• Food Allergy & hypersensitivity:
• It is ‘an immune response to food proteins.It occurs in 4-8% children commonly with those of +ve family Hx of atopy or allergies. It is IgE mediated or non-IgE mediated.
• its presentation varies with the agent and child's age:
• in infants the most common causes are milk, egg & peanut
• in older children peanut, tree nut and fish.
Fruit allergy, although common, is usually mild, causing an itchy mouth but no systemic symptoms, is called {oral allergy syndrome} & usually associated with spring hay fever due to cross-reaction with tree pollens.
Kiwi fruit, however, can cause anaphylaxis.
Food hypersensitivity is not related to food aversion, where the person refuses the food for psychological or behavioural reasons.
Management:
It involves avoidance of the food but, especially for milk & nuts, this is very difficult as they may be present in small quantities in many foods and food labels are often unclear. The advice of a pediatric dietician is essential.
• In addition, the child & family must be able to manage an allergic attack.
Drug Mx for mild reactions (no cardiorespiratory symptoms) is with antihistamines.
If the child had a severe reaction or has asthma, Rx is with epinephrine(adrenaline) given IM by auto-injector, which the child or parent should carry with them at all times.
• .
Cow’s Milk Protein Allergy(CMPA)
• Results from an immunological reaction to one or more of milk proteins,only 0.5% of breast fed infants are affected & 5-15% of infants show suggestive symptoms. It is either IgE- or non-IgE mediated.
• Prevalence highest < 1 year
• Cow’s Milk Intolerance:
• A transient intolerance to lactose and/ or protein found in cow’s milk following an infective episode of diarrhoea
• CHO intolerance is due to mucosal damage which results in reduced activity of disaccharide enzymes
• Protein intolerance is an immunomediated reaction to cow’s milk protein following mucosal damage.
• Clinical presentation:
• Early reactions (within 45 minutes):• Urticaria
• Angio-oedema
• Vomiting
• Acute flare up of atopic dermatitis
• Medium (45 minutes to 20 hours)
• Pallor
• GIT symptoms
• Late reactions (after 20 hours)
• Atopic dermatitis
• Respiratory symptoms
• Diarrhoea
•
Symptoms of CMPA
IgE-mediated(within 30 min)Non-IgE mediated(hrs-ds)
Anaphylaxis
Skin (50-60%):
Angio-oedema
Urticaria
Pruritis
GI (50-60%):
Nausea/Vomiting
Colicky abdo pain
Resp (20-30%):
Wheezing
Rhinitis
Laryngeal oedema
Asthma
Skin: Dermatitis
GIT:Chronic diarrhoea( intestinal protein loss produces edema and a protein-losing enteropathy)
Iron deficiency anaemia
Colic
Food refusal and poor growth
GERD
Blood in stool
Constipation
Enterocolitis
Eosinophilic oesophagogastroenteropathy
Respiratory:asthma
Examples of food allergy and hypersensitivity to milk. (b and c) Widespread urticaria and lip swelling during milk challenge
• Evaluation of a child with suspected CMPA:
• A comprehensive history:atopic one parent( risk 20-40%) or both(risk 40-50%) or sibling.• Symptoms:either GIT, skin or respiratory
• CMPA in Breast fed Infants:
• Symptoms include skin or GIT
• Most of symptoms are mild to severe.
• Infants with atopic dermatitis:
• Risk of CMPA x 4
• Risk of egg allergy x 8
• Diagnosis:
• allergy focused clinical Hx with careful & complete PE• IgE specific antibody
• Skin Prick Testing
• Elimination Diet & Food Challenge
• rectal mucosal biopsy shows eosinophilic inflammation of the mucosa.
• Visual findings at proctoscopy usually include mucosal friability & lymphoid hyperplasia.
• Treatment:
• Breast fed infants: Maternal exclusion diet avoiding food containing ( dairy products)
• Bottle fed infants: Cows Milk Free formula:
• Extensively hydrolysed Formulae (e.g., Nutramigen, Pregestamil, or Alimentum).
• Amino Acid based Formulae
• Prognosis:
• 50% resolve in first year of life
• 60-70% resolve by second year of life
• 80-90% resolve by fifth year of life
Skin prick testing. A drop of the allergen is placed on the skin, the site is marked and pricked with a needle, and any weal measured. Multiple +ve results are present
• Lactose intolerance
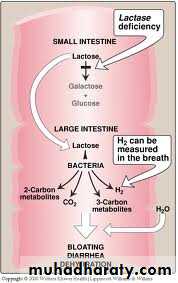
• Also called lactase deficiency and hypolactasia, is the inability to digest lactose, a sugar found in milk ( dairy products) .It is a genetically-determined.
• Lactase deficiency has a number of causes and is classified as one of three types:
• 1.Primary lactase deficiency(Primary adult type-hypolactasia) is genetic, only affects adults caused by the absence of a lactase persistence allele. It is the most common cause of lactose intolerance
2.Secondary, acquired, or transient lactase deficiency is caused by an injury to the small intestine, usually during infancy, from acute gastroenteritis(rotavirus infection),celiac disease, chemotherapy, intestinal parasites or other environmental causes.
• 3.Congenital lactase deficiency(CLD) is a very rare, autosomal recessive genetic disorder that prevents lactase expression from birth. It is particularly common in Finland. People with congenital lactase deficiency cannot digest lactose from birth.
• Clinical presentation:
• abdominal bloating & cramps, flatulence, diarrhea, nausea, borborygmi (rumbling stomach) and vomiting (particularly in adolescents).• These appear 30 min- 2 hrs after milk consumption. The severity of symptoms typically ↑ with the amount of lactose consumed; most lactose-intolerant people can tolerate a certain level of lactose in their diet without ill-effect.
pathophysiology
• Laboratory Studies:
• not mandatory, & often simple dietary changes that reduce or eliminate lactose from the diet relieve symptoms.• Stool exam: acidic stool PH(A stool pH ˂ 5.3 is suggestive of CHO malabsorption, whereas a stool pH ˃ 5.6 is evidence against this Dx). +ve for reducing substances(non specific)
• Low lactase activity in jejunal mucosa.
• Breath hydrogen test: Increased hydrogen in expired air.
DDx
Giardiasis
Inflammatory Bowel Disease
Irritable Bowel Syndrome
• Treatment:
• Advise pts to reduce or restrict products containing lactose.• Lactose-free formulas(LF) (based on either soy or cow's milk) are very effective. Yogurt and fermented products, such as cheeses, are better tolerated than regular milk.
• Commercially available lactase enzyme preparations are effective in reducing symptoms
• Supplemental calcium should also be recommended.
• In 2ry lactase def., Rx is directed at underlying cause.
Diet
Avoid or reduce intake of lactose-containing foods.Most pts who are lactose intolerant can ingest as much as 240 mL of milk without symptoms.
Certain medications & foods contain hidden lactose, such as breads, margarine, salad dressings, and candies.
Complications of lactose intolerance: may include osteopenia.