PEDIATRIC UNDERNUTRITION
Dr.Noor Sameer Yahya3/10/2019
UNDERNUTRITION
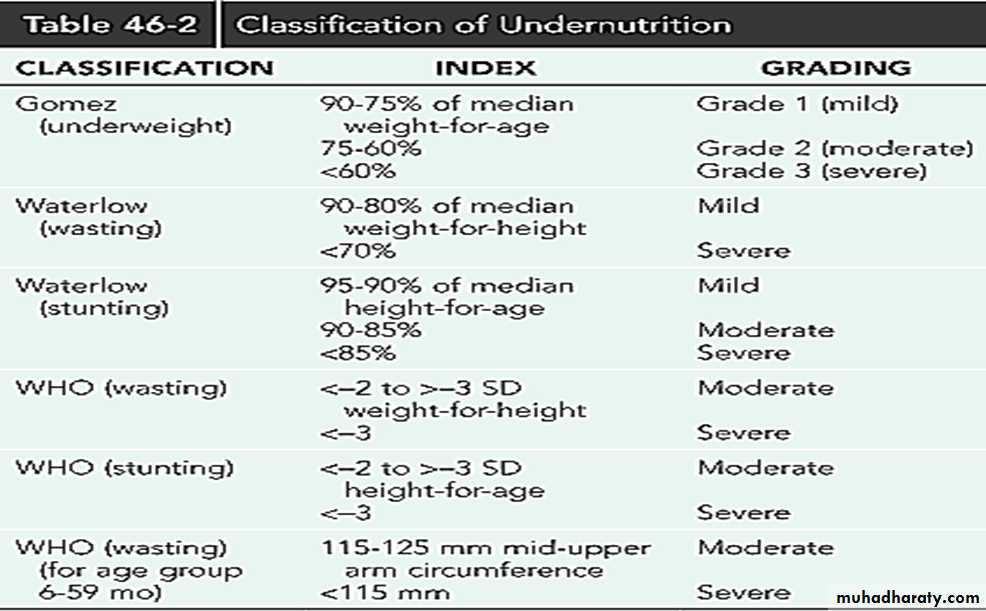
The greatest risk of undernutrition (underweight, stunting, wasting, and micronutrient deficiencies) occurs in the first 2 year of life, and this early damage to growth and development can have adverse consequences in later life on health, intellectual ability, school achievement, work productivity.Measurement of Undernutrition
Height-for-age (or length-for-age for children <2 yr) is a measure of linear growth, and a deficit result in stunting, or chronic malnutrition. it reflects socioeconomic disadvantage.A low weight-for-height, or wasting, usually indicates acute malnutrition. Conversely, a high weight-for-height indicates overweight.
Weight-for-age is the most commonly used index of nutritional status, although a low value has limited clinical significance as it does not differentiate between wasting and stunting.
• Weight-for-age has the advantage of being somewhat easier to measure than indices that require height measurements,
mid-upper arm circumference is used for screening wasted children
Micronutrient deficiencies
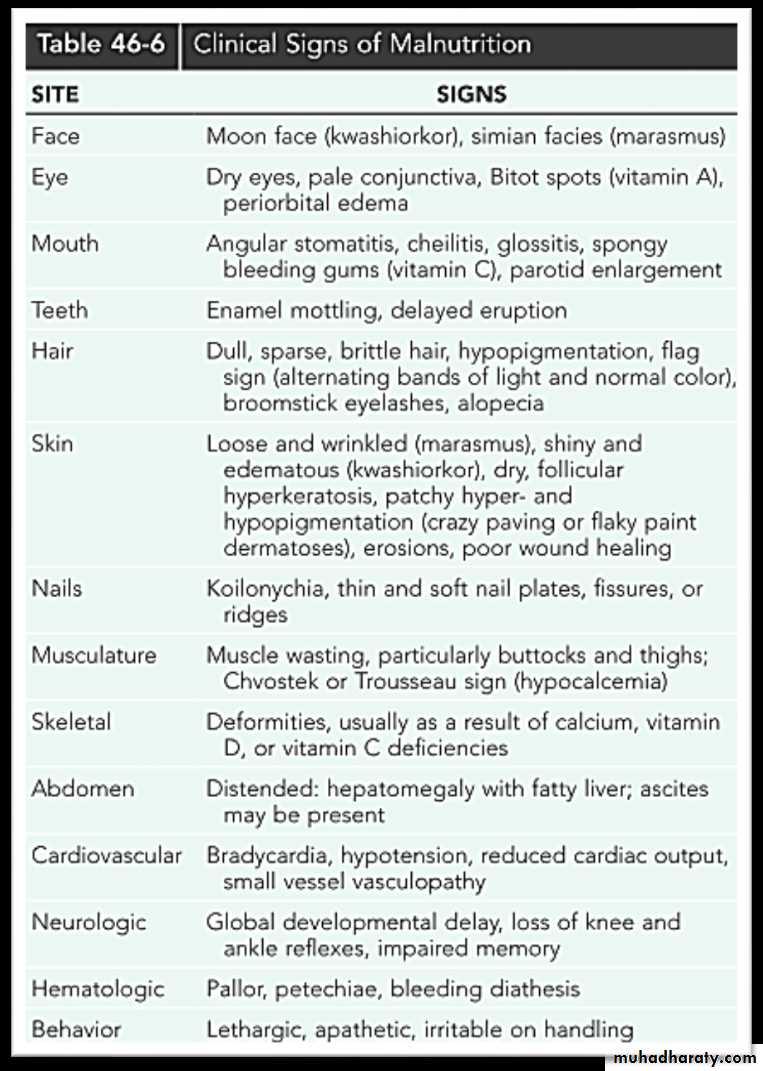
Vitamin A deficiency is caused by a low intake of retinol (in animal Foods ) or its carotenoid precursors, mainly beta-carotene in colored fruits and vegetables and dark green leaves). The prevalence of clinical deficiency is assessed from symptoms and signs of xerophthalmia (principally night blindness and Bitot spots.
Iodine deficiency is the main cause of preventable mental impair-ment. An enlarged thyroid (goiter) is a sign of deficiency. Severe deficiency in pregnancy causes fetal loss and permanent damage to the brain and central nervous system in surviving offspring (cretinism).
Iron-deficiency anemia is common in childhood either from low iron intakes or poor absorption, or as a result of illness or parasite infestation. Women also have
• relatively high rates of anemia as a result of menstrual blood loss, pregnancy, low iron intakes, poor absorption, and illness.
Hemoglobin cutoffs to define anemia are
110 g/L for children 6-59 mo,
115 g/L for children 5-11 yr,
120 g/L for children 12-14 yr.
for non pregnant women are 120 g/L,
110 g/L for pregnant women,
130 g/L for men.
4 .Zinc deficiency increases the risk of morbidity and mortality from diarrhea, pneumonia, and possibly other infectious diseases. also has an adverse effect on linear growth.
SEVERE ACUTE MALNUTRITION
is defined as severe wasting and/or bilateral edema.Severe wasting is extreme thinness diagnosed by a weight-for-length or height below −3 SD of the WHO Child Growth Standards.
• In children ages 6-59 mo, a mid-upper arm circumference <115 mm also denotes extreme thinness
Bilateral edema is diagnosed by grasping both feet, placing a thumb on top of each, and pressing gently but firmly for 10 seconds. A pit remaining under each thumb indicates bilateral edema.
This definition of severe acute malnutrition distinguishes wasted/edematous children from those who are stunted, as the latter (although underweight) are not a priority for acute clinical care as their deficits in height and weight cannot be corrected in the short term.
Other terms are marasmus (severe wasting) ,kwashiorkor (characterized by edema), and marasmic-kwashiorkor (severe wasting + edema).
A. Primary : social or economic factors that result in a lack of food.
B. Secondary
increased caloric requirements (infection, trauma, cancer(
increased caloric loss (malabsorption)
reduced caloric intake (anorexia, cancer, oral intake restriction, social factors
Clinical manifestation
• symtom• Severe wasting is most visible on the thighs, buttocks, and upper arms, and over the ribs and scapulae where loss of fat and skeletal muscle is greatest.
The skin loses turgor and becomes loose as subcutaneous tissues are broken down to provide energy.
The face may retain a relatively normal appearance, but eventually becomes wasted and wizened.
The eyes may be sunken from loss of retroorbital fat
lachrymal and salivary glands may atrophy leading to lack of tears and a dry mouth.
Weakened abdominal muscles and gas from bacterial overgrowth of the upper gut may lead to a distended abdomen.
Severely wasted children are often irritable.
In edematous malnutrition,
the edema is most likely to appear first in the feet and then in the lower legs. It can quickly develop into generalized edema affecting also the hands, arms, and face .
Skin changes commonly occur over the swollen limbs and include dark,
crackled peeling patches (flaky paint dermatosis) with pale skin
Treatment
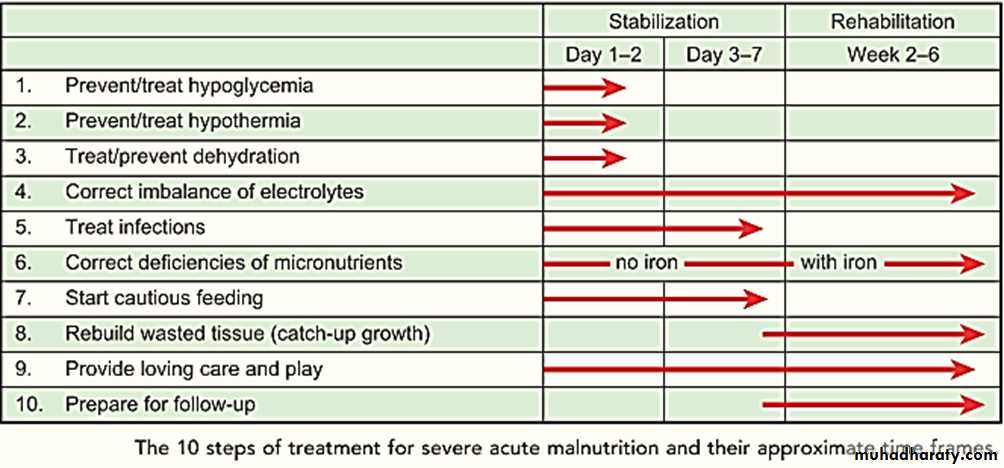
Stabilization:
feeding frequent small amounts of F75 (a specially formulated low-lactose milk with 75 kcal and 0.9 g protein per100 mL to which potassium, magnesium, and micronutrients are added), will reestablish metabolic control, treat edema, and restore appetite.
The parenteral route should be avoided; children who lack appetite should be fed by nasogastric tube, as nutrients delivered within the gut lumen help in its repair.
Dehydration status is easily misdiagnosed in severely wasted children, as the usual signs such as slow skin pinch, sunken eyes may be present even without dehydration. Rehydration must therefore be closely monitored for signs of fluid overload
1 . Prevent/treat hypoglycemia blood glucose <3 mmol/L
If conscious:1.10% glucose (50 mL), or a feed , or 1 teaspoon sugar under the tongue.
2. Feed every 2 hr for at least the first day.
3. Keep warm
4. Start broad-spectrum antibiotics
If unconscious:
.1. Immediately give sterile 10% glucose (5 mL/kg) by IV
.2. Feed every 2 hr for at least first day. Use nasogastric (NG) tube if unable to drink
3. Keep warm.
4. Start broad-spectrum antibiotics
2.Prevent/treat hypothermia axillary <35°C ; rectal <35.5°C
Actively rewarmFeed
Skin-to-skin contact with carer (“kangaroo technique”) or dress in warmed clothes, cover head, wrap in warmed blanket and provide indirect heat (e.g. heater)
Monitor temperature hourly (or every 30 min if using heater)
Stop rewarming when rectal temperature is 36.5°C (97.7°F)
3. Prevent/treat dehydration
Do not give IV fluids unless the child is in shock
Give ReSoMal l (37.5 mmol Na/L) is a low-sodium rehydration solution for malnutrition 5 mL/kg every 30 min for first 2 hr orally or NG tube
Then give 5-10 mL/kg in alternate hours for up to 10 hr. Amount depends on stool loss and eagerness to drink. Feed in the other alternate hour
Monitor hourly and stop if signs of overload develop (pulse rate increases by 25 beats/min and respiratory rate by 5 breaths/min; increasing edema; engorged jugular veins.
Stop when rehydrated (3 or more signs of hydration: less thirsty, passing urine, skin pinch less slow, eyes less sunken, moist mouth, tears, less lethargic, improved pulse and respiratory rate).
.4. Correct electrolyte imbalance—deficit of potassium and magnesium, excess sodium
5. Prevent/treat infectionsIf no complications Amoxicillin oral 25 mg/kg twice daily for 5 days
If complications (shock, hypoglycemia, hypothermia, skin lesions,
respiratory or urinary tract infections, or lethargy/sickly) Gentamicin (7.5 mg/kg IV or IM) once daily for 7 days And Ampicillin (50 mg/kg IV or IM) every 6 hr for 2 days, then oral amoxicillin 25-40 mg/kg) every 8 hr for 5 days
6.Correct micronutrient deficiencies
Do not give iron in the stabilization phase especially for children with kwashiorkor, for whom ferritin levels are often high. Additional iron may pose an oxidative stress; iron supplementation at this time is associated with higher morbidity and mortalityGive vitamin A on day 1 (under 6 mo 50,000 units; 6-12 mo 100,000 units; >12 mo 200,000 units) if child has any eye signs of vitamin A deficiency or has had recent measles. Repeat this dose on days 2 and 14
Folic acid 1 mg
Zinc (2 mg/kg/day) and copper (0.3 mg/kg/day). These are in the electrolyte/mineral solution and Combined Mineral Vitamin mix (CMV) and can be added to feeds and ReSoMal
Multivitamin syrup or CMV
7. Start cautious feeding
Give 8-12 small feeds of F75 to provide 130 mL/kg/day,
If gross edema, reduce volume to 100 ml/kg/day
Keep a 24-hr intake chart.
If child has poor appetite,encourage to finish the feed. If unfinished, reoffer later. Use NG tube if eating 80% or less of the amount offered
If breastfed, encourage continued breastfeeding but also give F75
Transfer to F100 when appetite returns (usually within 1 wk) and edema has been lost or is reduced
Weigh daily and plot weight
Rehabilitation:
The signals for entry to this phase are reduced/ minimal edema and return of appetite .A controlled transition over 3 days is recommended to prevent the “refeeding syndrome.”
To make the transition, for 2 days replace F75 with an equal volume of F100 and then increase each successive feed by 10mL until some feed remains uneaten (usually at around 200 mL/kg/day).
After the transition, unlimited amounts should be given of a high-energy, high- protein milk formula such as F100 (100 kcal and 3 g protein per 100 mL), or ready-to-use therapeutic food (RUTF), or family foods modified to have comparable energy and protein contents. and continue to give potassium, magnesium, and micronutrients. Add iron (3 mg/kg/day).
If breastfed, encourage continued breastfeeding
When nutritional rehabilitation has begun, caloric intake can be increased 10-20% per day, monitoring for electrolyte imbalances, poor cardiac function, edema, or feeding intolerance. If any of these occurs, further caloric increases are not made until the child’s status stabilizes.
8-Children with severe malnutrition have developmental delays, so loving care, structured play, and sensory stimulation during and after treatment are essential to aid recovery of brain function
Caloric intake is increased until appropriate regrowth or catch-up growth is initiated.
9-Catch-up growth refers to gaining weight at greater than 50th percentile for age and may require 150% or more of the recommended calories for an age-matched, well-nourished child. A general rule of thumb for infants and children up to 3 years of age is to provide 100-120 kcal/kg based on ideal weight for height.
Community-based treatment:
Many children with severe acute mal-nutrition can be identified in their communities before medical complications arise.If these children have a good appetite and are clinically well, they can be rehabilitated at home through community-based therapeutic care,
which has the added benefit of reducing their exposure to nosocomial infections and providing continuity of care after recovery.It also reduces the time caregivers spend away from home and their opportunity costs, and can be cost-effective for health services.
Community-based therapeutic care comprises steps 8-10, plus a broad-spectrum antibiotic (step 5).
RUTF ready to use therapeutic food is specially designed for rehabilitating children with severe acute malnutrition at home.
It is high in energy and protein and has electrolytes and micronutrients added.
The most widely used RUTF is a thick paste that contains milk powder, peanuts, vegetable oil, and sugar.
Pathogens cannot grow in it because of its low moisture content.
Hospitalized children who have completed steps 1-7 and the transition can be transferred to community-based care for completion of their rehabilitation, thereby reducing their hospital stay to about 7-10 days.
Refeeding Syndrome
Refeeding syndrome can complicate the acute nutritional rehabilitation of children who are undernourished from any cause. It is rare when the WHO recommendations for the treatment of malnutrition are followed ; however, it may follow overly aggressive enteral or parenteral alimentation.
Malnutrition usually has normal serum electrolytes but is associated withintracellular electrolyte depletion. When excessive carbohydrates are administered, the resultant increase in serum insulin levels may produce hypokalemia, hypophosphatemia, and hypomagnesemia.
The hallmark of refeeding syndrome is the development of severe hypophosphatemia after the cellular uptake of phosphate during the 1st wk of starting to reefed.
Serum phosphate levels of ≤0.5 mmol/L can produce weakness, rhabdomyolysis, neutrophil dysfunction, cardiorespiratory failure, arrhythmias, seizures, altered level of consciousness, or sudden death.
Phosphate levels should be monitored during refeeding, and if they are low, phosphate should be administered during refeeding to treat severe hypophosphatemia
• .
COMPLICATIONS OF MALNUTRITION• Malnourished children are more susceptible to infection, especially sepsis, pneumonia, and gastroenteritis.
• Hypoglycemia is common after severe fasting, but may be a sign of sepsis.
• Hypothermia : signify infection or with bradycardiadecreased metabolic rate
Bradycardia and poor cardiac output heart failure, exacerbated by acute fluid or
solute loads.
• Vitamin A and zinc deficiencies are common in the developing world and are an
important cause of altered immune response and increased morbidity and mortality.
• Children may have permanent growth stunting (from malnutrition in utero, infancy, or adolescence) and delayed development (from malnutrition in infancy or adolescence).