
1
) ﻋﺪد اﻻوراق
10
(
ﻋﯿﻮن
9
2
/
1
1
/
2019
.د
ﻋﺰام
Lec: 10
Laser in ophthalmology and vitreous
Objectives:
1 To record laser properties and emphasize on laser tissue
interactions.
2 To identify clinical application of laser in ophthalmology.
3 To tell anatomy and physiology of vitreous humor.
4 To differentiate causes of vitreous opacities with special
emphasis with regard of vitreous haemorrhage.
5 To identify the role of vitrectomy in various ocular pathologies.
Out-lines:
1 Laser properties.
2 Clinical laser application in ophthalmology.
3 Anatomy and Physiology of vitreous humor.
4 Vitreous opacities.
5 Indications of vitrectomy.
2
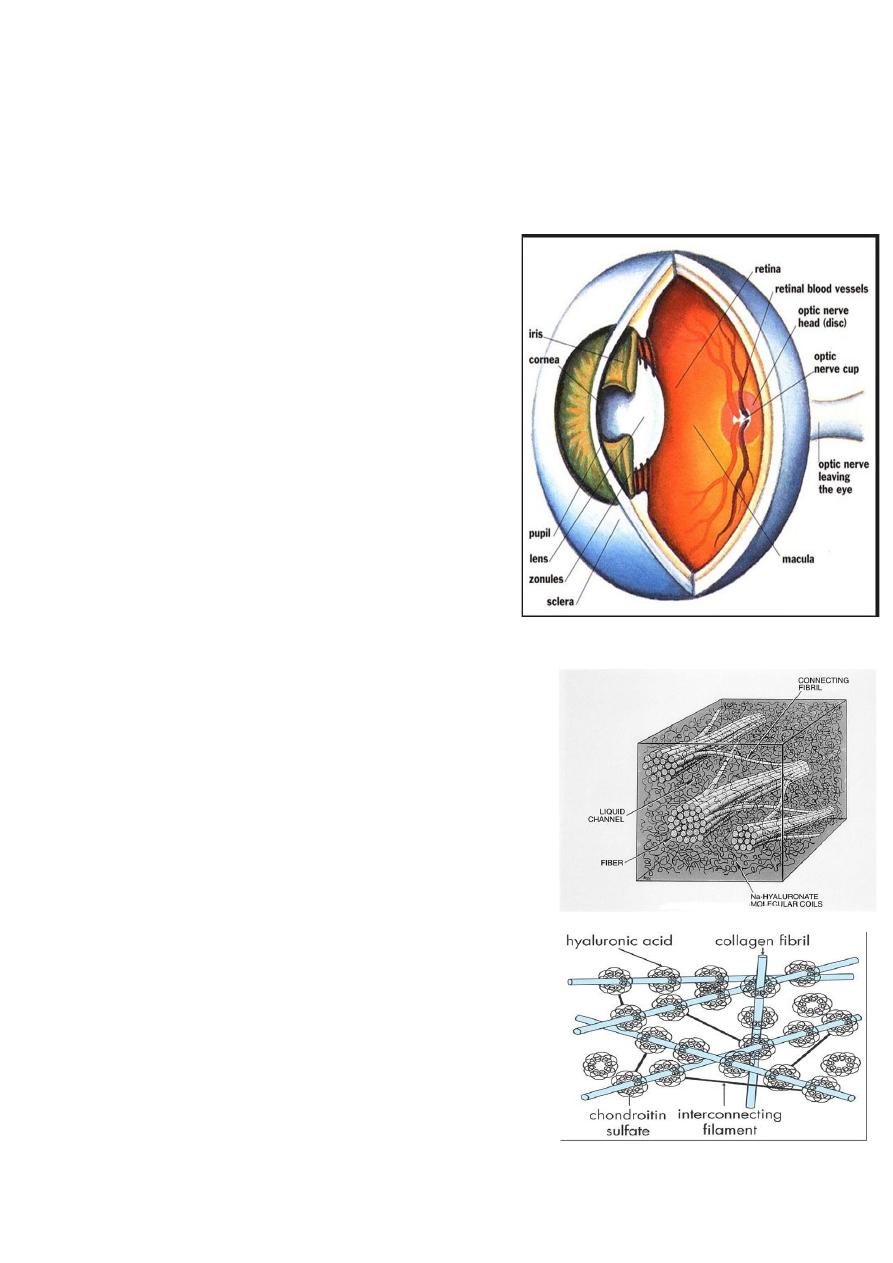
Vitreous Body:
The transparent vitreous body,
or hyaloid is one of the most delicate
connective tissues in the body.
A. It occupies the posterior or larger
compartment of the eye, filling the globe
between the internal limiting membrane
of the neural retina and the posterior lens
capsule.
B. The structure is composed of a
framework of extremely delicate
collagen filaments closely associated
with a large quantity of water binding
hyaluronic acid.
Anatomy of vitreous:
Features:
• Virtually acellular viscous content of
the globe.
• Framework of collagen fibrils
reinforced with hyaluronic acid
molecules
• 98 % water.
• Volume = 4-5 ml in emmetropic eye.
3
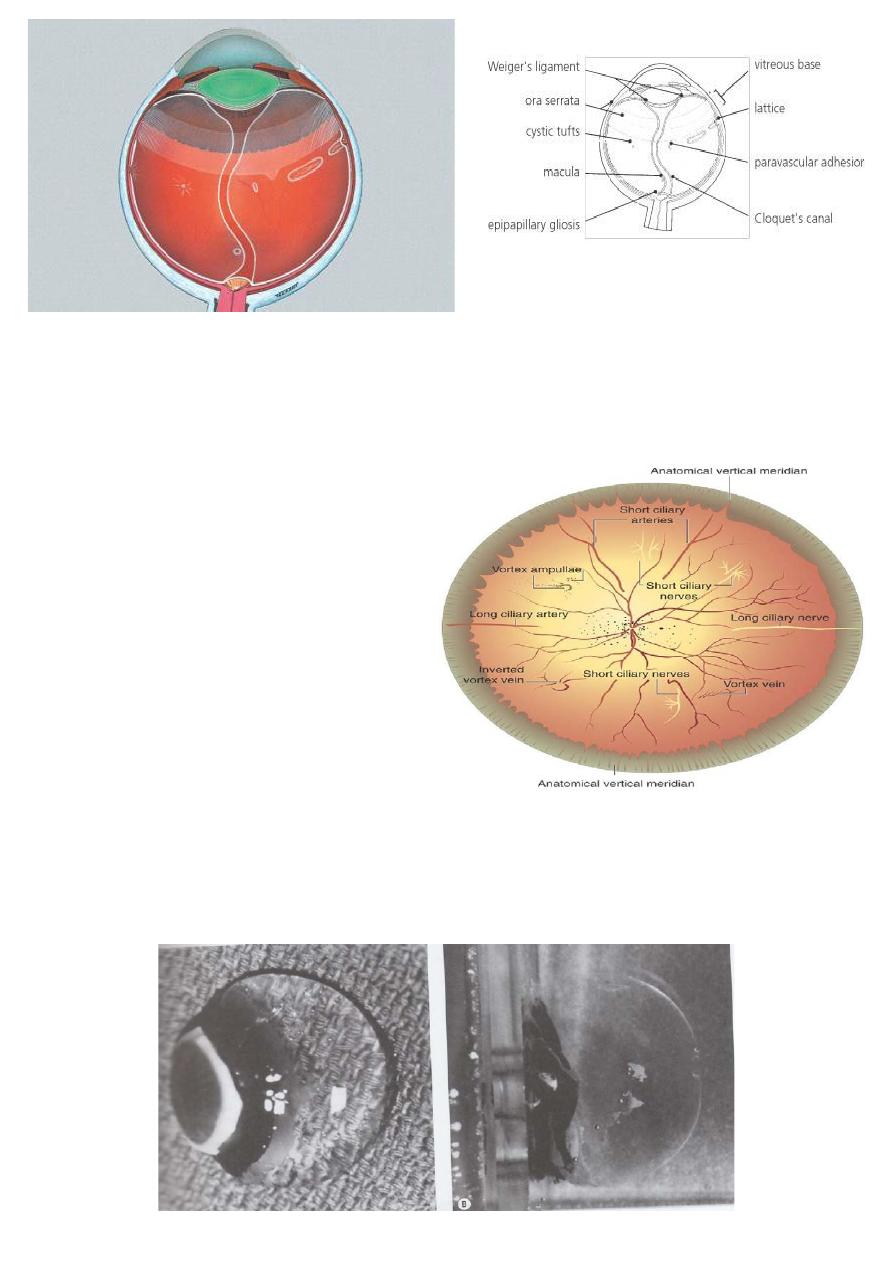
During embryologic development, the hyaloidal vasculature passes
through Cloquet’s canal to perfuse the embryonic lens before
regressing during the second trimester.
Ora serrata:
Attachments: Ora serrata most
peripheral attachment of
vitreous to retina.
Vitreous base:
3-4 mm annular attachment
Very strong straddling ora
serrata.
Ageing changes:
Dissociation of hyaluronic acid from fibrils Fibril degeneration and
reduced elasticity. Drainage of hyaluronic acid into retrovitreal space
producing posterior vitreous detachment (PVD).
4
Vitreous opacities:
1 Muscae volitantes: remnants of hyaloid system.
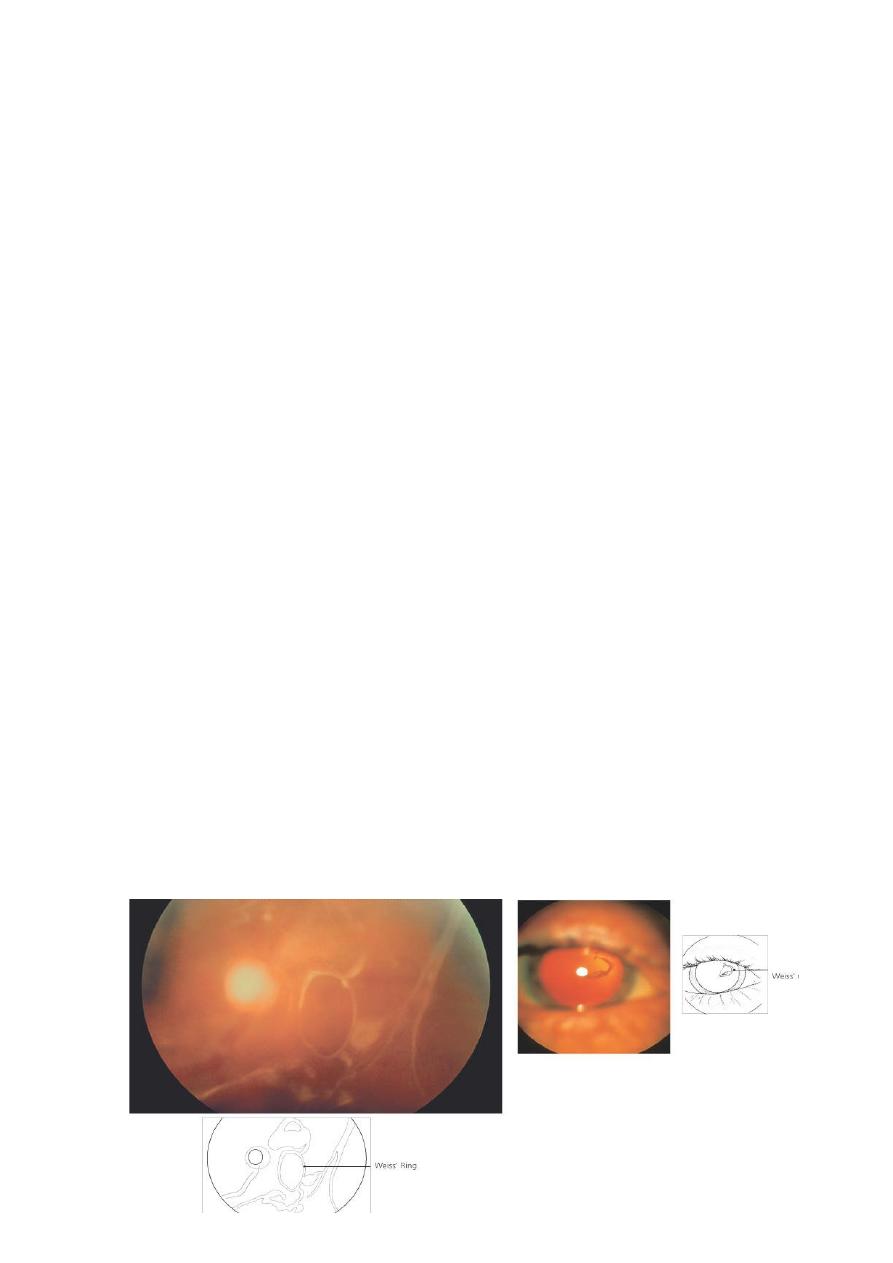
2 Syneresis: the Weiss ring ( posterior vitreous detachment PVD )
3 Hemorrhage
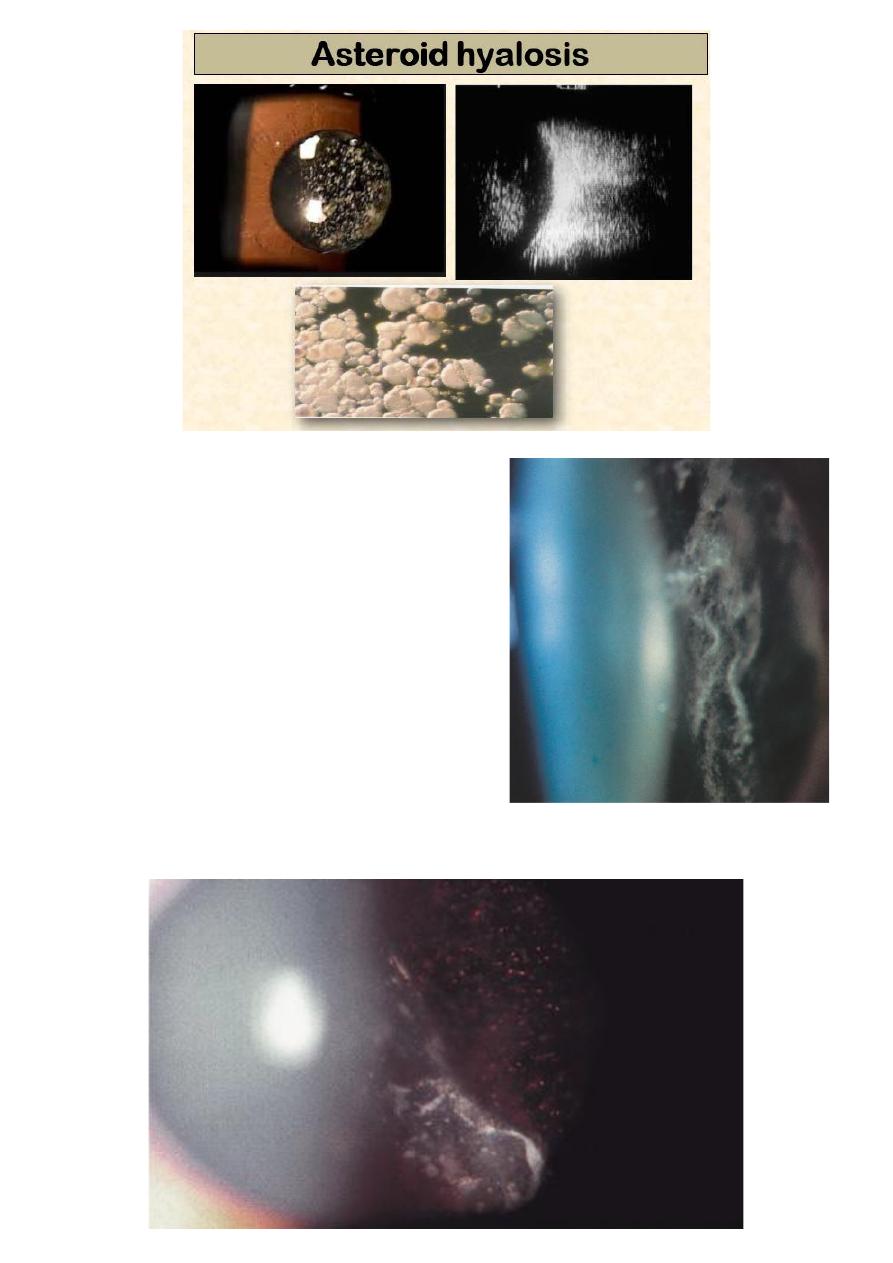
4 Asteroid hyalosis
Appears in 1 in 200 eyes
Composed of calcium soaps adherent to fibrils
Does not settle at rest
More common in diabetic people.
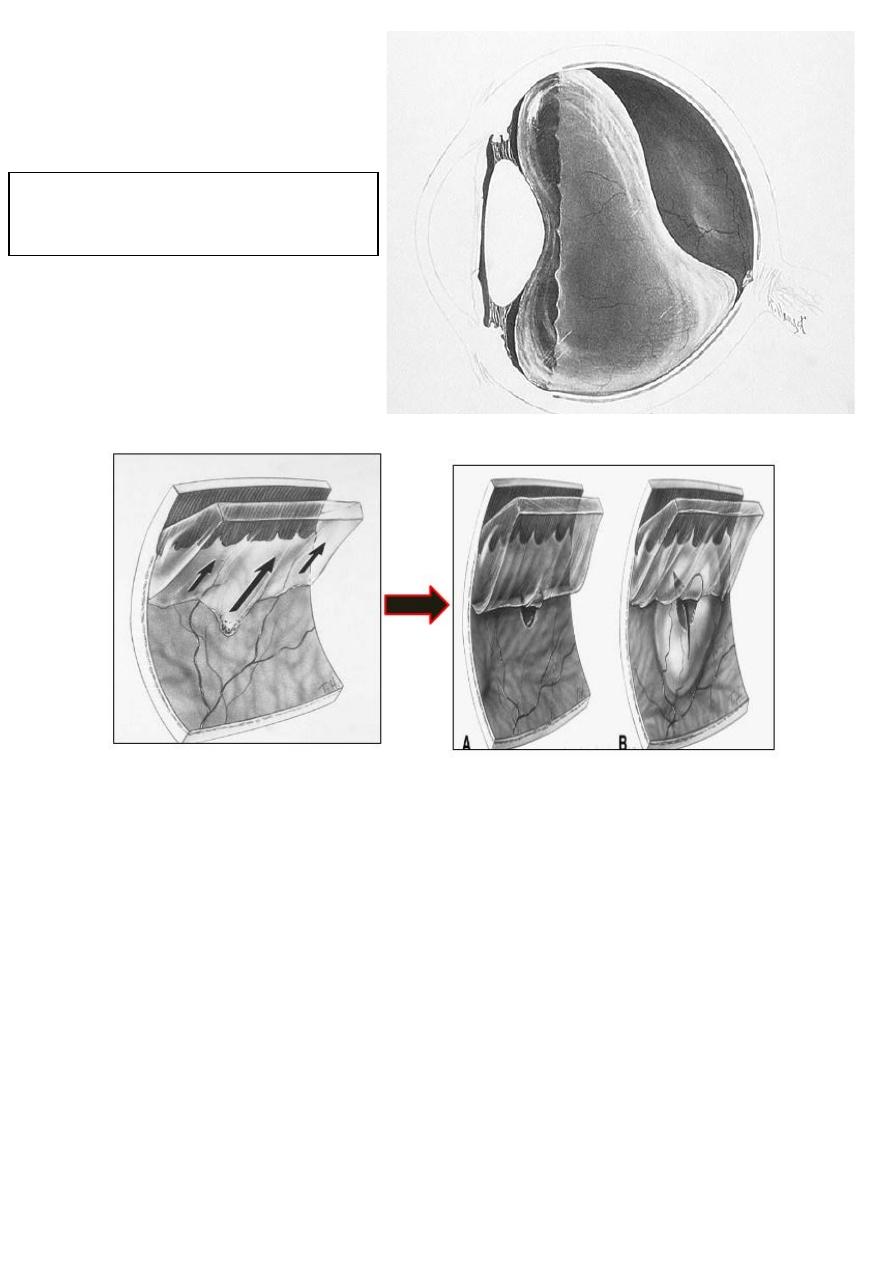
Posterior vitreous detachment
(PVD)
*Tears in the retina may develop as
a consequence of (PVD)
5
6
5 Synchisis scintillans
6 Inflammatory cells: Pars planitis,
Chorioretinitis
7 Neoplastic
8 Amyloid
9 Tobacco dust in retinal
detachment: pigment cells.
Tobacco dust (pigment cells in the
vitreous):
7
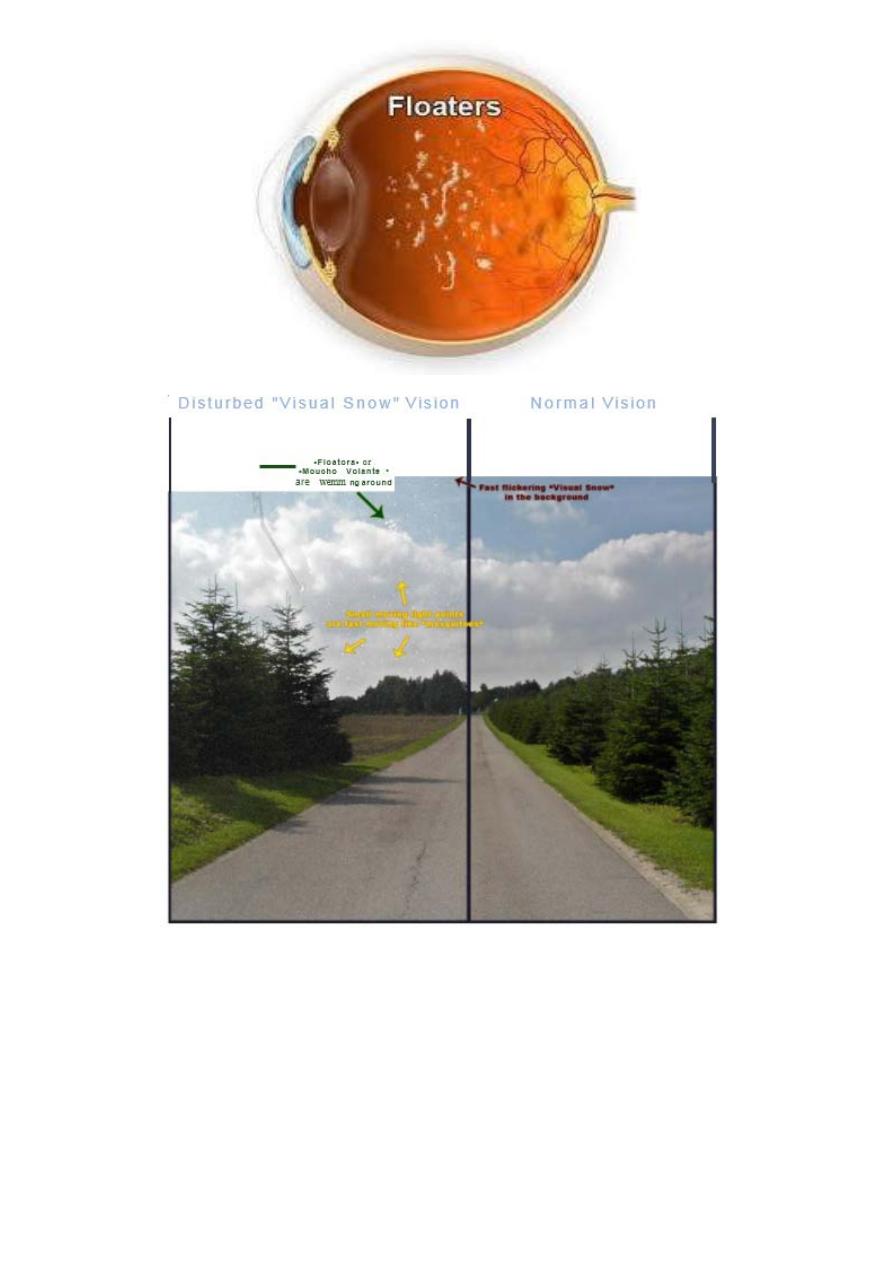
Vitreous degeneration:
1 Syneresis:
Vitreous liquefaction
Aggregation and condensation of collagen fibrils associated with
floaters
Causes:
Myopia, senescence, trauma, inflammation, hereditary e.g Stickler’s
disease
In patients who present with floaters,
You should examine the retina to rule out retinal tears.
Intervention is indicated when:
a) the number of floaters suddenly increase.
b) flash lights.
c) black curtain.
2 Detachment
Collapse of vitreous gel Associated with floaters and photopsia
Causes:
Senile, myopia, post inflammatory, post-vitreous hemorrhage, and
diabetic retinopathy.
Posterior vitreous detachment (PVD):
8
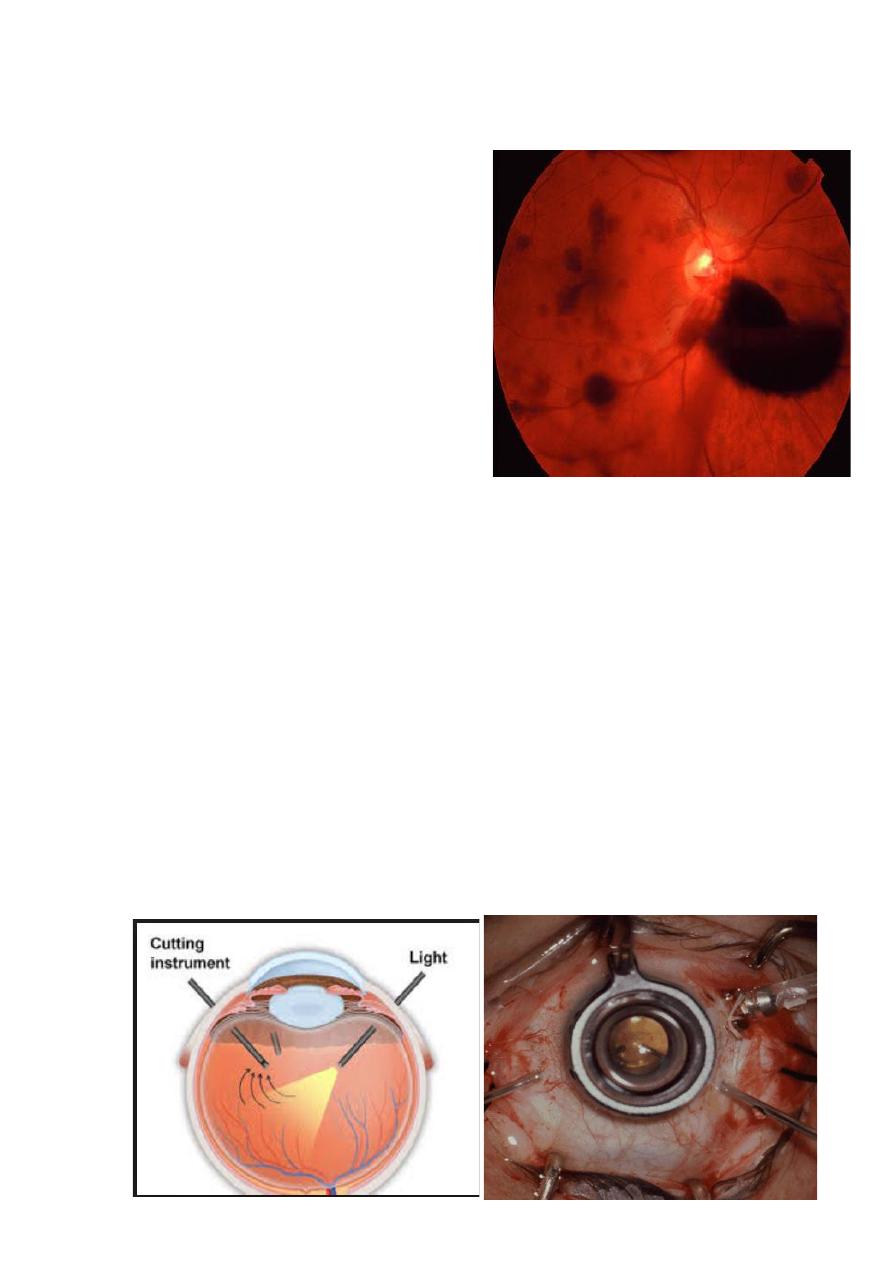
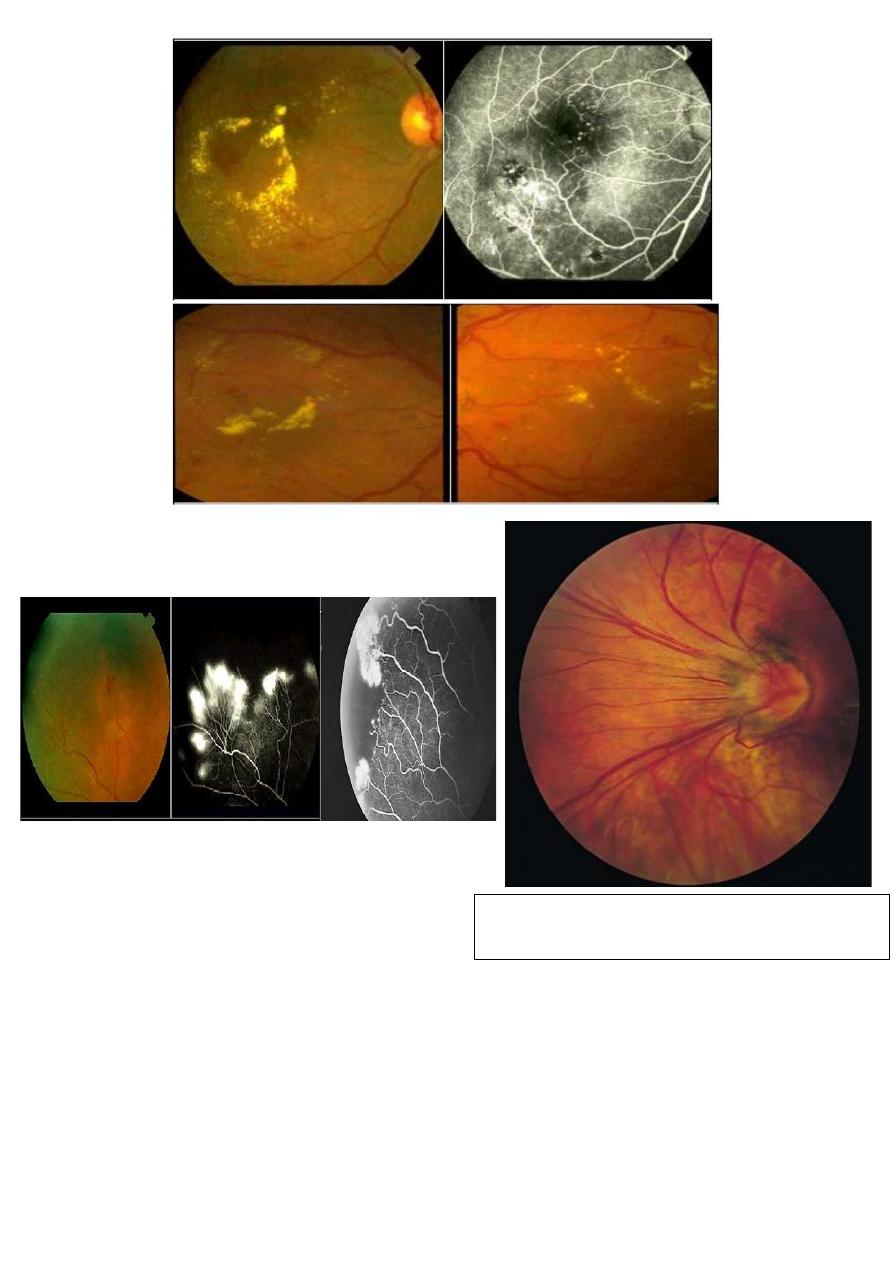
Vitreous Hemorrhage:
1- causes:
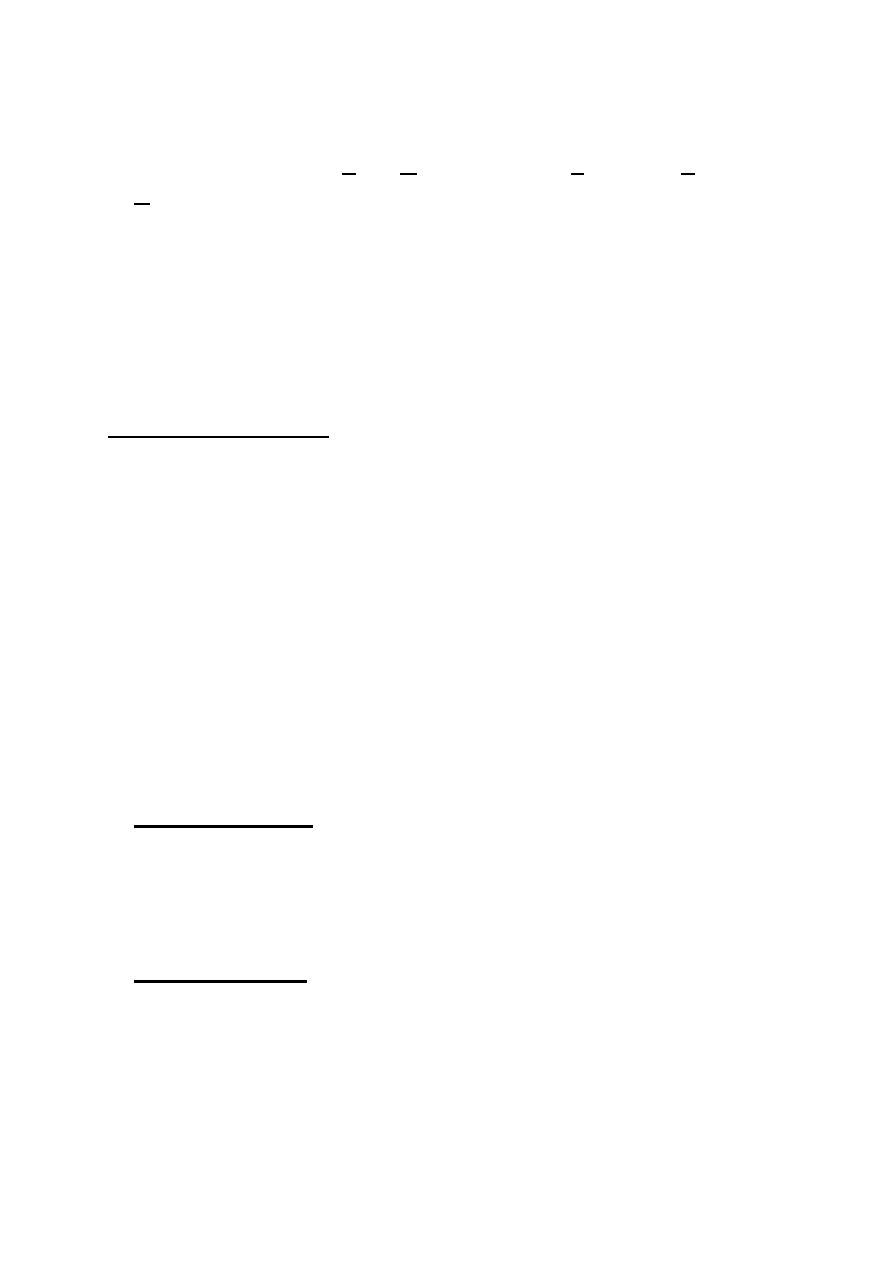
Proliferative retinopathy: DM,
retinal vein occlusion, sickle cell
retinopathy and retinopathy of
prematurity.
(Posterior vitreous detachment)
Trauma
Disciform macular degeneration
Blood dyscrasias
Subarachnoid hemorrhage (Terson’s syndrome)
Vitreous hemorrhage usually takes 2-3 months to resolve, And
non- resolving vitreous hemorrhage is an indication for
vitrectomy.
2- Complications:
Syneresis
Inflammation and fibrosis: leads to tractionl detachment
Haemosiderosis
Synchisis scintillans: cholesterol crystals; that
settles inferiorly at rest.
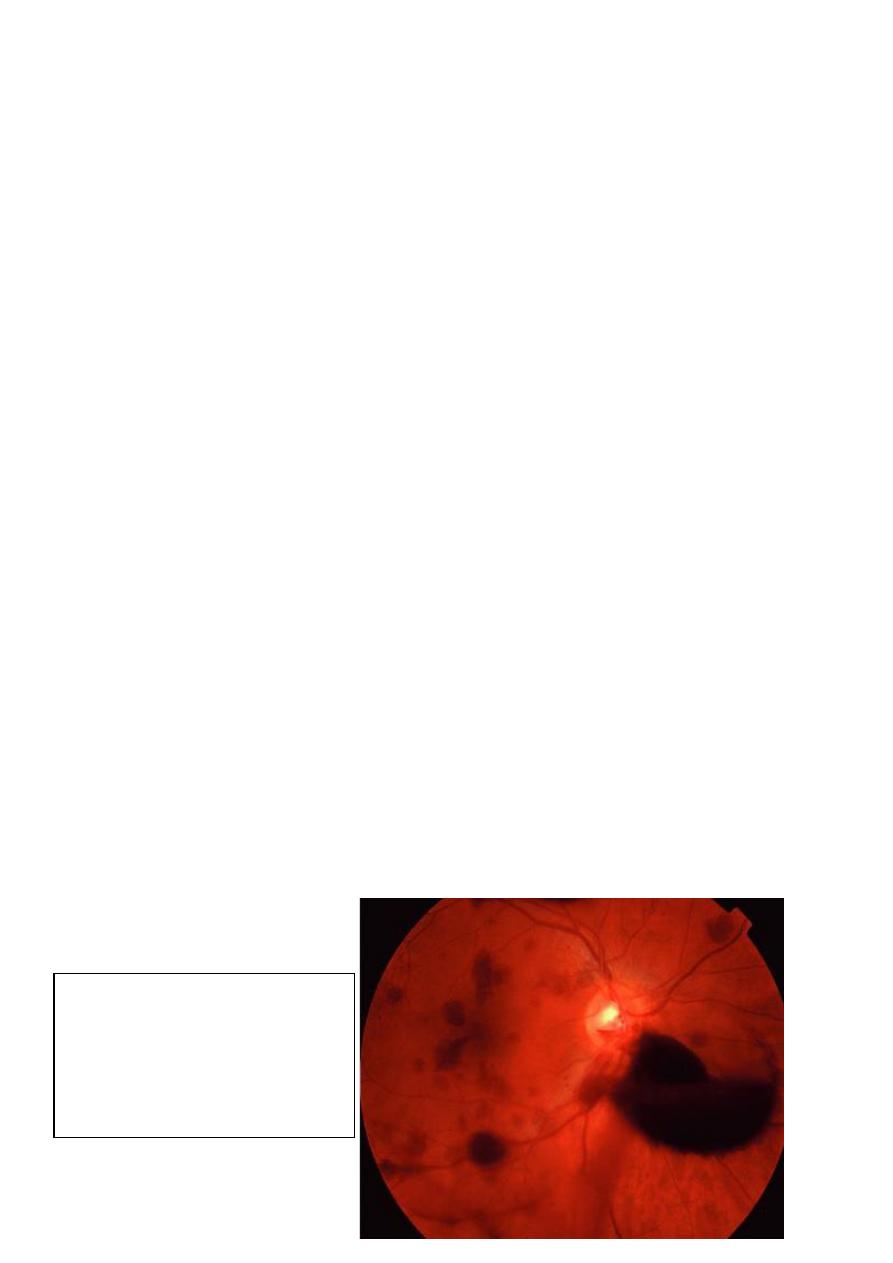
Vitrectomy:
9
Indications for Vitrectomy:
1- Anterior segment indications:
Incarceration of vitreous in cataract section
Vitreous touch causing bullous keratopathy
Accidental vitreous loss during surgery
Lensectomy e.g. for secondary cataract in childhood arthritis
Malignant glaucoma
Glaucoma drainage surgery in aphakic eye.
2- posterior segment indications:
Diabetic disease:
Persistent hemorrhage, rubeosis with poor view,
tractional RD involving macula.
Trauma: foreign body retrieval , dislocated lens,
vitreous hemorrhage, giant tears
Complicated RD: giant retinal tear, proliferative
vitreoretinopathy, large retinal breaks.
Endophthalmitis
Vitreous biopsy e.g. Amyloid.
Idiopathic macular hole.
Post test:
What is your diagnosis?
Answer: Vitreous
hemorrhage
10
LASER in Ophthalmology:
Laser is an acronym for Light Amplification by Stimulated Emission
of Radiation (L A S E R). Laser are used in the management of many
Ophthalmic conditions, particularly because so many ocular structures
can be easily visualized and because of precision of laser delivery.
Stringent safety regulations must be applied because of the risk of
laser damage to the eyes of patient, the operator and the bystander, so
it is recommended to wear safety goggles when entering the Laser
room.
The Physics of Laser:
Energy is applied to a potential light source, the applied energy
excites atoms raising their electrons to a higher energy level.
When an electron fall back to the lower energy level, it emits a
photon of light.
• In a Laser instrument, the process of excitation and photon
release is controlled and synchronized so that an extremely
bright light is emitted in which photons are of identical
wavelength, are in phase ( at the same stage of wave cycle at
any given point), and travel in parallel.
Laser- tissue interaction:
1- Photocoagulation:
conversion of Laser energy to heat ,with subsequent thermally
induced structural changes in the target,
e.g. Laser for diabetic retinopathy.
2- Photo disruption
High-peak-power pulsed laser to ionize the target and rupture the
surrounding tissues e.g. Nd:YAG Laser for peripheral iridotomy.
11
3- Photoablation:
A high powered ultraviolet laser pulses can precisely etch the cornea,
e.g. Excimer Laser (193 nm ) used in corneal refractive surgery.
In summary:
Laser light is coherent: all photons have
the same wavelength and in phase.
The Laser beam is also collimated i.e. the
waves of light are parallel and
monochromatic.
Clinical applications:
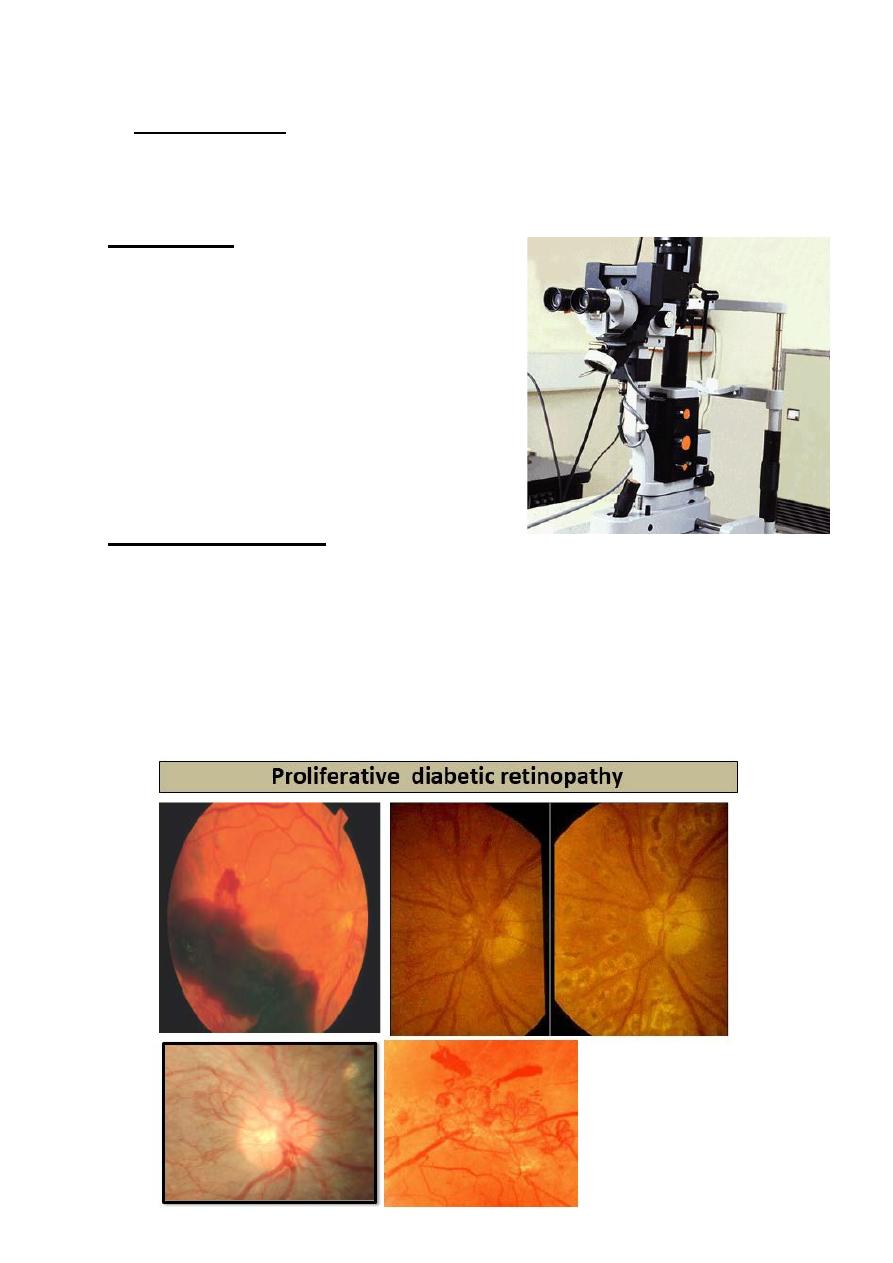
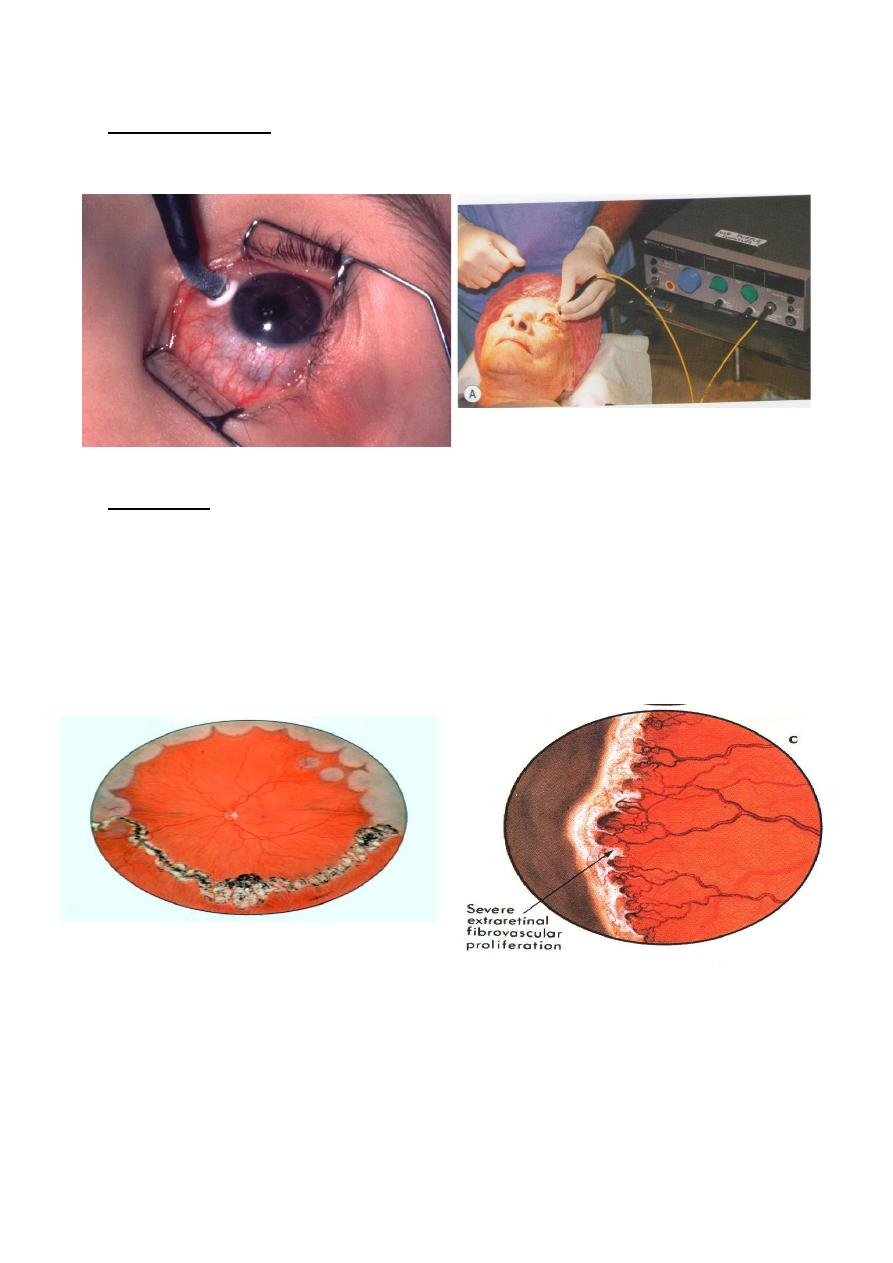
1- Diabetic Retinopathy
Laser treatment of proliferative diabetic retinopathy (PDR), and
macular edema has revolutionized the progress of these diseases.
In PDR: ischemic retina stimulates the growth of abnormal “New
Vessels” which can bleed and cause retinal detachment ( RD).
12
Laser for diabetic retinopathy
Sever
rubeosis iridis
13
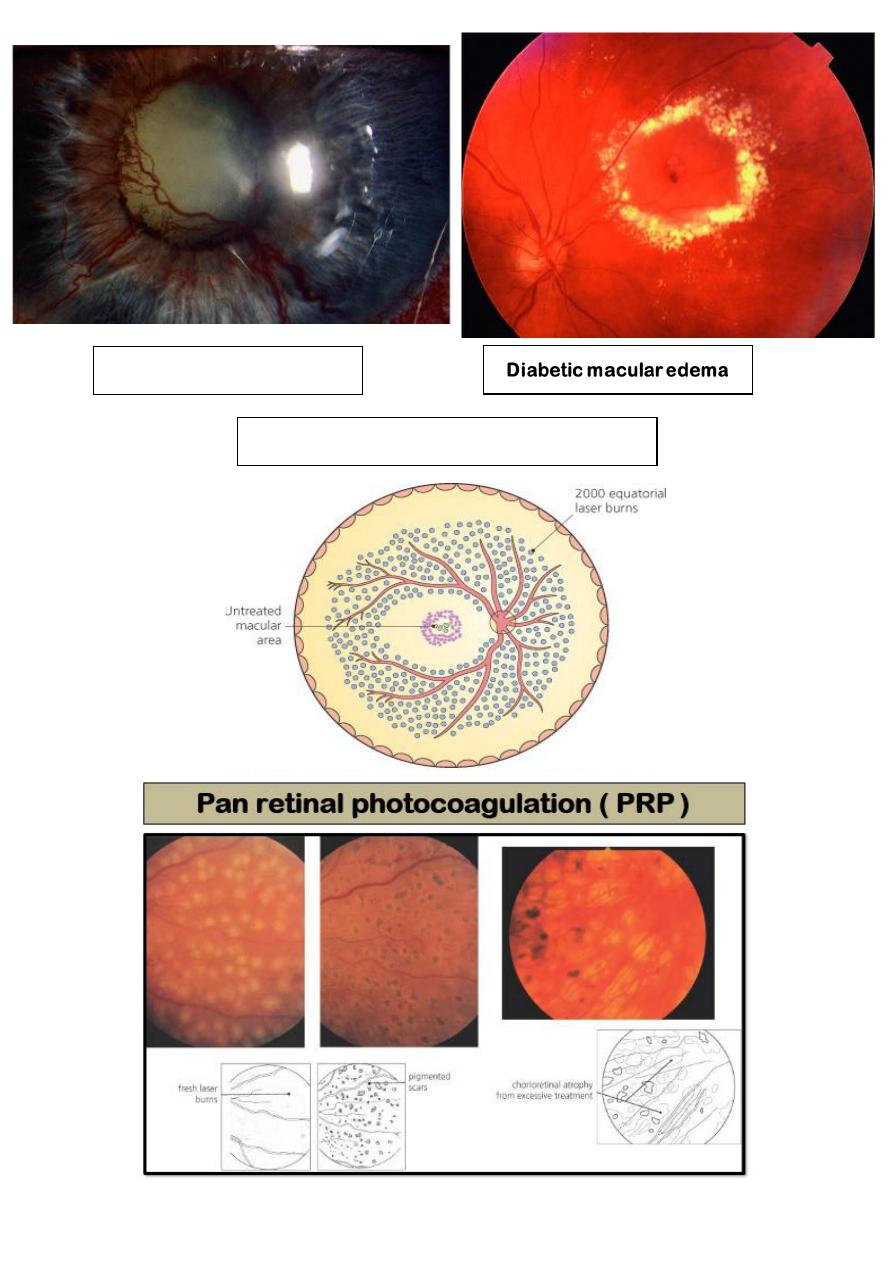
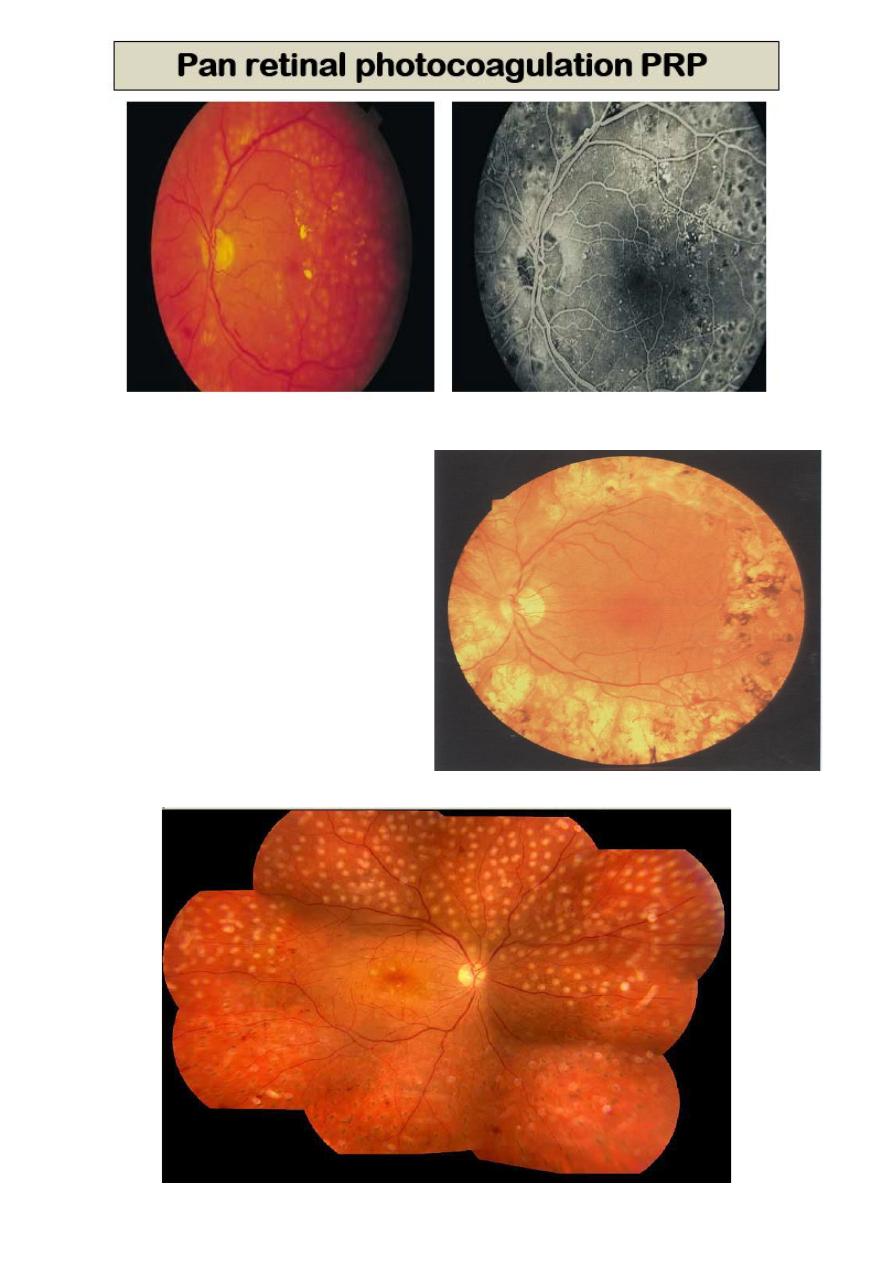
Argon or Diode Laser ablation
of ischemic areas pan retinal
photocoagulation (PRP), causes
regression of
neovascularization.
Certain types of Diabetic
macular edema respond to
gentle Argon laser treatment.
Same principle applied in cases
of Retinopathy of prematurity
(ROP).
14
Retinopathy of prematurity (ROP)
15
2- Glaucoma:
• Nd:YAG Laser peripheral iridotomy in angle closure glaucoma.
• Argon Laser trabeculoplasty in open angle glaucoma.
• Diode Laser as a cyclodestructive procedure in Rubeotic
glaucoma which occur in response to ischemic retina of PDR,
and retinal vein occlusion.
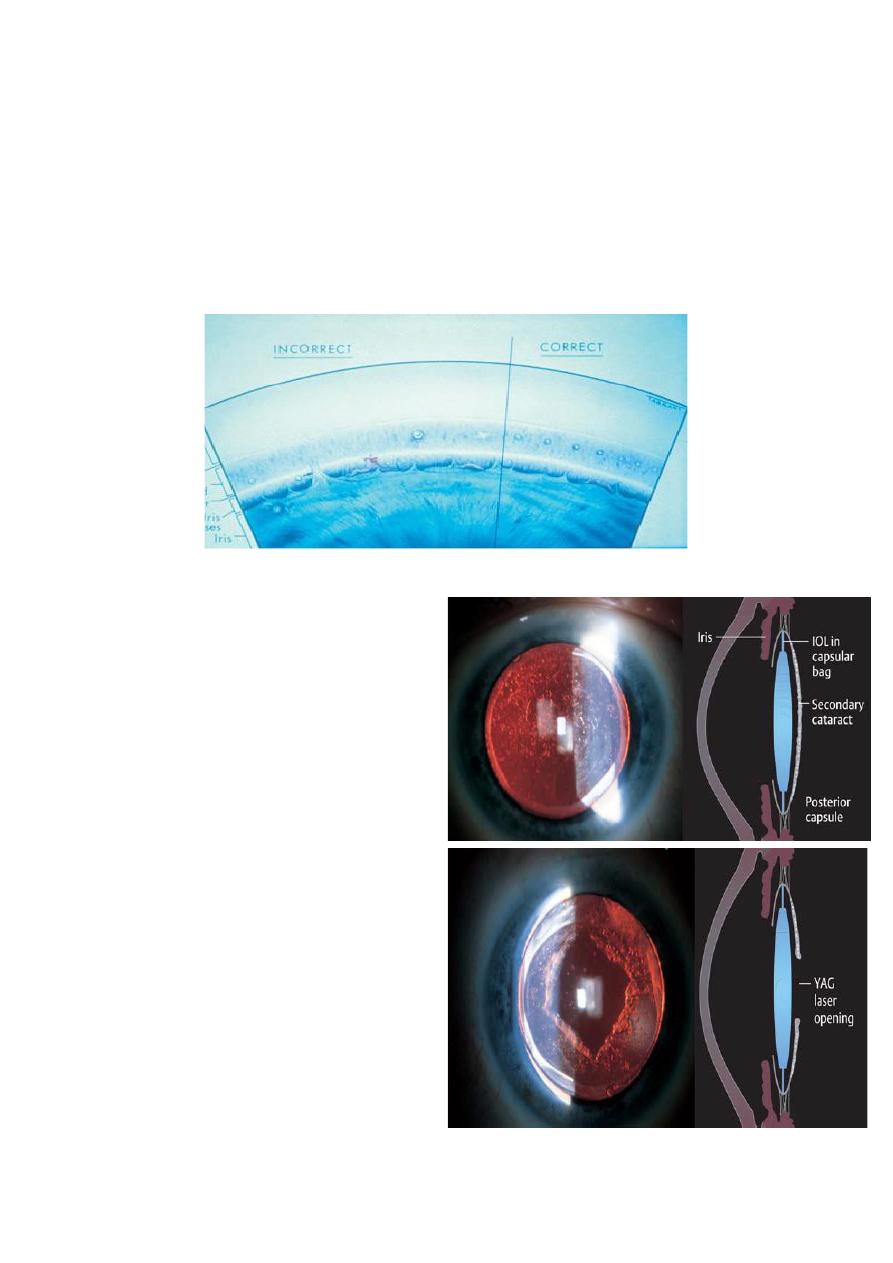
3- Posterior capsular opacification:
Posterior capsule thickening,
also known as “ After cataract
” is a common late
complication of cataract
extraction.
It occurs as a result of
proliferation and metaplasia of
residual lens fibers attached to
the capsule, symptoms include
poor vision and glare.
The Nd: YAG Laser is used to
create a central defect in the
posterior capsule. This does
not affect the position
or
integrity of the Intraocular
Lens Implant
(IOL).
16
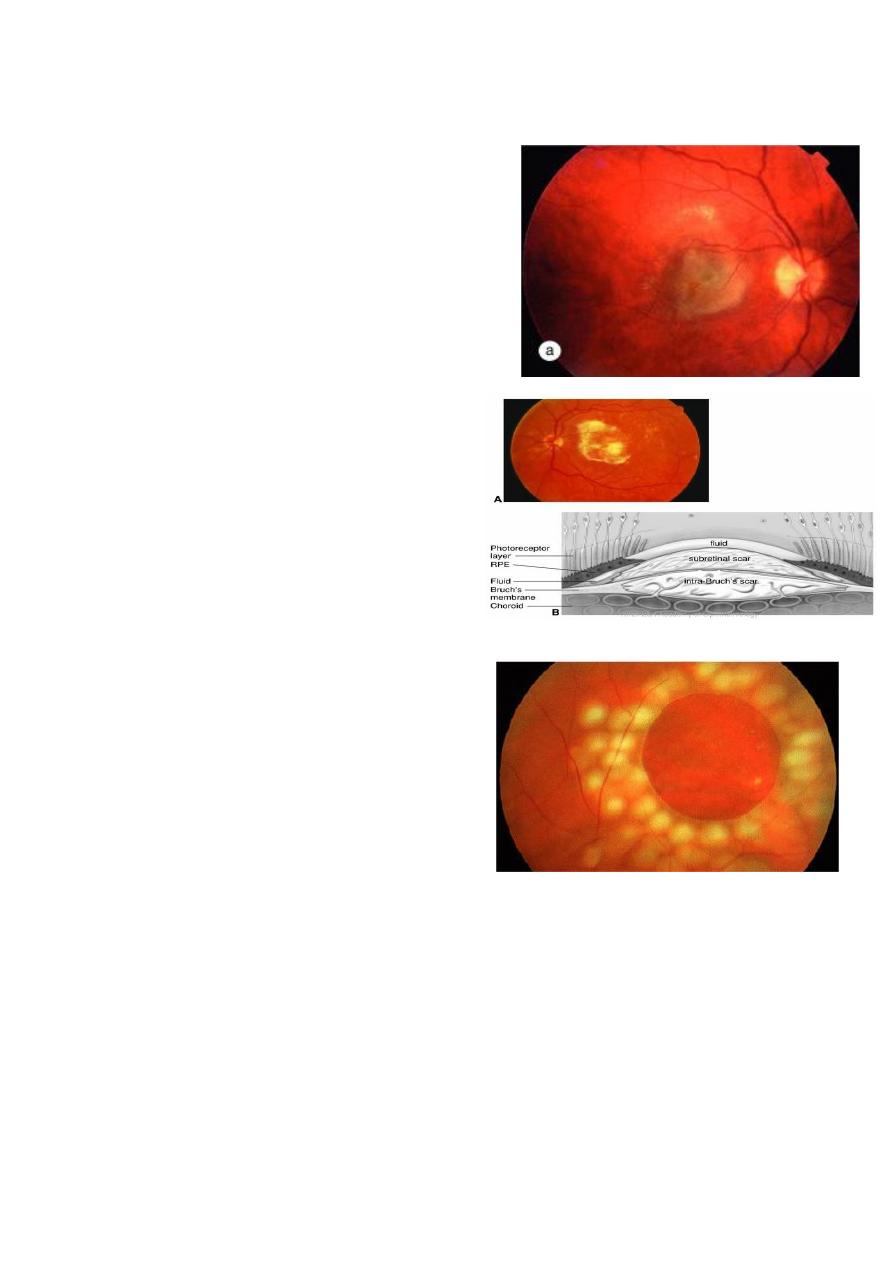
4- Age–related Macular Degeneration (AMD):
The growth of abnormal vascular
tissue from the choroid into the sub-
retinal spaces cause rapidly
progressive sight loss.
This tissue can be destroyed by Argon
Laser.
5- Retinal Detachment (RD):
A retinal tear or hole without RD
can be surround with laser to
induce Adhesion and prevent RD.
During RD Surgery, Laser is some
times used as an alternative to
cryotherapy to promote retinal
adhesion.
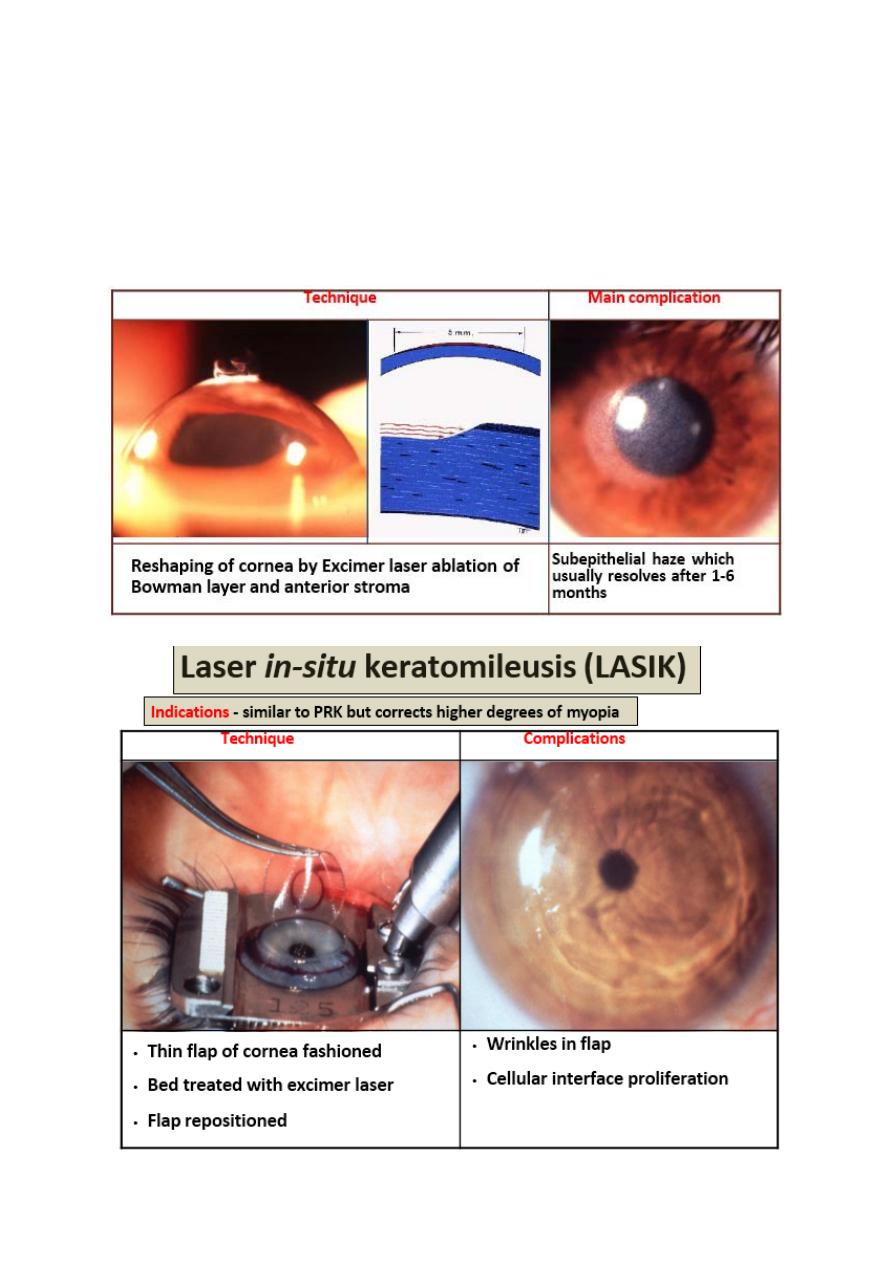
6- Refractive Errors
The Excimer Laser , applied with the computer assistance, very
precisely remove corneal tissue in the management of low-
moderate degree of myopia, hyperopia and astigmatism combined
with creation of hinged flap of cornea ( LASIK).
Larger Refractive Errors can now also successfully treated.
17
Photorefractive keratectomy (PRK):
Indications
• Stable myopia up to 6D with astigmatism no more than 3D
• Hypermetropia up to 2.5D

18
7- Miscellaneous uses:
A. ablation of intraocular and adnexal tumors.
B. division of intraocular post-inflammatory adhesions.
C. destruction of aberrant lashes.
D. removal of superficial corneal scars and calcific band
keratopathy (Excimer laser).
E. nasolacrimal duct obstruction by-pass.
Cryotherapy:
• Cryopexy means to produce tissue injury by application of
extremely low temperature ( -
40˚C to 100 ˚C).This is achieved
by a cryoprope from cryo-unit.
Working principle:
• Working of cryo-probe is based on the Joule Thompson
principle of cooling.
Gases used in cryo-machine:
• The cryo-unit uses Freon, nitrous
oxide or carbondiaxoide gas as a
cooling agent.
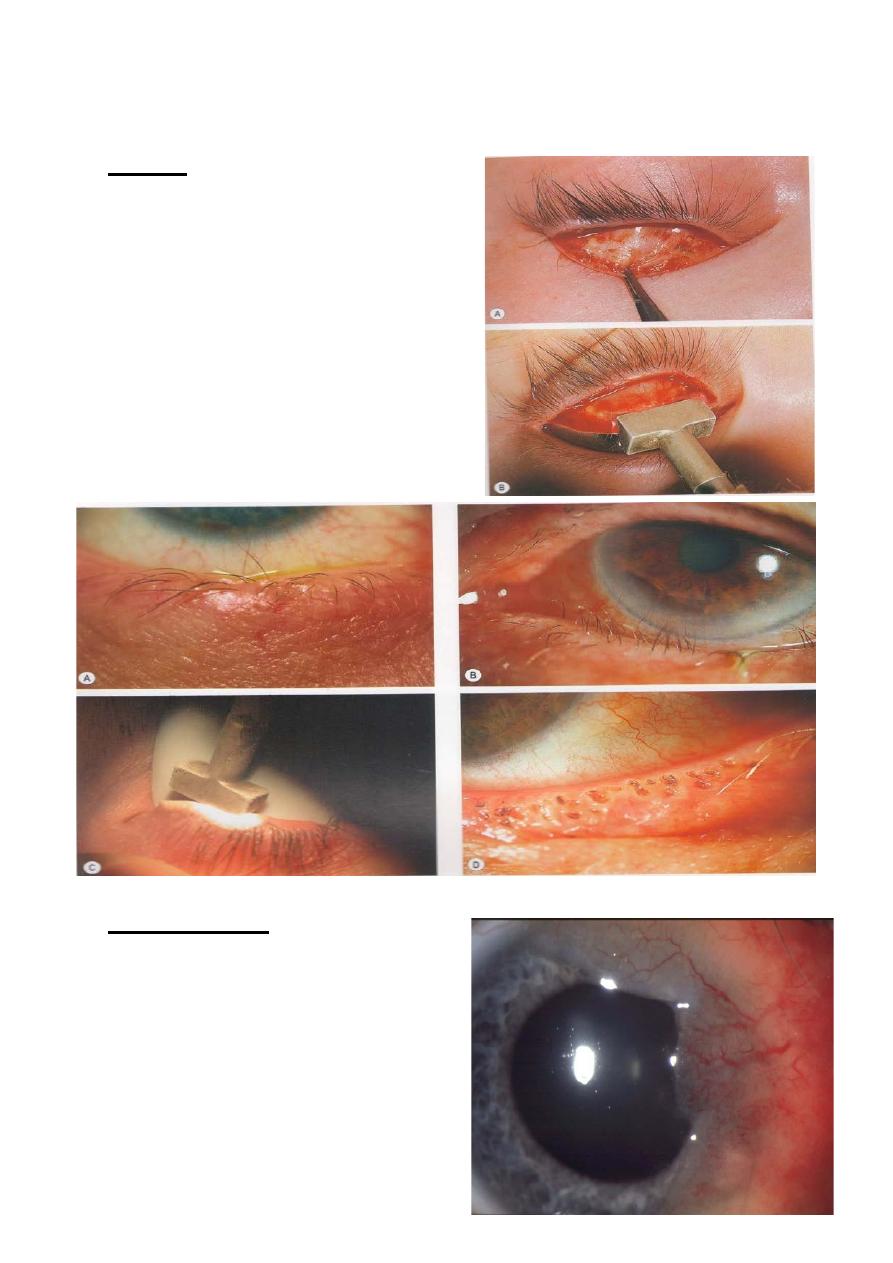
19
Clinical application of Cryotherapy in Ophthalmology:
1- Lids:
• (i) Cryolysis for Trichiasis.
• (ii) Cryotherapy for warts and
Molluscum contagiosum.
• (iii) cryotherapy for basal cell
carcinoma BCC and
haemangioma.
2- Conjunctiva:
• Cryotherapy for conjunctival
intraepithelial Neoplasia (CIN).
20
3- Ciliary body:
• Cyclodestruction of ciliary body for
neovascular glaucoma.
4- Retina:
• (i) Cryopexy for sealing retinal break to prevent propagation to
retinal detachment.
• (ii) Peripheral retinal application to ablate avascular retina in
ROP.
• (iii)Cryo-treatment of retinoblastoma.
