Mycobacterial
Infections
Dr Qassim S. Al- Chalabi
Mycobacterial infections
•
They include many pathogens of man, the
most important of which are:
M. tuberculosis.
M. leprae.
Atypical mycobacteria.
Cutaneous TB
•
The resident
Cutaneous TB
is caused by M. tuberculosis,
an acid and alcohol-fast bacillus.
•
Recently, there is increase in incidence of cutaneous TB
due to HIV epidermis, a rise in resistant strains of M.
tuberculosis , a decline in TB control efforts and drugs
which decrease immunity.
•
Classification of cutaneous TB
I) Inoculation TB from an exogenous source
•
Tuberculous chancre.
•
TB verrucosa cutis.
II) Secondary TB from an endogenous source:
•
Contiguous spread: scrofuloderma.
•
Autoinoculation: orificial TB.
IMP
Classification of cutaneous TB (Cont’d)
III) Hematogenous TB
•
Lupus vulgaris.
•
Acute miliary TB.
•
Tuberculous gumma.
IV) Tuberculids
•
Papulo-necrotic tuberculids.
•
Lichen scrofulosorum.
•
Erythema induratum (Bazin)
Primary inoculation complex
“Tuberculous chancre”
•
Results from
exogenous
direct inoculation of
M. tuberculosis into skin or mucosa of an
individual not previously infected with TB
,
mainly children.



Primary inoculation complex (Cont’d)
•
Usually
on
face
or
extremities
as
asymptomatic brownish-red papule or nodule
that erodes to form an indurated, non-tender
ulcer with sharply demarcated undermined
edges.
•
There is prominent regional lymphadeno-
pathy.
•
Tuberculin test is
–ve
.
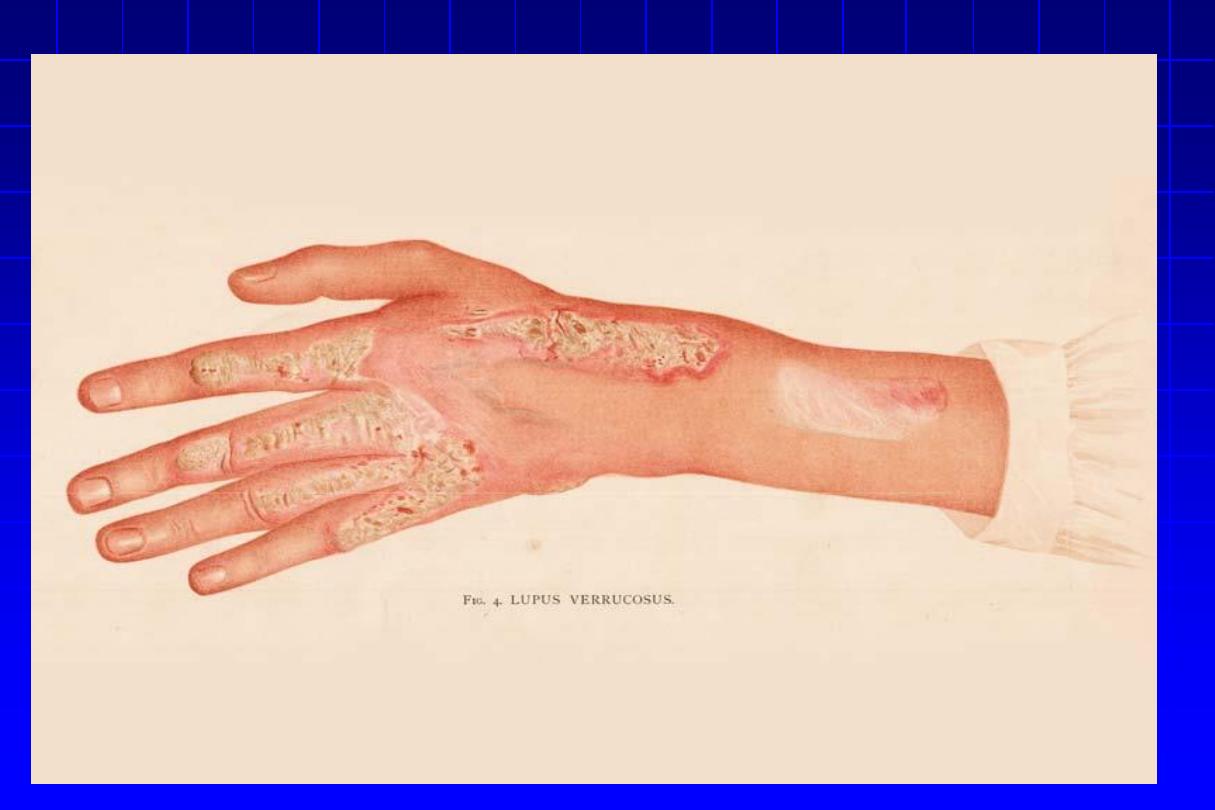
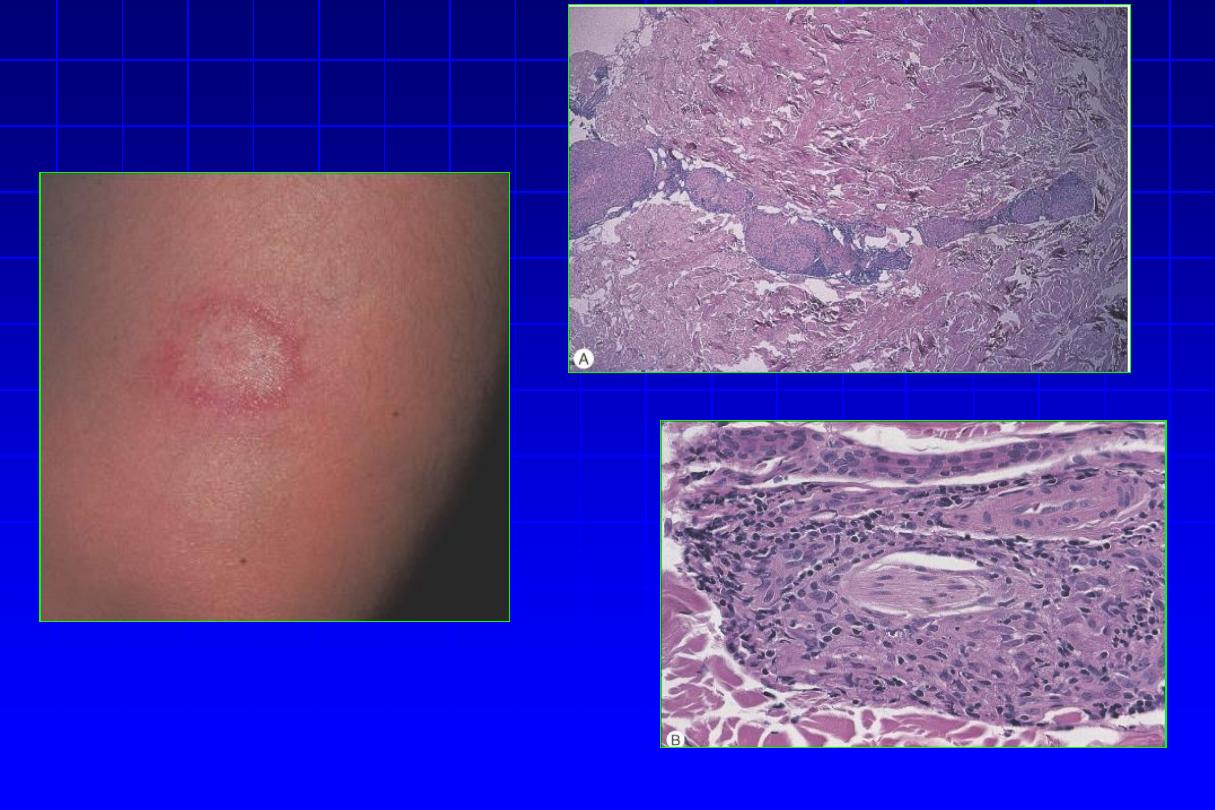
Tuberculosis verrucosa cutis “TVC”
Warty
TB(
The prosecutor’s wart)
•
Results from
exogenous
direct inoculation of M.
tuberculosis into the skin of an
individual with high
degree of immunity.
•
Usually on hands, knees & ankles as asymptomatic
papule
that
slowly
evolves
into
a
warty
hyperkeratotic irregular plaque that enlarges by
peripheral extension.
(LN. not enlarged)
Scrofuloderma
•
From
direct extension to the skin
from
underlying tuberculous focus, usually a
LN but sometimes a bone, joint or
epididymis.
•
Tuberculin
sensitivity
is
usually
pronounced
.
Scrofuloderma (Cont’d)
•
A bluish-red nodule that breaks down to form an
ulcer with bluish undermined edges & floor covered
with soft granulation tissue.
•
Progression & scarring produce irregular adherent
masses.(cord like lesion)
•
Healing
occurs
with
characteristic
puckered
scarring.

Tuberculosis cutis orificialis
•
In the
mucosa or the skin adjoining orifices
in a patient with advanced internal TB
with
weak tuberculin reaction
.
•
Painful shallow ulcers with undermined
bluish edges with no tendency to heal
spontaneously. It occurs around the mouth,
anus or genitalia.
Lupus vulgaris “LV”
•
The
most common type of cutaneous TB
.
•
It starts in
childhood
& progresses very slowly.
•
Tuberculin test is ++ve
.
•
It appears commonly on face, neck (90% of cases)
or buttocks & limbs, as sharply demarcated,
serpiginous reddish-brown soft plaque composed
of deep seated nodules.
Lupus vulgaris (Cont’d)
•
Slow
peripheral
extension
leading
to
thin,
contractile & unhealthy scar (i.e. new lesions
appear in areas of atrophy).
•
Scarring & destruction of underlying structures as
nose or ear cartilage usually occurs with various
mutilations as microstomia & ectropion,
… etc. SCC
& less commonly BCC may develop at the margin.
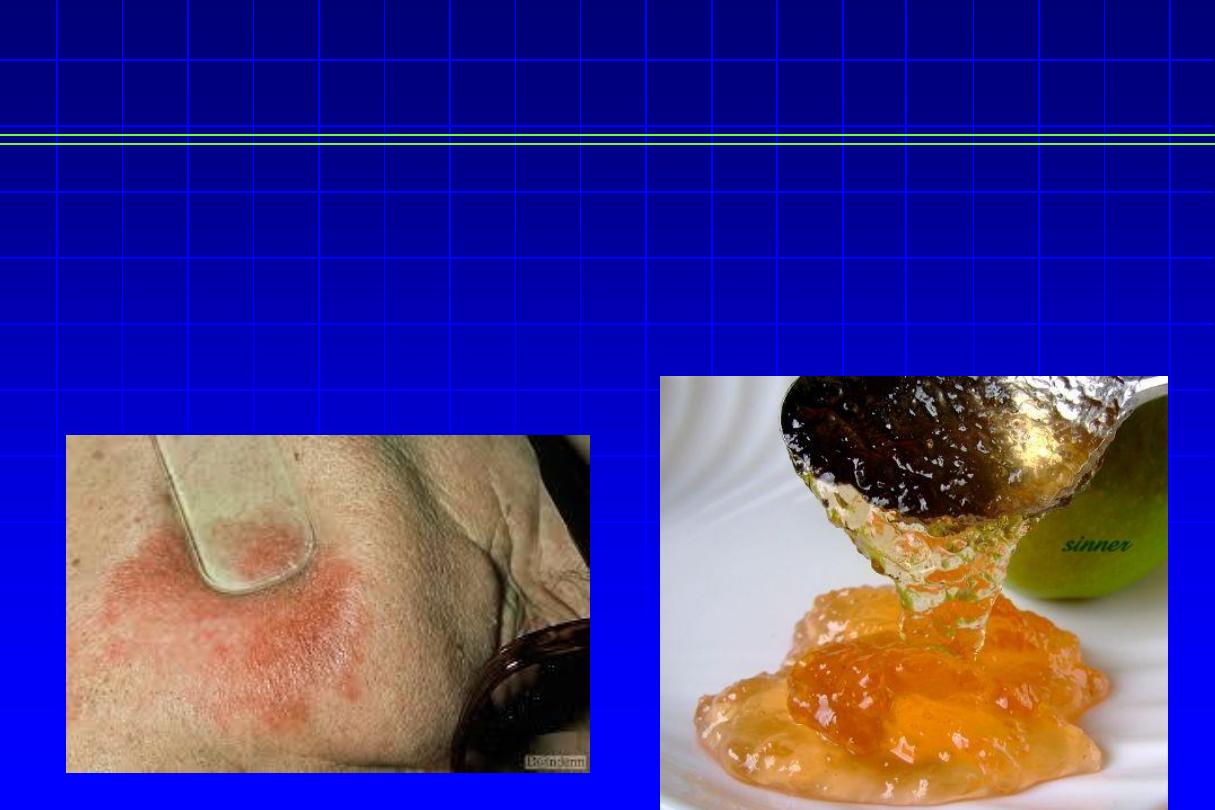
Lupus vulgaris (Cont’d)
Diascopy
test
•
Pressing of LV lesions with a glass slide, to diminish vascularity,
yellowish-brown spots appear
“apple jelly”
nodules.


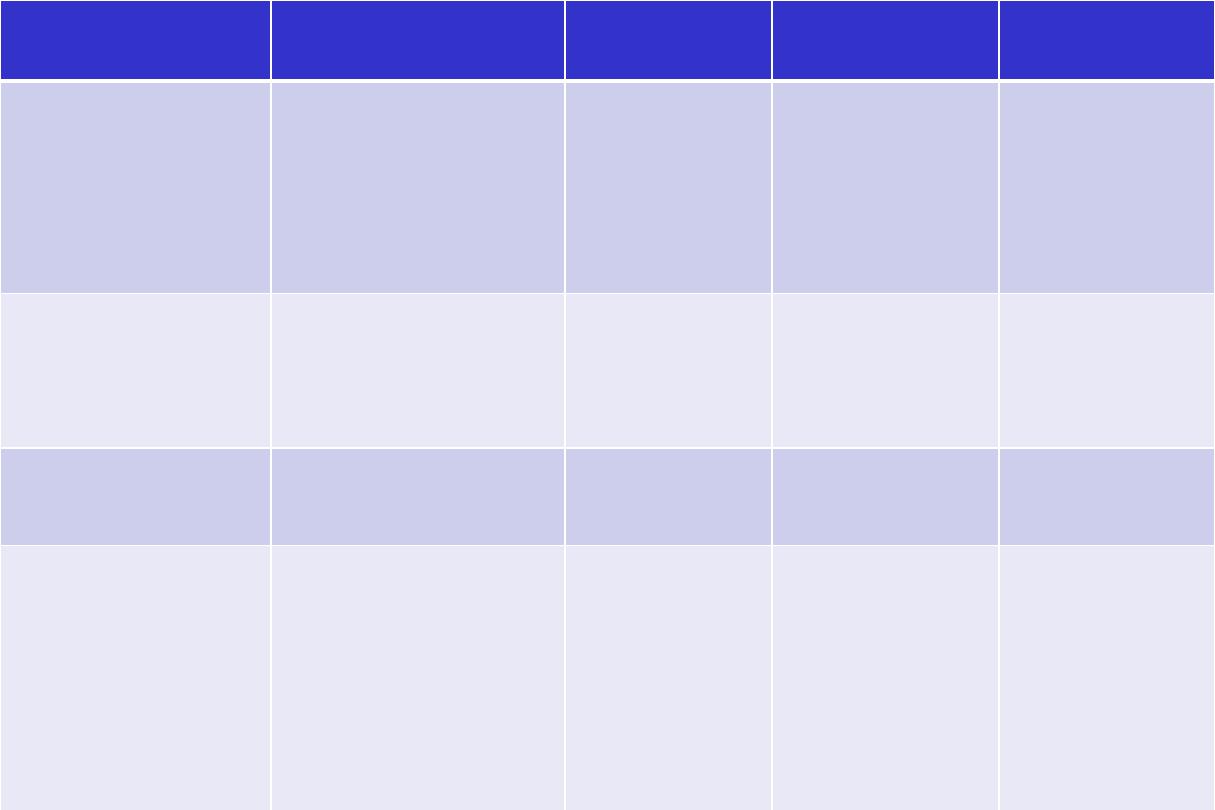
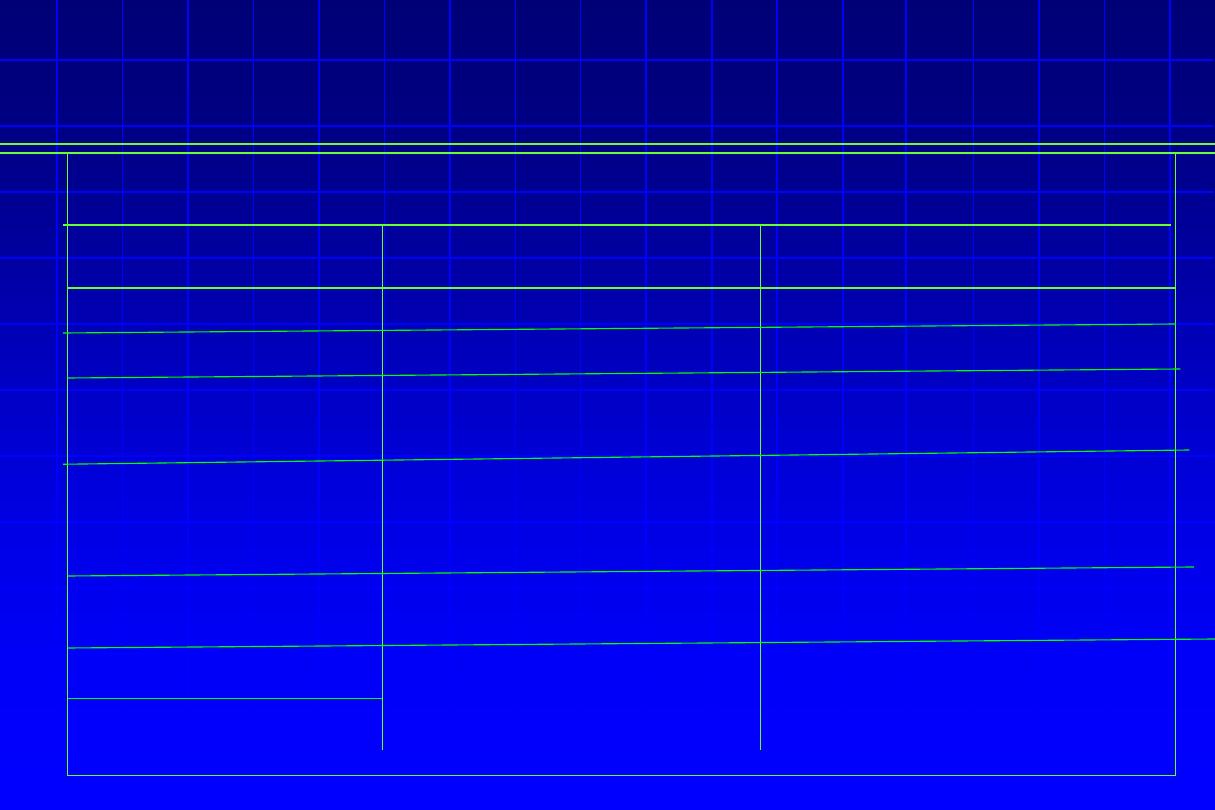
Tuberculosis
Cutis Orificialis
Scrofuloderma
Lupus Vulgaris
Tuberculosis Verrucosa
Cutis
Tuberculous Chancre
Autoinoculation
from underlying
advanced visceral
tuberculosis
Contiguous spread
onto skin from
underlying
tuberculous infection
Hematogenous,
lymphatic, or
contiguous
spread from
distant site
of tuberculous
infection
Exogenous reinfection
Primary (exogenous)
inoculation
Sensitized host
with diminishing
immunity
Sensitized host with
low immunity
·
Sensitized host
with
moderate to high
immunity
Sensitized host
with strong
immunity
Non-sensitized host
·
Multi-bacillary
Multi- or pauci-
bacillary
Pauci-bacillary
Paucibacillary
Pauci- or Multibacillary,
Punched-out
ulcers with
undermined
edges· On
mucocutaneous
junctions of
mouth, genitalia
Subcutaneous
nodules with
purulent or caseous
drainage· May
develop sinuses and
ulcers with
granulating bases·
Occurs over cervical
LN
Brownish-red
plaque· “Apple-
jelly” color on
diascopy.
Head/neck
involvement
in 90% of cases
Slowly growing verrucous
plaques with irregular
borders Typically on hand
Painless red-brown
papule that ulcerates
Tuberculous primary
complex: regional
lymphadenopathy, 3-8
weeks post infection
Treatment of TB cutis
•
Isoniazid (INH),
usually up to 300 mg daily in adults,
orally for 6 ms.
•
Rifampicin,
<50 kg
450 mg & > 50 kg
600 mg
daily orally for 6 ms.
•
Pyrazinamide,
for the 1
st
2 ms.
•
Ethambutol,
for the 1
st
2 ms (15 mg/kg) daily.
All drugs are taken on an empty stomach once daily.
Drug regimens
•
Initial phase, for 2-3 months using at
least 3 drugs (e.g. INH, rifampicin and
ethambutol).
•
Continuation phase, for several months
usually with 2 drugs only (e.g. INH &
rifampicin).
Tuberculids
• Tuberculids are a group of skin eruptions
associated with an underlying or silent focus
of TB.
• The bacilli are absent from the lesions. The
lesions are bilateral & symmetrical occurring in
crops with a tendency to spontaneous healing.
•
Papulonecrotic tuberculids
•
Recurring symmetric crops of non-itchy, dusky-red papules on extensor
surface of extremities, face, ears & buttocks which undergo central
necrosis & heal with pigmented pitted scars.
•
Lichen scrofulosum
•
Grouped, closely set, minute lichenoid, slightly scaly, reddish-brown,
often peri-follicular papules. They commonly occur on the trunk & heal
without scarring.
•
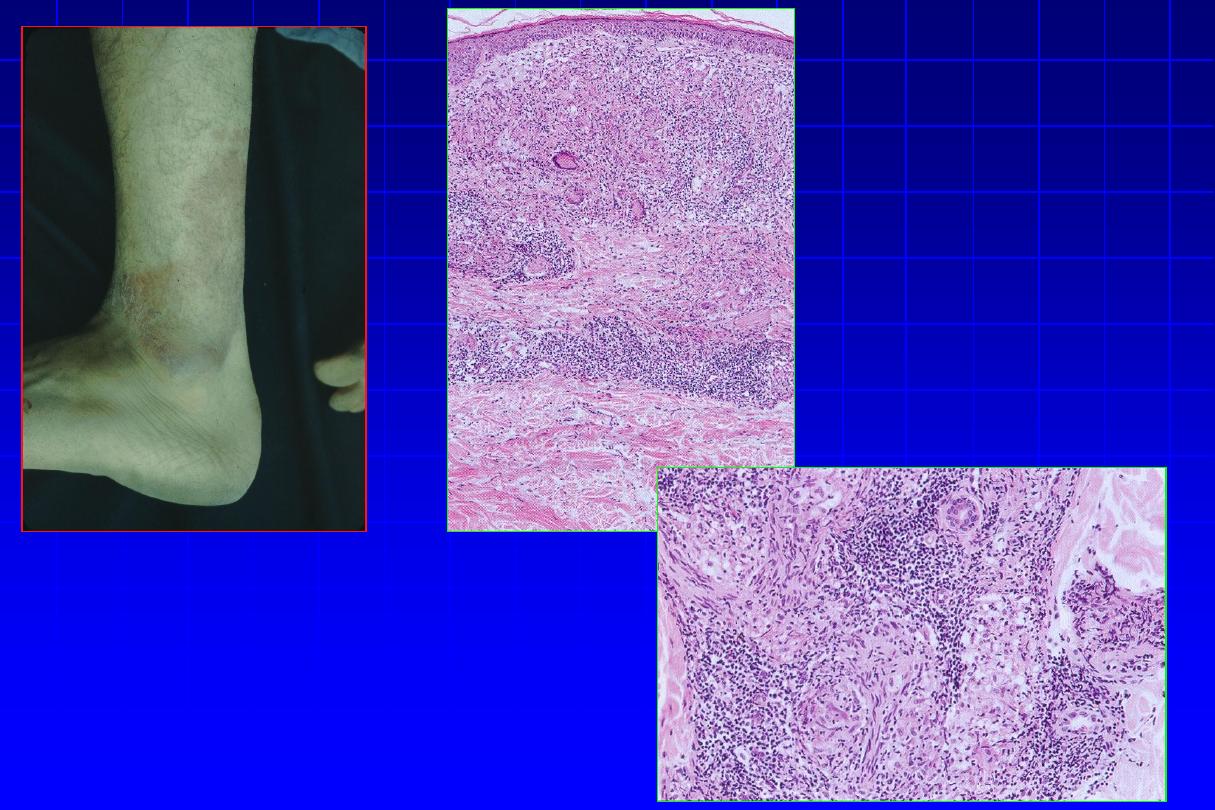
Erythema induratum
“of Basin’s”
•
deep purplish ulcerating nodules occur on the backs of the lower legs, usually in
women with a poor ‘chilblain’ type of circulation.
Leprosy
(Hansen’s disease)
Leprosy
(Hansen’s dis.)
•
It is a chronic infectious dis., affecting primarily the
peripheral nerves & secondarily the skin, mucous
membranes & internal organs.
•
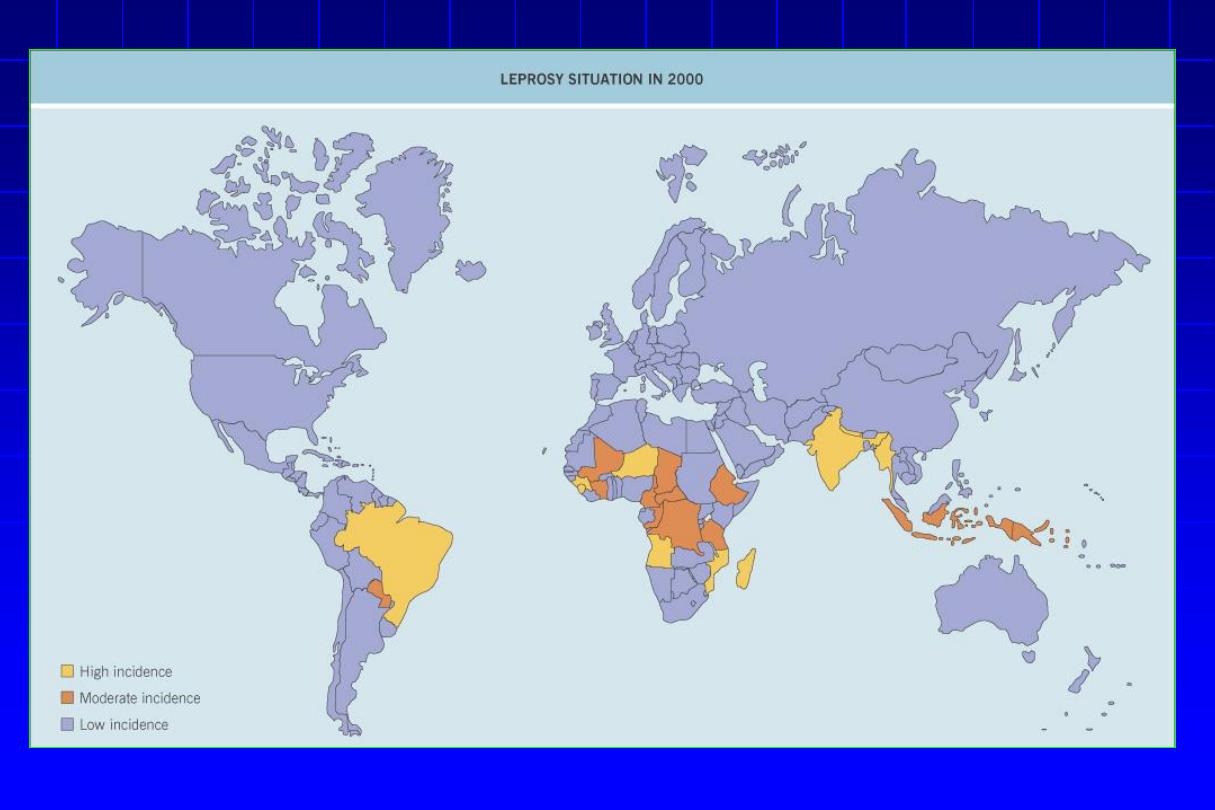
More prevalent in tropical & subtropical areas of
Africa, south east Asia & Latin America. The
estimated no. of leprosy cases in the world
after
the introduction of multidrug therapy
“MDT” from
12 million in 1980
’s to 2.7 million in 1994.
Etiology
Leprosy (Cont’d)
•
Mycobacterium leprae
which is an obligate intracellular
parasite. It could be stained by Ziehl-Neelsen method where
it is an acid-fast bacillus
“AFB”..
•
It
doesn’t grow
in usual media, however can be inoculated in
mice foot pads & in aramdillo.
•
M. leprae multiplies slowly, so leprosy develops slowly in ms
& yrs as compared with hrs & days in case of bacterial dis.
Mode of infection
Leprosy (Cont’d)
•
Through prolonged close contact of susceptible individual with an open
case of leprosy (i.e. untreated pts with multibacillary leprosy with +ve
nasal scrapings).
•
Infection may occur through droplet air-borne inf., contact with ulcerated
lesions, blood borne.
•
It can be transmitted via the placenta.
•
Genetic predisposition plays an important role.
•
Incubation period=
2-5 years.
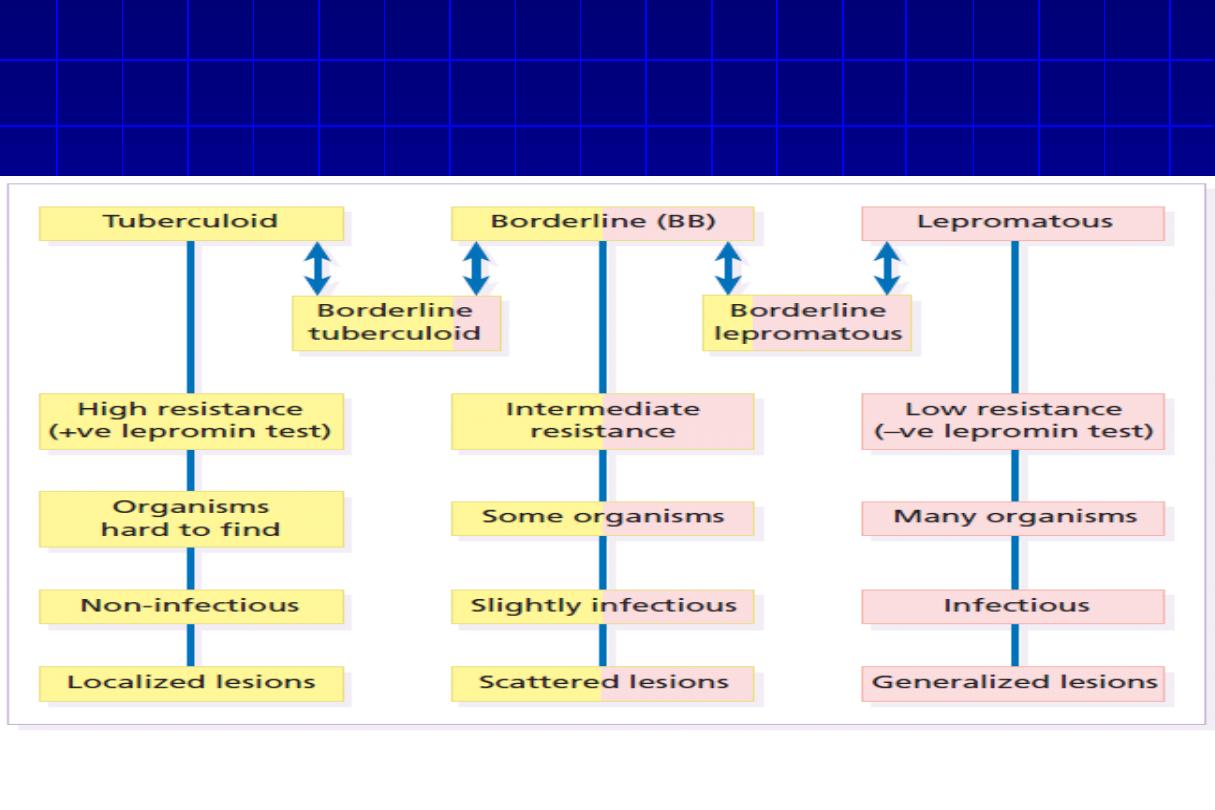
Classification
Lepromatous Leprosy.
Tuberculoid Leprosy.
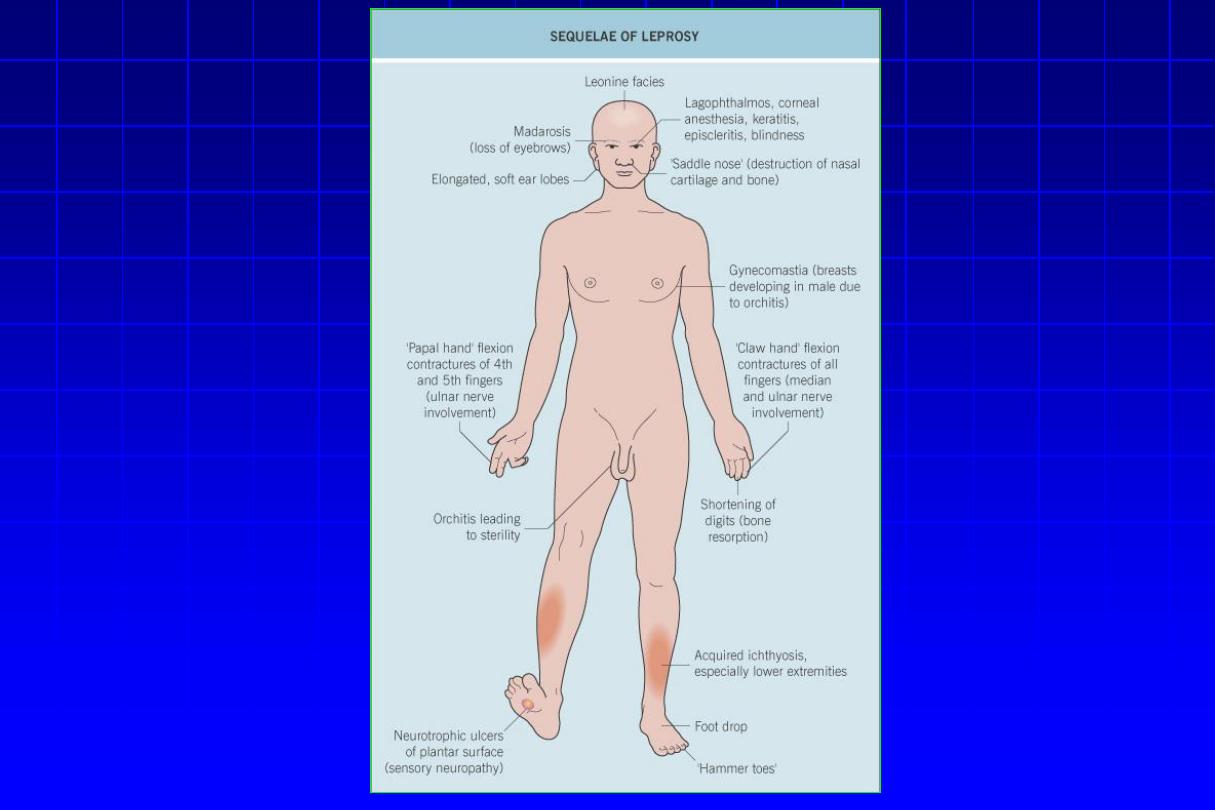
Clinical features
Many organ except GIT ,CNS and lung
Skin & nerve
Structure
involvement
Innumerable, widespread, symmetrical
5 or less (mainly face)
asymmetrical
No. of lesions
Macules, papules & nodules, thickness of
face (leonine facies), loss of eyebrow,
alopecia
Sharply marginated
hypopigmented macule,
slightly raised purplish rim,
hairless
Shape of lesion
Most peripheral nerves thickened
Thickened in vicinity of lesion
(great auricle, ulner radial
nerve)
Involvement of
nerve
Glove & stocking anesthesia, trophic ulcer of
periphery & muscle paralysis
Hypoaesthesia & loss of
sweating in lesion
Manifestation of
nerve involvement
Nasal crusting , epistaxes , saddle nose,
keratitis, infertility
None
Other
manifestation
Yes
No
Infectious
Leprosy (Cont’d)
•
Skin smears.
•
Nasal scrapings.
•
Skin biopsy
•
Nerve biopsy
•
Lepromin
test:
is
a
non-specific
test
of
delayed
hypersensitivity reaction, which is of value in classifying a
case of leprosy. It is an important prognostic test and is
not
a diagnostic one
. The test is strongly positive in TT type,
weakly positive in BT and is negative in BB, BL and LL types.
Diagnosis of leprosy

• Lepromatous Leprosy






Multi-
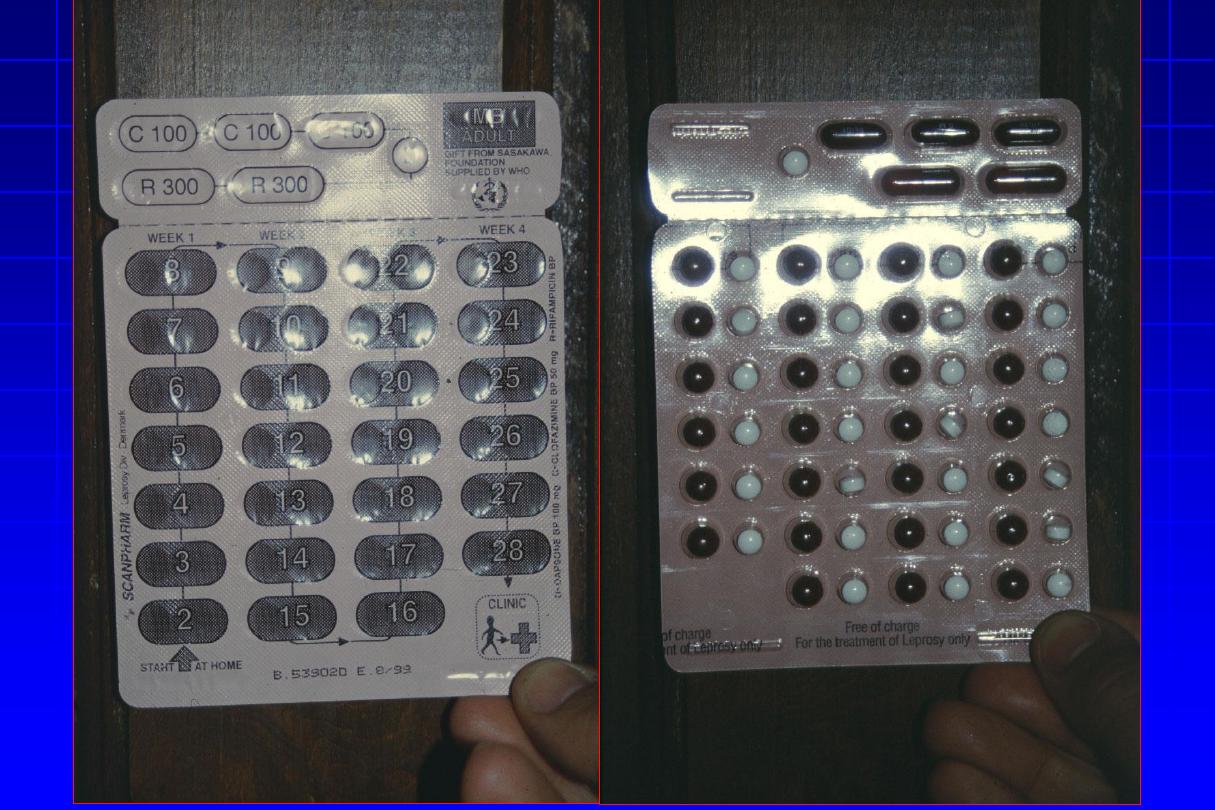
drug therapy (Cont’d)
Paucibacillary
Multibacillary
•
Daily (taken at home)
Dapsone 100 mg
•
Once a month (taken
under
supervision)
Rifampicin 600 mg
•
6 months
•
Daily (taken at home)
Dapsone 100 mg +
clofazimine 50 mg
•
Once a month (taken
under
supervision)
Rifampicin 600 mg +
clofazimine 300 mg
•
At
least
2
years,
preferably until
–ve skin
smears are obtained.
•
Regimen
•
Duration of ttt
Reaction in leprosy
Two types of reactions may occur:
Type I reaction
Type II reaction
Type of leprosy
Precipitating factor
Cause
Clinical features
Systemic
disturbances
Associated features
•
Mostly borderline
•
Drug
•
Change in cell-
mediated immunity
•
Signs of acute
inflammation of
existing lesions
•
Unusual
•
Nerve swelling with
pain & tenderness
•
Mostly LL & BL
•
Drug & pregnancy
•
Immune complex
syndrome
•
Erythema nodosum
leprosum (ENL)
•
Fever, malaise, etc. are
common
•
Oedema of hands &
feet, iritis, mild nerve
damage
Treatment of leprosy (Cont’d)
II) Treatment of reactions
•
Precipitated factors, e.g. immunization,
pregnancy & intercurrent inf. should be
avoided.
•
Chemotherapy is continued at the usual
dosage.
•
Mild reaction: aspirin 600 mg/4-6 hrs or
chloroquine 150 mg/8 hrs.
Treatment of leprosy (Cont’d)
Type I
•
Prednisolone starting at 50-80 mg daily &
gradually reducing the dose especially in
severe cases.
Type II
•
Thalidomide 400 mg at night, never to
women in child-bearing period due to its
teratogenic effects.
Treatment of leprosy (Cont’d)
Type II
(Cont’d)
•
Clofazimine, increasing the dose to 300 mg
daily & reduced gradually to normal within 2
ms to avoid toxicity.
•
Prednisone 30 mg tab. initially, if thalidomide
is contraindicated.
III) Educate the patient

That’s all for today
