Cells are active participants in their environment, constantly adjusting their structure and function to accommodate changing demands and extracellular stresses. Cells tend to maintain their intracellular milieu within a fairly narrow range of physiologic parameters; that is, they maintain normal homeostasis
As cells encounter physiologic stresses or pathologic stimuli, they can undergo adaptation, achieving a new steady state and preserving viability and function. The principal adaptive
responses are hypertrophy, hyperplasia, atrophy, and metaplasia
If the adaptive capability is exceeded or if the external stress is inherently harmful, cell injury develops . Within certain limits injury is reversible, and cells return to a stable baseline; however, severe or persistent stress results in irreversible injury and death of the affected cells. Cell death is one of the most crucial events in the evolution of disease in any tissue or organ.
CELLULAR RESPONSES TO STRESS AND NOXIOUS STIMULI
CELLULAR ADAPTATIONS TO STRESS
Adaptations are reversible changes in the number, size, phenotype, metabolic activity, or functions of cells in response to changes in their environment.
There two types of Adaptations:-
1-physiologic adaptations usually represent responses of cells to normal stimulation by hormones or endogenous chemical mediators (e.g., the hormone-induced enlargement of the breast and uterus during pregnancy).
2- Pathologic adaptations are responses to stress that allow cells to modulate their structure and function and thus escape injury. Such adaptations can take several distinct forms
Hypertrophy is an increase in the size of cells resulting in increase in the size of the organ. In contrast, hyperplasia is characterized by an increase in cell number. In hypertrophy there are no new cells, just bigger cells, enlarged by an increased amount of structural proteins and organelles. Hyperplasia is an adaptive response in cells capable of replication, whereas hypertrophy occurs when cells are incapable of dividing.
Hypertrophy can be physiologic or pathologic
physiologic enlargement of the uterus during pregnancy occurs as a consequence of estrogen-stimulated smooth muscle hypertrophy and smooth muscle hyperplasiapathologic hypertrophy include the cardiac enlargement that occurs with hypertension or aortic valve disease.
Hyperplasia
an increase in cell number resulting in increase the size of organ .hyperplasia takes place if the cell population is capable of replication; it may occur with hypertrophy and often in response to the same stimuli.
Hyperplasia can be physiologic or pathologic
physiologic hyperplasia are :-
(1) hormonal hyperplasia, exemplified by the proliferation of the glandular epithelium of the female breast at puberty and during pregnancy.
(2) compensatory hyperplasia, that is, hyperplasia that occurs when a portion of the tissue is removed or diseased. For example, when a liver is partially resected
pathologic hyperplasia are caused by excessive hormonal or growth factor stimulation. For example, endometrial hyperplasia
Atrophy
Shrinkage(decrease ) in the size of the cell by the loss of cell substance is known as atrophy. Atrophy results from decreased protein synthesis and increased protein degradation in cells .When a sufficient number of cells is involved, the entire tissue or organ diminishes in size, becoming atrophic.
1- decreased workload (e.g., immobilization of a limb to permit healing of a fracture).
2- loss of innervations.
3- diminished blood supply.
4- inadequate nutrition.
5- loss of endocrine stimulation.
6- aging (senile atrophy).
types of atrophy
- physiologic atrophy (e.g., the loss of hormone stimulation in menopause decrease the size of uterus after parturition )
- pathologic atrophy (e.g., denervation, atrophy of brain in old man ).
Metaplasia
Metaplasia is a reversible change in which one adult cell type (epithelial or mesenchymal) is replaced by another adult cell type. In this type of cellular adaptation, cells sensitive to a particular stress are replaced by other cell types better able to withstand the adverse environment.
- Epithelial metaplasia is exemplified by The normal ciliated columnar epithelial cells of the trachea and bronchi are focally or widely replaced by stratified squamous epithelial cells in cigarette smokers.
- mesenchymal Metaplasia For example, bone is occasionally formed in soft tissues, particularly in foci of injury.
Dysplasia
referred to as typical hyperplasia means disorder in cellular development. occur only in epithelial tissues characterized by cellular proliferation and cytological changes.:
CELL INJURY
Cell injury defined as a variety of stresses which the cell encounters as a result of changes in its internal and external environment.The cellular response to stress may vary and depended on the following :- 1- type of cell or tissue.
2- type of cell injury and its extension.
CAUSES OF CELL INJURY
1- Oxygen DeprivationA-Hypoxia, or oxygen deficiency
B- ischemia
C-reduction in the oxygen-carrying capacity of the blood, as in blood loss anemia or carbon monoxide (CO) poisoning.
2- Chemical Agents
glucose or salt ,air pollutants, insecticides, CO, asbestos, and social "stimuli" such as ethanol. Even therapeutic drugs
3 Infectious Agents
These range from submicroscopic viruses to meter-long tapeworms; in between are the rickettsiae, bacteria, fungi, and protozoa. The diverse ways by which infectious pathogens cause injury
4- Immunologic Reactions
Although the immune system defends the body against pathogenic microbes, immune reactions can also result in cell and tissue injury. Examples include autoimmune reactions against one's own tissues and allergic reactions against environmental substances in genetically susceptible individuals .5- Genetic defects
Genetic defects can result in pathologic changes as conspicuous as the congenital malformations associated with Down syndrome or as subtle as the single amino acid substitution in hemoglobin S giving rise to sickle cell anemia. Genetic defects may cause cell injury because of deficiency of functional proteins, such as enzymes, or accumulation of damaged DNA or misfolded proteins, both of which trigger cell death when they are beyond repair. Variations in the genetic makeup can also influence the susceptibility of cells to injury by chemicals and other environmental insults.6-Nutritional Imbalances
Nutritional deficiencies remain a major cause of cell injury. Protein-calorie insufficiency among underprivileged populations is only the most obvious example; specific vitamin deficiencies are not uncommon even in developed countries with high standards of living. excesses of nutrition are also important causes of morbidity and mortality; for example, obesity markedly increases the risk for type 2 diabetes mellitus. Moreover, diets rich in animal fat are strongly implicated in the development of atherosclerosis as well as in increased vulnerability to many disorders, including cancer.7- Physical Agents
Trauma, extremes of temperatures, radiation, electric shock, and sudden changes in atmospheric pressure all have wide-ranging effects on cells.8- Aging
Cellular senescence leads to alterations in replicative and repair abilities of individual cells and tissues.
Robbins Basic Pathology . Page 1
MECHANISM OF CELL INJURYCell injury results from functional and biochemical abnormalities in one or more of several essential cellular components. The most important targets of injurious stimuli are (1) mitochondria, the sites of ATP generation; (2) cell membranes, on which the ionic and osmotic homeostasis of the cell and its organelles depends; (3) protein synthesis; (4) the cytoskeleton; and (5) the genetic apparatus of the cell.
1- ATP Depletion
ATP, the energy store of cells, is produced mainly by oxidative phosphorylation of adenosine diphosphate (ADP) during reduction of oxygen in the electron transport system of mitochondria. In addition, the glycolytic pathway can generate ATP in the absence of oxygen using glucose derived either from the circulation or from the hydrolysis of intracellular glycogen. The major causes of ATP depletion are reduced supply of oxygen and nutrients, mitochondrial damage, and the actions of some toxins (e.g., cyanide).
2- Damage to Mitochondria
Mitochondria are the cell's suppliers of life-sustaining energy in the form of ATP, but they are also critical players in cell injury and death. Mitochondria can be damaged by increases of cytosolic Ca2, and oxygen deprivation, and so they are sensitive to virtually all types of injurious stimuli, including hypoxia and toxins.3- Influx of Calcium
Cytosolic free calcium is normally maintained by ATP-dependent calcium transporters at concentrations that are as much as 10,000 times lower than the concentration of extracellular calcium or of sequestered intracellular mitochondrial and ER calciumIschemia and certain toxins cause an increase in cytosolic calcium concentration, initially because of release of Ca2+ from the intracellular stores, and later resulting from increased influx across the plasma membrane. Increased cytosolic Ca2+ activates a number of enzymes, with potentially deleterious cellular effects. These enzymes include phospholipases (which cause membrane damage), proteases (which break down both membrane and cytoskeletal proteins), endonucleases (which are responsible for DNA), and adenosine triphosphatases (ATPases; thereby hastening ATP depletion).
4- Accumulation of Oxygen-Derived Free Radicals
Free radicals are chemical species with a single unpaired electron in an outer orbital. Such chemical states are extremely unstable and readily react with inorganic and organic chemicals; when generated in cells they avidly attack nucleic acids as well as a variety of cellular proteins and lipids.5- Defects in Membrane Permeability
The most important sites of membrane damage during cell injury are the mitochondrial membrane, the plasma membrane, and membranes of lysosomes.loss of selective membrane permeability leading ultimately to overt membrane damage is a consistent feature of most forms of cell injury. The plasma membrane can be damaged by ischemia, various microbial toxins, lytic complement components, and a variety of physical and chemical agents.
6-Damage to DNA and Proteins
Cells have mechanisms that repair damage to DNA, but if this damage is too severe to be corrected (e.g., after radiation injury or oxidative stress), the cell initiates its suicide program and dies by apoptosis.REVERSIBLE CELL INJURY
Intracellular edema
Fatty change
Hyaline change
Ayloidosis
Mucoid degeneration
Pathologic pigments
Intracellular edema (Cellular swelling)
Also known as cloudy swelling or hydropic degeneration its accumulation of watery fluid in cell due to impaired regulation of sodium and potassium at the level of cell membrane . Its commonest and earliest form of cell injury.Etiology (causes )
Bacterial toxins
Chemical
Poisons
Burns
High fever
Gross Appearance
swollen with rounded edges ;increases the volume and weight of organs; and imparts pallor to them. It is important to distinguish hydropic degeneration from more positive adaptations, such as hypertrophy or hyperplasia.Microscopic Appearance
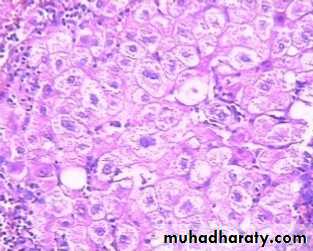
The influx of water in hydropic degeneration dilutes the cytosol, separates its organelles, and distends the cell, giving the affected cells a swollen, pale, and finely vacuolated appearance. The clear cytoplasmic vacuoles in affected cells are mainly water-distended mitochondria or Golgi complex or ER .
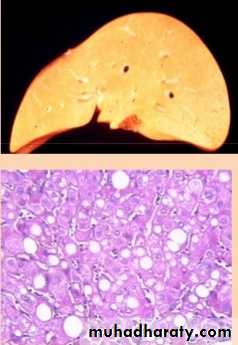
Fatty change ( steatosis)
Fatty change refers to any abnormal accumulation of triglycerides within parenchymal cells. It is most often seen in the liver, since this is the major organ involved in fat metabolism, but it may also occur in heart, skeletal muscle, kidney, and other organs .Causes
1-toxins,
2- protein malnutrition,
3-diabetes mellitus,
4-obesity,.
4- Alcohol abuse
5- diabetes associated with obesity