ABNORMAL UTERINE BLEEDING
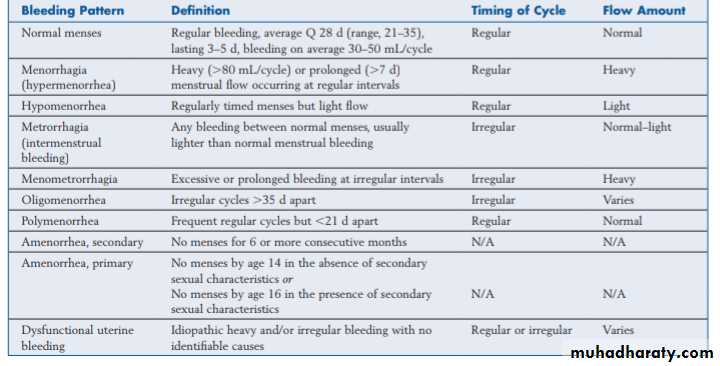
Abnormal uterine bleeding refers to any departure from the norm in the menstrual cycle.The mean interval between menses is 28 days (±7 days). Thus if bleeding occurs at intervals of 21 days or less or 35 days or more it is abnormal.
The mean duration of menstrual flow is 4 days. Few women with normal menses bleed more than 7 days, so bleeding for longer than 7 days is considered to be abnormally prolonged.
It is useful to document the duration and frequency of menstrual flow with the use of menstrual diary cards.
The mean total blood loss is less than 80 ml,however, it is difficult to determine the amount of menstrual blood loss (MBL) by subjective means.
It can involve too much bleeding (heavy periods, frequent menses, or bleeding between periods) too little bleeding (light periods, infrequent periods, or complete absence of periods) or inappropriate unscheduled bleeding (postcoital spotting, postmenopausal bleeding).
HMB: heavy cyclical menstrual bleeding over several consecutive cycles (Objectively is a total menstrual blood loss >80ml )
IMB: bleeding between periods, often seen with endometrial and cervical polyps
PCB: bleeding after sex. Often associated with cervical abnormalitiesPMB: bleeding more than 1 year after cessation of periods. Exclude endometrial pathology or vaginal atrophy
BEO: ‘bleeding of endometrial origin’, a diagnosis of exclusion, has replaced the term ‘dysfunctional uterine bleeding’ (DUB): describes idiopathic heavy and/or irregular bleeding that cannot be attributed to another cause following a complete evaluation, most commonly due to anovulation or oligoovulation.
Older classification includes:
Aetiology:
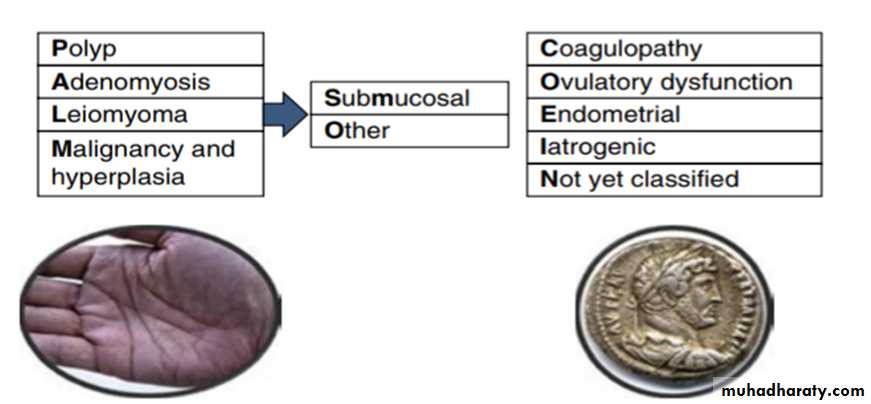
The new classification system PALM-COEIN was introduced by the International Federation of Gynecology and Obstetrics (FIGO) and is supported by the American College of OB/GYN (ACOG) classifies AUB by both the pattern and the etiology of the bleeding.The acronym AUB is followed by the letters PALM-COEIN and a subscript 0 or 1 associated with each letter to indicate the absence or presence, respectively, of the abnormality. For example, a patient with abnormal bleeding due to a polyp would be described as AUB-P1A0L0M0-C0O0E0I0N0.
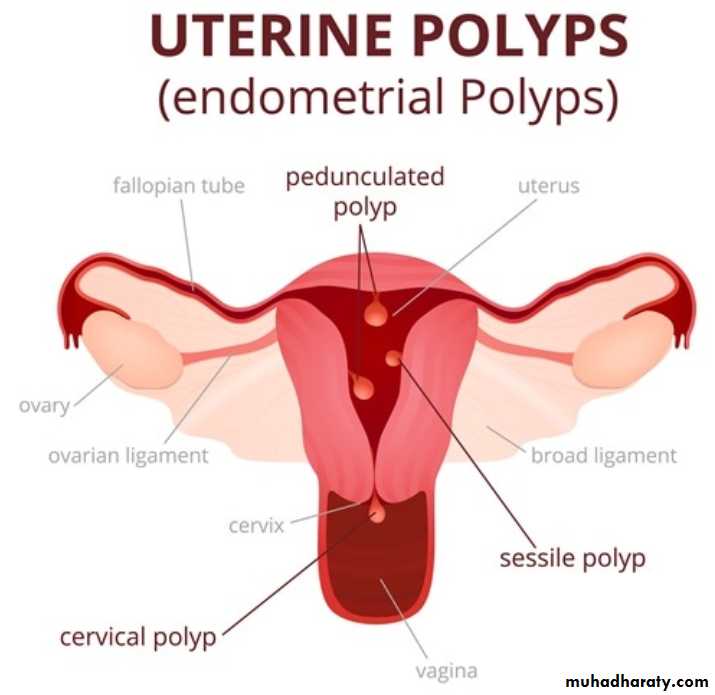
Endometrial Polyps
Are localized overgrowths of endometrial tissue, containing glands, stroma, and blood vessels, covered with epithelium. Endometrial polyps are most commonly found in reproductive-age women, and estrogen stimulation is thought to play a key role in their development. As such, polyps are rarely found before menarche. The majority of endometrial polyps are benign. Transvaginal ultrasound detected asymptomatic polyps in up to 12% of women undergoing routine gynecologic examination; small endometrial polyps smaller than 1 cm appear to regress spontaneously. Women with symptomatic polyps can be treated safely and effectively with operative hysteroscopy.Adenomyosis
Adenomyosis is defined by the presence of endometrial glands and stroma in the uterine myometrium. The presence of ectopic endometrial tissue leads to hypertrophy of the surrounding myometrium.Peak incidence is in the fifth decade of life. Multiparity is considered the most significant risk factor. Adenomyosis is a histologic diagnosis, but findings of an enlarged, asymmetric uterus on ultrasound and magnetic resonance imaging (MRI) are indicative. Abnormal bleeding due to adenomyosis is thought to be a result of altered uterine contractility and is commonly associated with profound dysmenorrhea.Leiomyoma
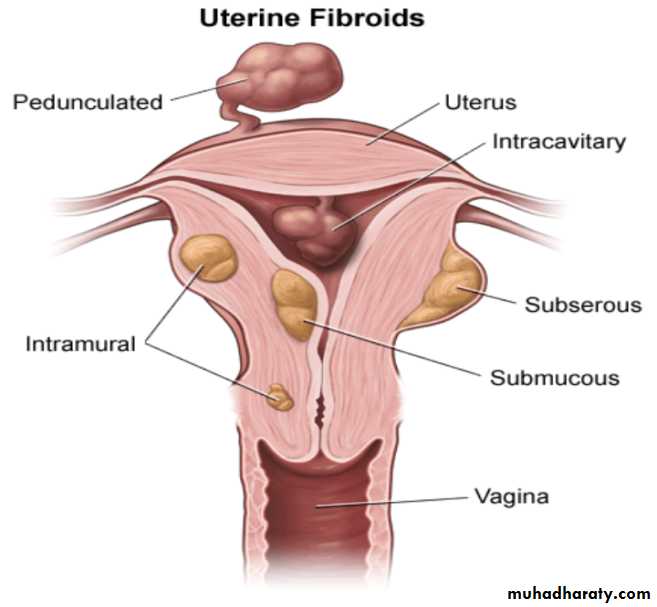
Leiomyoma, or fibroids, are benign tumors of the uterine myometrium with a complex and heterogeneous clinical presentation as varied as their biologic origins. Mechanisms by which fibroids cause abnormal bleeding are varied and depend on size, location, and number. Submucosal fibroids, as well as intramural fibroids, which are large, may increase the overall surface area of the endometrial cavity or alter uterine contractility. These effects in turn lead to abnormal and excessive uterine bleeding.Malignancy
Malignancies associated with the female reproductive tract include vulvar, vaginal, cervical, endometrial, uterine, and adnexal (ovarian or fallopian tube) cancers. Bleeding from cervical malignancy classically presents as coital bleeding or intermenstrual bleeding; thus a thorough cervical evaluation is an important part of the workup of any woman with these symptoms. AUB is the most common presenting symptom of endometrial hyperplasia and cancer. Although endometrial cancer presents most often in the seventh decade, 15% of cases are diagnosed in premenopausal women. estrogen-producing ovarian tumors may become manifest by abnormal uterine bleeding. Granulosa theca cell tumors are the most common tumors to have this presentation.Coagulopathy
Systemic diseases, particularly disorders of blood coagulation such as von Willebrand disease and prothrombin deficiency, may initially present as AUB. Routine screening for coagulation defects is mainly indicated for the adolescent who has prolonged heavy menses beginning at menarche. In adults, screening for these disorders is of little value unless otherwise indicated by clinical signs such as bleeding gums, epistaxis, or ecchymosis.Ovulatory Dysfunction
The predominant cause of ovulatory dysfunction in postmenarchal and premenopausal women is secondary to alterations in neuroendocrine function. In women with AUB-O, there is continuous estradiol production without corpus luteum formation and progesterone production. The steady state of estrogen stimulation leads to a continuously proliferating endometrium, which may outgrow its blood supply or lose nutrients with varying degrees of necrosis. In contrast to normal menstruation, uniform slough to the basalis layer does not occur, which produces excessive uterine bleeding. Anovulatory bleeding occurs most commonly during the extremes of reproductive life—in the first few years after menarche and during perimenopause. The pattern of anovulatory bleeding may be oligomenorrhea, intermenstrual bleeding, or heavy menstrual bleeding. Apart from the extremes of reproductive life, women in their reproductive years often have a cause for anovulatory bleeding. This is most frequently because of polycystic ovary syndrome (PCOS), which may be suggested by other symptoms and signs, such as acne, hirsutism, and increased body weight.anovulation can result from hypothalamic dysfunction, which could have no known cause or be related to weight loss, severe exercise, stress, or drug use. In addition, abnormalities of other nonreproductive hormones can lead to anovulation. The most common hormones involved are thyroid hormone, prolactin, and cortisol. Accordingly, TSH and PRL assays should be part of the normal workup of anovulatory women.
Iatrogenic
Iatrogenic bleeding (AUB-I) is abnormal bleeding resulting from medications. hormonal preparations, All hormonal long-acting reversible contraceptives, chronic progestogen therapy, antipsychotic drugs, combined and progesterone-only oral contraceptives may result in breakthrough bleeding.Endometrial
Women who present with heavy menstrual bleeding in the absence of other abnormalities are thought to have underlying disorders of the endometrium (AUB-E) or are otherwise unclassified. The primary line of defense to excessive bleeding during normal menses is the formation of the platelet plug. This is followed by uterine contractility, largely mediated by prostaglandin F2α (PGF2α). Chronic inflammatory changes of the endometrium (endometritis) resulting from a variety of factors including infection as subclinical infection with Chlamydia trachomatis has also been associated with AUB.Not Otherwise Specified
Abnormal bleeding not classified in the previous categories is considered AUB-N. Examples of such conditions may include foreign bodies or trauma. Treatment is tailored to the specific cause.
History And Examination
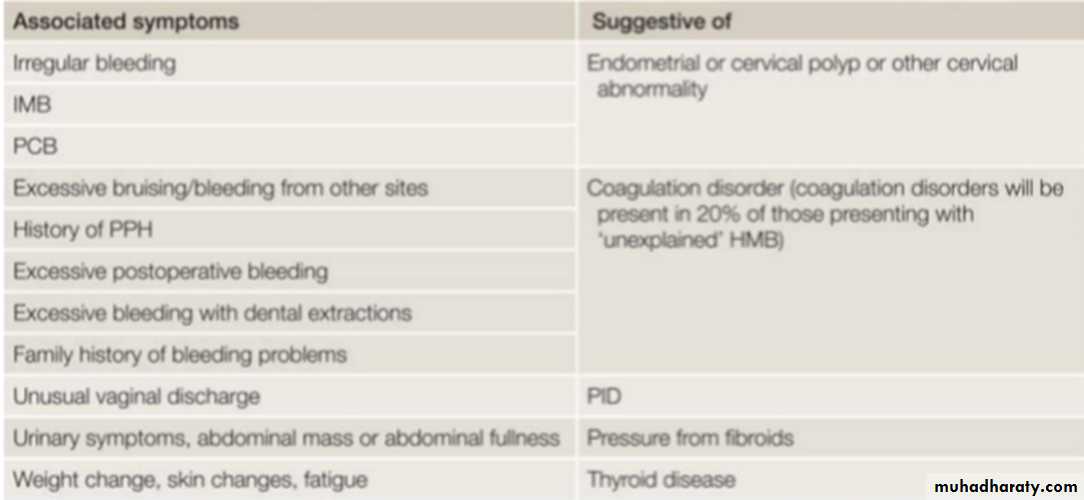
The regularity of the menstrual cycle, length of time of problem, Amount of blood loss, relationships of bleeding to sex and to menstrual cycle, or to the last menstrual bleed in the case of postmenopausal bleeding (PMB) are important questions.In younger women it is important to question whether HMB started at menarche, as this is much less likely to be associated with pathology.
After examining the patient for signs of anaemia, it is important to perform an abdominal and pelvic examination. This enables any pelvic masses to be palpated, the cervix to be visualized for polyps/carcinoma, swabs to be taken if pelvic infection is suspected or a cervical smear to be taken if one is due. Care should be taken to look for sequelae of PCOS (hirsutism, acne, truncal obesity, acanthosisnigricans), thyroid disease (thyromegaly, skin changes, increased pulse), and signs of bleeding disorder (bruising, petechiae).
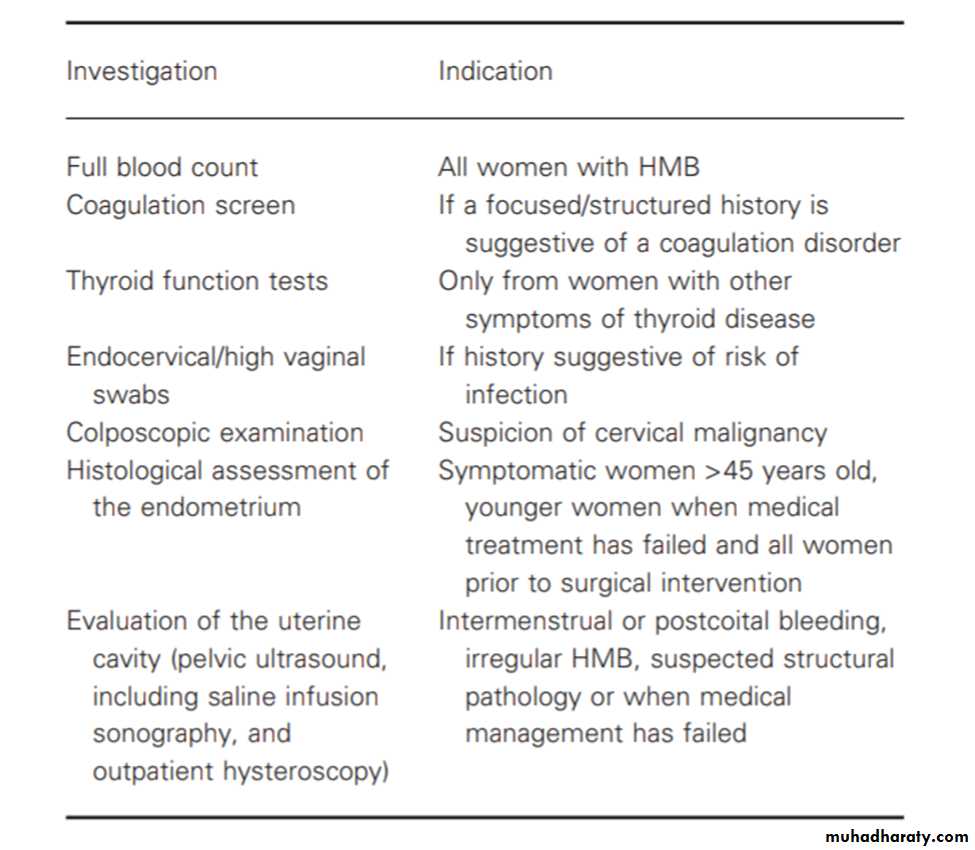
Investigations :
References:
Gynecology by ten teachers
Comprehensive gynecology
Dewhurst’s textbook in obstetrics and gynecology
Blueprints obstetrics and gynecology