Approach to Shortness of Breath (Dyspnea)
Dr. Zaid M. YassenAsst. Prof. Family Medicine
Dyspnea derives from Greek for “hard breathing”.
It is often also described as “shortness of breath”.This is a subjective sensation of breathing, from mild discomfort to feelings of suffocation.
Always when managing a patient with dyspnea, one must quickly check the ABC’s (airways, breathing, and circulation).
Once satisfied with the stability of these aspects of the patient’s vitals, one may then proceed to the history and physical part of the assessment which should provide the diagnosis most cases.
During assessment, one can initiate management based on initial assessment:
1)Place all patients on supplemental oxygen, pulse oximetry, and cardiac monitor
2)Initiate therapy for suspected cause of dyspnea such as:
Asthma/COPD --nebulized bronchodilators and I.V. steroids
Congestive heart failure -- diuresis, morphine, nitrates, sit upright
Intubate patients if impending respiratory failure
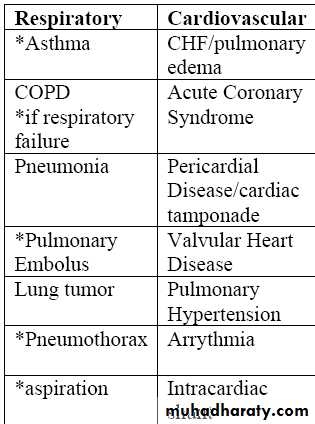
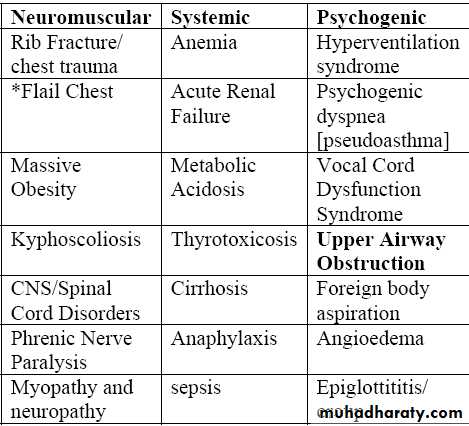
Think of the etiology as arising from 4 main categories:
RespiratoryCardiac
Neuromuscular
Psychogenic and other systemic causes.
The following table lists the common causes under these category in order of importance.
History:
Ask about the onset and course of dyspnea and if it was a chronic issue.One can think of:
1- Very sudden onset [minutes] and [usually] immediately life threatening conditions such as flail chest, pulmonary embolism, and asthma.
2- Acute [hours] causes of dyspnea include pneumonia, CHF [pulmonary edema], pericardial disease, valvular heart disease, and acute renal failure.
3- Subacute [days/weeks] etiologies could also include pneumonia ,TB, CHF, pericardial disease, and anemia.
4- Chronic [recurrent/months] causes of dyspnea are COPD, CHF, Neuromuscular problems, pulmonary hypertension, anemia, and asthma.
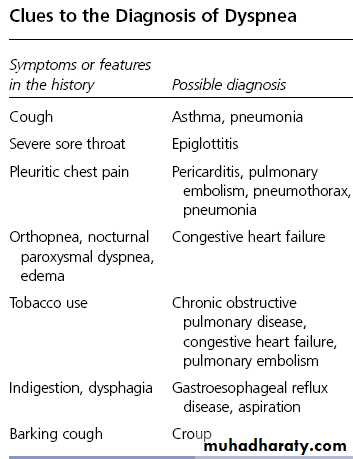
Ask about the following associated symptoms:
Stridor.
Cough – sputum production and color.
Fever and chills, sweats, lethargy.
Pleuritic chest pain, wheeze, chest tightness, hemoptysis, hoarseness.
Edema, weight loss/gain, orthopnea, PND, anxiety, confusion, lightheadedness.
Physical Examination:
Check for tachycardia, tachypnea, fever, and hypertension.
Weight increase may signal worsening CHF.
Contractions of the accessory muscles of respiration suggest severe difficulty.Physical Examination:
Prolonged expiratory phase are signs outflow obstruction.Retraction of the intercostal muscles on inspiration is characteristic of emphysema.
Percuss for dullness and hyperresonance.
Physical Examination:
Auscultate for wheezes, and quality of breath sounds.Crackles suggest fluid in the airway, as occurs with bronchitis, pneumonitis, and CHF.
Normal findings on lung examination do not rule out pulmonary pathology (probability and the likelihood that it is severe).
Physical Examination:
The cardiac examination should focus on signs of left-sided heart failure, detection of left-sided heart murmurs, and signs of pulmonary hypertension and its consequences.
Examine the abdomen for ascites and hepatojugular reflux as well as the legs for edema.
Standard workup for dyspnea:
• CXR• EKG