Bacterial
infections
Dr Qassim S. Al-Chalabi
F.A.B.H.S
Bacterial infections
The normal skin flora
•
Protects the skin from bacterial infections through bacterial
interference.
•
The resident skin flora consists of:
Staphylococcus species, e.g. S. hominis & S. epidermidis. Staph.
aureus
isn’t a member of resident skin flora except in anterior nares
or perineum and axilla (in 20% of individuals) & in lesional skin of
atopic dermatitis (90% of pts).
- Micrococcus species. - Aerobic coryneforms.
- Anaerobic propionibacterium species, e.g. P. acnes. commonly
inhabit the sebaceous hair follicles.
- Yeasts: pityrosporum.
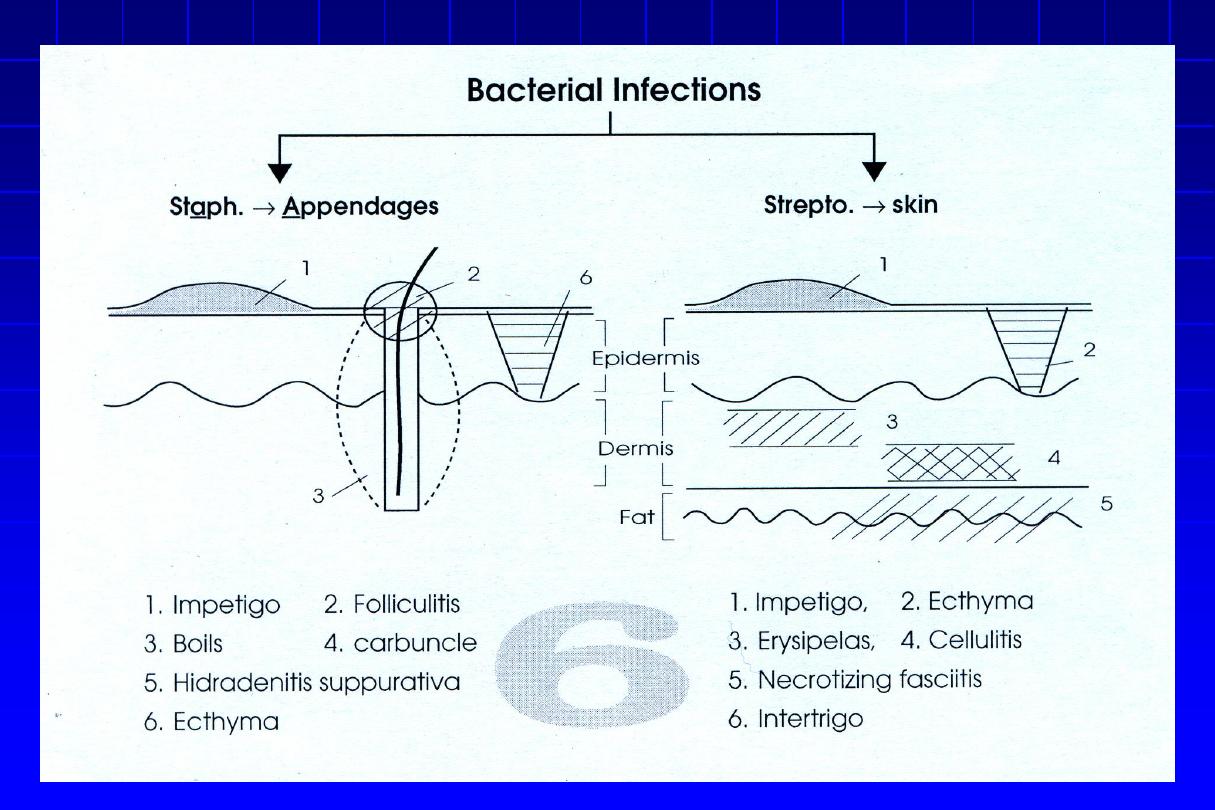
Impetigo contagiosum
•
Acute contagious superficial pyogenic infection of the skin.
•
Staph. Aureus and Streptococcus Pyogens
are the most
common cause of skin infections.
•
Impetigo occurs most frequently in early childhood,
although all ages may be affected. It occurs in the temperate
zone,
mostly during the summer in hot, humid weather
.
Predisposing factors for pyoderma
• Common sources of infection for children are
pets, dirty
fingernails, and other children in schools, daycare
centers, or crowded housing areas; for adults, common
sources include infected children and self-inoculation
from nasal or perineal carriage.
• Impetigo often complicates
pediculosis capitis, scabies,
herpes simplex, insect bites, eczema, and other itching
skin diseases.
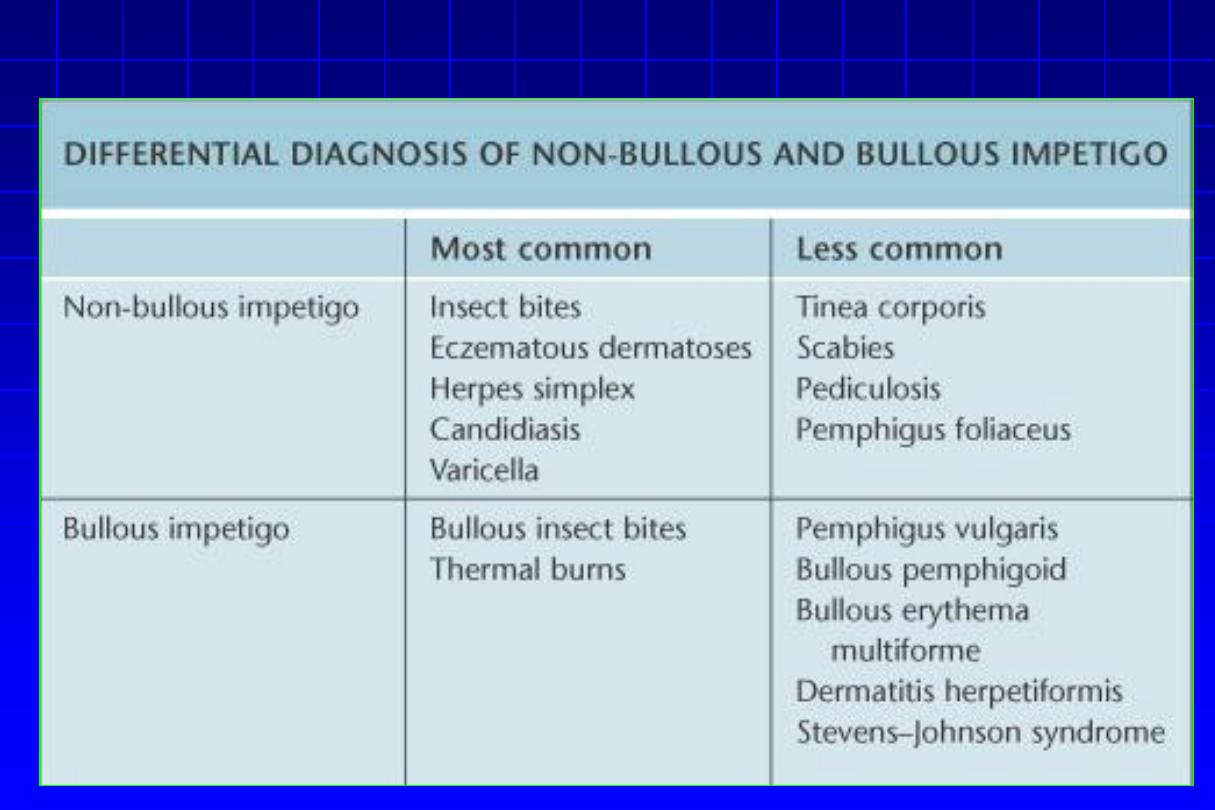
IMP
1- Non-bullous impetigo
•
Staph. aureus or group A stretp. or both
“mixed
infections”.
•
May arise as 1
ry
inf. or as 2
ry
inf. of pre-existing
dermatoses, e.g. pediculosis, scabies & eczemas.
•
An intact st. corneum is probably the most
important defense against invasion of pathogenic
bacteria.
Clinical feature
•
A thin-walled vesicle on erythematous base, that soon
ruptures & the exuding serum dries to form
golden-yellowish
(honey-color) crusts
that dry & separate leaving erythema
which fades without scarring.
•
Regional adenitis with fever may occur in severe cases.
•
Sites:
face & scalp (in pediculosis). Any part could be affected
except palms & soles.
•
Complications: Post-streptococcal acute glomerulo-nephritis
“AGN” especially in cases due to strepto. Pyogenes


Look for head lice for recuurent impetigo of the head
and neck
Non-bullous impetigo
– varieties (Cont’d)
•
Ecthyma
(ulcerative
impetigo):
adherent
crusts, beneath which purulent superficial
saucer-shaped ulcer occur. Healing occurs
after few wks, with scarring.
Site:
more on distal extremities (thighs & legs).

SSSS (Cont’d)
Treatment of impetigo
1. Treatment of predisposing causes,
e.g. pediculosis
& scabies.
2. Remove the crusts:
by olive oil or hydrogen
peroxide or soap and water.
3. Topical antibiotic ointment,
e.g. tetracycline,
bacitracin, mupiracin (Bactroban
®
), Fusidic acid
(Fucidin
®
).
SSSS
– treatment (Cont’d)
4. Systemic antibiotics are indicated
especially in the
presence
of
fever
or
lymphadenopathy,
in
extensive infections involving scalp, ears, eyelids
or if a nephritogenic strain is suspected, e.g.
penicillin, erythromycin & cloxacillin.
•
Azithromycin caps 500 mg daily for 3 days in
adults.
•
In erythromycin-resistant S. aureus: amoxicillin +
clavulanic a. (Augmentin
®
) 25 mg/kg/day.
2- Bullous impetigo
•
Staph. aureus through
staphylococcal toxin (exfoliatin).
•
Age:
all ages, but more common in childhood & newborn.
•
The bullae are
less rapidly ruptured
(persist for 2-3 days) &
become much larger. The contents are at first clear, later
cloudy, after rupture thin, brownish crusts are formed.
•
Site:
face is often affected, but the lesions may occur
anywhere,
including palms & soles.

Syndromes caused by staph. exotoxins
Staph. Scalded Skin Syndrome
“SSSS” (Ritter’s dis.)
•
It occurs mainly in infancy & childhood or rarely in adults
with renal failure or immunological incompetence.
•
The condition is usually caused by
a toxin produced by
staphylococcal infection elsewhere
(e.g. impetigo or
conjunctivitis). Staph. aureus of phage group II, mostly type
71, which elaborates two exotoxins, epidermo-lytic toxins A
& B (ET-A & ET-B).
SSSS (Cont’d)
Clinically
•
it begins suddenly with fever, diffuse, tender,
red skin simulating
“scald”. Large flaccid bullae
occur
rupture immediately. Large sheets of
superficial epidermis separate & exfoliate. There
is sparing of the palms, soles, and mucous
membranes. Nikolsky sign is positive. Healing
occurs usually within 7-14 days with or without
treatment. Usually good prognosis.
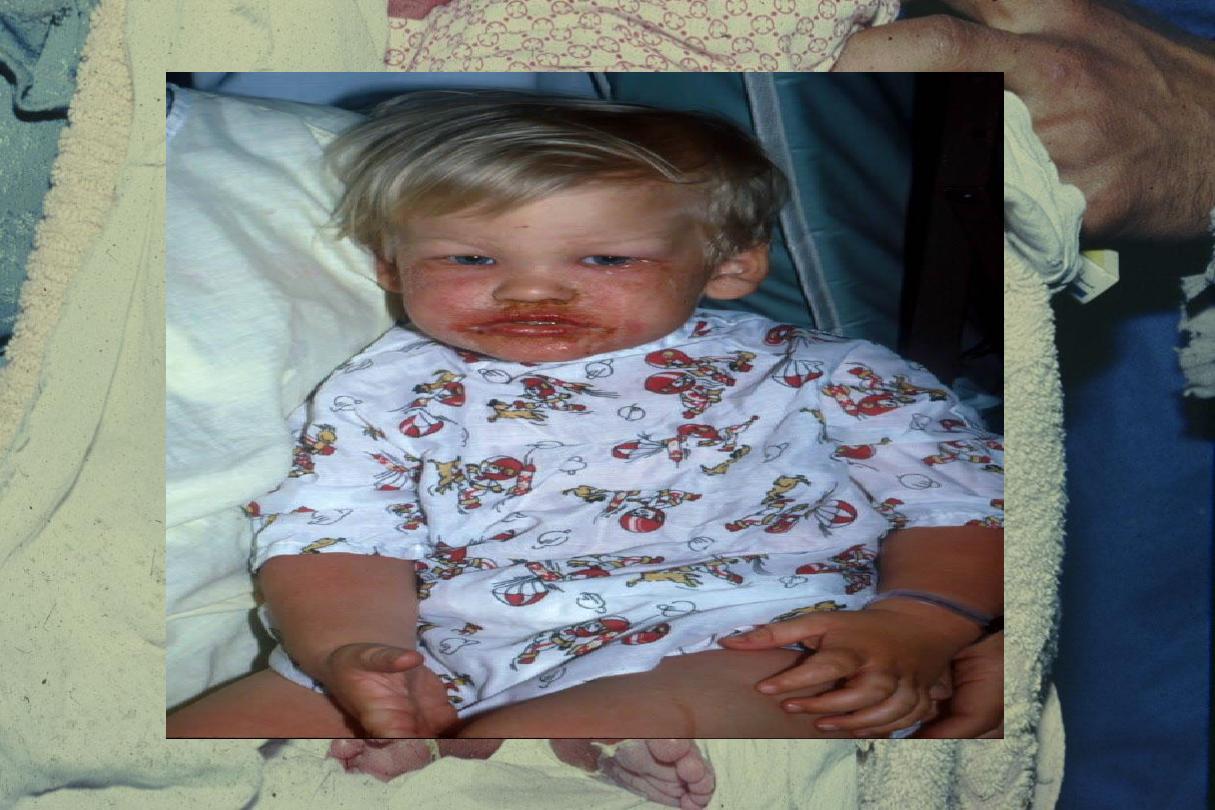
SSSS
– clinically (Cont’d)
Treatment (good prognosis)
•
Systemic & topical antibacterial agent:to
secondary infection.
•
Supportive
treatment:
iv
fluid,
electrolyte
disturbance.

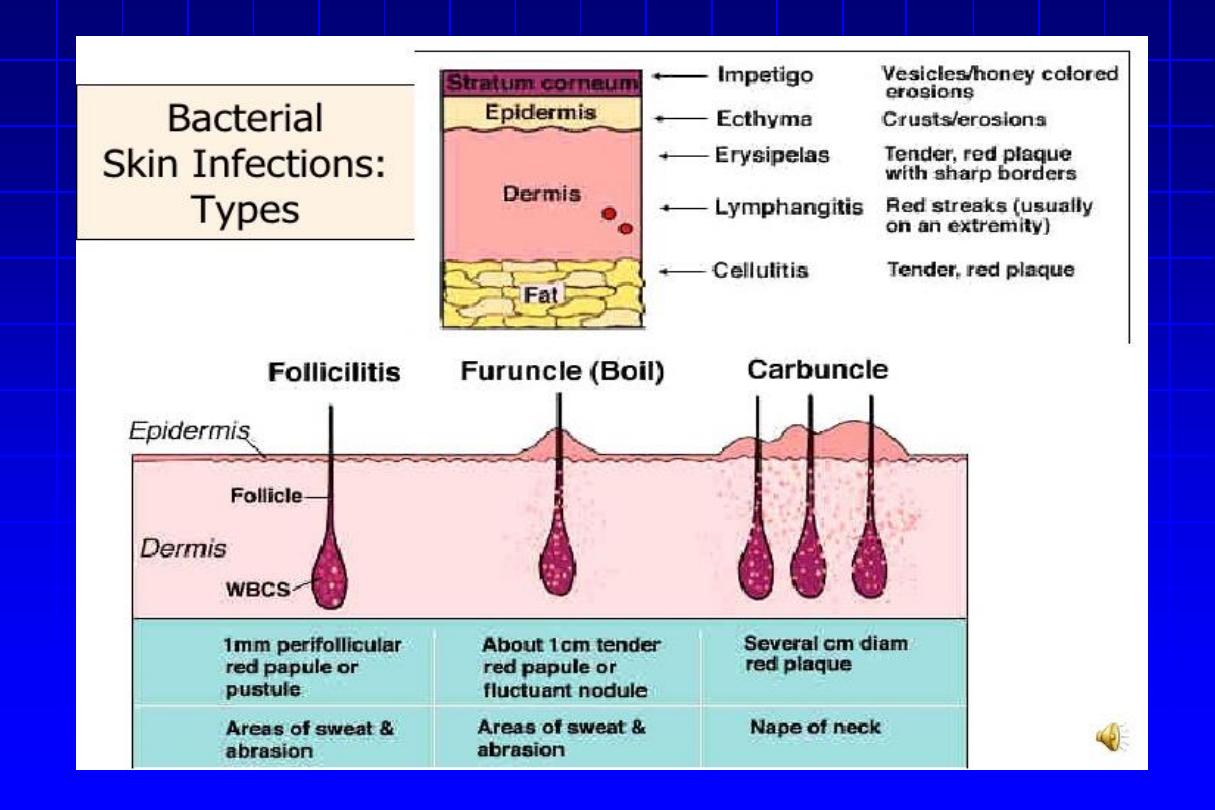
Erysipelas
It’s due to infection of the dermis & upper subcutaneous
tissue by
group A streptococci.
The organism reaches the dermis through a wound or small
abrasion.
Site
: Leg & face.
It begins with high fever & rigors
. There is a well-demarcated
erythematous, hot, tender swelling of the skin. The surface
may
show
vesicles
or
bullae.
Lymphangitis
&
lymphadenopathy are frequent.


Erysipelas (Cont’d)
Complications
•
Recurrences may lead to lymphedema.
•
Subcutaneous abscess.
•
Septicemia.
•
Nephritis.
Differential Diagnosis:
1.Contact dermatitis
from plants, drugs,dyes.
2.Angioneurotic edema
;.
3.A butterfly pattern on the face may mimic
lupus erythematosus
4. Erysipeloid:
is caused by
Erysipelothrix rhusiopathiae
. is present on dead
matter of animal origin(swine, turkey, slime of saltwater fish, on crabs, and
on other shellfish) The most frequent form of erysipeloid is a purplish
marginated swelling on the hands.
The majority of the mild cases of erysipeloid run a self-limited
course of about 3 weeks. Penicillin, 1 g/day for 5–10 days, or ampicillin,
500 mg four times daily, is the best treatment for localized disease.
Cellulitis
•
It is an acute inflammation of subcutaneous
tissue. Currently, erysipelas is regarded as a
form of cellulitis rather than a distinct entity.
•
Cellulitis is usually caused by gp A strept.,
but staph. aureus may be implicated.
Cellulitis (Cont’d)
•
Clinically:
the edge is diffuse with indurated, red, tender area
of the skin.
•
Recurrent strept. cellulitis or erysipelas
is due to lymphatic
damage & venous insufficiency.
•
Treatment of erysipelas & cellulitis :
•
Systemic antibiotics,
especially penicillin, e.g. benzyl
penicillin 600-1200 mg IV/6 hrs or erythromycin.
•
Rest, analgesics

Scarlet Fever
•
Pyrogenic exotoxin (erythrogenic toxin)
– mediated: types A,
B, and C
• Associated with
streptococcal pharyngitis
• Children 2–10 years of age.
•
Enanthem
: Exudative pharyngitis,
strawberry tongue
•
Exanthem
: Diffuse erythematous eruption with
“sandpaper”
texture, beginning on head and neck, and then generalizes,
sparing palms/soles;
circumoral
pallor
;
Pastia’s lines
(linear
petechial patches in axillae and antecubital fossae)
•
Desquamation of palm&sole
upon resolution of exanthem.

Folliculitis
= inflammatory disease of the hair follicles, which may be
infectious or non-infectious.
Superficial folliculitis
It isn’t always infective in origin, physical or chemical injury or
adhesive plasters may be associated with folliculitis,
usually sterile.
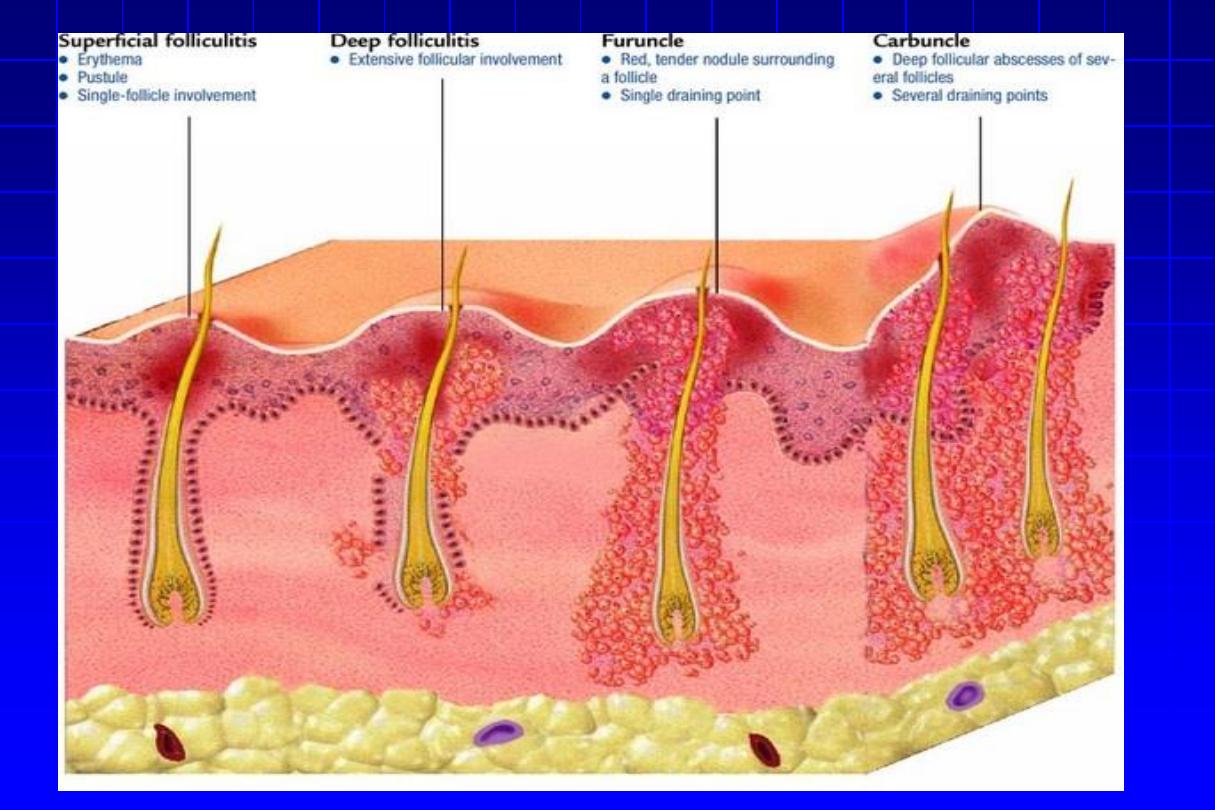
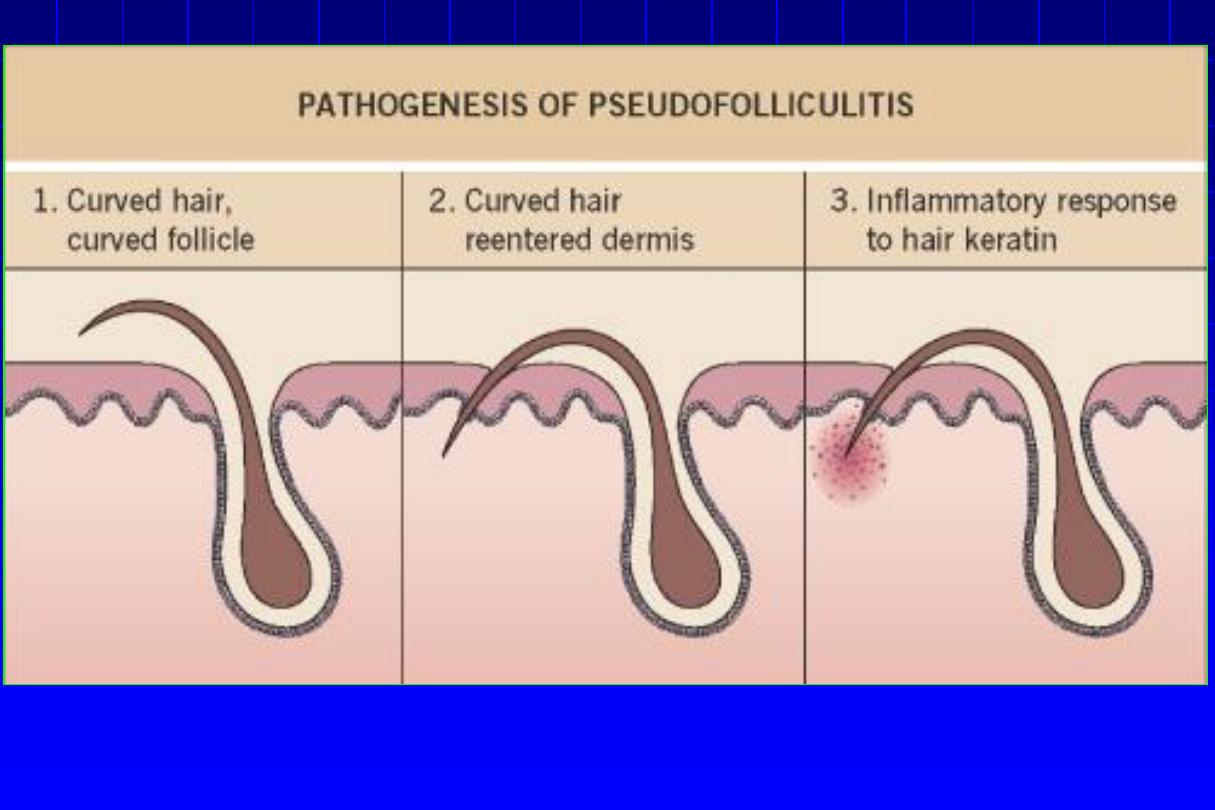
Superficial folliculitis (Cont’d)
1. Follicular impetigo of Bockhart:
a dome-
shaped pustule at the orifice of a hair follicle
that heals within 7-10 days. Topical steroids
are a common predisposing factor.
2. Pseudofolliculitis
of
the
beard:
from
penetration into the skin of sharp tips of
shaved hairs.

Deep folliculitis
1. Sychosis
“Folliculitis barbae”
•
Red follicular papules or pustules centered on a
hair, usually remain discrete over the beard or
upper lip, but may coalesce to produce raised
plaques studded with pustules later will be
scaring and hair loss.
•
DD:
pseudofolliculitis of the beard, Tinea barae.

Deep folliculitis (Cont’d)
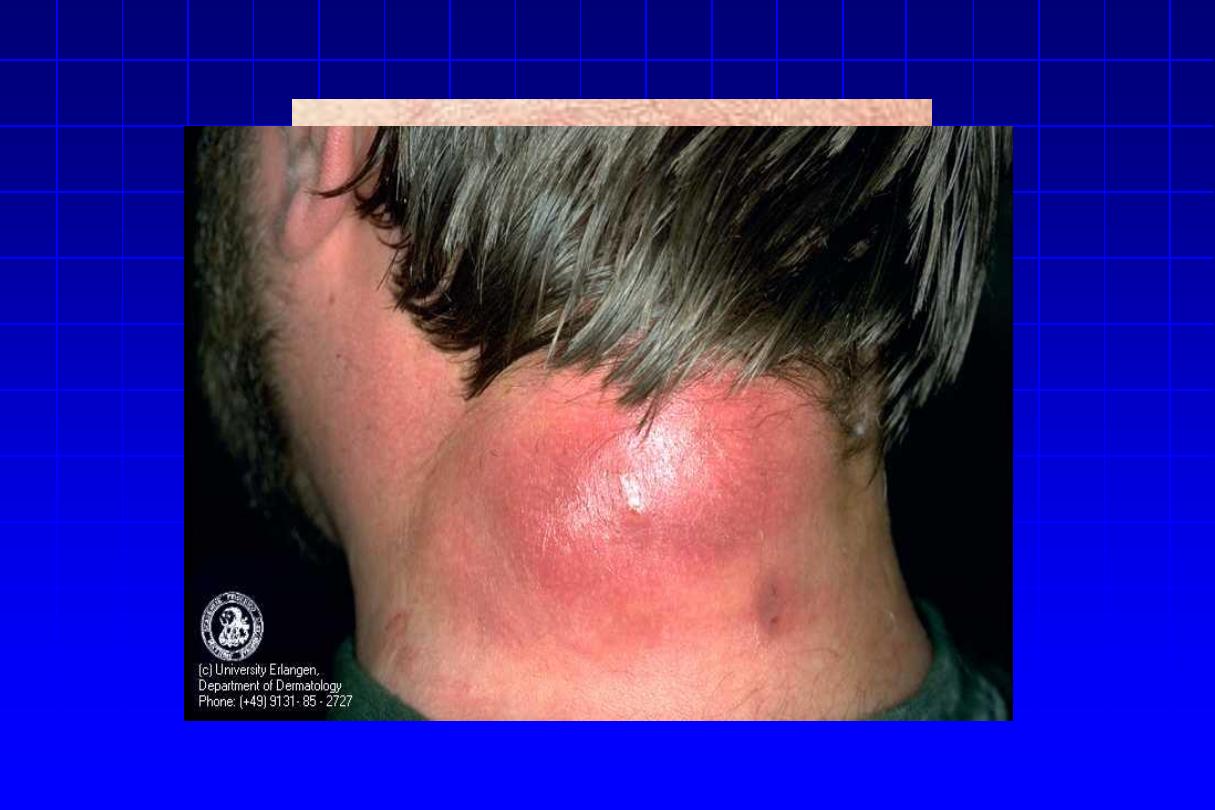
2. Furunculosis
“Boils”
•
It is a staphylococcal infection similar to, but deeper than
folliculitis & invades the deep parts of the hair folliculitis.
•
A tender red nodule enlarges, and later may discharge
pus and its central ‘core’ before healing to leave a scar.
Fever and enlarged draining nodes are rare
.
•
Occasionally several closely grouped boils will combine to form a
carbuncle
. The carbuncle usually occurs in diabetic cases. The site
of predliction is the back of the neck.
Other causes of folliculitis
•
Gram negative folliculitis with antibiotic treatment
of Acne Vulgaris.
•
Pityrosporum folliculitis.
•
Eosinophilic folliculitis in HIV infections.
•
Pseud. aeruginosa folliculitis.
Hidradenitis suppurativa “Apocrinitis”
•
is a chronic disease characterized by recurrent abscess
formation, primarily within the folded areas of skin that
contain both terminal hairs and apocrine glands
.
•
It begins after
puberty, commonly in females.
•
Sites:
axillary & anogenital regions where apocrine glands
are present. There is small red, tender, subcutaneous
nodules that become fluctuant, becomes chronic & indolent
due to subcutaneous extension. Rupture & sinuses
discharging pus occur. Healing occurs with scar formation.

Hidradenitis suppurativa (Cont’d)
Treatment
•
Appropriate antibiotics for 2 wks, e.g. erythromycin and
metronidazole or clindamycin or long term of tetracyclines.
•
Systemic corticosteroids, e.g. prednisolone 60 mg daily.
•
Oral contraception containing 50 mg ethyl estradiol may be
useful.
•
Isotretinoin for 4 months .
•
Surgery in refractory resistant cases.
Erythrasma
•
It is chronic, localized superficial infection of skin by
Corynebacterium Minutissimum
•
There is sharply-defined but irregular brown, scaly patches
usually localized to groins, axillae, toe clefts or may cover
extensive areas of trunk & limbs. Obesity & DM may coexist.
•
It gives
coral-red fluorescence under
Wood’s light.
•
Topical treatment with antifungal agents for 2 weeks or
topical fusidic acid.
•
Erythromycin orally.



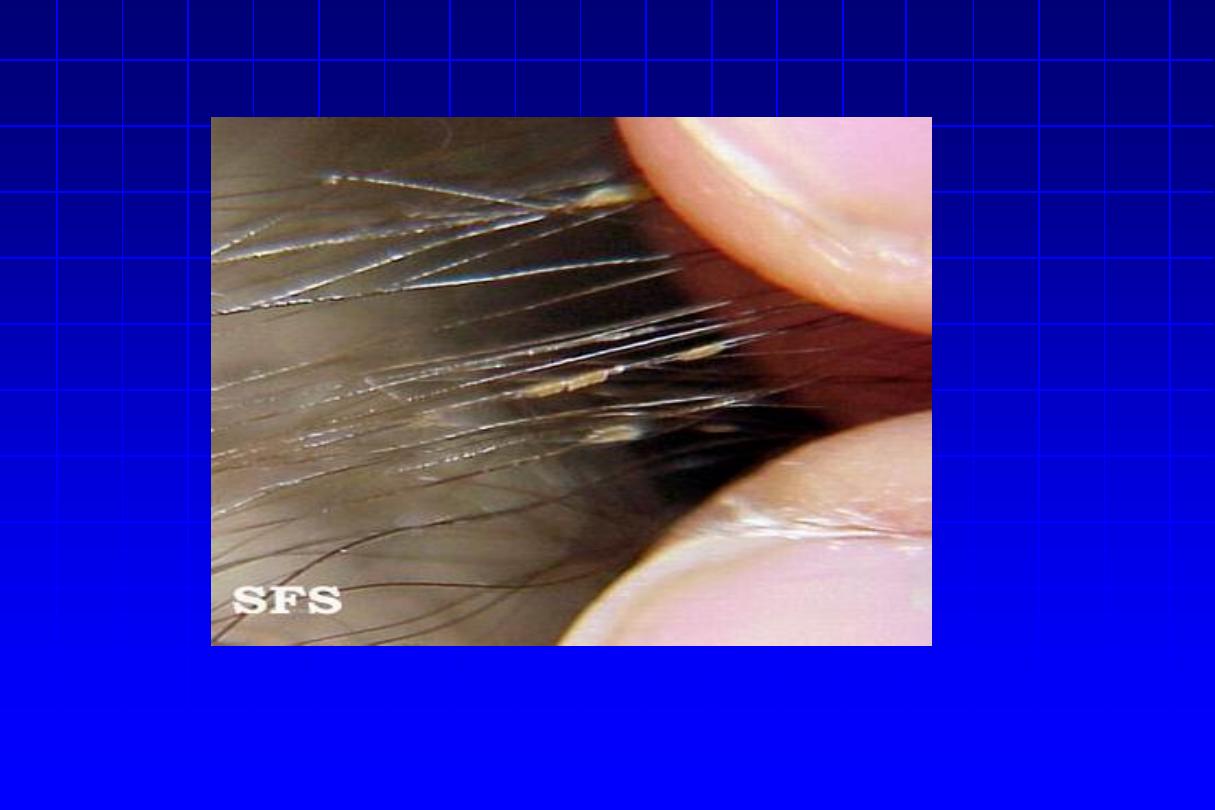
Trichomycosis axillaris
•
Causative organism
: Corynebacterium tenuis
•
Characteristic features
: Yellowish brown concretions on
axillary hair shafts
• Treatment: Shaving; topical erythromycin.
Pitted keratolysis
The combination of unusually sweaty feet and
occlusive shoes encourages the growth of organisms
that can digest keratin. The result is a cribriform
pattern of fine punched-out depressions on the
plantar surface, coupled with an unpleasant smell.

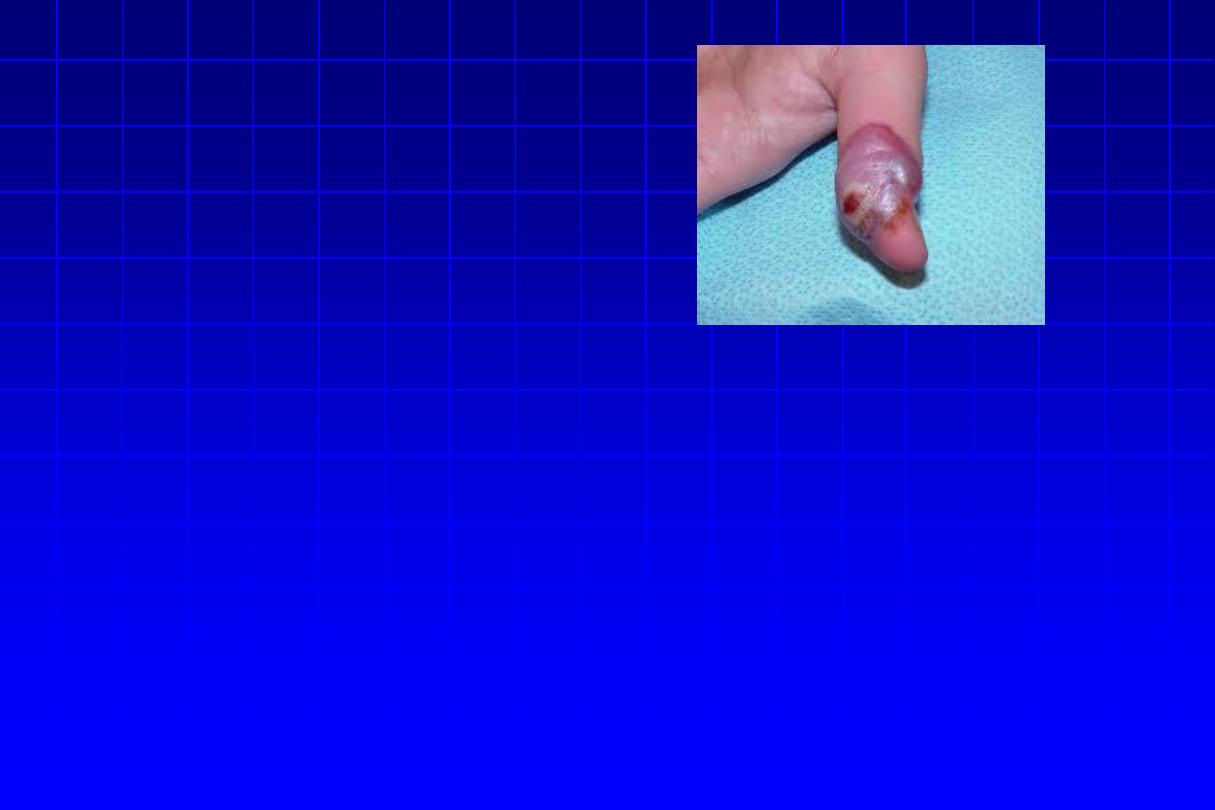
Anthrax (Malignant Pustule)
• Acute disease in humans and animals caused by
Bacillus anthracis , a Gram-positive spore-
forming rod.
• Primarily caused by contact with infected wild or
domestic animals, or their products (e.g., wool,
goat, animal hides, bones, etc.)

Clinical picture
• Clinical forms: cutaneous, pulmonary, and GI.
• IP= ultra short 1-5 days patients may experience
low-grade fever and malaise
• Primary lesion is a “malignant pustule,” which
begins as a painless papule, evolves into a
hemorrhagic bulla with surrounding nonpitting
edema, and ultimately forms a characteristic black
eschar surrounded by vesicles.
• Regional lymph glands become tender an
enlarged, and frequently suppurate.

DDGX:
ORF
Rx:
• (i) Bioterrorism associated: ciprofloxacin or
doxycycline
• (ii) Conventional anthrax: Penicillin
