I
Fifth stage
ENT
Lec-3
د.سعد
5/10/2015
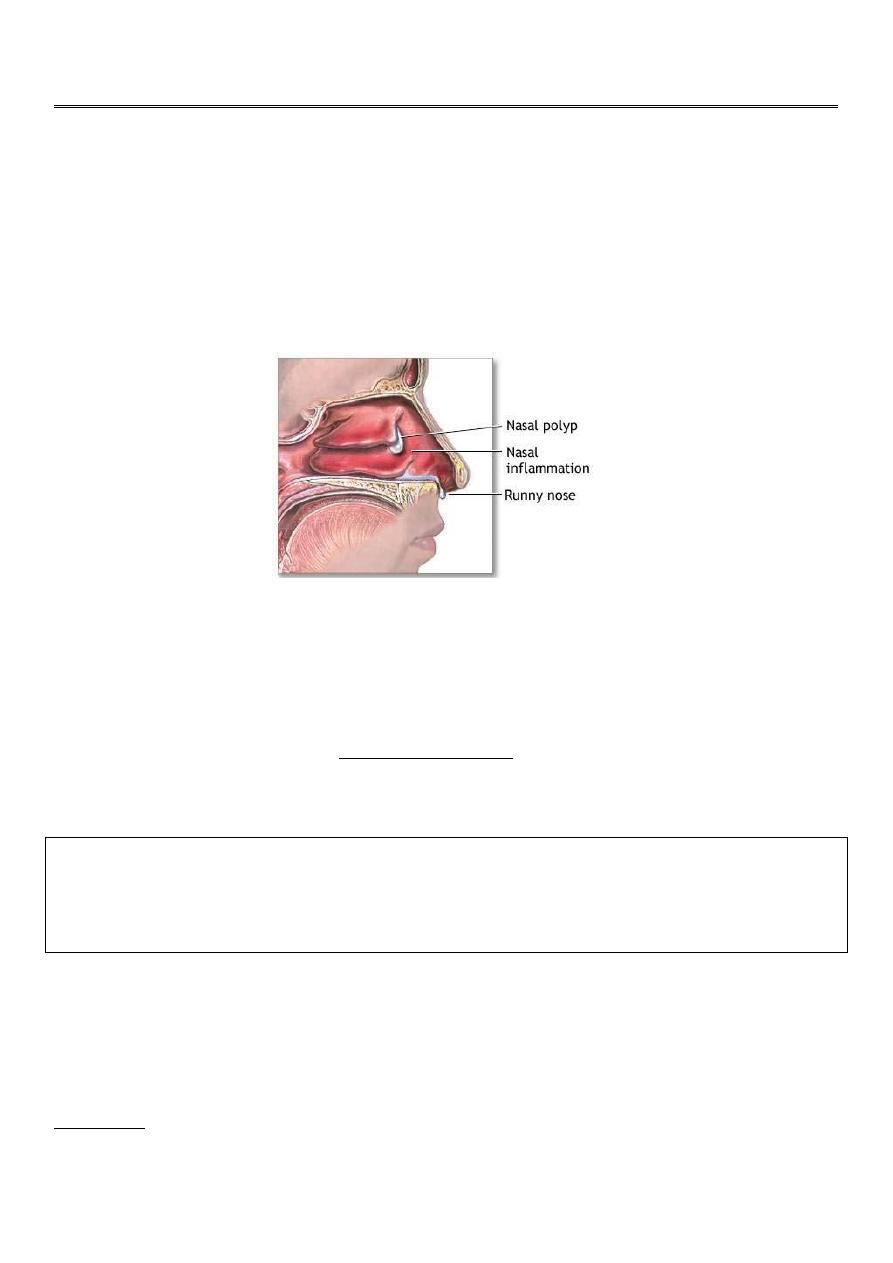
NASAL POLYPS
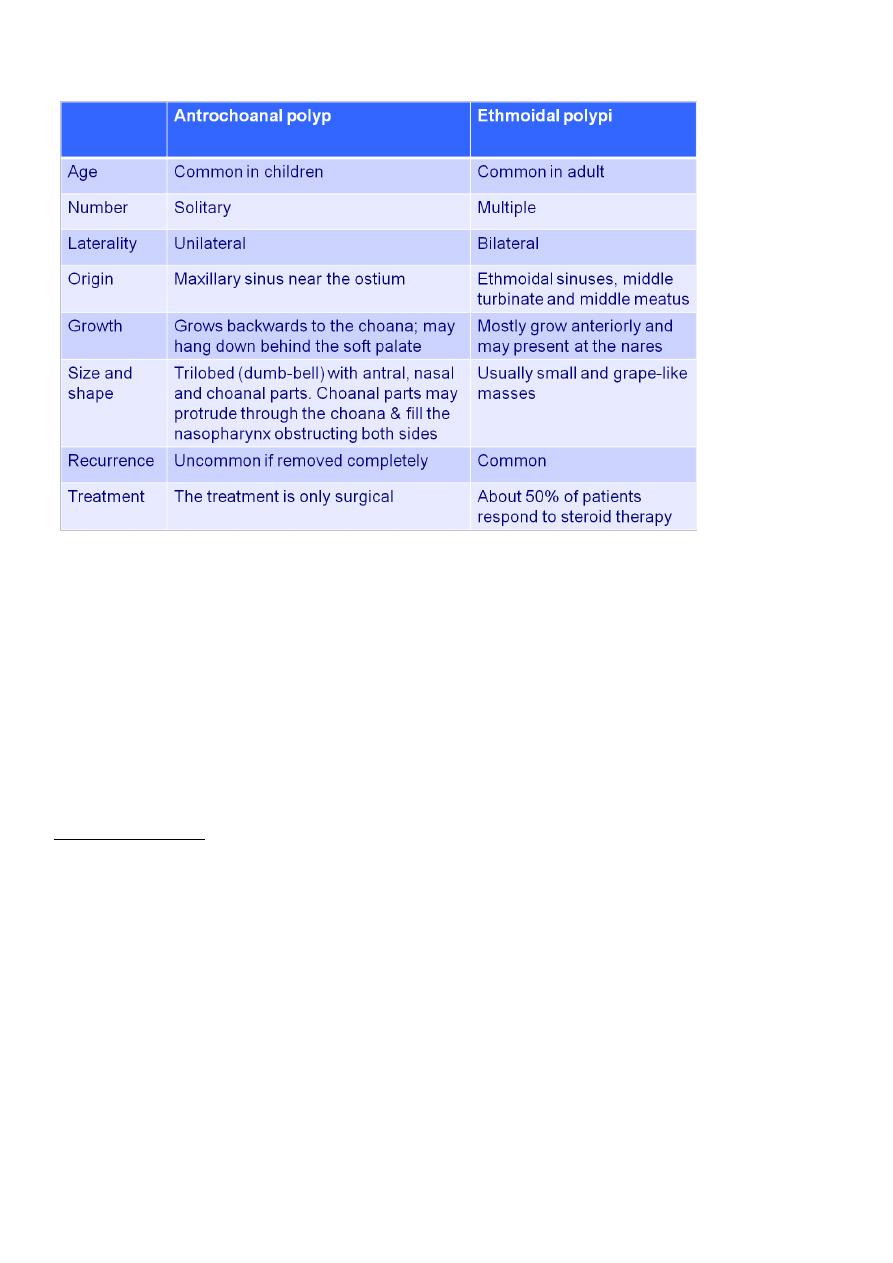
Nasal polyps are usually classified into antrochoanal polyps and ethmoidal polyps.
Antrochoanal polyps arise from the maxillary sinuses and are much less common, ethmoidal
polyps arise from the ethmoidal sinuses. Antrochoanal polyps are usually single and
unilateral whereas ethmoidal polyps are multiple and bilateral.
Ethmoidal polyps
Are benign grayish, soft, translucent, multiple masses of pedunculated tissue most often
originate from the mucus membrane of the ethmoidal sinuses and project into the nasal
cavity, resembling a bunch of peeled grapes. They are usually bilateral.
The aetiology of nasal polyps is poorly understood. There is no single predisposing factor,
but classically they are caused by allergy and infection. It may also be associated with aspirin
sensitivity and asthma, cystic fibrosis and Kartagener syndrome.
It is thought that repeated insult to the mucous lining of the ethmoid sinus cause increased blood vessel permeability
which in turn causes oedema of the mucosa. Eventually this mucosa prolapses out of the sinus. Repeated blowing of
the nose decreases the pressure in the nasal cavity which pulls down the polyp and encourages its growth (Bernoulli's
phenomena). The increasing size of the polyp predisposes to infection and the vicious cycle encourages more growth
.
DIAGNOSIS:
It is a disease of adult (but may occur in children with cystic fibrosis). Male affected more
than female.
Symptoms: Nasal obstruction, anosmia, colourless or purulent rhinorrhoea, copious post
nasal drip, snoring, and headache due to chronic sinusitis that result from occlusion of sinus
ostia.
II
Signs: Hyponasal voice, mouth breathing, flaring of alar cartilage, `frog face` i.e. widening of
the nasal bones if polyps develop in children before facial bone fuse.
Anterior rhinoscopy; the polyps appear as translucent, smooth-walled, grayish mass,
sometimes protrude out of the nostrils. The polyps are non-tender and moves backwards
when probed. These features clinically separate them from turbinates. They tend to be
bilateral and multiple. If unilateral, one should exclude antrochoanal polyp, neoplasia and
meningocoeles.
Investigations: The usual investigations are radiography of the sinuses and allergy skin tests.
Treatment:
1) Medical treatment: About 50% of patients respond to steroid therapy (local or
systemic). If no response after one month of treatment, then surgical treatment is
recommended.
2) Surgical treatment:
Simple polypectomy.
Internal ethmoidectomy under endoscopic control.
External ethmoidectomy.
Postoperative therapy; Recurrence of polyps is common, therefore local or systemic
steroids are prescribed to prevent symptoms of rhinitis and prevent recurrence.
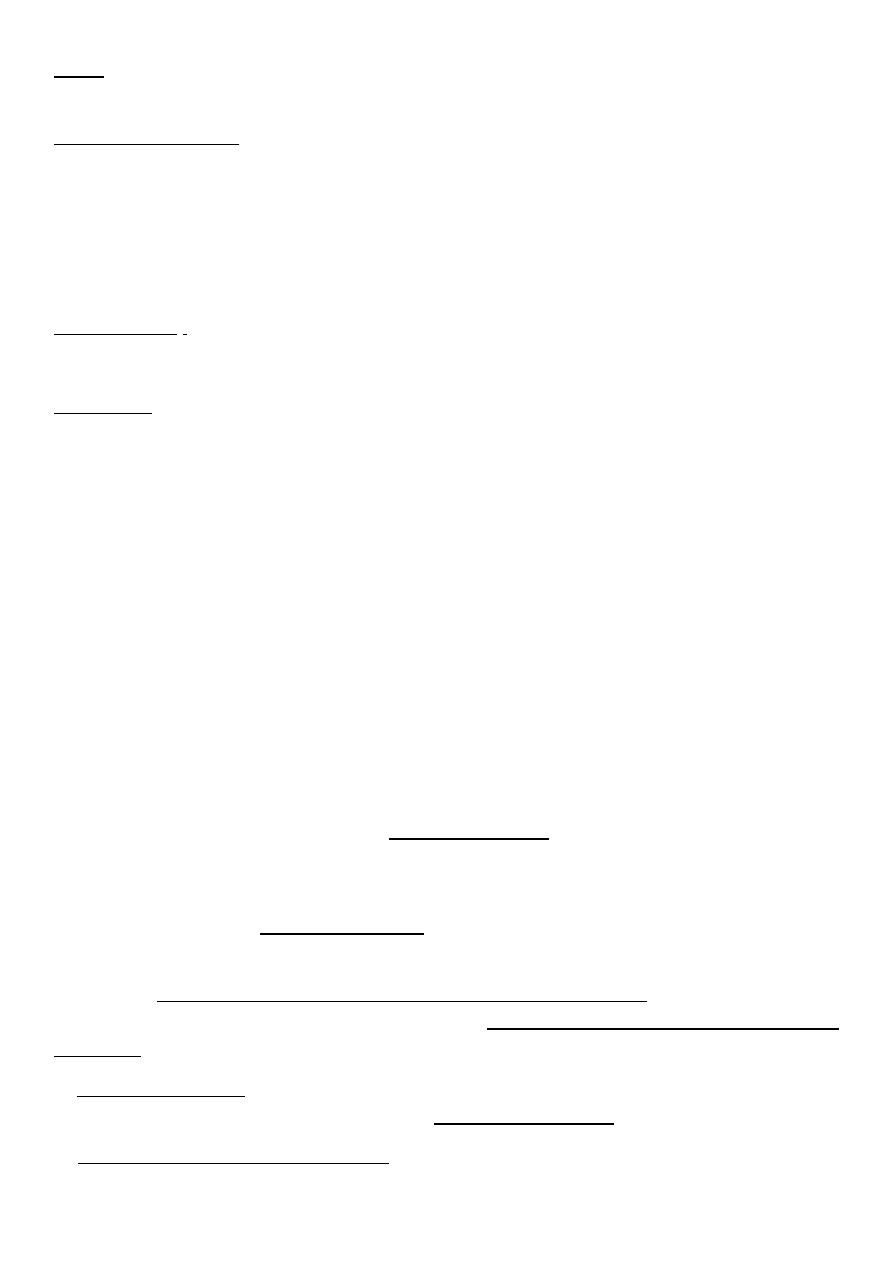
Antrochoanal polyps
These polyps arise from the lining of the maxillary sinus and prolapse through the ostium
in the middle meatus and extend backwards through the posterior choana to the
nasopharynx. The choanal part of the polyp may be seen in the oropharynx.
The polyp tend to be dumb-bell in shape with a constriction where they pass through the
ostium of the sinus.
They are often unilateral but may cause bilateral nasal obstruction by expanding into the
entire nasopharynx. The classical presentation is a good inspiratory airway with blockage on
expiration. This is the result of ball-valve effect of the polyp blocking the posterior choana.
Anterior rhinoscopy may look normal as only a thin stalk may be present in the nose. The
enlarged posterior end may only be seen on posterior rhinoscopy.
They are not associated with allergy and histologically the cellular infiltrate has no
eosinophilia.
III
The aetiology is unknown.
Radiography of the maxillary sinus will show complete opacification of the affected
antrum.
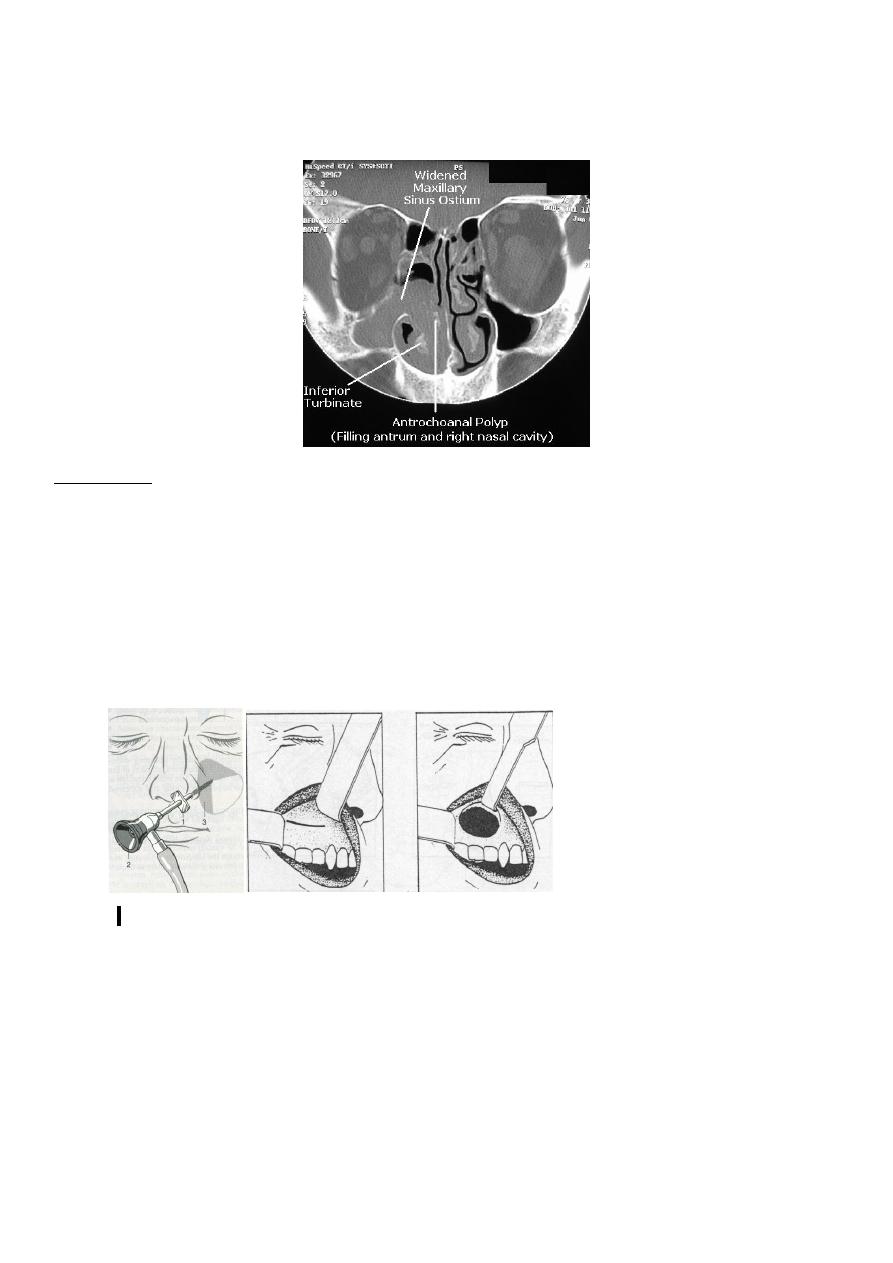
Treatment;
There is no medical treatment pre or post operatively.
Simple polypectomy; the polyp is delivered through the oropharynx and it is necessary to
remove both parts of the polyp (antral and intranasal).
Removal of the lining of the sinus; is necessary to avoid recurrence and this is achieved either
through sinoscopy or by Caldwell-Luc procedure.
Sinoscopy Caldwell-Luc procedure
IV
Differences between antrochoanal polyp and ethmoidal polyps:
INFLAMMATION OF THE SINUSES
Sinusitis is a very common disease. The maxillary sinus is the most commonly affected
in adults, followed by the ethmoid, frontal, and sphenoid sinuses. In children, the ethmoid
sinuses are most frequently affected.
Pathophysiology;
There are three important factors which impair the normal physiology of the paranasal
sinuses;
(1) Obstruction of the sinus ostia. Factors predisposing to ostial obstruction can be
further subdivided into;
a) Factors causing mucosal swelling (e.g. URTI, allergic rhinitis, swimming/diving…
etc.)
b) Factors causing mechanical obstruction. (Anatomical variants which narrow the
already narrow drainage channels of the sinuses and predispose to chronic
sinusitis e.g. chonca bullosa, i.e. aerated middle turbinate, reversed middle
turbinate, deviated nasal septum).
(2) Impaired function of the cilia; most commonly secondary to viral or bacterial infection
that cause partial destruction and paralysis of the mucosal surface, others include

V
chemical substances, foreign bodies... etc. It may be primary (genetically inherited) as
in Kartagener syndrome (Immotile cilia syndrome).
(3) Overproduction or change in the viscosity of secretions; e.g. in inflammatory
condition, long-standing dehydration…etc.
ACUTE SINUSITIS:
Is defined as acute inflammation in the mucus membrane of the paranasal sinuses. It
commonly follows common cold but may also follow dental infection, dental extraction,
swimming and diving, trauma or after a nose operation.
Bacterial infection quickly follows any viral insult and the most important pathogens
responsible for acute sinusitis include Streptococcus, Haemophilus influenzae and
Moraxella catarrhalis.
The ostium of the maxillary sinus is high and not gravity dependant, hence more
commonly affected than other group of sinuses.
Clinical presentation:
There are two common clinical presentations depending on the virulence of the
pathogens and the immune resistance of the patient;
1) A cold which lasts longer than 10 days (viral infection rarely last longer than
that).
2) A cold that seems more severe than usual, with a high fever (at least 39°C)
and a purulent nasal discharge.
Symptoms & Signs:
a) Acute severe pain:
Increase in bending forwards.
Often non-specific and the whole face aches.
In sphenoiditis (uncommon) it is localized to the top of the head or over the
trigeminal distribution.
b) Pyrexia and general feeling of malaise.
c) Copious nasal mucopurulent discharge.
d) Nasal obstruction.
e) Loss of smell.
f) General feeling of fullness in the face.
g) The nasal mucosa is often erythematous.
h) Localized tenderness may indicate the group of sinuses involved, although in acute
situation a pansinusitis is common.
Investigations;
The diagnosis is usually clinical, but the following may be helpful in confirming the
diagnosis;
VI
Plain sinus radiograph; may show opacification or mucosal thickening.
Raised WBC count and raised ESR.
Positive blood culture and culture of nasal secretion.
Treatment;
It is primarily medical and include:
1) Antibiotics; should be used for 10 days -2weeks. Amoxicillin is the preferred choice in
most cases. However there are several situation where broader spectrum antibiotic is
appropriate. Co-amoxiclave is effective for beta-lactamase producing H.influenzae. If
the sinusitis of dental origin, addition of metronidazole is required as anaerobic
infection is suspected.
Other antibiotics include co-trimoxasole , cephalosporines , ciprofloxacin and azithromycin.
2) Decongestant; Topical nasal drops of oxymetazoline and xylometazoline are used to
shrink the mucosa, improve the airway and assist sinus drainage. They should not be
used for long time to avoid the development of rhinitis medicamentosa.
3) Analgesic.
If the condition does respond to these simple measures, a surgical drainage procedure is
necessary. It is essential that adequate antibiotic therapy is given prior to surgery to prevent
septic venous thrombosis that might lead to cavernous sinus thrombosis. The most important
sinus to drain is the maxillary antrum as this is the 'conductor of the orchestra' .If the sinus
settles, oedema in the middle meatus will disappear and permits adequate drainage of the
frontal and anterior ethmoid sinuses.
The most common procedures used are;
Antral lavage.
Intranasal antrostomy used when there is pus under pressure inside the sinus.
Indwelling tube may be used for repeated irrigation without new puncture.
Complication of acute sinusitis
The most common complication of acute sinusitis is chronic sinusitis . Complications
beyond the sinus may follow an acute infection or an exacerbation of a long-standing chronic
infection and these infections may be multiple. CT scan is especially valuable in assessing
such patient.
1) Orbital cellulitis and abscess:
These conditions complicate both ethmoidal and frontal sinusitis. Three forms of
infection occur;
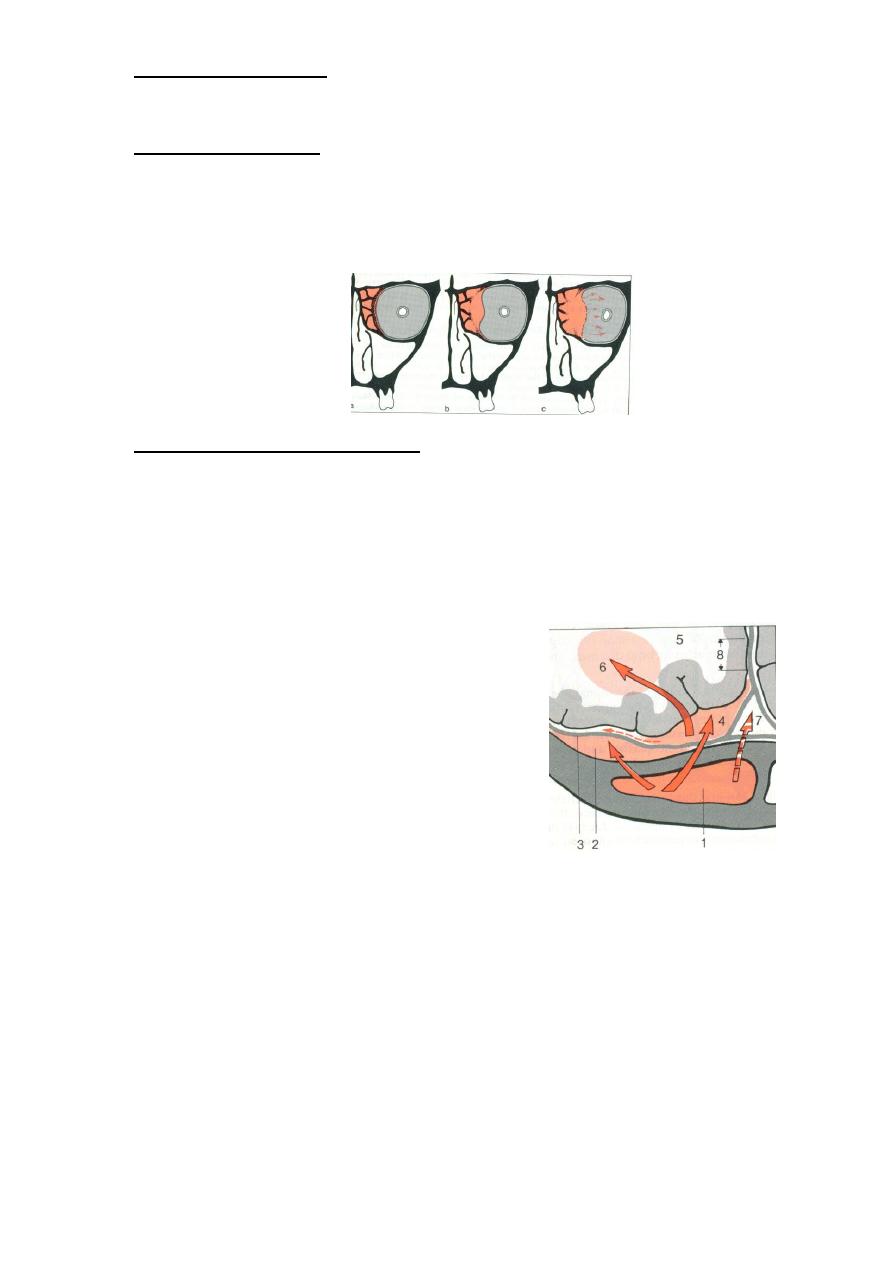
VII
a) Cellulitis of the eyelids; Usually caused by ethmoiditis in young patient. When the
eyelids are separated it is found that the eye movement, position, vision and
conjunctiva are all normal.
b) Subperiosteal abscess; Formation of pus between lamina papyracea and the orbital
periosteum. The eye is painful , slightly proptosed and displaced laterally.
Movement of the eyeball may be impaired and tension on the optic nerve may
cause blindness.
c) Cellulitis of the orbital contents; is a dangerous infection that may lead to a
dangerous cavernous sinus thrombosis and meningitis. There is severe pain and
tenderness on slight pressure over the globe. When the swollen eyelids are opened,
eye movements are found to be impaired. The eye is proptosed, the conjunctiva
oedematous, and vision may be failing. There is no papilloedema (differentiate it
from cavernous sinus thrombosis).
Genesis of intracranial complication of sinusitis
2) Intracranial complication:
a) Meningitis.
b) Brain abscess.
c) Encephalitis.
d) Cavernous sinus thrombosis;
results from thrombophlebitis of the
frontal, ethmoidal and sphenoidal
sinuses.
8
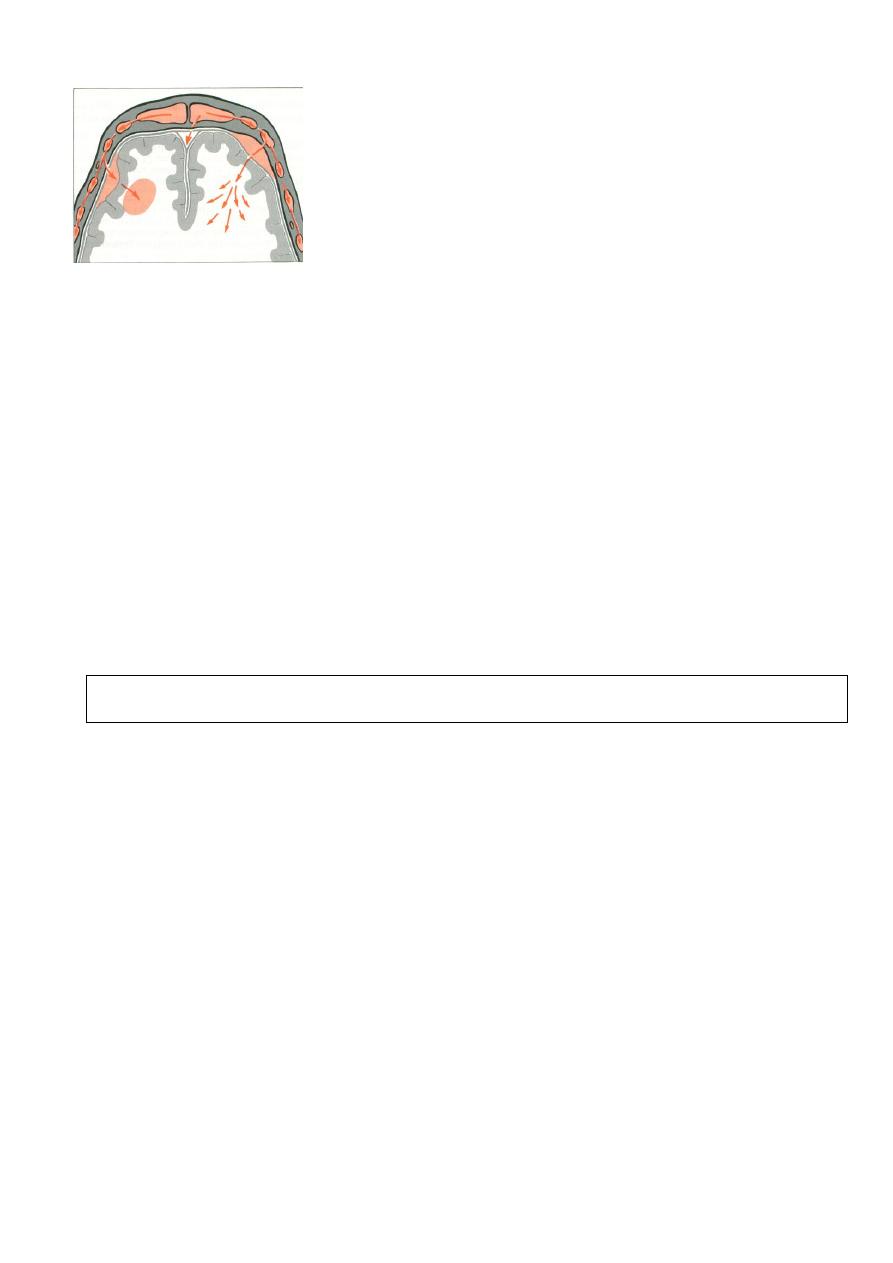
Genesis of Osteomyelitis of the flat bone of the skull
3) Osteomyelitis:
This is a rare and dangerous extension of frontal sinus disease into the diploic bone between the inner and
outer tables of the skull. Initial symptoms are minimal and the patient feels well, even though there may be already a
large extradural collection of pus. A limited area of swelling and tenderness above the sinus (Pott`s puffy tumor) is soon
followed due to subperiosteal abscess formation. It is important to recognize the significance of this type of swelling;
(The condition is dangerous although the patient does not feel ill)
4) Cutaneous fistula:
This condition is rare. Fistulae are situated near the inner canthus or eyebrow and sometimes be on the
forehead if they arise from the frontal sinus. They may develop spontaneously or occur when a subcutaneous
abscess is incised.
Chronic complication of sinusitis is frontoethmoidal mucocoeles, will be discussed in the lecture of chronic
sinusitis.
