1
Fifth stage
Pediatric
Lec-4
د.ربيع
7/10/2015
Congestive heart failure
Refers to a clinical state of systemic and pulmonary congestion resulting from inability of
the heart to pump as much blood as required for the adequate metabolism of the body.
Etiology:
Cardiac
congenital structural malformations
excessive preload
excessive afterload
no structural anomalies
cardiomyopathy
myocarditis
myocardial infarction
acquired valve disorders
hypertension
kawasaki syndrome
arrhythmia (bradycardia or tachycardia)
NONCARDIAC
Anemia
Sepsis
Hypoglycemia
Diabetic ketoacidosis
Hypothyroidism
Other endocrinopathies
Arteriovenous fistula
Renal failure
Muscular dystrophies
History
Children do not present with the typical features of congestive heart failure as seen in
adults.
2
Age is very important when assessing child.
Infants:
} Feeding difficulties
} Easily fatigued
} Sweating while feeding
} Rapid respirations
Older children:
} Shortness of breath
} Dyspnea on exertion
Physical examination:
• Tachycardia
• Rapid respiration
• Tender hepatomegaly
• Pulmonary rales
IMAGING STUDIES
The absence of cardiomegaly on a chest x-ray usually rules out the diagnosis of heart
failure.
An Echocardiogram assesses the heart chamber sizes, measures myocardial function, and
diagnoses congenital heart defects when present.
Treatment
The goals of medical therapy for congestive heart failure include the following:
Reducing the preload
Enhancing cardiac contractility
Reducing the afterload
Improving oxygen delivery
Enhancing nutrition
3
General measures:
Bed rest and limit activities
Nurse propped up or in sitting position
Expressed breast milk for small infants
Fluid restriction in volume overloaded
Correction of anemia ,acidosis, hypoglycemia and hypocalcaemia if present
Oxygen
Treatment: Phrmacological therapy
Preload reduction:
1. Diuretics: (po)or (IV) diuretics (furosemide, thiazide. Metolazone).
2. Venous dilators (eg, nitroglycerin).
Contractility support:
1. Dopamin, dobutamin
2. Digoxin
Afterload reduction
1.Oral (ACI) inhibitors
2. IV hydralazine, nitroprusside, or alprostadil
Doses:
Furosemide: 1 mg/kg/dose PO or IV
Hydrochlorothiazide: 2 mg/kg/d PO divided bid
Digoxin :TDD followed by maintenance.
IV Dopamine : 5-10 mcg/kg/min IV (usual dosage; maximal dosage May be up to
28 mcg/kg/min)
Dobutamine: 5-10 mcg/kg/min iv
Captopril: 0.1-0.5 mg/kg/d PO divided q8h
Enalapril: 0.1 mg/kg/d PO divided qd/bid, not to exceed 0.5 mg/kg/d
Carvidolol: 0.2-0.4 mg/kg/dose bid.
4
Spironolactone: 1-3 mg/kg/day.
Digoxin: Rapid digitalization can be achieved by administration of “total digitalizing dose
(TDD) as follow:
Premature: 20 μg/kg
Full-term neonate (up to 1 mo): 20-30 μg/kg
Infant or child: 25-40 μg/kg
Adolescent or adult: 0.5-1 mg in divided doses
NOTE: these doses are PO; IV dose is 75% of PO dose.
½ TDD is given initially followed by 1/4 TDD in 2 doses 12 hrs apart.
Maintenance digoxin : 5-10 μg/kg/day, divided q12h
Managing Acute Congestive Heart Failure (Acute Pulmonary Edema) in Children:
Admit to the ICU.
Head up position.
Oxygen.
IV furosemide: 1-2mg/kg.
???Digoxin (TDD).
Dopamine if ↓BP: (5-10 mcg/kg/min) .
Nitrates (nitroprusside, nitroglycerin) as venodilators if ↑ pulmonary capillary wedge
pressure
Rheumatic fever:
Due to an immunologic reaction that is a delayed sequela of group A beta-hemolytic
streptococcal infections of the pharynx.
A family history of rheumatic fever and lower socioeconomic status are additional factors.
The infection often precedes the presentation of rheumatic fever by 2 to 6 weeks.
Streptococcal antibody tests, such as the antistreptolysin O (ASOT) titer, are the most
reliable laboratory evidence of prior infection.
5
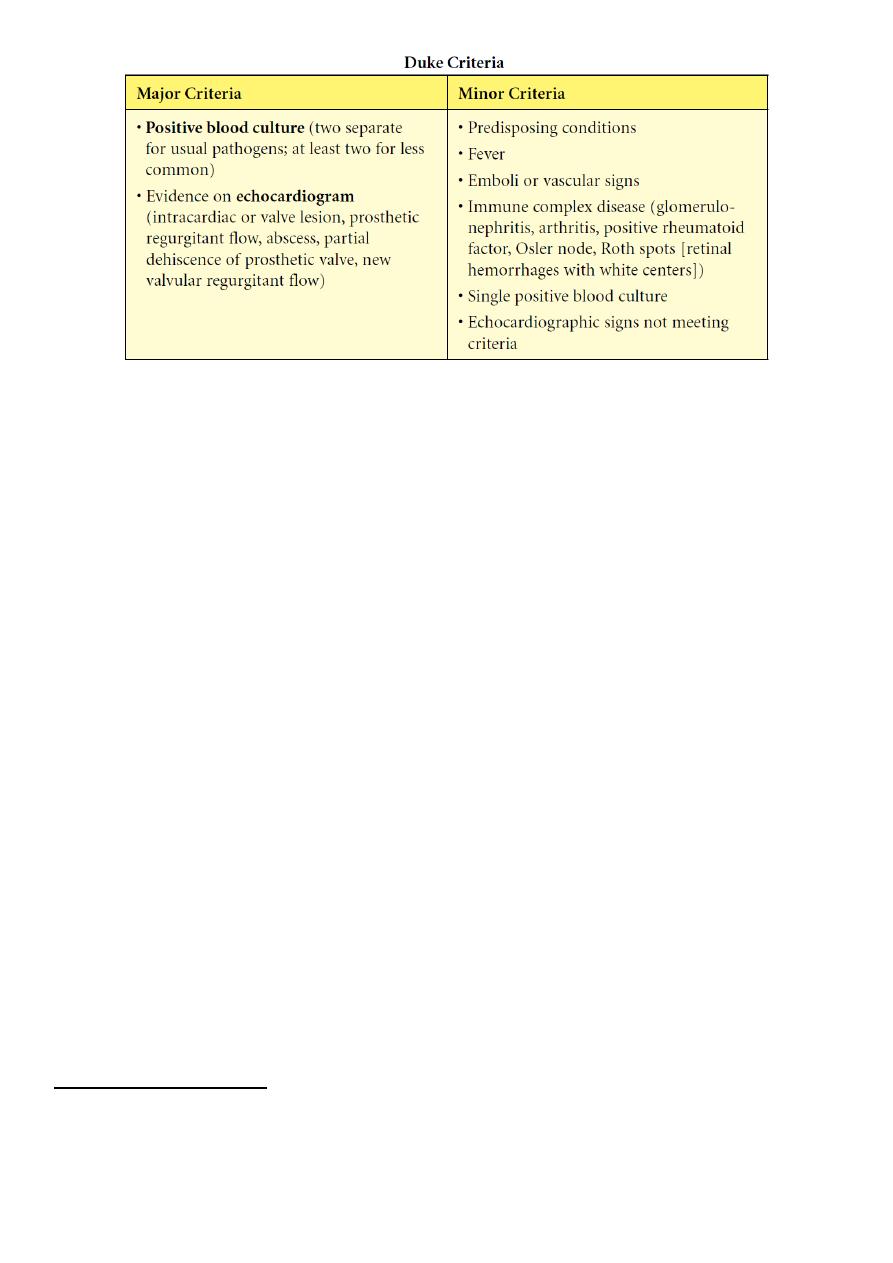
Diagnosis:
= {2 Major OR (1Major + 2Minor) Jones Criteria} + Evidence of antecedent
Streptococcal infection.
Major : Migratory polyarthritis, Carditis, Erythema marginatum, Chorea,
Subcutaneous nodules.
Minor : Fever, arthralgias, previous rheumatic fever, leukocytosis, elevated ESR/C-reactive
protein, and prolonged PR interval.
The presence of Sydenham’s chorea alone is sufficient for diagnosis.
Evidence of recent group A Streptococcal disease (e.g. scarlet fever, positive throat culture,
or elevated ASOT or other antistreptococcal antibodies) .
Treatment
Bed rest
Benzathine Penicillin 1.2 million unit im.
Salicylate: 50-70 mg/kg/day in 4divided doses PO for 3-5 days, followed by 50 mg/kg/day in
4 divideddoses PO for 3 wk and half that dose for another 2-4 wk
Prednisolone: 1-2mg/kg/day for 3 weeks for severe carditis or congestive HF.
Prevention:
Benzathine Penicillin 600,000 IU for children weighing ≤60 lb 1.2 million IU for children
weighing >60 lb, every4 wk.
Duration of prophylaxis for pt.
without carditis: 5years or until he is 21 years old.
With carditis : 10 years or until age is 40.
Infective Endocarditis ;
Etiology/epidemiology
− Most are Streptococcus viridans (alpha hemolytic) and Staphylococcus aureus
6
− Organism associations
° S. viridans—after dental procedures
° Group D streptococci—large bowel or genitourinary manipulation
° Pseudomonas aeruginosa and Serratia marcescens— intravenous drug users
° Fungi—after open heart surgery
° Coagulase-negative Staphylococcus—indwelling intravenous catheters
− Highest risk with prosthetic valve and uncorrected cyanotic heart lesions
Clinical presentation
− Prolonged intermittent fever, weight loss, fatigue, myalgia, arthralgia, headache,
nausea, vomiting
− New or changing heart murmur
− Splenomegaly, petechiae, embolic stroke, CNS abscess, CNS hemorrhage, mycotic
aneurysm (all more with Staphylococcus)
− Skin findings—rare; late findings (uncommon in treated patients); represent vasculitis
from circulating Ag-Ab complexes; if present, are highly suggestive
° Osler nodes—tender, pea-sized, intradermal nodules on pads of fingers and toes
° Janeway lesions—painless, small erythematous or hemorrhagic lesions on
palms and soles
° Splinter hemorrhage—linear lesions beneath nail beds
º Roth spots —retinal exudates
Diagnosis
Three to 5 separate blood collections should be obtained after careful preparation of the
phlebotomy site.
7
Complications
− Most common—heart failure from aortic or mitral lesions
− Others—systemic or pulmonary emboli, myocardial abscess, myocarditis, valve
obstruction, heart block, meningitis, osteomyelitis, arthritis, renal abscess, immune
complex−mediated glomerulonephritis
TREATMENT
-Empirical antibiotic therapy may be started for acutely ill persons after blood cultures are
obtained.
-High doses of bactericidal antibiotics are required for an extended period of treatment (4
to 8 weeks).
Vancomycin or a β-lactam antibiotic, with or without gentamicin, for a 6-week course is the
most common regimen.
CARDIOMYOPATHIES:
-CONGESTIVE(DILATED)
-HYPERTROPHIC
-RESTRICTIVE
Dilated Cardiomyopathy
Pathophysiology
- Extensive ventricular dilatation; mostly left ventricle.
8
- Vast majority is idiopathic (may be familial).
- Other causes-viral infection, endocrine (hypothyroidism), metabolic (storage disease),
systemic disease (connective tissue), hereditary muscle or neurologic disease (muscular
dystrophies), abnormality of coronary arteries.
Clinical presentation
- Initially nonspecific (respiratory symptoms, failure to thrive, abdominal complaints).
- Then findings of failure:
- Tachycardia, decreased pulse pressure, cool and pale skin, decreased pulses, increased
jugular venous pressure, hepatomegaly, edema, rales
- Cardiomegaly, mitral insufficiency, tricuspid insufficiency, gallop rhythm
Diagnosis
- ECG-atrial enlargement, left ventricular or right ventricular enlargement; nonspecific T-
wave changes
-Chest x-ray--cardiomegaly, pulmonary congestion.
-Echocardiogram-dilatation of left atrium and left ventricle ± right ventricle and decreased
contractility; decreased flow velocity across aortic valve with mitral regurgitation.
Prognosis-downward progression; relapses; emboli; ventricular arrhythmias & sudden
death.
Treatment
- Antifailure.
- Antiarrhythmic agents
- May need an implantable cardioverter-defibrillator (ICD)
-Systemic anticoagulation
-Beta blocker (metoprolol, carvedilol)
- Trial of PO carnitine (for possibility of mitochondrial disorder)
-Referral to transplant center
