infection
Herpes simplex virus
type 1 (HSV-1) (HHV-1)
Alphaherpesvirinae
Epithelial cells
Neurons
Herpes simplex virus
type 2 (HSV-2)
(HHV-2)
Alphaherpesvirinae
Epithelial cells
Neurons
Varicella–zoster virus
(VZV) (HHV-3)
Alphaherpesvirinae
Epithelial cells
Neurons
Epstein–Barr virus
(EBV) (HHV-4)
Gammaherpesvirinae
B cells, epithelial cells
B cells
Human herpesvirus
Classification
Predominant cell type infected
Lytic infection
Latentinfection
Cytomegalovirus
(CMV) (HHV-5)
Betaherpesvirinae
Lymphocytes,
macrophages, endothelial
cells
Lymphocytes,
macrophages
Human herpesvirus 6
(HHV-6)
Betaherpesvirinae
CD4+ T cells
Lymphocytes,
macrophages
Human herpesvirus 7 (HHV-7)
Betaherpesvirinae
• T cells
T cells
Human herpesvirus 8
(HHV-8)
Gammaherpesvirinae
Lymphocytes
Lymphocytes,
endothelial
cells
HERPES SIMPLEX VIRUSES (HSV-1 AND HSV-2)Synonyms/clinical variants: ■ herpes simplex ■ Herpeslabialis – cold sore, fever blister, herpes febrilis ■ Herpes gladiatorum ■ Herpetic whitlow ■ Genital herpes
Herpes simplex viruses produce primary and recurrent vesicular eruptions that favor the orolabial and genital regions
The word “herpes” was first defined by Greek scholars as “to creep or crawl” in reference to the spreading nature of the skin lesions
Type I: which cause extra genital infection.
Type II: which cause genital disease.
Pathogenesis
Transmission of HSV can occur during asymptomatic periods of viral shedding.HSV-1 is spread primarily through direct contact with contaminated saliva or other infected secretions
while HSV-2 is spread primarily by sexual contact
Virus replicates at the mucocutaneous site of infection and then travels by retrograde axonal flow to the dorsal root ganglia, where it establishes latency until reactivation.
Latency enables the virus to exist in a relatively non-infectious state for varying periods of time in its host.
• CLINICAL DISEASE
• Local & systemic manifestation, Antibodies develop in the course of illness.
• PRIMARY INFECTION
• Susceptible individual (–ve antibodies)
• LATENT PHASE
• No evidence of clinical disease. Antibodies persist.
• SUBCLINICAL INFECTION
• Absent clinical manifestations, only Antibodies develop.
• NO SUBSEQUENT VISIBLE DISEASE THROUGHOUT LIFE
• May intermittently excrete virus. Antibodies persist.
• RECURRENT LESIONS
• Usually local lesion without systemic manifestationClinical FeaturesPrimary infections
* Primary type I infectionasymptomatic infection is very common.
Symptoms typically occur within 3 to 7 days after exposure.
A prodrome of tender lymphadenopathy, malaise, anorexia, and fever often occurs before the onset of mucocutaneous lesions, which may be preceded by localized pain, tenderness, burning, and tingling.
Painful, grouped vesicles appear on an erythematous base followed by erosions, and/or ulcerations with a characteristic scalloped border.
Crusting of lesions and resolution of symptoms typically occurs within 2 to 6 weeks.
Primary type II infection
asymptomaticalso present as an excruciatingly painful, erosive balanitis, vulvitis, or vaginitis.
In women, lesions often also involve the cervix, buttocks, and perineum and may be associated with inguinal adenopathy and dysuria
Genital lesions in men typically occur on the glans or shaft of the penis, and the buttocks are occasionally affected.
Systemic complications are more common in women than men
Extragenital lesions, urinary retention, and aseptic meningitis occur in 20%,
The presence of more extensive local involvement, regional
lymphadenopathy, and fever generally distinguishes primary herpes
infection from recurrent disease.
Recurrent infection
The lesions usually occur roughly the same place each time. They may be precipitated by:1. Fever.
2. Respiratory tract infection.
3. UV radiation.
4. Menstruation.
5. or even stress.
The common sites include the face and lips (type I) and the genitalia (typeII).
The infection start with tingling, burning, or even pain, which last 2-24 hr followed by erythema and clusters of tense vesicles. Crusting occurs within 24-48 hr and the whole episode lasts about 12 days.