Irreversible cell injury1- Necrosis2- Apoptosis3-Gangreen4-Pathological calcification
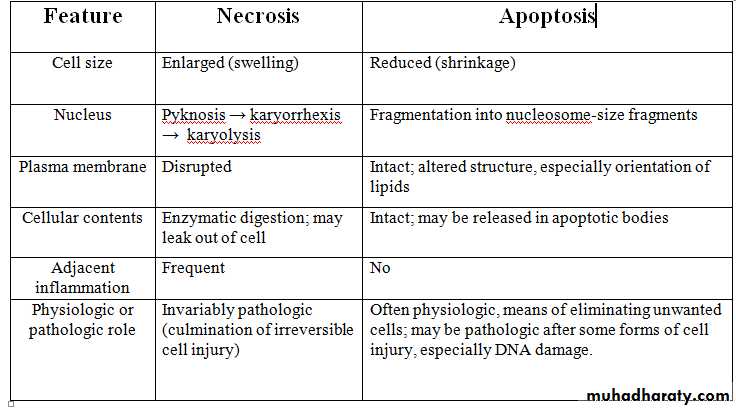
1Necrosis refer to a series of changes that accompany cell death, resulting from the degradative action of enzymes liberated from death cells. Necrotic cells are unable to maintain membrane integrity, and their contents often leak out. The enzymes responsible for digestion of the cell are derived either from the lysosomes of the dying cells themselves or from the lysosomes of leukocytes that are recruited as part of the inflammatory reaction to the dead cells.
2
Causes1-Poisons A- Chemical poisons such as insecticides ,fungicides.B- Bacterial toxins. C- Plant poisons. D-Eterotoxins.2- loss of blood supply.3- physical agents as trauma ,burn ,radiation, UV.4- Immunologic reaction as AG -AB reactions
3
Morphology1-The necrotic cells show increased eosinophilia (i.e., pink staining from the eosin dye, the "E" in "H&E"). This is attributable in part to increased binding of eosin to denatured cytoplasmic proteins and in part to loss of the basophilia that is normally imparted by the ribonucleic acid (RNA) in the cytoplasm (basophilia is the blue staining from the hematoxylin dye, the "H" in "H&E").2- The cell may have a more glassy homogeneous appearance than viable cells, mostly because of the loss of glycogen particles.3- When enzymes have digested the cytoplasmic organelles, the cytoplasm becomes vacuolated and appears motheaten.
4
4- Dead cells may be replaced by large ,whorled phospholipid masses which then either phagocytosed by other cells or further degraded into fatty acids which will be calcified resulting in the appearance of calcified dead cells.
5
Nuclear changes occur due to breakdown of DNA and chromatin which include :-A- pyknosis, characterized by nuclear shrinkage and increased basophilia; the DNA condenses into a solid shrunken mass.B- karyorrhexis, the pyknotic nucleus undergoes fragmentation. And then completely disappears. C- karyolysis- The basophilia of the chromatin may fade, presumably secondary to deoxyribonuclease (DNase) activity.
6
Patterns of Tissue Necrosis1- Coagulative necrosis is a form of tissue necrosis in which the component cells are dead but the basic tissue architecture is preserved for at least several days. The affected tissues take on a firm texture .
7
the injury denatures not only structural proteins but also enzymes and so blocks the proteolysis of the dead cells; as a result, eosinophilic, anucleate cells may persist for days or weeks. the necrotic cells are removed by phagocytosis of the cellular debris by infiltrating leukocytes and by digestion of the dead cells by the action of lysosomal enzymes of the leukocytes. Coagulative necrosis is characteristic of infarcts (areas of ischemic necrosis) in all solid organs except the brain.
8
Coagulative necrosis. Show kidney infarct (yellow)
9
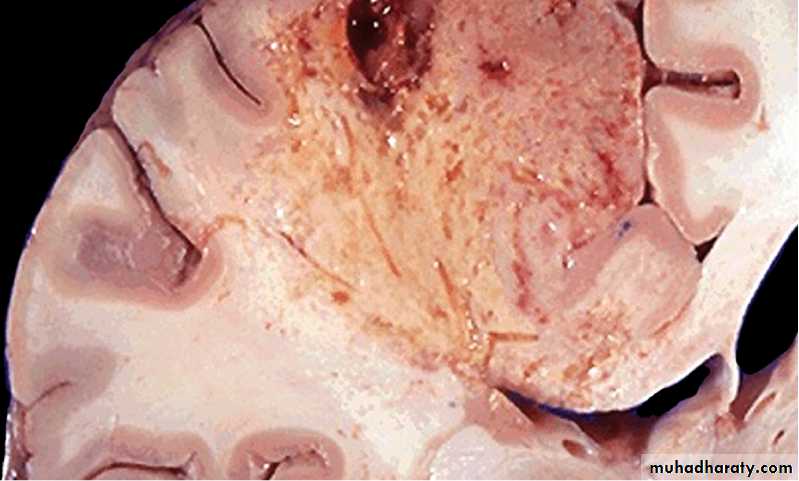
2- Liquefactive necrosis is seen in focal bacterial or, occasionally, fungal infections, because microbes stimulate the accumulation of inflammatory cells and the enzymes of leukocytes digest ("liquefy") the tissue. For obscure reasons, hypoxic death of cells within the central nervous system evokes liquefactive necrosis . liquefaction completely digests the dead cells, resulting in transformation of the tissue into a liquid viscous mass. If the process was initiated by acute inflammation, the material is frequently creamy yellow and is called pus.
10
Liquefactive necrosis of the brain,
11
3- gangrenous necrosis is not a distinctive pattern of cell death, the term is still commonly used in clinical practice. It is usually applied to a limb, generally the lower leg, that has lost its blood supply and has undergone coagulative necrosis involving multiple tissue layers. When bacterial infection is superimposed, coagulative necrosis is modified by the liquefactive action of the bacteria and the attracted leukocytes (so-called wet gangrene).
12
4- Caseous necrosis is encountered most often in foci of tuberculous infection. The term "caseous" (cheese-like) is derived from the friable yellow-white appearance of the area of necrosis . On microscopic examination, the necrotic focus appears as a collection of fragmented or lysed cells with an amorphous granular appearance. Unlike coagulative necrosis, the tissue architecture is completely obliterated and cellular outlines cannot be discerned. Caseous necrosis is often enclosed within a distinctive inflammatory border; this appearance is characteristic of a focus of inflammation known as a granuloma.
13
Caseous necrosis. A tuberculous lung with a large area of caseous necrosis containing yellow-white and cheesy debris.
14
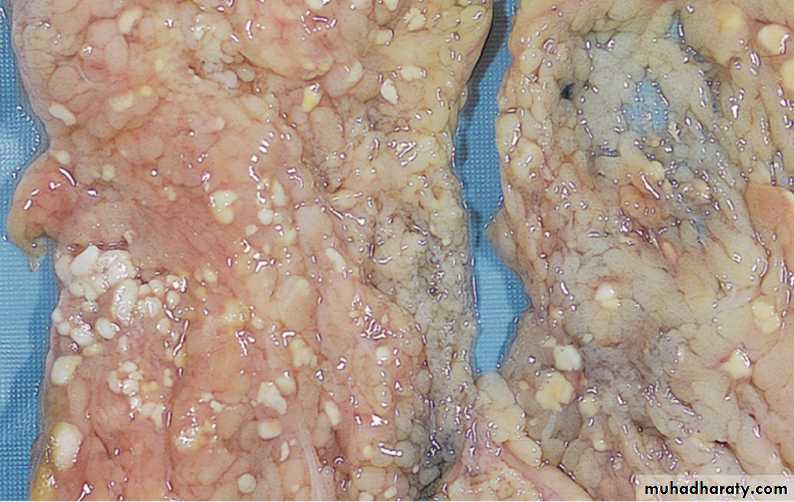
5- Fat necrosis, refers to focal areas of fat destruction, resulting from release of activated pancreatic lipases into the substance of the pancreas and the peritoneal cavity. This occurs in acute pancreatitis. In this disorder, pancreatic enzymes that have leaked out of acinar cells and ducts liquefy the membranes of fat cells in the peritoneum, and lipases split the triglyceride esters contained within fat cells. The released fatty acids combine with calcium to produce grossly visible chalky white areas (fat saponification), which enable the surgeon and the pathologist to identify the lesions . On histologic examination, the foci of necrosis contain shadowy outlines of necrotic fat cells with basophilic calcium deposits, surrounded by an inflammatory reaction.
15
The areas of white chalky deposits represent foci of fat necrosis with calcium soap formation (saponification) in the mesentery.
16
6- Fibrinoid necrosis is a special form of necrosis usually seen in immune reactions involving blood vessels. This pattern of necrosis is prominent when complexes of antigens and antibodies are deposited in the walls of arteries. Deposits of these "immune complexes," together with fibrin that has leaked out of vessels, result in a bright pink and amorphous appearance in H&E stains, called "fibrinoid" (fibrin-like).
17
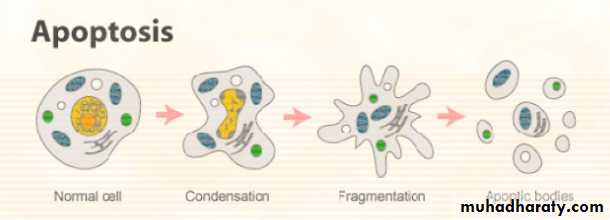
2- Apoptosis (Programmed cell death )
Apoptosis is a pathway of cell death that is induced by a tightly regulated suicide program in which cells destined to die activate enzymes capable of degrading the cells' own nuclear DNA and nuclear and cytoplasmic proteins. Fragments of the apoptotic cells then break off, giving the appearance that is responsible for the name (apoptosis, "falling off").The plasma membrane of the apoptotic cell remains intact, but the membrane is altered in such a way that the cell and its fragments become avid targets for phagocytes. The dead cell is rapidly cleared before its contents have leaked out, and therefore cell death by this pathway does not elicit an inflammatory reaction in the host. Thus, apoptosis differs from necrosis, which is characterized by loss of membrane integrity, enzymatic digestion of cells, leakage of cellular contents, and frequently a host reaction.18
19
CAUSE OF APOPTOSIS
Apoptosis occurs normally in many situations, and serves to eliminate potentially harmful cells and cells that have outlived their usefulness. It is also a pathologic event when cells are damaged beyond repair, especially when the damage affects the cell's DNA or proteins; in these situations, the irreparably damaged cell is eliminated.20
1- Apoptosis in Physiologic Situations
1-The programmed destruction of cells during embryogenesis, including implantation, organogenesis, developmental involution, and metamorphosis.2-Involution of hormone-dependent tissues upon hormone deprivation, such as endometrial cell breakdown during the menstrual cycle, and regression of the lactating breast after weaning.
3-Cell loss in proliferating cell populations, such as intestinal crypt epithelia, so as to maintain a constant number.
4-Death of cells that have served their useful purpose, such as neutrophils in an acute inflammatory response, and lymphocytes at the end of an immune response.
5-Elimination of potentially harmful self-reactive lymphocytes, either before or after they have completed their maturation, in order to prevent reactions against one's own tissues.
6-Cell death induced by cytotoxic T lymphocytes, a defense mechanism against viruses and tumors that serves to kill and eliminate virus-infected and neoplastic cells.
21
2-Apoptosis in Pathologic Conditions
Apoptosis eliminates cells that are genetically altered or injured beyond repair without eliciting a severe host reaction, thus keeping the damage as contained as possible. Death by apoptosis is responsible for loss of cells in a variety of pathologic states:1-DNA damage. Radiation, cytotoxic anticancer drugs, extremes of temperature, and even hypoxia can damage DNA, either directly or via production of free radicals. If repair mechanisms cannot cope with the injury, the cell triggers intrinsic mechanisms that induce apoptosis.
2-Accumulation of misfolded proteins lead to apoptotic cell death .
3-Cell injury in certain infections, particularly viral infections, in which loss of infected cells is largely due to apoptotic death that may be induced by the virus.
4-Pathologic atrophy in parenchymal organs after duct obstruction, such as occurs in the pancreas, parotid gland, and kidney.
22
Mechanisms of Apoptosis
Apoptosis is an active enzymatic process in which nucleoproteins are broken down and then the cell is fragmented.
Morphology of apoptosis
In H&E-stained tissue sections, apoptotic cells may appear as round or oval masses with intensely eosinophilic cytoplasm . Nuclei show various stages of chromatin condensation and aggregation and, ultimately, karyorrhexis.23
24
25
3-Gangrene
Is a form of tissue necrosis with superadded putrefaction characterized by liquefaction due to action of putrefactive bacteria. It may be caused either by ischemia asA- Gangrene of bowel
B-Gangrene of limb
Or by inflammation which provoked by virulent bacteria resulting in massive tissue necrosis as
A-gangrenous appendicitis
B-gangrenous stomatitis
26
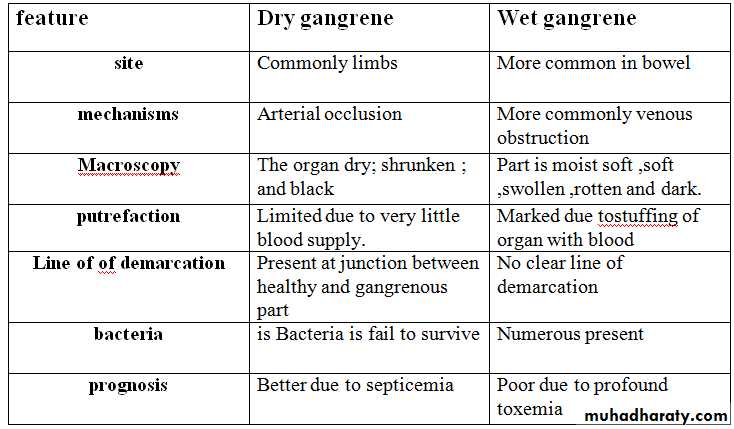
Types of gangrene
1-Dry gangrene2-Wet gangrene
A-Gas gangrene
1-Dry gangrene
This type of gangrene is begins in the distal part of the limbs and spreads slowly upwards until it reaches a point where the blood supply is adequate to keep the tissue viable
A line of separation is formed at the point between gangrenous part and viable part.
27
28
Morphology
-GrosslyThe affected part is dry ;shrunken; and dark black . its black color due to liberation of hemoglobin from haemolysed red blood cells which combined hydrogen disulfide produced by bacteria result in formation of black iron sulfide.
Microscopic
-The necrosis with smudging of the tissue.
- the line of separation consist of inflammatory granulation tissue.
29
2-Wet gangrene
Occur in naturally wet tissues such as mouth ;bowel; cervix; and vulva. Its develop rapidly due to blockage of venous and less commonly arterial blood flow by thrombosis and embolism. The affective part is stuffed with blood which favours the rapid growth of putrefactive bacteria. The toxic products formed by bacteria are absorbed causing profound systemic manifestation of septicemia and finally death.30
Morphology
-Grossly-the affected part is soft ;swollen ;putrid;rotten; and dark such as gangrene of bowel due to strangulated hernia , volvulus , and intussuscepion. The part is dark due to the same mechanism in dry gangrene.
31
32
Microscopically
-coagulative necrosis with stuffing of affected part with blood.- there is ulceration of the mucosa and inflammatory infiltration.
- the lumen of bowel contains mucus and blood.
-the line between gangrenous segment and viable bowel is generally not clear-cut.
33
34
Gas gangrene
Is special form of wet gangrene caused by gas forming gram positive anaeropic bacteria such as clostridia which enter in to the tissue through open contaminated wounds as in muscles or complication after operation on colon.Morphology
-Grossly
-The affected area is swollen ,edematous, painful ,and crepitant due to accumulation of gas bubbles within the tissue.
- subsequently, the affected tissue becomes dark black and foul smelling.
Microscopic
-muscle fibers undergo coagulative necrosis and liquefaction.
- large number of gram positive bacilli can be identified .
-a zone of leucocytes infiltration ,edema ,congestion are found.
35
36