1
Dermatitis ( Eczema )
By
Hala Al- Salman
The term dermatitis and eczema are now regarded as synonymous.
The word "eczema" comes from the Greek word 'eczein" which mean
'boiling" referring to the tiny vesicles (bubbles) that are seen in acute
stages of the disease.
The condition makes up to 20% of all new patients referred to
dermatology clinics.
Classification of eczema:
There is no universal classification which is entirely satisfactory. The
most acceptable classification is according to the etiology which include
exogenous and endogenous eczema.
Other classification depend on the appearance of the lesions e.g.
nummular or discoid eczema, or according to the location e.g. hand
eczema.
Exogenous eczema:
1. Contact dermatitis:
a. Allergic.
b. Irritant.
2. Photodermatitis.
3. Infective dermatitis.
Endogenous eczema:
1. atopic dermatitis.
2. Seborrhoeic dermatitis.
3. Discoid ( nummular ) eczema.
4. Stasis ( gravitational ) eczema.
5. Pityriasis alba.
Unclassified eczema:
1. Asteatotic eczema.
2. Juvenile plantar dermatosis.
3. Localized neurodermatitis (lichen simplex chronicus).
2
Clinically :
1. Acute eczema:
- Redness and swelling usually with ill-define border.
- Papules, vesicles and even large blisters.
- Exudation, crusting and scaling.
2. Chronic eczema.
- Less vesicular and exudative.
- More scaly and thickened.
- More likely to be
lichnified
((dry leathery thickened
hyperpigmented skin with increase skin marking secondary to
repeated scratching or rubbing)).
Complication of eczema:
1. Secondary bacterial infection.
2. Dissemination provoked by medications.
3. Anxiety state may develop with severe form of eczema and affect the
quality of life.
Histopathology:
Acute stage:
There is edema in the epidermis (spongiosis), which may progress to the
formation of intraepidermal vesicles.
Chronic stage:
Show less spongiosis and vesiculation but more thickening of prickle
cell layer (acanthosis) and horny layers (hyperkeratosis and
parkeratosis).
Atopic dermatitis
The word atopy comes from the Greek (a-topos: without place). Atopy
is a state in which an exuberant production of IgE occurs as a response
to common environmental allergens.
Atopic subjects may, or may not, develop one or more of the atopic
diseases such as asthma, hay fever, eczema and food allergies. The
prevalence of atopy is steadily rising.
A strong genetic component is responsible for atopic dermatitis, but
environmental factors may be responsible for exacerbation as well as for

3
the peculiar distribution of the disease on the body surface, e.g. food,
pollen, feather, silk, dog and cat hair……
The development of atopic dermatitis probably depend on the interplay
of numerous constitutional, immunological, psychological and climatic
factors.
80% of patients with atopic dermatitis have high level of IgE and
impaired cell- mediated immunity with subsequent increased
susceptibility to bacterial, viral and fungal infections.
70% of the patients have family history of one of the atopic disorders
(atopic dermatitis, asthma, or hay fever).
50% of patients with Atopic dermatitis have other associated atopic
disorders.
15% of the population have at least one of the atopic manifestations.
The concordance rate for atopic dermatitis in monozygotic twins is 86%
and in dizygotic twins is 21%.
The atopic diseases are the same types within each family (e.g. most of
the affected have eczema, other family members have respiratory
allergy…)
There is also a tendency for atopic disease to be inherited more often
from the mother than the father.
Clinical presentation:
75% of the cases begin before the age of 6 months, and 80-90% before
the age of 5 years.
It affects at least 3% of infants, but the onset may be delayed until
childhood or adulthood.
60-70% of children will clear by their early teens, although subsequent
relapses are possible.
The distribution and character of the lesions vary with age but a general
dryness of the skin may persist throughout life.
1.
Infantile stage:
the lesions tend to be vesicular and weeping, often
start on the face with a non-specific distribution elsewhere,
commonly sparing the napkin area.
2.
Childhood stage:
the lesions tend to be leathery, dry and
excoriated, affecting mainly the elbow and knee flexures, wrists and
ankles. A reverse pattern affecting the extensor aspect of the limbs is
also recognized.
4
3.
Adulthood stage:
the distribution is as in childhood with a marked
tendency toward lichenification and more widespread but low-grade
involvement of the trunk, face and hands.
White dermographism is often striking, but not diagnostic of Atopic
dermatitis.
The cardinal feature of Atopic eczema is itching and scratching.
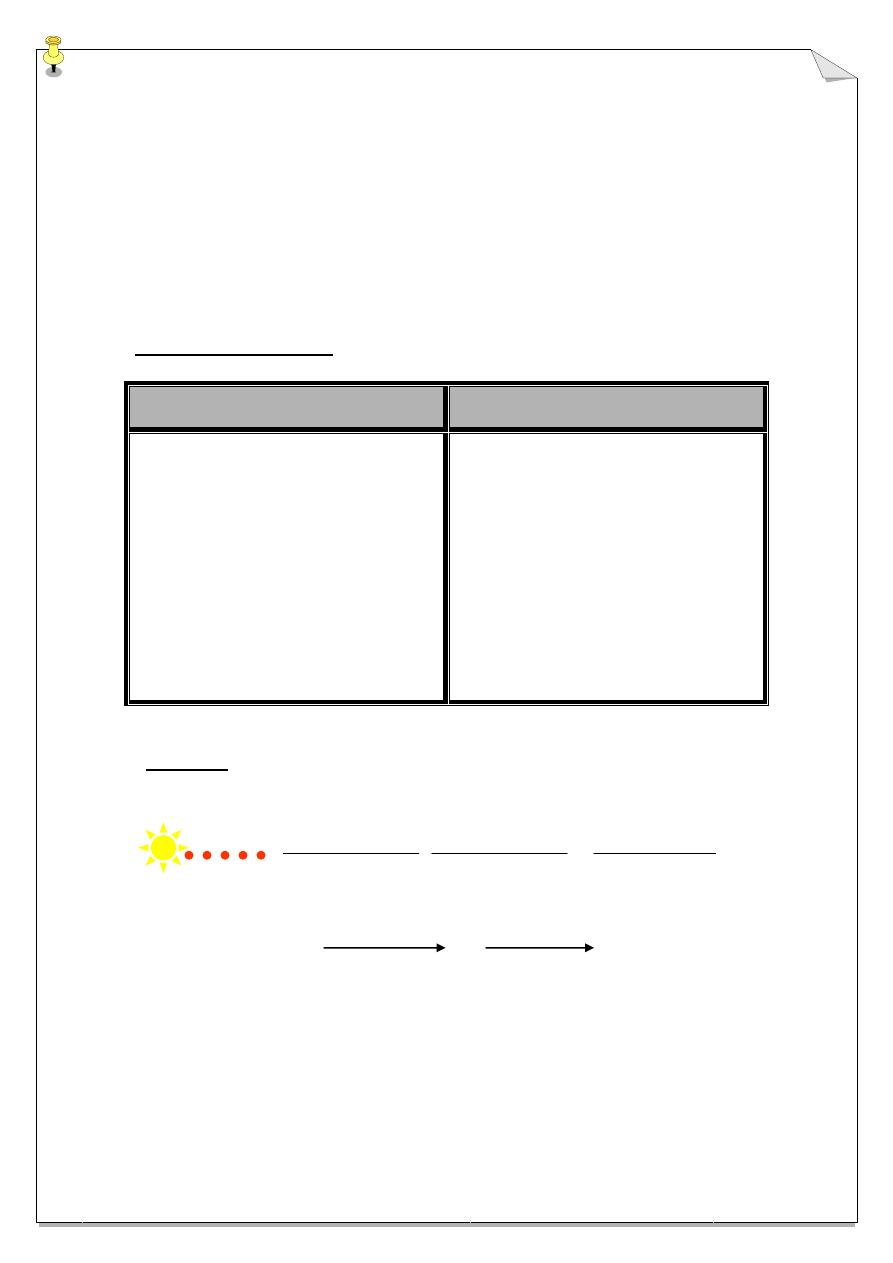
Diagnostic criteria:
Major criteria
Minor criteria
1. Pruritus.
2. Typical morphology & distribution
of lesions for age group.
3. Chronic or chronic relapsing
dermatitis.
4. Personal or family history of atopy.
Xerosis
Elevated IgE
Early age of onset
Recurrent skin infection
Hand & nipple eczema,
cheilitis
Pit. Alba
Hyperlinear palm, keratosis
pilaris, ichthyosis
White dermographism
Central pallor of face
Infraorbital folded eyelid &
darkening
Course:
Infantile
childhood adulthood
Birth 2 m. 2 y. 10 y.
1/3 1/3
5
Complications:
1. Secondary bacterial infection.
2. Viral infection, the most dangerous eczema herpiticum, also
molluscum contagiosum and warts.
3. Poor growth, due to disturbed sleep and absorption of topical steroid.
4. Exfoliative dermatitis.
Treatment:
1st. line:
1. Explanation & assurance
2. Avoid irritant (soap, perfume, detergent, house dust,
excessive bathing, extreme heating, woolen clothing next
to the skin… etc)
3. Eliminate suspected allergens (contact, food &
aeroallergens)
4. Relive stress (anxiolytic)
5. Treat infection (staph, herpes, & fungal infection)
6. Hydrate skin (emollient)
7. Interrupt itch-scratch cycle (sedative antihistamine)
8. control inflammation by use of topical steroid.
2nd. Line:
1. Wetting & occlusion
2. PUVA & UVB
3. Systemic glucocorticoid
4. Hospitalization
5. Immunotherapy: Cyclosporin & Azathiaprin.
Seborrhoeic dermatitis
A common chronic, inflammatory disease affecting mainly the hairy
areas, characterized by greasy yellowish scales.
Cause:
The yeast pityrosporium ovale probably is a causative factors, but both
genetic and environmental factors may influence the onset and course of
the disease.
Many adult patients have an oily complexion (seborrhoeic diathesis) and
the condition may be familial.
Seborrhoeic dermatitis may be an early sign of AIDS.
6
Seborrhoeic dermatitis may affect infants and clears quickly, but its most
common in adult males and its course is unpredicted and may be chronic
or recurrent.
Severe cases occurred in patients with AIDS.
Clinically:
Infant (cradle cap):
It affect male more than female. Infants commonly develop a greasy
adherent scales on the scalp. The scale may accumulate and become thick
and may accompanied by inflammation and secondary infection. Lesions
may affect the trunk and the flexures including the napkin area and in
severe cases it may be generalized.
Adolescents and adults:
More common in male, between 3
rd
– 6
th
decade. Patients may show fine,
dry, white or yellow scaling on inflamed base. The distribution may be
diffuse or affect the seborrhoeic area.
There are 3 patterns:
1. Red scaly or exudative eruption of the scalp, ears, face and eyebrows.
May be associated with chronic blepharitis and otitis externa.
2. Dry scaly 'petaloid' lesions of the presternal and interscapular area.
There may be extensive follicular papules or pustules on the trunk
(seborrhoeic folliculitis or pityrosporium folliculitis).
3. Intertriginous lesions of the armpits, umbilicus, groin, or under
spectacles or hearing aids.
Complication:
1. Furunclosis.
2. Superadded candida infection is common in the intertriginous area.
7
Treatment:
Therapy is suppressive rather than curative.
1. Topical imidazole (1
st
. line).
2. 2% sulphur.
3. 2% salicylic acid.
4. tar.
5. Selenium sulphide.
6. Weak steroid with antiseptic or antifungal preparation.
7. Oral itraconazole (severe cases).
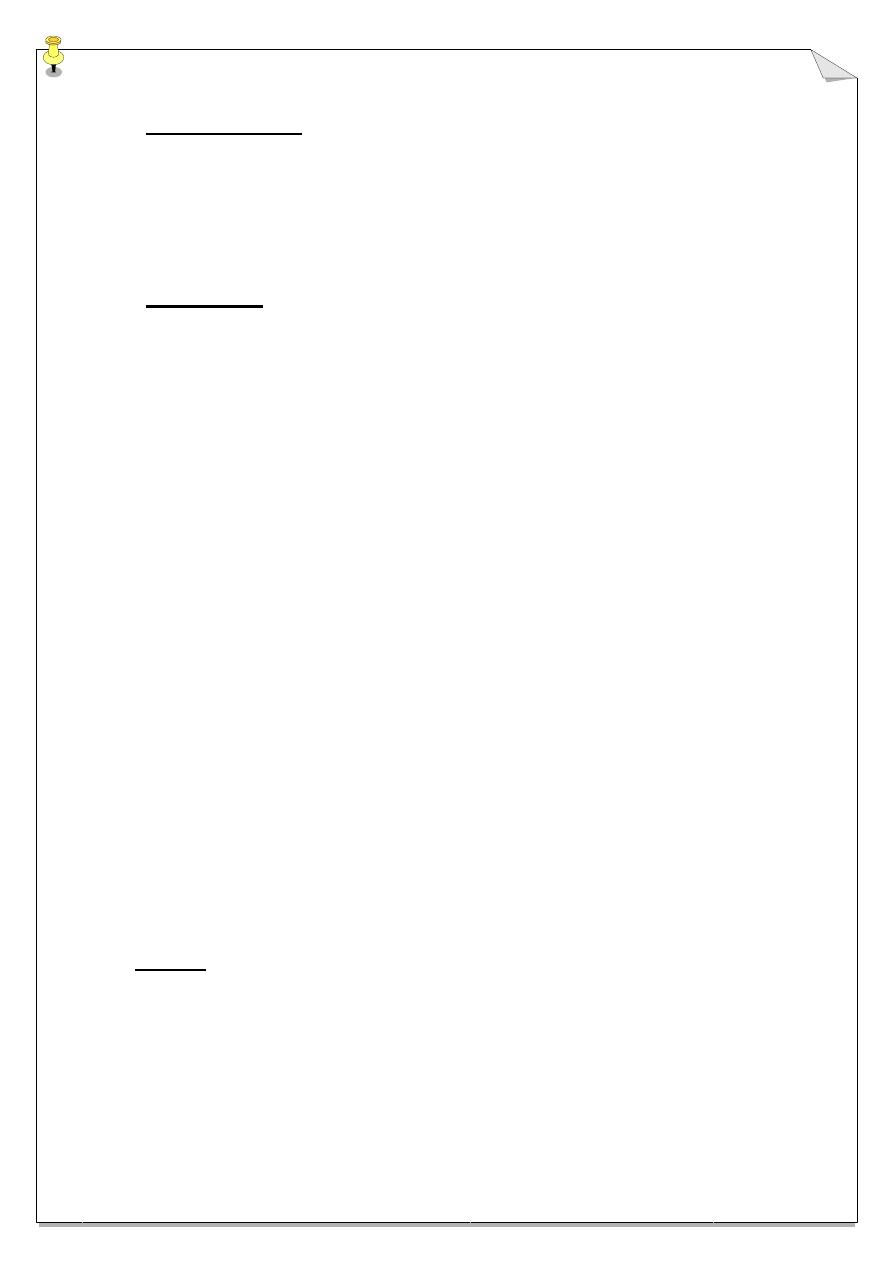
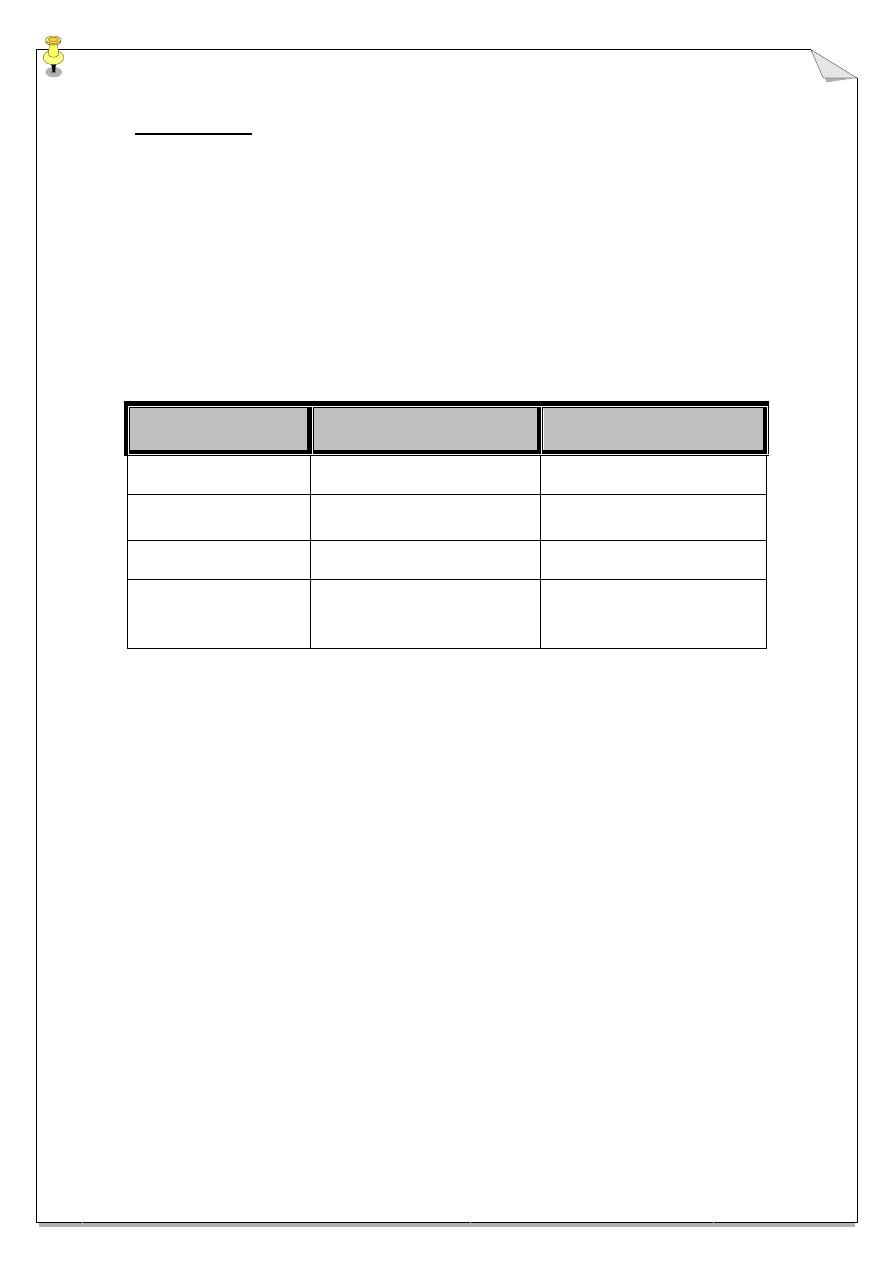
Characteristic
SD
AD
1. Age of onset
Since birth
Not before 2 months
2. Prognosis
Subside before the 1st birthday
Pass to childhood & adult life
3. State of baby
Quite, mild itching
Irritable & severe itching
4. Site of lesions
Scalp (cradle cape), face,
retroauricular, axilla & napkin area
(napkin dermatitis)
Scalp, checks, wrists & ankles,
napkin area is speared
