
department of Pathology
2
nd
class /2021-2022
Prof. Dr.Nihad N. Hilal

Inflammation
: is a response of vascularized tissues
to infections and tissue damage that brings cells and
molecules of host defense from the circulation to the
sites where they are needed, to eliminate the
offending agents.
Cardinal signs of inflammation
i. Rubor (redness)
ii. Calor (heat)
iii. Tumor (swelling)
iv. Dolor (pain)
v. (loss of function)

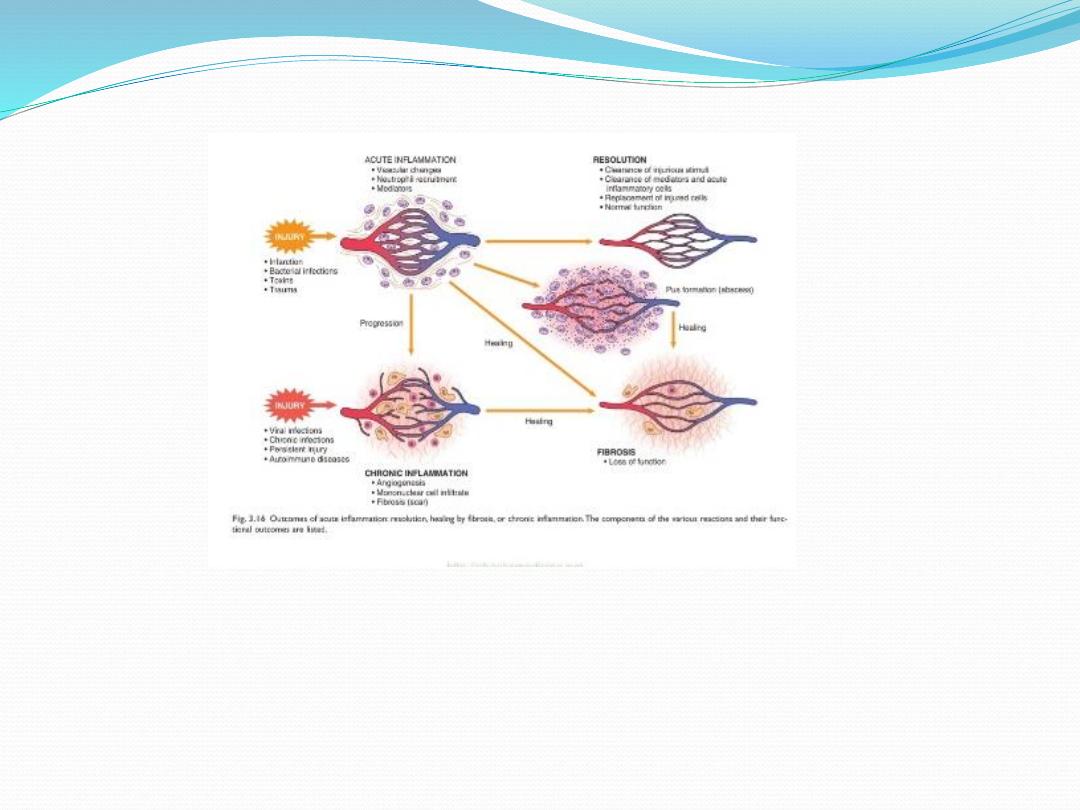
Types of inflammation
1. Acute inflammation:
2. Sub acute inflammation
3. Chronic inflammation

The major local manifestation of acute inflammation are:
1.
The vascular dilatations causing erythema
(redness) and warmth (heat).
2.
Extravasations of plasma fluid & proteins
causing edema (swelling)
3.
Leucocytes emigration & accumulation at the
site of injury.

Two major events occur in acute inflammation
1. Vascular:
2. Cellular:
(Leukocytes margination, Sticking
&rolling, Emigration, Chemotaxis,
Phagocytosis)
Initial transient vasoconstriction
(neural stimulus myospasm)
Massive vasodilatation
(mediated by histamine, bradykinin, & prostaglandins)
vascular permeability
(mediated by chemical mediators e.g., histamine, & serotonin
Mechanism of
vascular permeability
• Endothelial cell & pericyte contraction
• Direct endothelial cell injury
•Leukocyte injury of endothelium
exudation (leakage of protein rich fluid)
stasis (slowness of blood flow) due to
viscosity
margination of neutrophils

Margination
Normal blood flow is characterized by axial flow
The cellular components (RBCs, WBCs and platelets)
occupy the central column.
RBCs & more importantly WBCs will become more
closely packed near vessel wall, this is called
margination or pavementing of leukocytes .
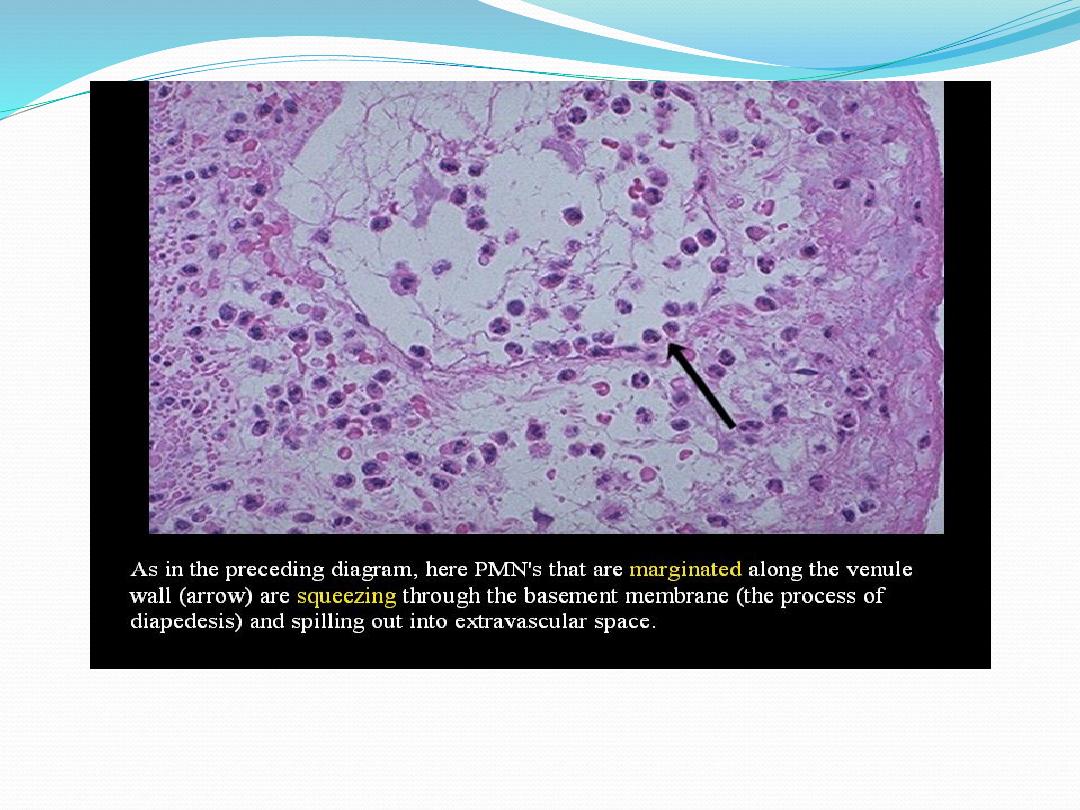
Some of leukocytes may pass through the vessel wall &
migrate into the extravascular spaces of the inflamed
area.

Sticking and rolling
The WBCs adhere in great numbers to the endothelial
surfaces of blood vessels
Emigration
-A process by which mobile WBCs escape from blood
vessels into the perivascular spaces & tissues.
- PMN emigrate from the vasculature by extending
pseudopods between endoth. cells then move between
the endoth. cells, migrating through the basement
membrane toward the inflammatory stimulus

Chemotaxis
Chemotaxis is the attraction of cells toward a chemical
mediator that is released in area of inflammation.
Important chemotactic factors for neutrophils
1. Bacterial products
2. Leukotriene B4 (LTB4)
3. Complement system product C5a
4. interleukines IL

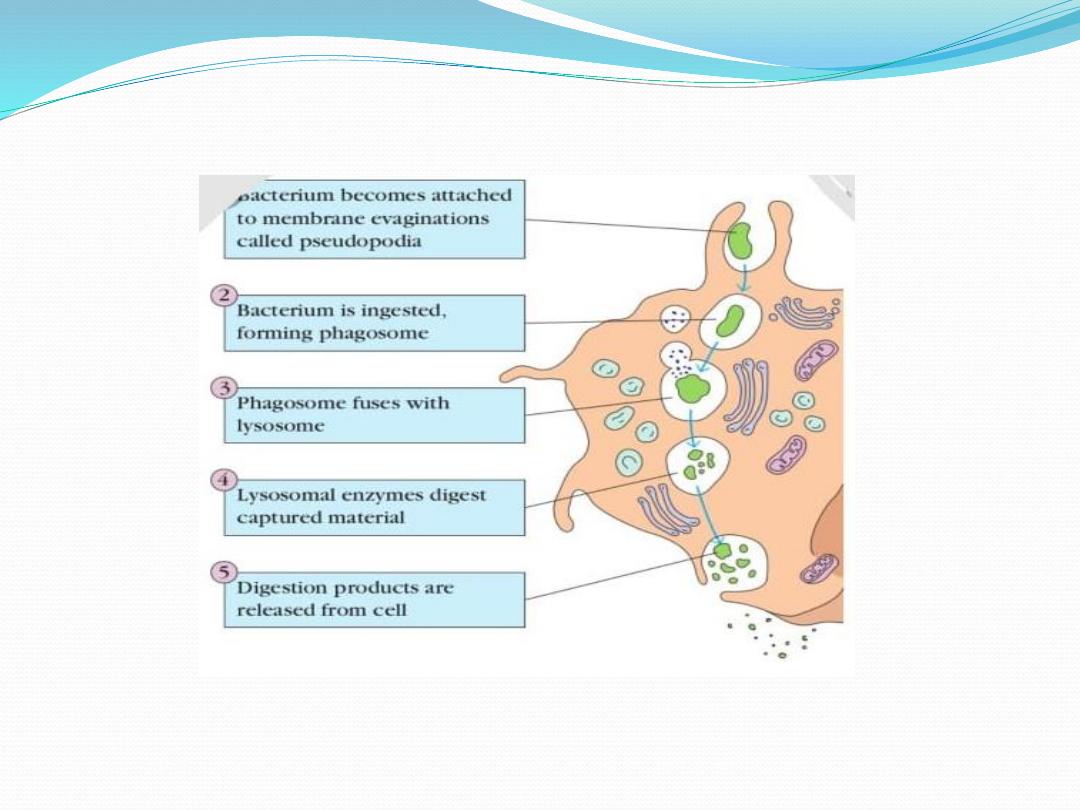
Phagoctosis & degranulation
There are four distinct steps in phagocytosis:
1
. Recognition
2
. Attachment
3
. Engulfment
4
. Killing and degradation of the ingested
material.

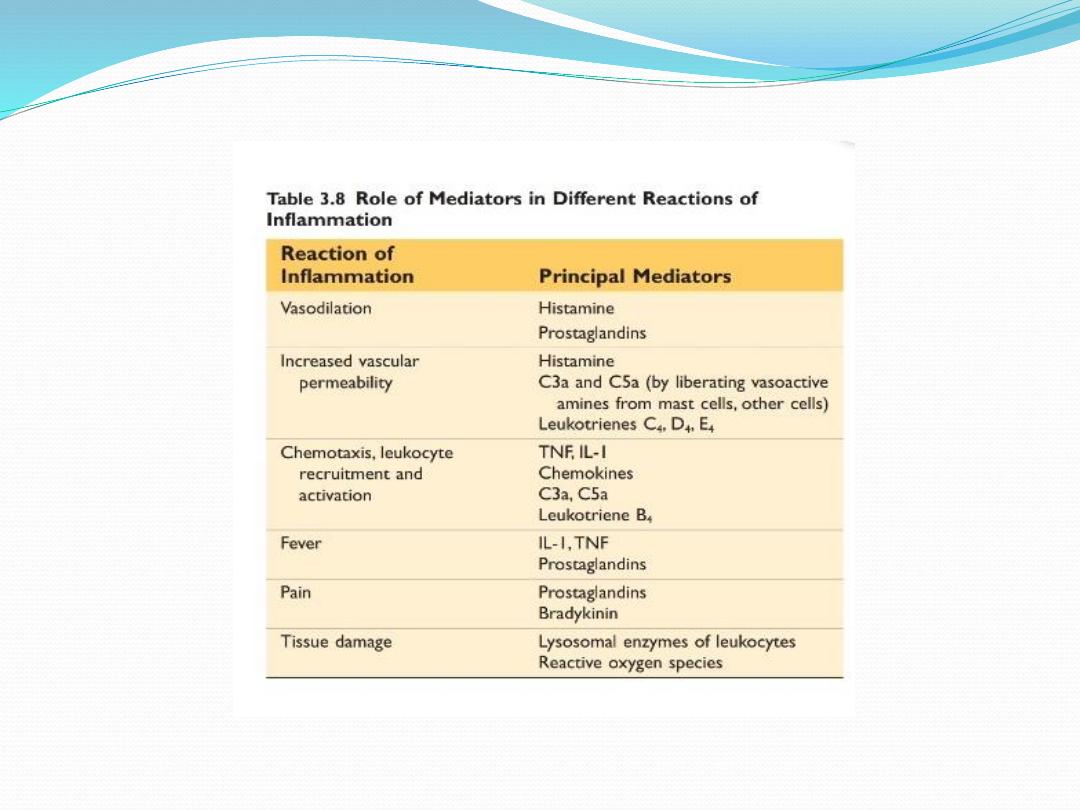
Chemical mediators of inflammation
substances that modulate (enhance, or inhibit) inflammation
1. Vasoactive amines
vasodilation &
vascular
permeability
(i) histamine:
from mast cells, basophils & platelets
(ii) serotonin:
from platelets
2.Bradykinin:
vasodilatation;
vascular permeability &
pain
3. Arachidonic acid metabolites:
injuryactivate
phospholipaserelease arachidonic acid from cell
membrane

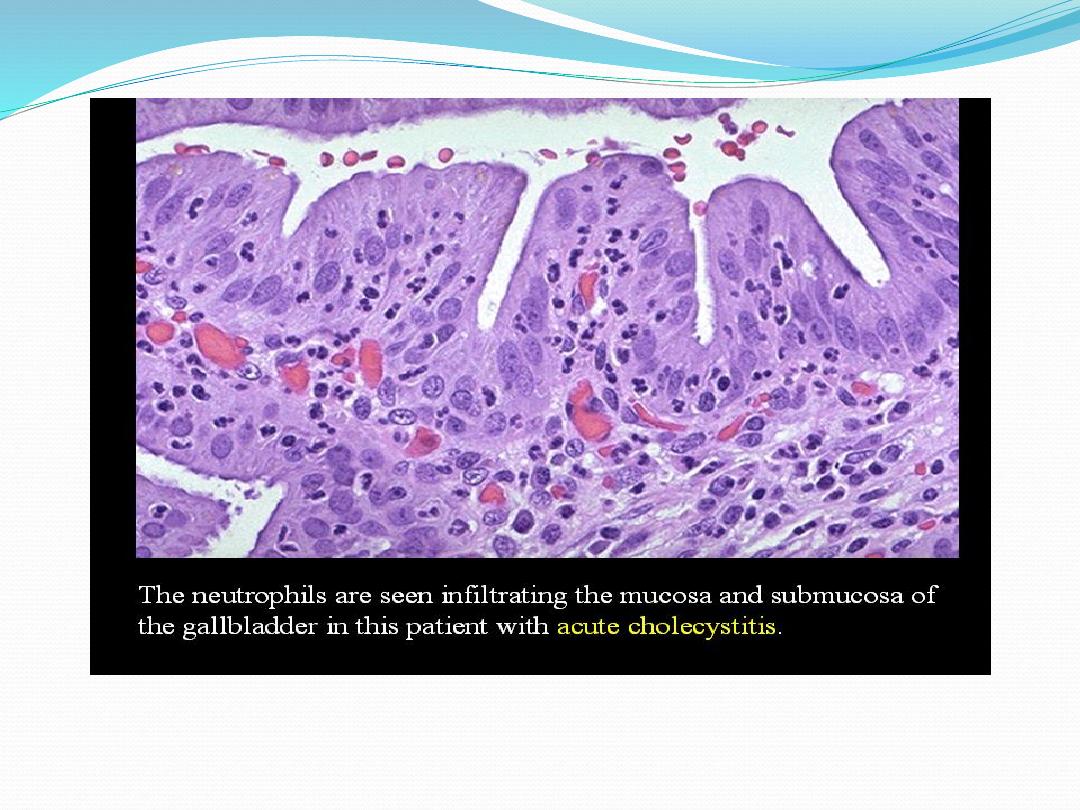
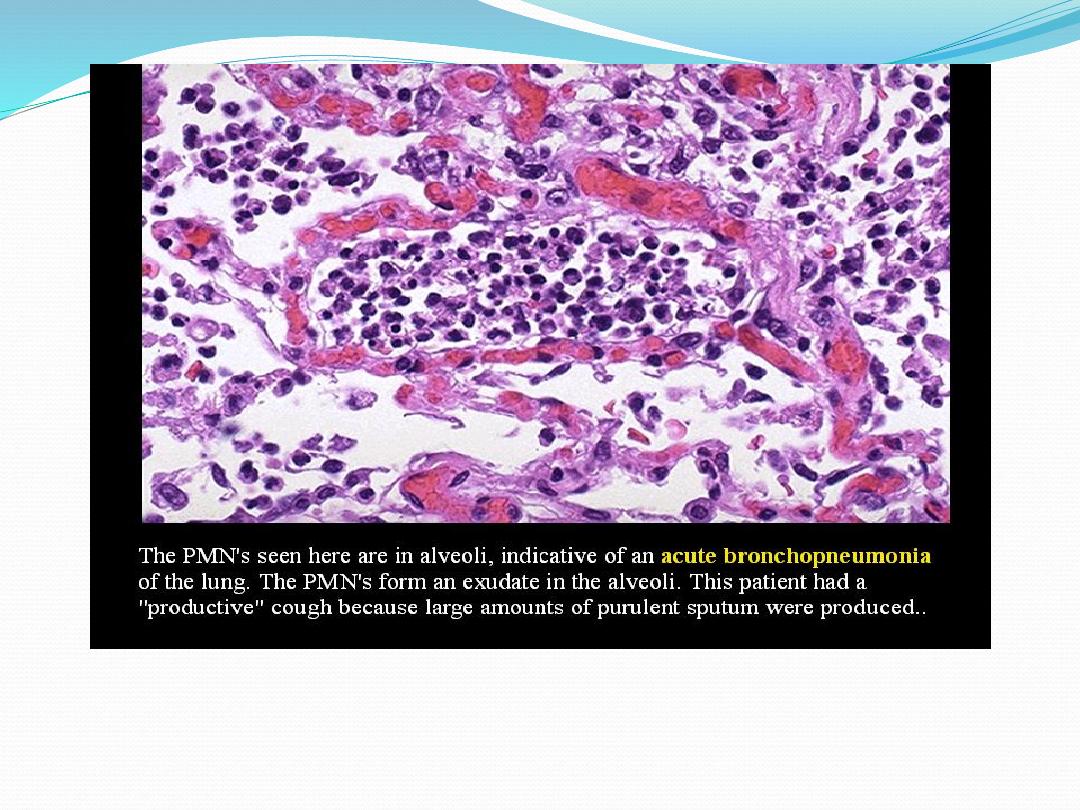
Gross morphologic patterns of acute inflammation
1. serous;
protein- rich exudate/scant cells & fibrin; serous
membrane (pleura, peritonium,synovium, pericardium)
2. fibrinous;
deposition of fibrin rich exudate as a thick layer.
3. suppurative/pyogenic
bact/fungal liquefactive necrosis
pus walled by granulation tissue (pyogenic membrane)
4. catarrhal
= inflam of mucous membranes mucus-rich
exudate (e.g., RTI, GE)
5. hemorrhage
= inflam+ hemorrhage due to vascular damage
e.g. ,meningococcemia, viral pneumonia.
6. pseudomembranous
pseudomembrane (no epith) = inflam
cells + superficial ulceration.
7. membranous
inflam of lining epithmembrane+fibrin
+ epith + inflam cells.

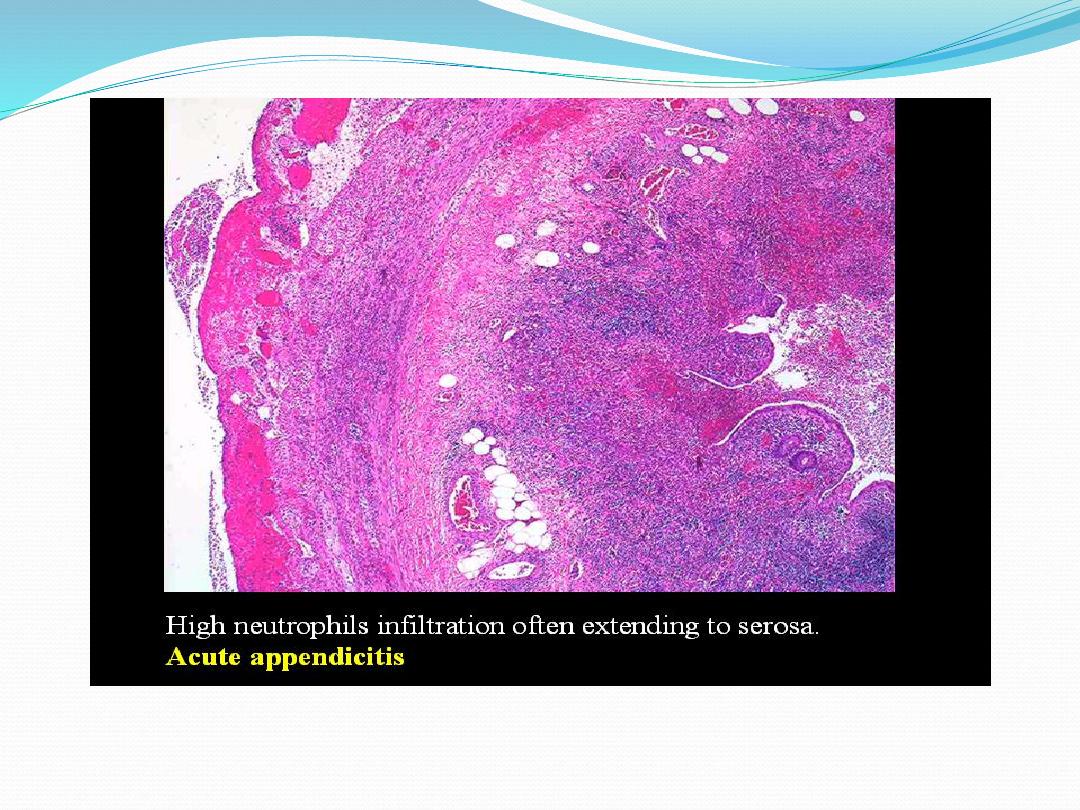
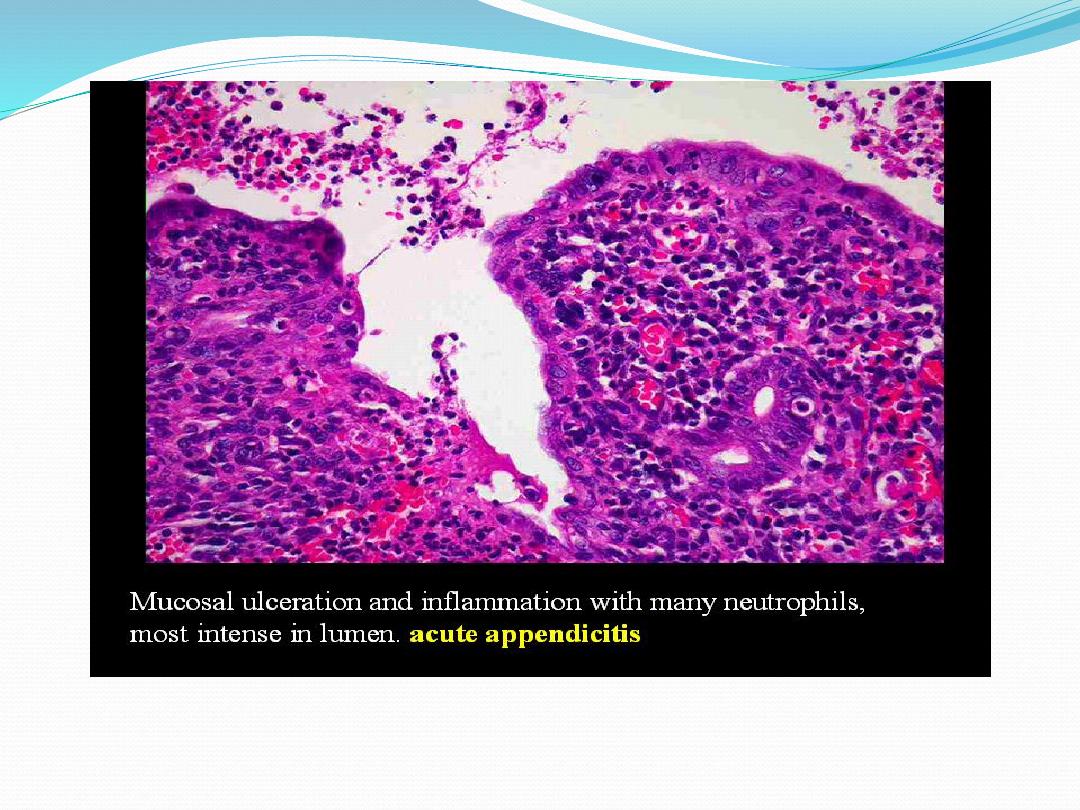
Practical - inflammation
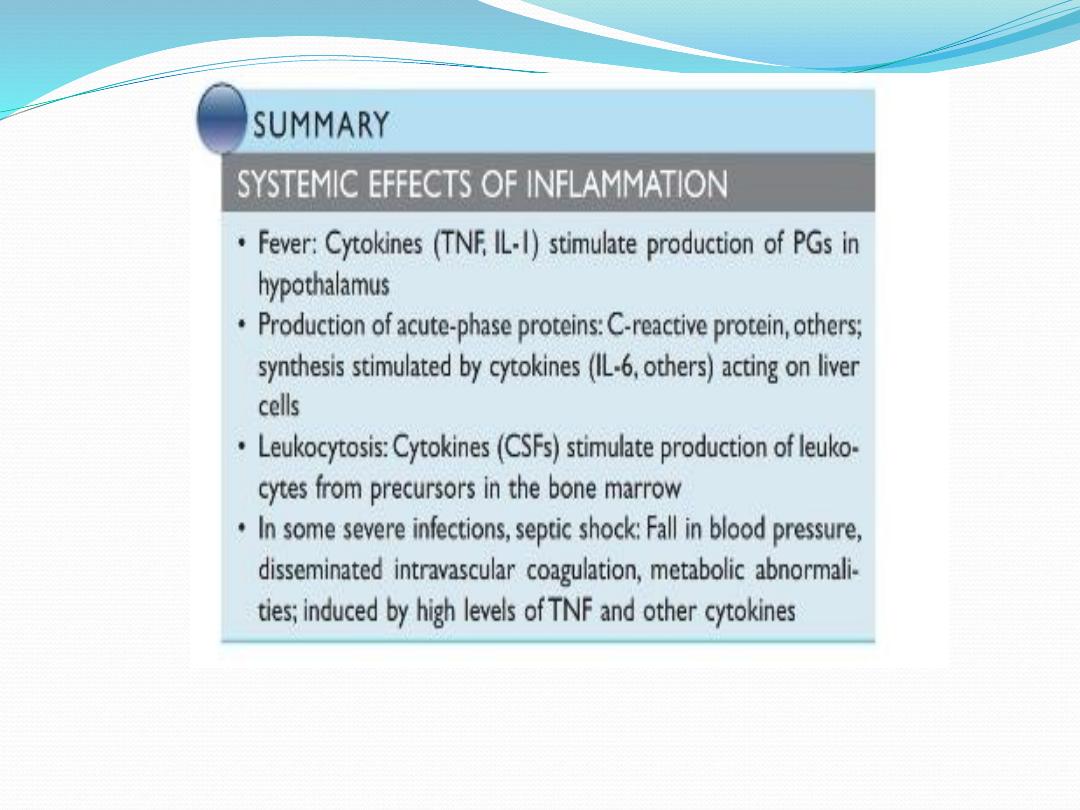
Chronic inflammation
Definition:
Inflammation of prolonged duration (weeks,
months, years) in which active inflammation, tissue
injury & healing proceed Simultaneously
Etiology
;
1.
Persistent acute/or recurrent due to persistent injury of
failure of inflammatory response to completely
degrade the agent (microbe, Fb, etc)
2
. chronic disease in origin.
(i) prolonged exposure (e.g., silicosis)
(ii) autoimmune
(iii) low virulence e.g., M Tb, fungi, syphilis, cat scratch

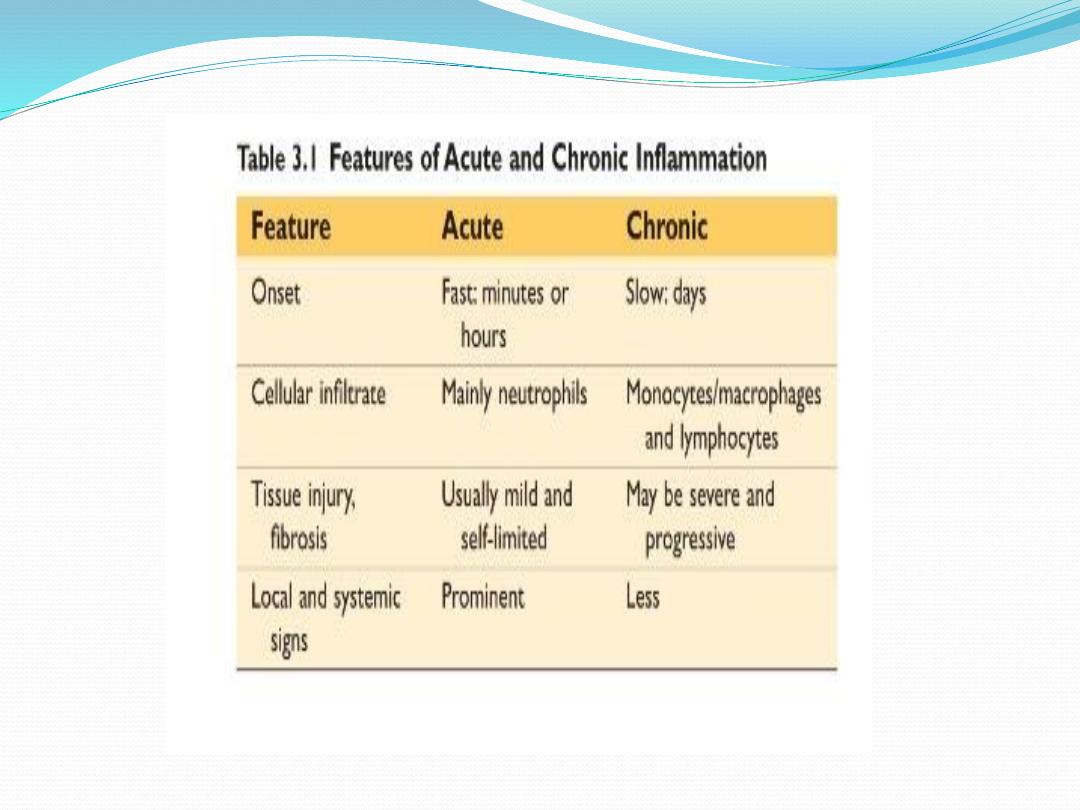
Chronic vs acute inflammation
1. mononuclear infiltration vs PMN
2. granulation tissue formation vs exudation
3. fibrosis & angiogenesis.
4. prolonged duration.
5. associated with cell mediated immunity (CMI)

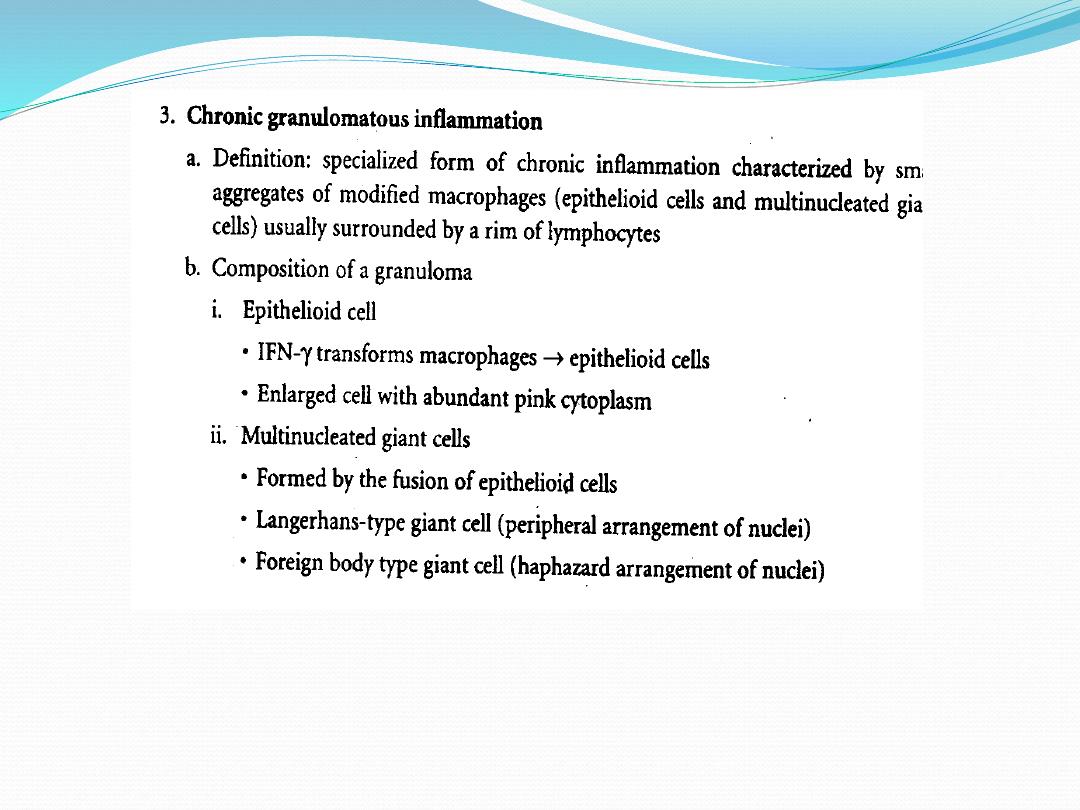
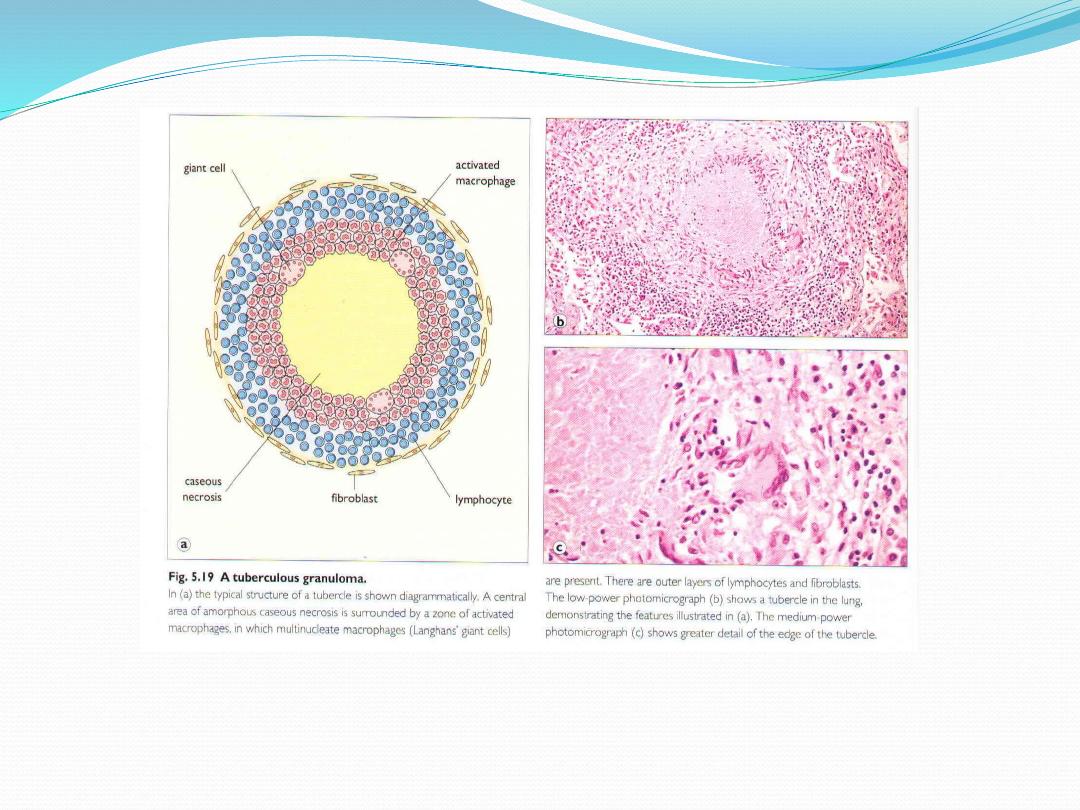
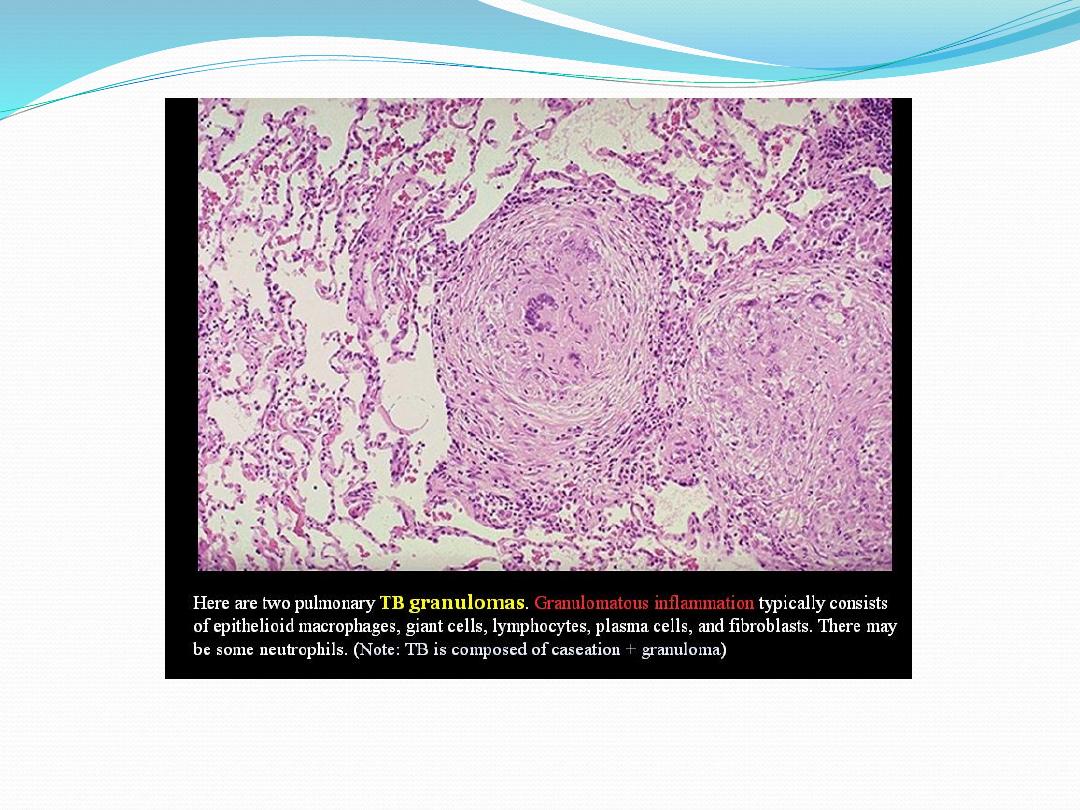
Microscopic forms of chronic inflammation
Chronic non-specific
1.
mononuclear cell infiltration (macrophages,
lymphocytes & plasma cells) & release of mediators
2. repair by connective tissue (fibrosis) involve;
(i)
angiogenesis,
(ii)
deposition of ECM
(iii)
remodeling; maturation & reorganization of
fibrous tissue.

Thank you
