
Behavioral disorders in children
Lec .4 Dr.Farah Sameer Yahya
Wed. 15/10/2019
Pica
Pica involves the persistent eating of nonnutritive, nonfood substances (e.g., paper, soap, charcoal, clay, paint etc.)
over a period of at least 1 mo. The eating behavior is inappropriate to the developmental level and, therefore,
a minimum age of 2 yr is suggested. The eating behavior is not part of a culturally supported or socially
normative practice.
EPIDEMIOLOGY
Pica can occur throughout the lifetime, but occurs most commonly in childhood. It appears to be more common
in those with intellectual disability and autism spectrum disorders, and to a lesser degree in obsessive-
compulsive and schizophrenic disorders. It usually remits in childhood but can continue into adolescence and
adulthood.
Geophagia (eating earth) is associated with pregnancy and is not seen as abnormal in some cultures (e.g., rural
or preindustrial societies in parts of Africa and India).
Children with pica are at increased risk for :
A. lead poisoning
B. iron-deficiency anemia
C. mechanical bowel problems, intestinal obstruction, intestinal perforations.
D. dental injury,
E. and parasitic infections.
F. It can be fatal based on substances ingested
ETIOLOGY AND DIFFERENTIAL DIAGNOSIS of pica:
Numerous etiologies have been proposed but not proved, ranging from psychosocial causes to physical ones. They
include :-
A. nutritional deficiencies (e.g., iron, zinc, and calcium),
B. low socioeconomic factors
C. child abuse and neglect, family disorganization (e.g., poor supervision),
D. mental disorder,
E. learned behavior,
F. underlying (but undetermined) biochemical disorder,
G. and cultural and familial factors.
The differential diagnosis includes:-
a. anorexia nervosa
b. factitious disorder,
c. and non suicidal self-injury in personality disorders.
Treatment
Combined behavioral, social, and medical approaches are generally indicated for pica. Assessment for
neglect and family supervision combined with a psychiatric assessment for co-occurring mental disorders
and developmental delay are important .Behavioral treatment interventions, particularly applied
behavioral analysis in patients with intellectual disability or autism spectrum disorders, have
increasing evidence for being helpful.
The sequelae related to an ingested item can require specific treatment (e.g., lead toxicity, iron-
deficiency anemia, parasitic infestation). Ingestion of hair can require medical or surgical intervention for a
gastric bezoar.
Nocturnal Enuresis
Enuresis is defined as voiding in bed or on clothes that occurs at least twice per week for at least 3 consecutive
months in a child who is at least 5 years of age.
Five years is considered the age of anticipated 24-hour-per-day bladder control. Children who are intellectually
disabled should reach a mental age of 4 years before they are considered enuretic.
Two types of enuresis are described based on the time of occurrence of these inappropriate voiding patterns:
Diurnal enuresis describes wetting in the daytime, whereas nocturnal enuresis refers to the passage of urine during
the night.
Enuresis is described as primary when it occurs in children who have never had a period of sustained dryness and
secondary when it occurs in children who have been dry in the past for a period of at least 6 months, with nocturnal
enuresis and 3 months with diurnal enuresis.
Nocturnal enuresis can be monosymptomatic when
no
daytime symptoms to suggest lower urinary tract disorders
are present and polysymptomatic when it is associated with symptoms such as urgency, frequency, dribbling, or
daytime enuresis.
Epidemiology
Approximately 60% of children with nocturnal enuresis are boys. Family history is positive in 50% of cases.
Although primary nocturnal enuresis may be polygenetic, candidate genes have been localized to
chromosomes 12 and 13.
If one parent was enuretic, each child has a 44% risk of enuresis; if both parents were enuretic, each child has
a 77% likelihood of enuresis.
it ceases spontaneously in approximately 15% of involved children every year thereafter. Its frequency among
adults is <1%.
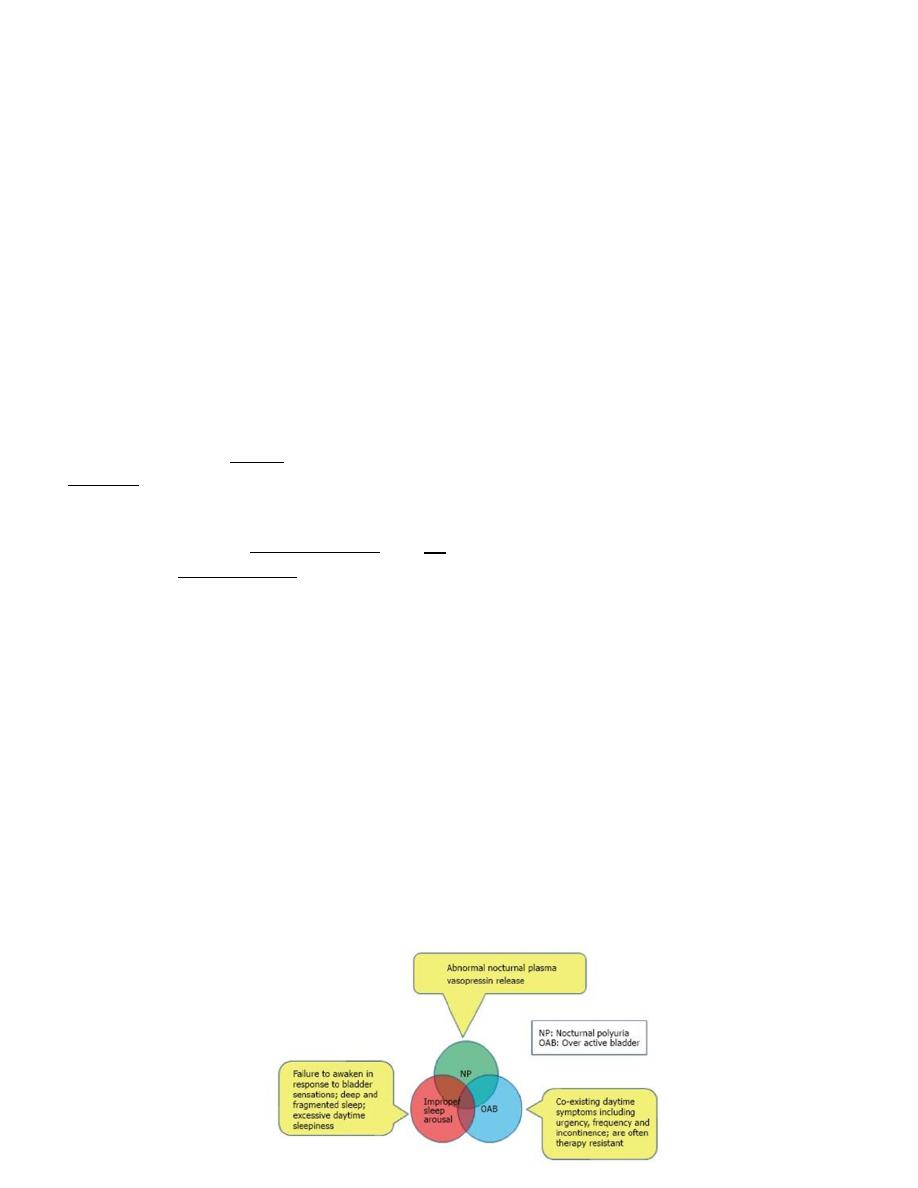
Pathophysiology of nocturnal enuresis
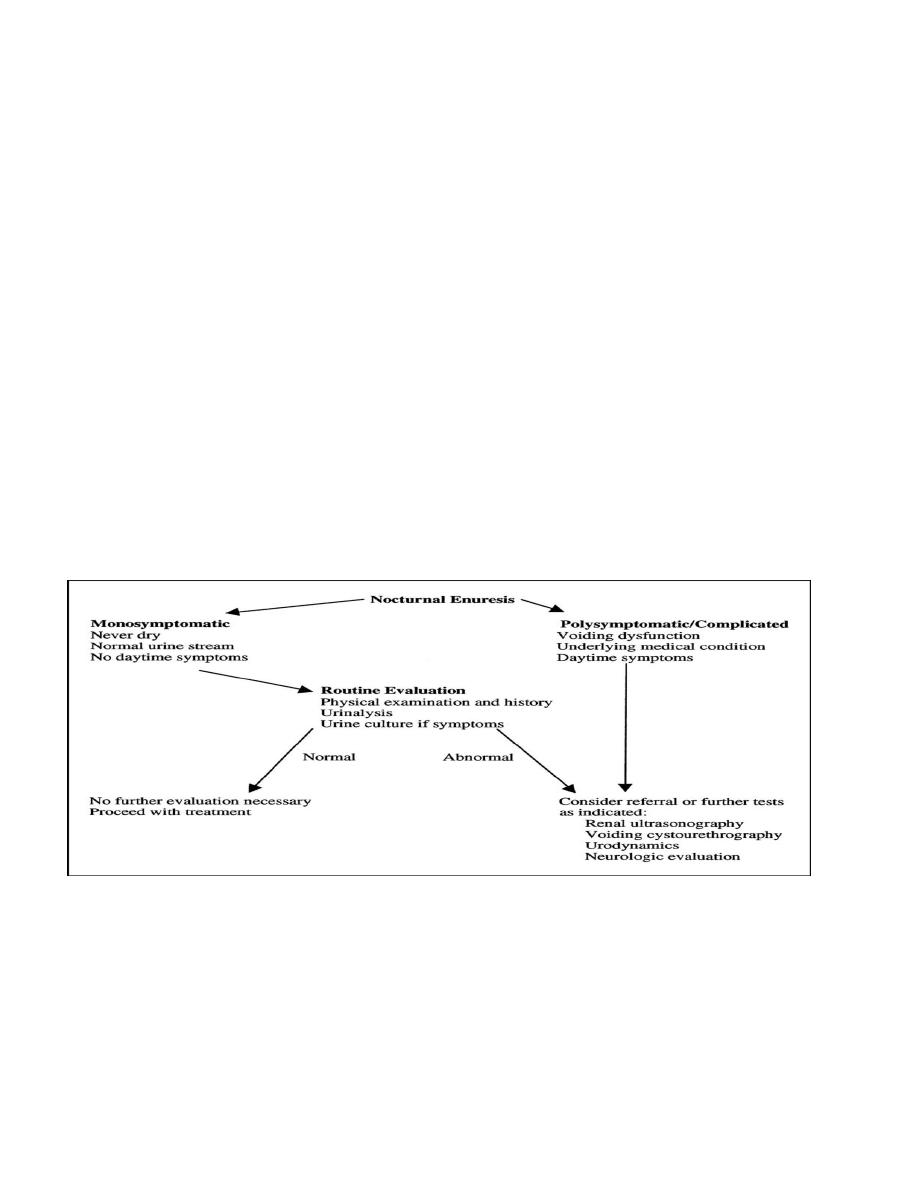
Clinical manifestations and diagnosis
A careful history should be obtained, especially with respect to:-
a. fluid intake at night and pattern of nocturnal enuresis.
b. Children with diabetes insipidus
c. diabetes mellitus
d. and chronic renal disease
e. The family should be asked whether the child snores loudly at night.
A complete physical examination should include
palpation of the abdomen and rectal examination after voiding to assess the possibility of a
chronically distended bladder.
careful examination for neurologic and spinal abnormalities.
There is an increased incidence of bacteriuria in enuretic girls, and, if found, it should be investigated
and treated.
A urine sample should be obtained after an overnight fast and evaluated for specific gravity or
osmolality to ascertain that the concentrating ability is normal. The absence of glycosuria should be
confirmed.
The growth spurt is a relatively late event; it can occur from 10.5 years of age to 16 years of age. Deepening
of the voice, facial hair, and acne indicate the early stages of puberty.
Treatment
The best approach to treatment is to reassure the child and parents that the condition is self -limited and to avoid
punitive measures that can affect the child’s psychologic development adversely.
Fluid intake should be restricted to 2 oz after 6 or 7 pm.
The parents should be certain that the child voids at bedtime. Avoiding extraneous sugar and caffeine after 4 pm
also is beneficial. If the child snores and the adenoids are enlarged, referral to an otolaryngologist should be
considered, because adenoidectomy can cure the enuresis.

Active treatment should be avoided in children younger than 6 yr of age, because enuresis is extremely
common in younger children.
Treatment is more likely to be successful in children approaching puberty compared with younger children.
1) The simplest initial measure is motivational therapy and includes a star chart for dry nights. Waking children a
few hours after they go to sleep to have them void often allows them to awaken dry, although this measure is not
curative.
2) Conditioning therapy
involves use of a loud auditory or vibratory alarm attached to a moisture sensor in the underwear. The alarm sounds
when voiding occurs and is intended to awaken children and alert them to void.
This form of therapy has a reported success of 30-60%, although the relapse rate is significant.
2)Pharmacologic therapy
is intended to treat the symptom of enuresis and thus is regarded as second line and is not curative . Direct
comparisons of the bell and bed with pharmacologic therapy favor the former because of lower relapse rates,
although initial response rates are equivalent. One form of treatment is desmopressin acetate , a synthetic analog
of antidiuretic hormone that reduces urine production overnight.
This medication is FDA-approved and is available as a tablet, with a dosage of 0.2-0.6 mg at bedtime.In the past a
nasal spray was used, but some children experienced hyponatremia and convulsions with this formulation and the
nasal spray is no longer recommended for nocturnal enuresis. Fluid restriction at night is important .
and the drug should not be used if the child has a systemic illness with vomiting or diarrhea or if the child has
polydipsia.
Desmopressin acetate is effective in as many as 40% of children. If effective, it should be used for 3-6 months,
and then an attempt should be made to taper the dosage. If tapering results in recurrent enuresis, the child should
return to the higher dosage.
For therapy-resistant enuresis or children with symptoms of an overactive bladder, anticholinergic therapy is
indicated. Oxybutynin 5 mg at bedtime often are prescribed.
The clinician should monitor for constipation as a potential side effect.
A third-line treatment is imipramine , which is a tricyclic antidepressant.
This medication has mild anticholinergic and α-adrenergic effects, reduces urine output slightly, and also
might alter the sleep pattern. The dosage of imipramine is 25 mg in children age 6-8 yr, 50 mg in children
age 9-12 yr, and 75 mg in teenagers. Reported success rates are 30-60%. Side effects include anxiety,
insomnia, and dry mouth, and heart rhythm may be affected.
If there is any history of palpitations or syncope in the child, or sudden cardiac death or unstable
arrhythmia in the family, long QT syndrome in the patient needs to be excluded. The drug is one of the most
common causes of poisoning by prescription medication in younger siblings.
In unsuccessful cases, combining therapies often is effective.Alarm therapy plus desmopressin is more successful
than either alone. The combination of oxybutynin chloride and desmopressin is more successful than either
alone. Desmopressin and imipramine also may be combined.
Encopresis and Functional Constipation
Constipation is defined as a delay or difficulty in defecation present for 2 wk or longer and significant
enough to cause distress to the patient.
Chronic Constipation: Rome III Criteria
INFANTS AND TODDLERS
Must include 1 mo. of at least 2 of the following in infants up to 4 yr. of age:
• ≤2 Defecations per week
• ≥1 Episode of incontinence after the acquisition of toilet training skills
• History of excessive stool retention
• History of painful or hard bowel movements
Presence of a large fecal mass in the rectum
• History of a large-diameter stool that might obstruct the Toilet
Accompanying symptoms may include irritability, decreased appetite, and/or early satiety. The
accompanying symptoms disappear immediately following passage
of a large stool.
CHILDREN WITH A DEVELOPMENTAL AGE OF 4-18 YR
Must include 2 or more of the following :-
• ≤2 Defecations per week
• ≥1 Episode of fecal incontinence per week
• History of retentive posturing or excessive volitional stool retention
• History of painful or hard bowel movements
• Presence of a large fecal mass in the rectum
• History of a large-diameter stool that might obstruct the toilet
Encopresis
is defined as voluntary or involuntary passage of feces into inappropriate places at least once a month for
3 consecutive months once a chronologic or developmental age of 4 yr has been reached.
Encopresis is not diagnosed when the behavior is exclusively the result of the
direct effects of a substance (e.g., laxatives). Subtypes include retentive encopresis (with constipation
and overflow incontinence) representing 65-95% of cases, and nonretentive encopresis (without
constipation and overflow incontinence).
Encopresis can persist from infancy onward (primary) or can appear after successful toilet training
(secondary).
Functional constipation
This encompasses all children in whom constipation does not have an organic aetiology.
Approximately 40% of children with functional constipation develop symptoms during the 1st year of life,
and incidence peaks at 2–4 years with an excess of boys.
The exact aetiology of functional or ‘simple’ constipation remains
uncertain
Onset often occurs during one of three periods:
when changed to formula milk or weaned
Toddlers acquiring toilet skills with painful defecation
At start of school
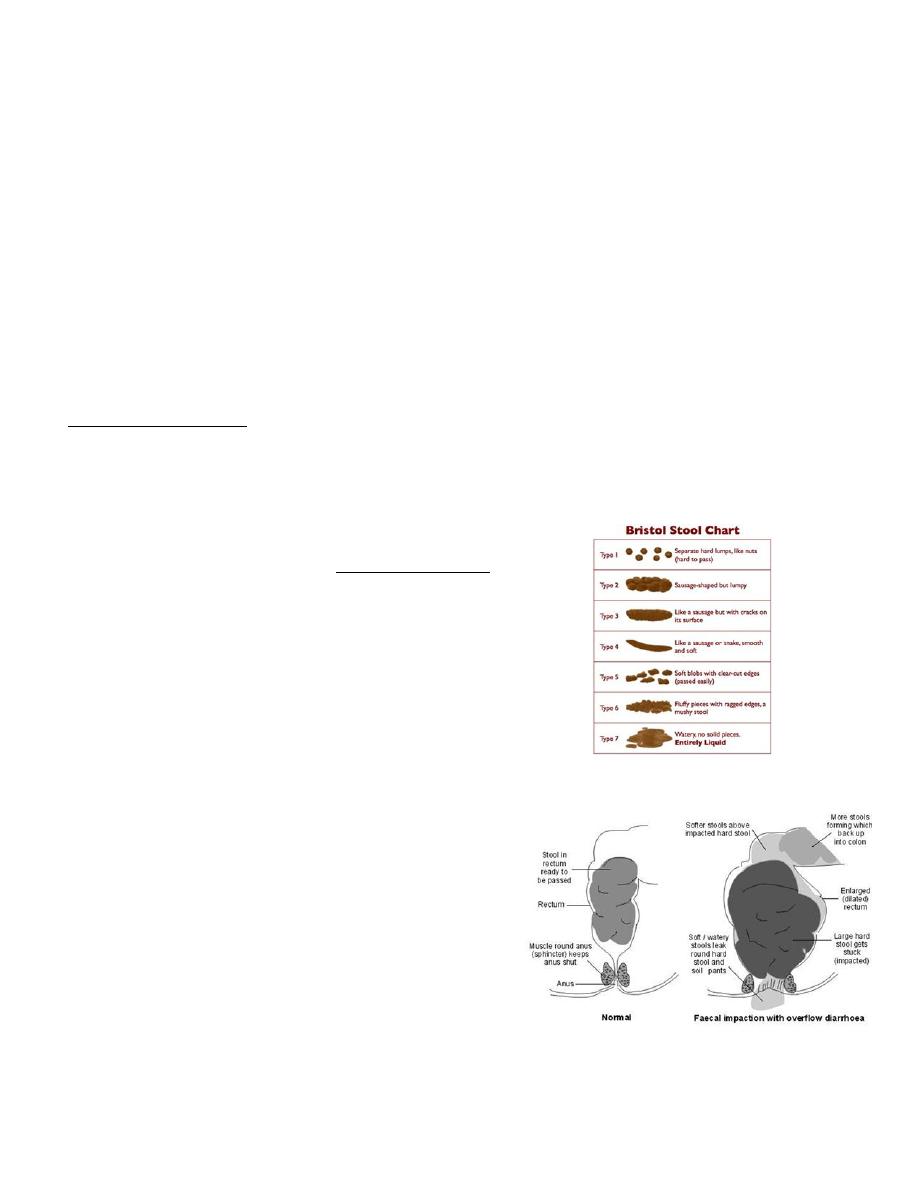
Faeces accumulate and stretch the rectum leading to a vicious circle in which the desire to defecate is
reduced and passage of infrequent large stools is painful.
‘Overflow incontinence’ causes soiling.
History and physical examination often demonstrates
Children with encopresis often present with reports
of underwear soiling(miss dx as diarrhea)
In retentive encopresis, associated complaints of difficulty with defecation, abdominal or rectal
pain, impaired appetite with poor growth, and Urinary tract symptoms include recurrent urinary
tract infection and enuresis.

Children often have large bowel movements that obstruct the toilet.
There may also be retentive posturing or recurrent urinary tract infections.
Nonretentive encopresis is more likely to occur as a solitary symptom and have associated
primary underlying psychological etiology.
Children with encopresis can present with poor school performance and attendance that is
triggered by the scorn and derision from schoolmates because of the child’s offensive odor.
a large volume of stool palpated in the suprapubic area;
rectal examination demonstrates a dilated rectal vault filled with stool.
The presence of a hair tuft over the spine or spinal dimple. failure to elicit a cremasteric refl ex or
anal wink suggests spinal pathology.
A tethered cord is suggested by decreased or absent lower leg reflexes.
In refractory patients (intractable constipation), specialized testing should be considered to rule
out conditions such as hypothyroidism, hypocalcemia, lead toxicity, celiac disease.
Children with no evidence of abnormalities on physical examination rarely require radiologic
evaluation.
Selected children can benefit from
a) MRI of the spine to identify an intraspinal process,
b) motility studies to identify underlying myopathic or neuropathic bowel abnormalities,
c) or a contrast enema to identify structural abnormalities. (functional constipation reveal
megarectosigmoid )
Treatment
Therapy for functional constipation and encopresis includes:-
patient education,
relief of impaction,
and softening of the stool.
1)Caregivers must understand the pathophysiology of constipation.There needs to be a focus on
adherence with regular postprandial toilet sitting and adoption of a balanced diet. In addition,
caregiver should be instructed not to respond to soiling with retaliatory or punitive measures.
2)Disimpaction If an impaction is present on the initial physical examination, an enema is usually
required to clear the impaction.
3)Maintenance
This can be achieved using stool softeners, either polyethelne glycol PEG-based or Lactulose.addition,
parents should be encouraged to:Increase fluid, fruit, and vegetable intake ,Use gastrocolic reflex in toilet
training: encourage the child to sit on the toilet for 5 min after each meal.Use a diary and star chart to
monitor bowel habit and adherence to therapy.

