Secondary amenorrhea
Presented by :Dr. Aseel Basim Al_taee
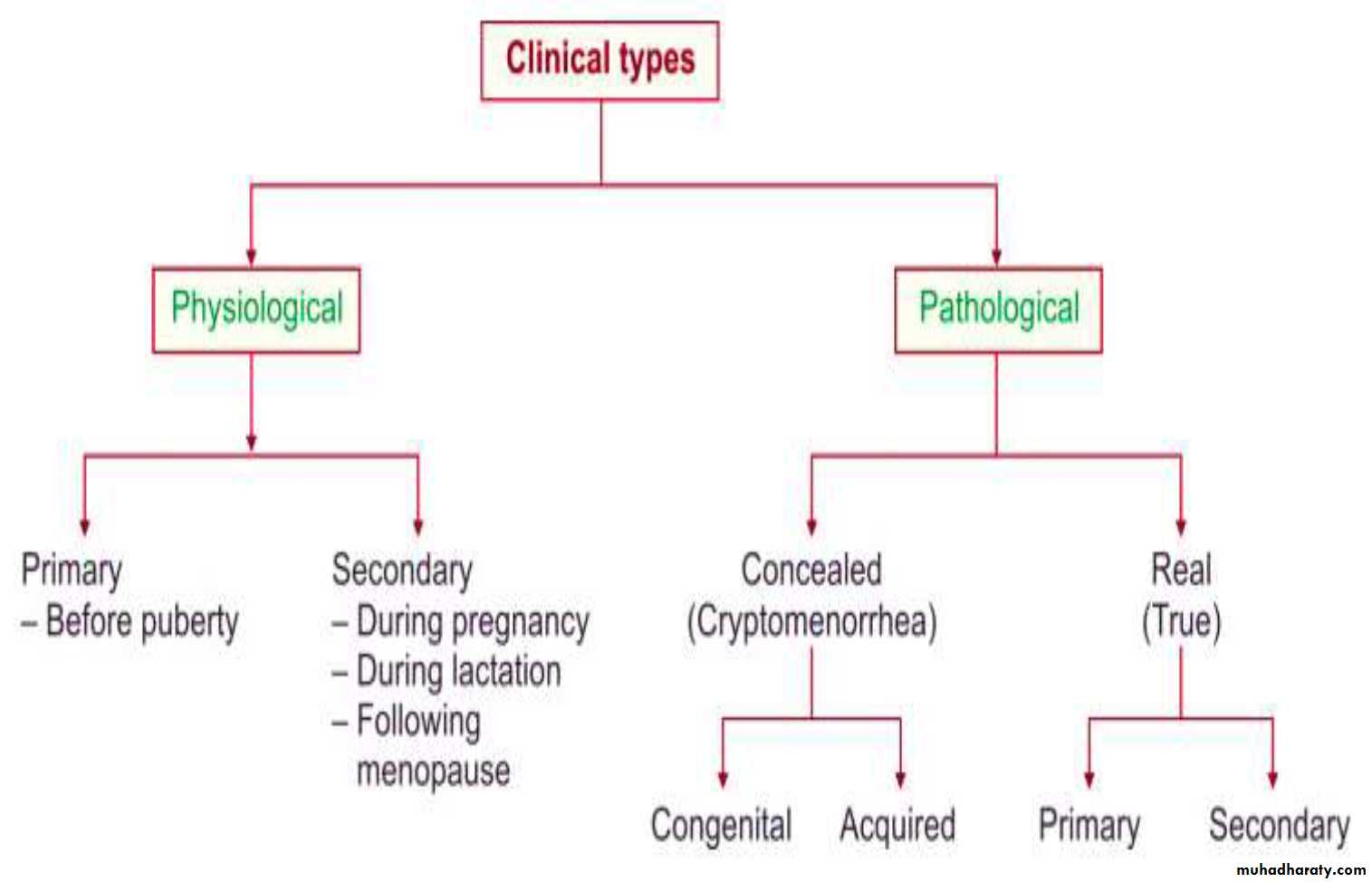
Definition
Absence of menses for6 months in a previously menstruating female with irregular cycles
Or
3 months with regular cycles and not due to pregnancy.
prevalence about (3%)
ETIOLOGY (Physiological )
The most common cause of secondary amenorrhea in reproductive age women is pregnancy and this should always be excluded by physical exam and laboratory testing for the pregnancy hormone - HCG. even if the patient thinks it to be unlikely.ETIOLOGY (pathological )
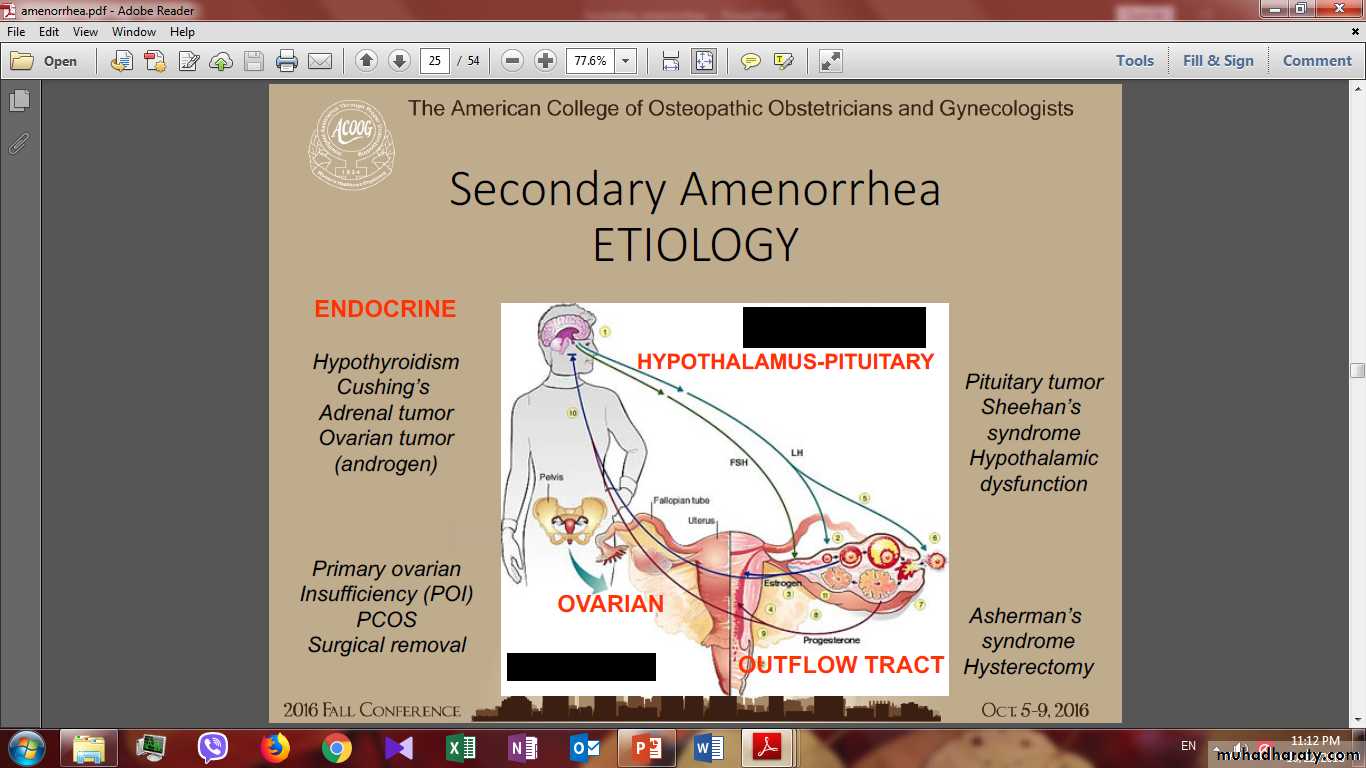
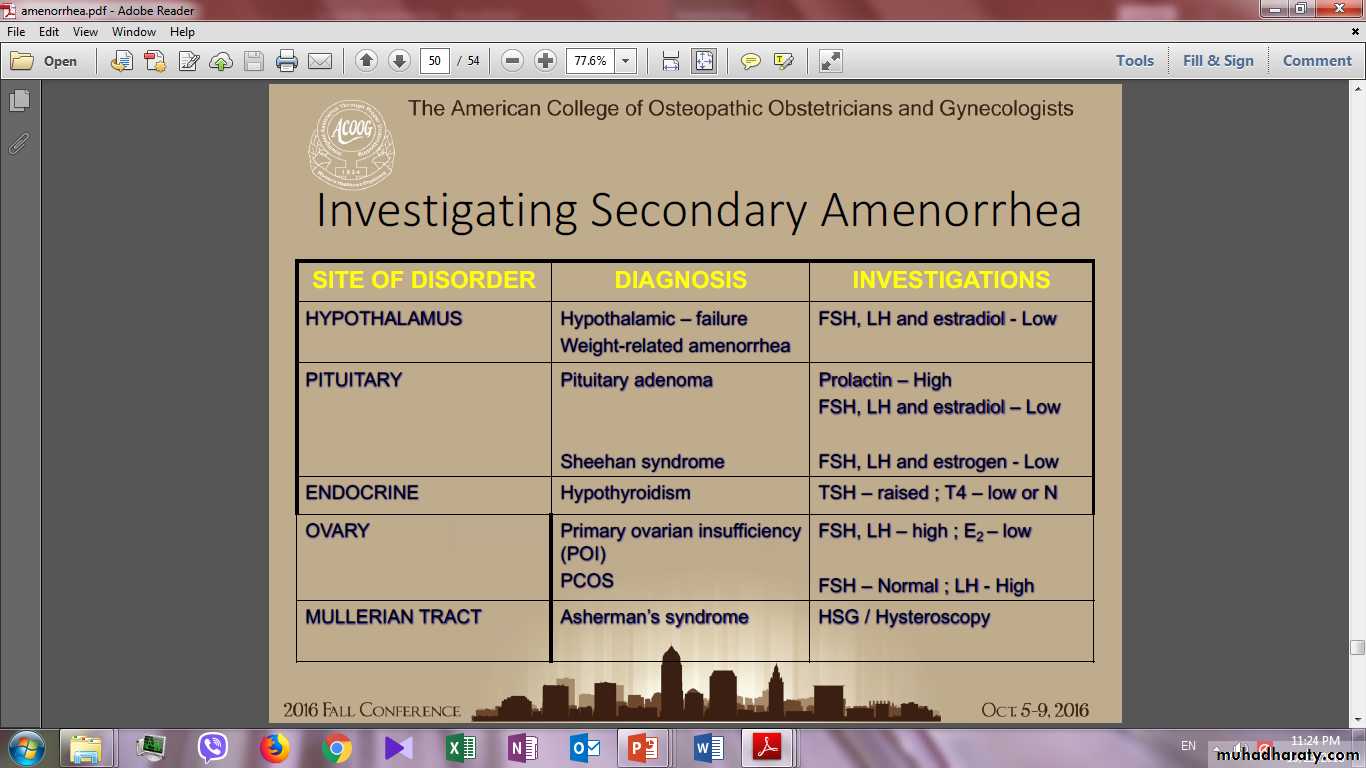
HORMONAL/ENDOCRINOLOGICHypothalamic- causes
Hypothalamic dysfunction is a common cause (30%-35%)
Functional Hypothalamic Amenorrhea ( Heavy exercise , Psychological stress ,Anorexia nervosa )
Hypothalamic- causes
Heavy exercise, Psychological stress , these will switch off the hypothalamus(Suppression of GnRH pulsatile secretion this causes low FSH and LH and, therefore, also a low estrogen level ) causing hypogonadotropic hypogonadism, and causing amenorrhea.Any process that destroys the hypothalamus can impair GnRH secretion and lead to hypogonadotropic hypogonadism and amenorrhea
The tumors most often associated with amenorrhea include craniopharyngiomas , germinomas ,gliomas, and metastatic lesions.
The most common of these tumors, craniopharyngiomas.
Alternatively, impaired GnRH secretion may follow trauma, radiation, infections such as tuberculosis, or infiltrative diseases such as sarcoidosis
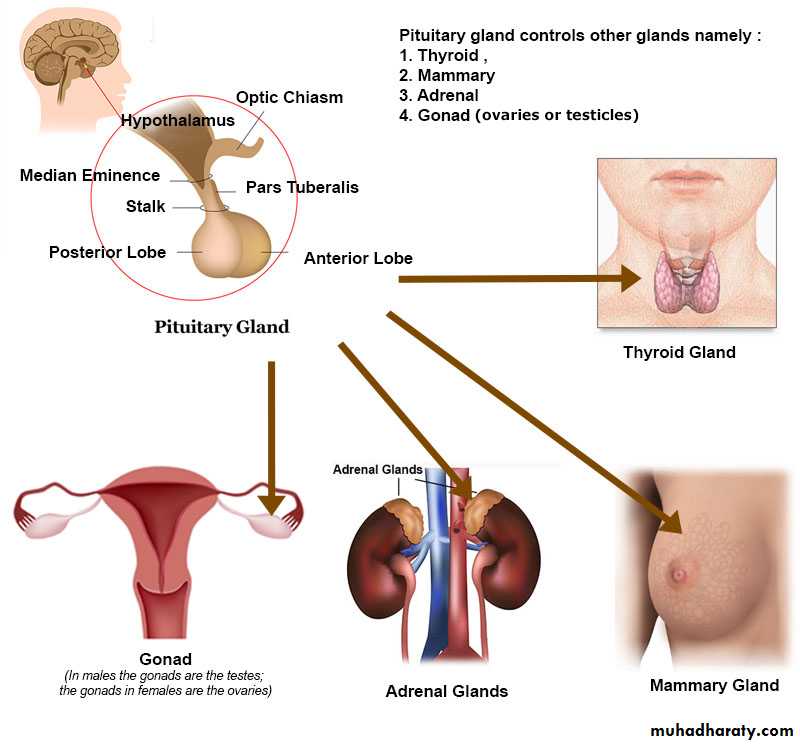
PITUITARY- causes
Most pituitary dysfunction is acquired after menarche and therefore presents with normal pubertal development followed by secondary amenorrhea.1. Pituitary adenomas are the most frequent cause of acquired pituitary dysfunction.
prolactinoma(benign adenomas of lactotrophs) is the commonest adenoma causing amenorrhea.
It produce prolactin, elevated levels inhibit pulsatile secretion of GnRH
It is common
Found in 1/3 of women with secondary amenorrhea
Only 1/3 of women with high prolactin levels have galactorrhea
Almost never malignant
PITUITARY- causes
2. As in the hypothalamus, pituitary function may also be diminished by inflammation, infiltrative disease, metastatic lesions, surgery, or radiation treatmentPITUITARY- causes
3. Sheehan’s syndromeSheehan syndrome refers to panhypopituitarism. It classically follows massive postpartum hemorrhage and associated hypotension.
The abrupt, severe hypotension leads to pituitary ischemia and necrosis.
Patients with Sheehan's syndrome have varying degrees of anterior pituitary hormone deficiency.
Sheehan's syndrome usually presents progressively with a variety of developing symptoms
Sheehan’s syndrome
Patients with the most sever form develop shock due to pituitary apoplexy.Pituitary apoplexy is characterized by a sudden onset of headache, nausea, visual deficits, and hormonal dysfunction due to acute hemorrhage or infarction within the pituitary.
In less severe forms, loss of gonadotrope activity in the pituitary leads to anovulation and subsequent amenorrhea.
Damage to the other specific pituitary cell types lead to a failure to lactate, loss of sexual and axillary hair, and hypothyroidism or adrenal insufficiency symptoms.
OVARIAN - causes
Primary ovarian Insufficiency (POI)PCOS
Resistant ovary syndrome.
Radiation and chemotherapy.
Functioning ovarian tumor (virilizing tumors).
Surgical removal
OVARIAN - causes
1-Premature ovarian failure (POF) /PRIMARY OVARIAN INSUFFICIENCY (POI)ovarian failure before the age of 40 years. Its incidence 1/100 at age 40, 1/250 < 35 y/o
90% idiopathic
exhaustion of primordial follicles and normal follicular development despite the pituitary high production of gonadotrophins (LH and FSH),
Causes can be:
Genetic (gonadal dysgenesis in Turner Syndrome XO-female)
Fragile X syndrome (X linked, common form of mental retardation, 2% sporadic cases, 14% familial)
Autoimmune disease especially thyroid, adrenal, occur in 20% of women with POI
Infections such as mumps oopheritis
Chemo/radio therapy /smoking
Ovarian failure may result from ovarian torsion, surgery
OVARIAN - causes
2- Polycystic Ovarian Syndrome (PCOS),chronic anovulation or oligo-ovulation with clinical or laboratory evidence of hyperandrogenism and without evidence of any other underlying condition
The etiology is probably related to insulin resistance, with a failure of normal follicular development and ovulation
Criteria for PCOS
Patients with PCOS will present with:Oligo/amenorrhoea in 65-75% of patients
Hirsutism in 30-70% of patients
Subfertility, up to 75% of patients will have difficulty in conceiving.
Obesity in 40% of patients.
Acanthosis nigricans: areas of increased skin pigmentation with velvety texture occurring in the axillae, between the legs and other flexures, 2% of patients
Endocrine causes
Hyperprolactinemia ( tumor , drugs, TSH _induced hyperprolactinemia)
Thyroid disease( High level of thyroxine inhibit FSH release.)
Cushing syndrome
AcromegalyOvarian tumors (steroid producing)
Anatomical causes
Usually due to previous surgery.Commonest example:
1) Hysterectomy
2) Endometrial ablation
3)Severe postpartum infection.
4) Asherman’s syndrome (damage to the endometrium with adhesion formation)
5) Stenosis of the cervix following cone biopsy/LEEP
6) Vaginal agglutination (radiation therapy)
Endometrial atrophy secondary to prolonged progesterone administration
Anatomical causes
ASHERMAN’S SYNDROM
Asherman's Syndrome, or intrauterine adhesions/scarring or synechiae, is an acquired uterine condition, characterized by the formation of adhesions (scar tissue) inside the uterus and/or the cervix. In many cases the front and back walls of the uterus stick to one another
Symptoms
• No menstrual flow (amenorrhea) or decreased menstrual flow
• Infertility
• Recurrent miscarriages
Causes
• Pregnancy-related D&Cs have been shown to account for 90%• pelvic surgeries such as Cesarean section, surgery to remove fibroids or polyps
• genital tuberculosis
Other Causes
Drugs: (phenothiazine, metoclopromide, cocaine and opioids.)chronic diseases including end-stage kidney disease, liver disease.
Malignancies.
acquired immunodeficiency syndrome.
malabsorption syndromes.
EVALUATION
History:The questions to ask include:
LMP and Previous menstrual history: (Age of menarche, concentrate on asking its nature spontaneous not primary amenorrhoea with withdrawal bleeding due to exogenous hormone administration).
What was the nature of the periods when present – regularity, length, heaviness of flow?
Is there a possibility of pregnancy?
Is there a history of previous pregnancy complications, such as postpartum haemorrhage, evacuation of retained products of conception Or termination of pregnancy?
What contraception is used – could it be causing amenorrhoea?
In some cases, the hormonal contraception itself may be the cause of the amenorrhea as:Mirena (progestrone IUD), medroxy progesterone acetate, after stopping of combined oral contraceptive pills.
Is exercise excessive (More than 8 hours of vigorous exercise a week may cause amenorrhea.)? Has there been recent weight loss?
Any breast discharge?( milk produced in non lactating breast)
Is there a history of chronic illness, radiotherapy or chemotherapy?
Does the woman experience headaches or visual symptoms?Are there associated endocrine symptoms such as obesity, hirsutism, acne or symptoms of hypothyroidism?
Are there associated menopausal symptoms such as hot flushes, night sweats or vaginal dryness? Or Family Hx of POF ?
What medications are being taken?
Prior surgeries ?
Examination:
All women should have body mass index calculated .The normal range is 20–25 kg/m2, and a value above or below this range may suggest a diagnosis of weight related amenorrhoea.Blood pressure measurement.
Signs of hyperandrogenism (acne, hirsutism, balding (alopecia)).
Signs of virilization (deepening of the voice, breast atrophy, increase in muscle bulk and cliteromegaly).
Examination should be directed by the history, looking for signs of PCOS (obesity, hirsutism and acne) or endocrine disease such as hypothyroidism(Enlarged thyroid) ,Cushing disease (Hypertension ,Central Obesity, Easy bruisability , Straie )
If a prolactinoma is suspected then the visual fields should be checked.
Examine for Galactorrhea.Abdominal examination:
A physical examination may uncover unexpected findings that are indirectly related to the loss of menstrual regularity (eg, hepatosplenomegaly).Uterine enlargement in pregnancy.
Pelvic examination:
If the patient married, pelvic examination should be done.Look for signs of pregnancy.
Look for evidence of atrophic effects of hypo-oestrogenism within the lower genital tract (Thin and pale vaginal mucosa with absent rugae).
A bimanual examination may be indicated, for example to check for uterine size in suspected haematometra.
Ovarian enlargement may be found upon pelvic examination in some cases.
Investigations:
In most cases, doctors need investigations which should be directed by history and examination.A pregnancy test is usually indicated in secondary amenorrhea.
A hormone profile should then generally indicate the diagnosis.
Gonadotrophin level (FSH, LH)
Reduced Gonadotrophin level seen in pituitary or hypothalamic disorder.
Elevated Gonadotrophin level seen in premature ovarian failure and primary ovarian insufficiency. An FSH level in the menopausal range (>40IU) is indicative of ovarian insufficiency.
If premature ovarian failure is confirmed by gonadotrophin levels, then karyotype and autoimmune tests should be arranged for genetic causes and associated autoimmune disease, respectively.
Hypothyroidism is associated with low thyroxine and raised thyroid stimulating hormone.
Serum prolactin should always be checked, but caution is needed in interpreting the result as a prolactin level up to 1000 mU/ml may be due to stress, breast examination, PCOS or the venipuncture itself.
Androgen profile, A very high testosterone level indicates further investigation for a possible androgen-secreting tumor, for example from the ovary or adrenal gland
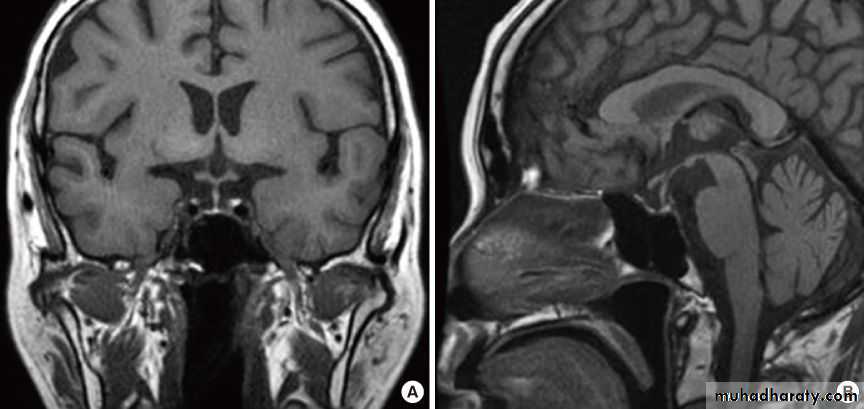
Computed tomography or magnetic resonance imaging of the pituitary fossa and formal visual field testing should be arranged in cases of suspected prolactinoma.
Pelvic ultrasound is helpful for complicated cases of pelvic organ
If Asherman’s syndrome is suspected from previous uterine evacuation, then a hysteroscopy/ Hysterosalpingography is indicated.
Laparoscopy:
To inspect pelvic organs and to take biopsy of ovaries. if the biopsy revealed presence of primordial follicle mean resistant ovary syndrome while if there is no primordial follicle in ovarian biopsy mean premature ovarian failure.Progesterone challenge test (Progesterone withdrawal test):
Previously was used. If there is adequate level of estrogen, withdrawal bleeding will occurred when patient taking progesterone but if there is no adequate level of estrogen no bleeding will occurred when patient taking progesterone.
Management
Management of secondary amenorrhea depends on the cause of the problem.
No evidence of underlying disease:
- Reassurance and spontaneous recovery is to be expected
Pituitary insufficiency (Sheehan syndrome) can be managed by replacing target organ hormones as well as HRT as for menopausal symptoms.
Polycystic ovaries
Treatment with a COCP will restore periods and should be used if the woman has had fewer than four periods per yearIf obesity is a problem in these women, then weight loss usually restores periods and fertility.
If the woman is trying to conceive, then ovulation may be induced with clomiphene.
Premature ovarian failure (spontaneous or iatrogenic)
As with primary ovarian failure, counselling is an essential part of the management of women in whom the amenorrhea is permanent, in view of the anxiety caused about fertility, sexuality and long-term health issues such as osteoporosis.Hormone replacement therapy (HRT) for osteoporosis prevention is necessary and counselling support should be offered.
Fertility is only a possibility by ovum donation and in vitro fertilization
Anorexia- or exercise-related amenorrhea
Clear advice about lifestyle and diet is essential to restore periods.Most women recommence menstruating once exercise is reduced or the body mass index is above 19.
If a woman continues to be amenorrhoeic, then some form of hormone replacement with COCP or HRT is needed to prevent osteoporosis.
Prolactinoma
Prolactinoma is generally managed by endocrinologists with bromocriptine or cabergoline.
Surgery is only indicated for macroadenomas or cases resistant to medication.
Hypothyroidism
Hypothyroidism should be treated with thyroxine replacement.
Asherman’s syndrome
Adhesions can be broken down hysteroscopically and a combination of an IUCD with a 3-month course of systemic oestrogen is necessary to prevent reformation. However, although periods may return, pregnancy is unlikelyContraceptive-related amenorrhoea
Amenorrhoea related to depot medroxyprogesterone acetate may continue for 12–18 months after the last injection.However, ovulation is likely to occur before a period and effective contraception should still be advised.
Women who are amenorrhoeic with the progesterone-only pill, LNG-IUS or implant should be reassured that this is normal and that the contraceptive method does not need to be changed.
The presentation of Asherman's Syndrome typically involves:
A. Hypomenorrhea and amenorrhea.B. Galactorrhea.
C. Menorrhagia.
D. Metrorrhagia.
Key a.
The most common cause associated with amenorrhea in a reproductive age women is:
A. Follicular cyst.
B. Corpus luteal cyst.
C. Benign cystic teratoma.
D. Leiomyoma.
E. Pregnancy.
Key E