Gynecology
For
5
th
stage
http://goo.gl/rjRf4F
I
LOKA
©
http://www.muhadharaty.com/gynecology
I

Content
Topics:
Page:
Gynecological history
3
Gynecological examination
7
Instruments
11
Anatomy of female genital tract
17
Normal and abnormal sexual development
18
Hirsutism
25
Disorders of the menstrual cycle
26
Genital infections
27
Fertility control and contraception
33
Infertility
38
Fibroid
42
Endometriosis
45
Ovarian cyst
46
Polycystic Ovarian Syndrome (PCOS)
48
Ovarian neoplasia
51
Endometrial carcinoma
52
Premalignant condition of the cervix
54
Cervical cancer
59
Conditions affecting the vagina and vulva
61
Urinary incontinence
67
Prolapse
69
Abnormal vaginal discharge
75
Gestational trophoblastic disease
77

Part1
: Gynecological History
Gynecological history taking has a number of questions that are not part of the standard
history taking format and therefore it’s important to understand what information you are
expected to gain when taking a gynecological history.
1- General information:
Name.
Age.
Occupation.
Residence.
Blood group.
Educational background.
Husband information.
2- Date of admission + date of examination.
3- Chief compliant:
A brief statement of the general nature and
duration of the main complaints.
Try to use the patient’s own words rather than
medical terms at this stage.
Even if the patient is being seen for an annual gynecologic examination, it is helpful
to begin the interview by asking whether the patient is experiencing any problems.
4- History of presenting illness:
This will differ slightly depending on the presenting complaint but follows a vague structure:
If pain is involved ascertain site, radiation (if any) and character
Onset
Periodicity
Duration
Recurrence?
Aggravating & relieving factors
Severity
Additional information:
o The circumstances at the time the problem began (activities, medical problems, medications).
o The time course of the problem (transient problem, chronic, recurrent, persistent)
o Relation between symptoms and the menstrual cycle.
o New or old symptom.
Full Gynecological history:
1
General information
2
Date of admission +
date of examination
3
Chief compliant
4
History of presenting illness
5
Menstrual history
6
Past Gynecological History
7
Previous obstetric history
8
Sexual and contraceptive history
9
Systemic review
10
Past Medical History
11
Drug History
12
Family History
13
Personal History
14
Social history

o If the problem involves disruption of an otherwise normal function (such as amenorrhea), did the
patient have normal function at some point in the past?
o Characteristics of the problem, and associated symptoms.
o In the case of pain, this would include questions about the location, severity, nature (e.g., sharp,
dull, cramp-like), exacerbating factors, relieving factors, and whether the pain radiates to another
location.
o With respect to bleeding, this would include the frequency, amount, and duration of flow, and
whether the patient is experiencing fatigue or lightheadedness.
o To what extent is the problem interfering with the patient’s usual activities?
o Has the patient undergone any previous evaluation or treatment for the problem? If so, it is helpful
to obtain the patient’s permission to request these medical records.
o Why did the patient seek evaluation of the problem at this point? Have the symptoms changed or
increased in severity?
o Pelvic pain:
– Site, nature, severity.
– Aggravates or relieves the pain – specifically enquire about relationship to menstrual cycle and
intercourse.
– Does the pain radiate anywhere or is it associated with bowel or bladder function (menstrual
pain often radiates through to the sacral area of the back and down the thighs)?
o Vaginal discharge:
– Amount, color, odor, presence of blood.
– Relationship to the menstrual cycle.
– Any history of sexually transmitted diseases (STDs) or recent tests.
– Any vaginal dryness (post-menopausal).
5- Menstrual history:
Age of menarche.
Usual duration of each period and length of cycle usually written as mean number
of days of bleeding over usual length of full cycle, e.g. 5/28.
LMP First day of the last period.
Frequency and Regularity
Amount of blood loss more or less than usual, number of sanitary towels or
tampons used.
Passage of clots or flooding.
Any inter-menstrual or post-coital bleeding.
Any pain relating to the period use the SOCRATES method.
Any medication taken during the period including over-the counter preparations.
If post-menopausal:
o Date of last period.
o Any post-menopausal bleeding.
o Any menopausal symptoms (hot flushes, vaginal dryness, irregular periods).
6- Past Gynecological History:
Previous gynecological symptoms, diagnosis, treatment (medical, surgical).
Previous cervical smears date of last, abnormal results, treatments (LETZ).

Current contraception COCP, POP, Depot, Implant, Coil.
7- Previous obstetric history:
G: gravida number of all pregnancies (delivered or aborted).
P: para or parity number of deliveries after 24 weeks (live or dead).
A: abortion number of expulsions of products of conception before 24 weeks
(normal or ectopic or hydatidiform)
Each Pregnancy Current age of child, Birth weight, Complications of pregnancy
and labor and after birth (puerperium).
Ask sensitively regarding miscarriages / terminations / ectopic pregnancies
Number, cause, complication of each.
8- Sexual and contraceptive history:
The type of contraception used and any problems with it.
Establish whether the patient is sexually active and whether there are any difficulties
or pain during intercourse.
9- Systemic review:
Cardiovascular Chest pain, Palpitations, Cyanosis, SOB, Syncope, Orthopnea, Ankle
swelling.
Respiratory Cough, Sputum, Chest Pain, SOB, Wheezing, Stridor, Hemoptysis.
GI Appetite, Nausea, Vomiting, Indigestion, Dysphagia, Weight loss, Pain, Bowel
habit.
Urinary Frequency, Dysuria, Polyuria, Urgency, Hesitancy, Nocturia, Incontinence.
Nervous System Vision, Headache, Weakness, Sensory disturbance, LOC, Seizures,
Incontinence.
Musculoskeletal Bone & Joint pain, Muscle pain, Joint swelling, Difficulty
mobilizing.
Dermatology Rashes, Skin breaks, Ulcers.
10- Past Medical History:
Medical conditions CIN, Genital Tract Cancers, Breast Cancers, etc.
Previous surgery abdominal or gynecological.
Any hospital admissions when & why?
11- Drug History:
Regular medication example: tranexamic acid (Treating heavy menstrual
bleeding), hormone replacement therapy (HRT).
Over the counter drugs.
Non-prescribed medications/herbal remedies.
Contraception COCP / POP / Coil / Implant / Depot.

Allergens.
12- Family History:
Consanguinity.
Any illnesses that run in the family Medical conditions or Gynecological
conditions.
Uterine / Ovarian / Genital tract / Breast cancers.
13- Personal History:
Smoking How many cigarettes per day? for how many years?
Alcohol How many units a week? – Be specific about type / volume / strength of
alcohol.
Recreational drug use.
Sleep, Appetite, Micturition, Defecation, Weight loss or gain.
14- Social history:
House? – the presence of stairs is important – will the patient manage?
Who lives with the patient? – are they a source of support?
Any carer input? – what level of care do they receive?
Occupation?
Part2
: Gynecological Examination
Introduction:
Obtain patient’s consent and with appropriate
privacy and sensitivity.
The gynecologic examination includes
examination of the breasts, abdomen, and
pelvic organs.
Many gynecologic problems have symptoms
that involve other organ systems.
General examination:
Walking poor mobility may affect decisions
regarding surgery or future management.
Examining the hands and mucous membranes
for evidence of anemia.
The supraclavicular area should be palpated for
the presence of nodes (Virchow’s node this is
also known as Troissier’s sign).
The thyroid gland should be palpated.
The chest and breasts should always be
examined (if there is a suspected ovarian mass,
as there may be a breast tumor with
secondaries of the ovaries known as
Krukenburg tumors).
Pleural effusion may be elicited as a consequence of abdominal ascites.
A general neurological assessment should be performed (suspicion of underlying
neurological problems).
The next step should be to proceed to abdominal and pelvic examination.
Abdominal examination
General notes:
The patient should empty her bladder before the abdominal examination.
The patient should be comfortable and lying semi-recumbent.
The patient is covered with a sheet from the waist down, but the area from the
xiphisternum to the symphysis pubis should be left exposed.
It is usual to examine the women from her right hand side.

Inspection:
Shape and size of the abdomen.
Abdominal distention gradual distention is caused by benign conditions like
fibroid or ovarian cyst.
Abdominal mass.
The presence of surgical scars (laparoscopy scars, Pfannenstiel scars).
Dilated veins or striae gravidarum (stretch marks) should be noted.
Hernia (the patient should be asked to raise her head or cough and any hernias or
divarication of the rectus muscles will be evident).
Pubic hair distribution (absent or reduced in conditions that cause adrenal
insufficiency such as hypopituitarism, Turner's syndrome, Alopecia and Delayed
Puberty).
Palpation:
First, if the patient has any abdominal pain she should be asked to point to the site –
the area should not be examined until the end of palpation.
Palpation using the right hand and start at left lower quadrant and proceeding to the
other quadrants.
Palpation should include examination for masses, the liver, spleen and kidneys.
Mass (abdominal mass can palpate below it, pelvic mass cannot palpate below it).
Examine the inguinal hernias and lymph nodes.
Look for signs of peritonism (guarding and rebound tenderness).
It may be helpful to ask the patient to raise her head so as to flex the rectus
abdominus muscles. Tenderness localized to the abdominal wall will typically worsen
with this maneuver.
Percussion:
Ascites (shifting dullness, fluid thrill).
An enlarged bladder due to urinary retention will also be dull to percussion (many
pelvic masses have disappeared after catheterization).
Percussion is utilized to determine the size of abdominal and pelvic structures such as
the liver and masses.
Percussion is also useful for assessing abdominal and pelvic tenderness.
Auscultation:
This method is not specifically useful for the gynecological examination.
Auscultation aids in the assessment of intestinal peristalsis (bowel sounds).
Detection of abdominal bruits.
Helpful in acute abdomen with bowel obstruction or a postoperative patient with
ileus.

Pelvic examination
General notes:
Before proceeding to a vaginal examination, the patient’s verbal consent should be
obtained and a female chaperone should be present for any intimate examination.
Patient asked to empty her bladder before the examination (except in urinary
incontinence).
Midstream sample should be collected (If a urine infection is suspected).
The examiner should wear gloves for this part of the procedure.
Inspection
The patient in the dorsal position, the hips flexed and abducted and knees flexed.
The left lateral position can also be used.
Examine the external genitalia and surrounding skin, including the peri-anal area.
Patient is asked to strain down to enable detection of any prolapse.
Patient is asked to cough, as this may show the sign of stress incontinence.
Any lesions or developmental abnormalities are noted.
Hormonal abnormalities may cause changes in the external genitalia, such as
clitoromegaly. States accompanied by low levels of estrogen are associated with
atrophy of the mucosa.
The skin should be inspected and palpated for superficial and subcutaneous lesions.
The Bartholin’s gland openings may be visible, but the normal Bartholin’s gland is not
palpable.
The urethra is inspected for the presence of caruncle and other findings.
Speculum:
A speculum is an instrument which is inserted into the vagina to obtain a clearer view
of part of the vagina or pelvic organs.
There are two principal types:
1- Bi-valve or Cusco’s speculum allows visualization of the cervix, take sample
from the cervix, e.g. smear or swab.
2- Sim’s speculum useful for examination of prolapse as it allows inspection of the
vaginal walls.
There is plastic disposable speculums, but a metal one can be warmed to make the
examination more comfortable for the patient.
Excessive lubrication should be avoided and if a smear is being taken, lubrication with
anything other than water should be avoided.
The vagina and cervix are inspected for lesions. The vagina is also inspected for the
presence or absence of rugae to assess the level of estrogen present.
The examiner assesses any vaginal discharge that is present for normalcy in
appearance, color, consistency, and odor. Physiologic vaginal discharge is scant in

amount, flocculent, and white. The pH of the normal vagina is less than 4.2. Normal
cervical mucus is clear.
Bimanual examination:
This is usually performed after the speculum examination and is performed to assess
the pelvic organs.
It is customary to use the left hand to part the labia and expose the vestibule and
then insert one or two fingers of the right hand into the vagina. The fingers are
passed upwards and backwards to reach the cervix
The cervix is palpated any irregularity, hardness or tenderness noted.
The left hand is now placed on the abdomen below the umbilicus and pressed down
into the pelvis to palpate the fundus of the uterus.
The fundus size, shape, position, mobility, consistency and tenderness are noted.
The normal uterus is pear shaped and about 9 cm in length. It is usually anterior
(antiverted) or posterior (retroverted) and freely mobile and non-tender.
The tips of the fingers are then placed into each lateral fornix to palpate the
adenexae (tubes and ovaries) on each side.
The fingers are pushed backwards and upwards, while at the same time pushing
down in the corresponding area with the fingers of the abdominal hand.
It is unusual to be able to feel normal ovaries, except in very thin women.
Ovaries Any swelling or tenderness is noted, although remember that normal
ovaries can be very tender when directly palpated.
The posterior fornix should also be palpated to identify the uterosacral ligaments
which may be tender or scarred in women with endometriosis.
Rectal examination:
A rectal examination can be used as an alternative to a vaginal examination in:
Children and in adults who have never had sex.
It will help pick up a pelvic mass.
To differentiate between an enterocele and a rectocele or to palpate the uterosacral
ligaments more thoroughly.
Occasionally, a rectovaginal examination (index finger in the vagina and middle finger
in the rectum) may be useful to identify a lesion in the rectovaginal septum and when
one suspects endometriosis or a pelvic mass, or if there are symptoms attributable to
the rectal area.
Breast examination
Systemic way (setting, inspection, palpation, examine L.N).
Changes in pregnancy (enlargement, secondary areola).
Nipple (retraction, cracking, discharge).
Breast lump examination.
Part3
: Instruments
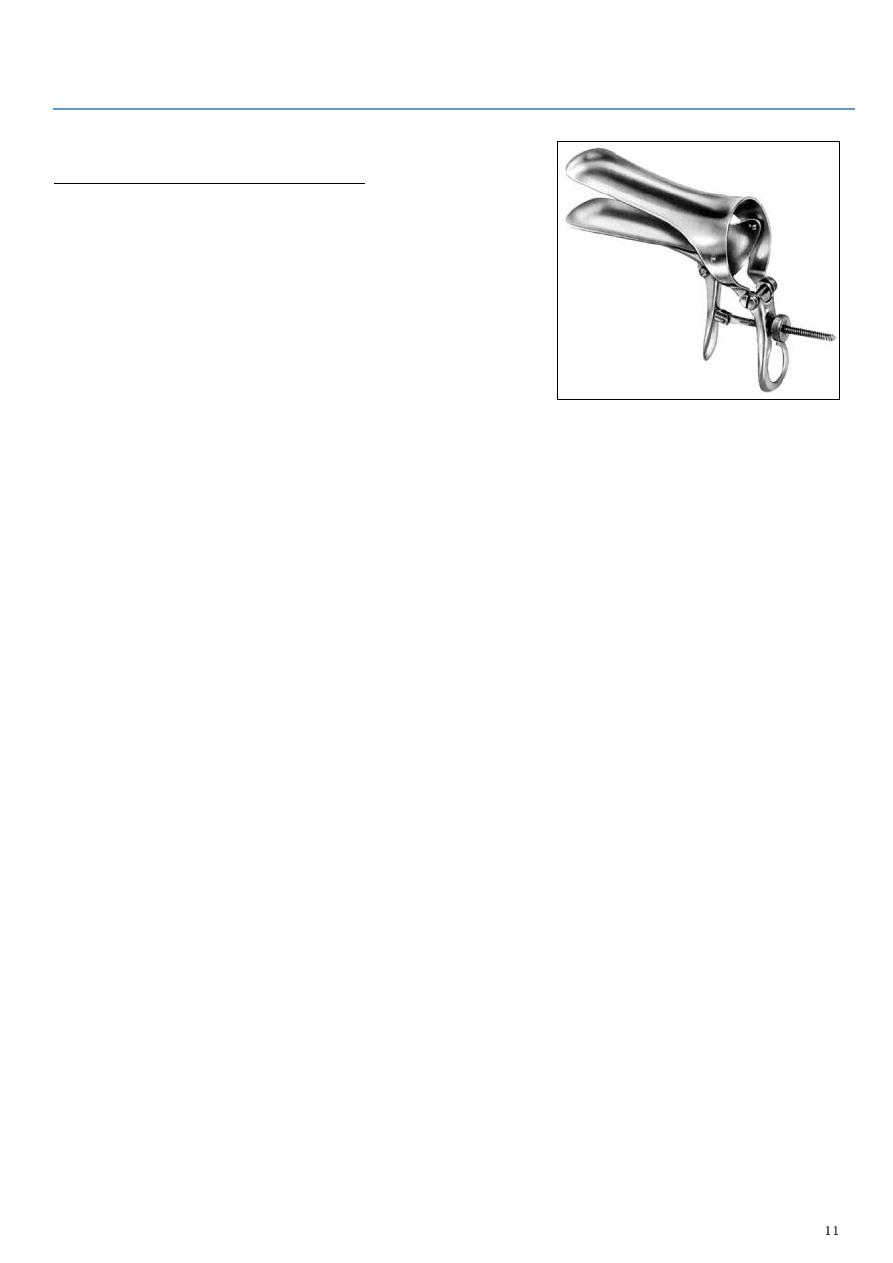
1: Bi-valve or Cusco’s speculum
Consist of upper and lower plates.
Enter through the vagina.
Used to examine the vaginal wall, visualization of the
cervix, and take biopsy.
At the beginning close the speculum and put it at 9
o'clock degree, then start to enter it through the
vestibule until reach the vagina, then rotate it to 6
o'clock or 12 o'clock, then open it and fixed it by
screw, complete the examination and investigations, then start to remove the speculum,
close the upper and lower plate by using the screw, rotate to 9 o'clock then remove it
from the vagina.
In Cusco's speculum no need for assistance and it is self-retaining.
When the speculum inside the vagina, see the following:
o Cervix: color, ulcer, abnormal discharge, nodules, erosions.
o Fornices: fullness.
o Lateral vaginal wall: rogue.
At same time of examination do some investigations like:
o Cotton for high vaginal swap put the cotton on the posterior fornix (site of
discharge accumulation) then remove the cotton without touching the vaginal
wall, then put it in container and write the name of the patient and the time of
examination and send it to the lab swap for culture and sensitivity.
o Pap smear use the spatula.
Advantages:
o It is self-retaining speculum.
o It is easy to use.
o The vaginal walls can be retracted to a variable extent.
o It gives a good exposure of the cervix.
o Both anterior and posterior vaginal walls can be retracted with a single
instrument.
o It causes least discomfort to the patient.
Disadvantages: the space available for carrying out any procedure is limited by the rim
of instrument.
Uses:
o When the biopsy is to be taken from the cervix.
o For cauterization of cervical erosions.
o For insertion of IUCD.
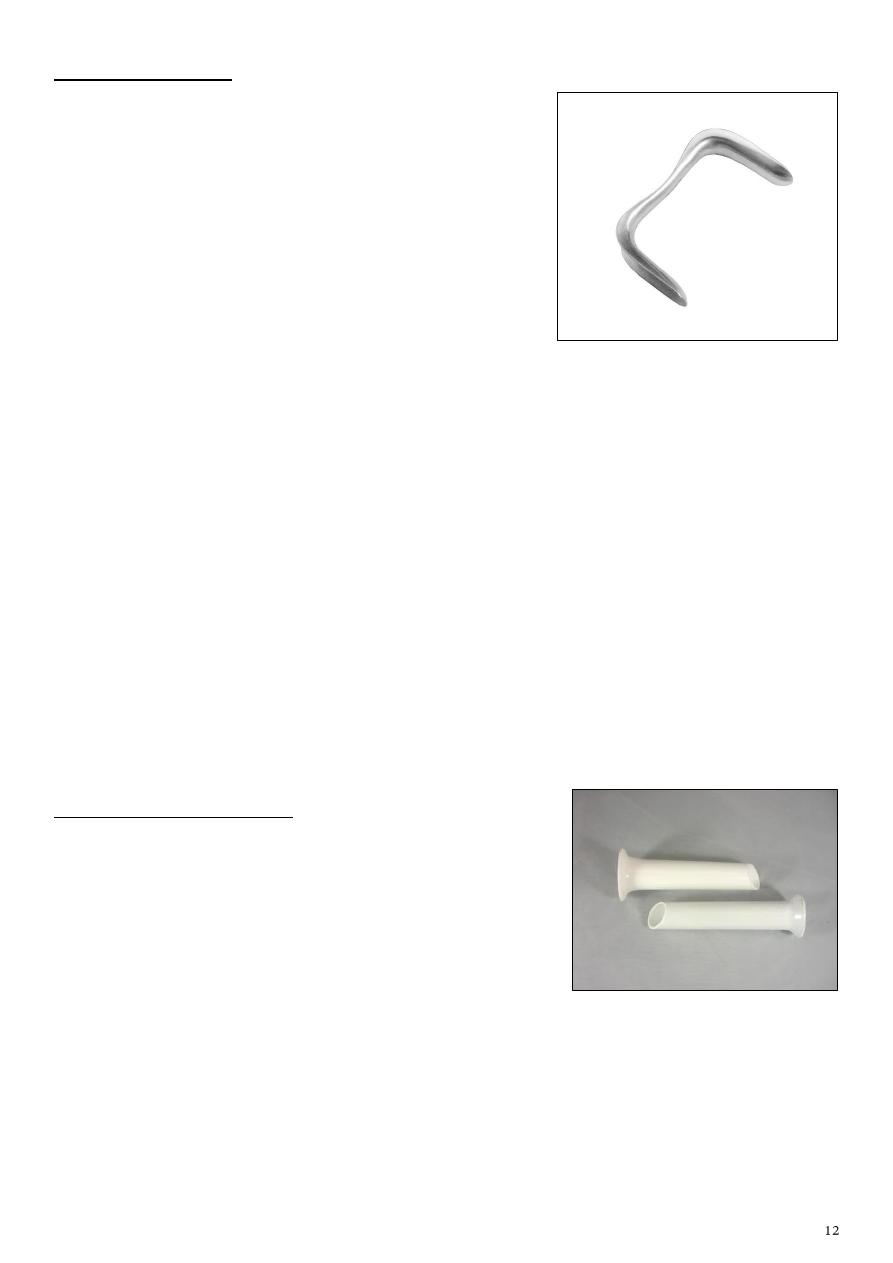
2: Sim’s speculum
Need for assistance by another person or nurse.
Used for diagnosis to see the anterior and posterior
vaginal wall.
Same procedure of Cusco's speculum, but we should
press sim's speculum downward to see the anterior
vaginal wall or pull it upward to see the posterior
vaginal wall.
Uses:
o See the Bulging of bladder (cystocele): due to
weakness of anterior vaginal wall, you can examine it by asking the patient to
come with full bladder or ask the patient to cough so the bulging become more
obvious, and see some fluid.
o Bulging of the rectum (rectocele)
o Cystorectocele.
o Used for retracting the posterior vaginal wall during dilatation & curettage (D & C)
and during dilatation & evacuation (D & E).
o For taking biopsy from genital tract.
o For routine per speculum examination.
o Outdoor cauterization of erosion.
#Note: causes of prolapse: congenital, weakness.
Disadvantages:
o An assistant is required.
o An anterior vaginal retractor is required to get a good view.
3: Ferguson's speculum:
It is a tubular speculum having no valves.
Advantages: it is protect the vaginal wall during
examination.
Uses:
o Taking biopsy or smear from the cervix.
o For cauterization of cervical erosions.
o For schiller's test ( medical test in which iodine solution is applied to the cervix in
order to diagnose cervical cancer).
o To protect the vaginal walls during decapitation operation with Gigli's wire.
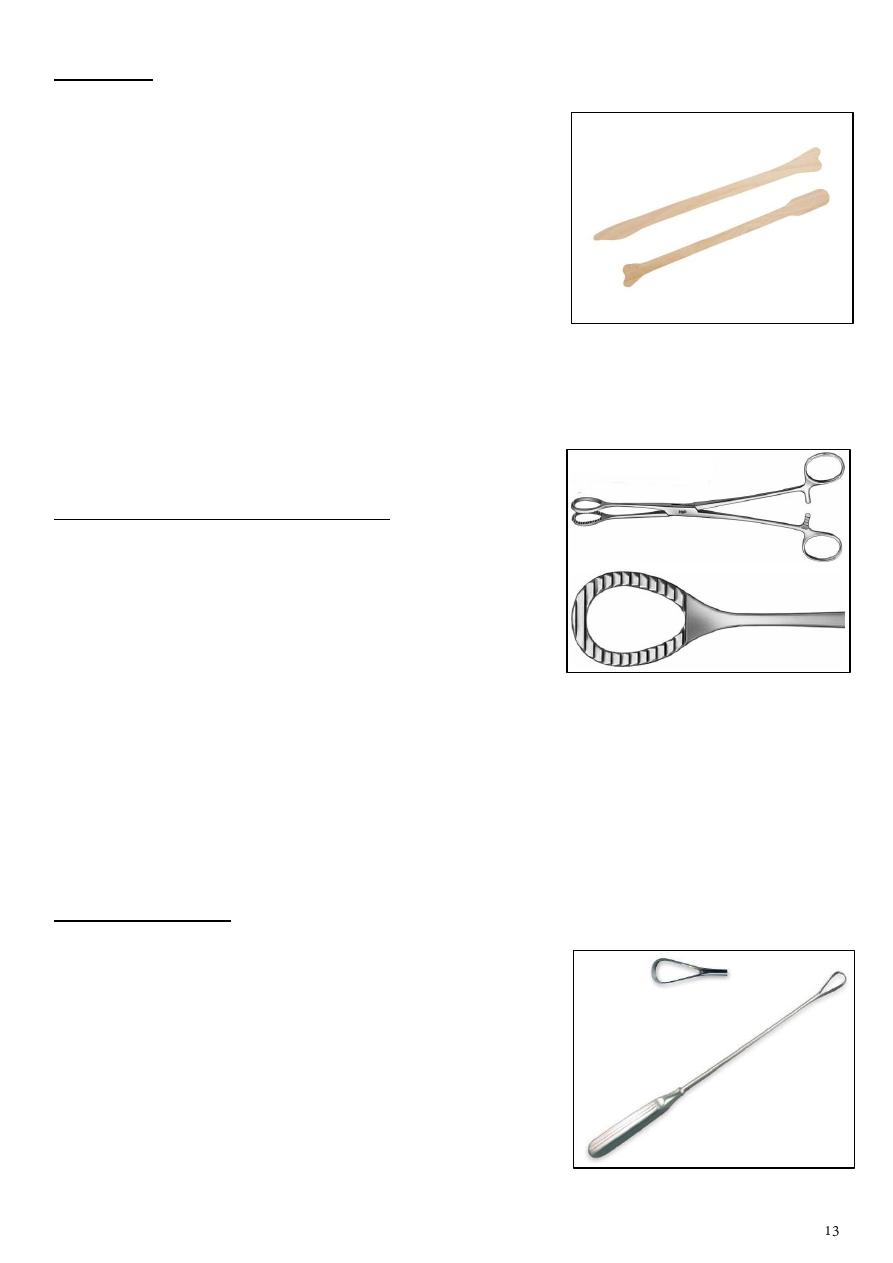
4: Spatula
Used for Pap smear do it annually to screening for
cancer.
Could be woody or plastic.
Use it with Cusco's speculum, enter it to the vagina and
take the smear.
At the top of the spatula there is lingual part (put it in
the inner part of the cervix) and shoulder part (put it in
the ectocervix).
Rotate the spatula and take columnar cells (by lingual
part) and squamous cells (by shoulder part).
Put the spatula on the slide and do fixation.
Send the slide to the lab for cytology.
5: Sponge (swab) holding forceps:
It has ring shapes tips, which may be serrated or
smooth.
Uses:
o It used for holding the sponges to swab out
cavities (vagina for example).
o Some times when the anterior lip of the cervix is friable and cannot be held by
volsellum, sponge holding forceps can be used.
o It can be used in place of ovum forceps.
o For applying antiseptics over vulva, vagina or abdominal skin before operation.
o It may be applied on infundibulopelvic ligaments to control bleeding in
myomectomy.
6: Uterine curette
Used for dilatation and curettage (D & C).
It is used under general anesthesia.
Hormonal disturbances lead to increase thickness to 7
cm and this could be pathological or cancer so do D
& C first use uterine sound 4 then 5,6,7,8 to open
the os and it is used for dilatation to prevent injury
then use curette start form anterior then posterior
then lateral vaginal wall bleeding and tissue put
them in container lab histopathology.
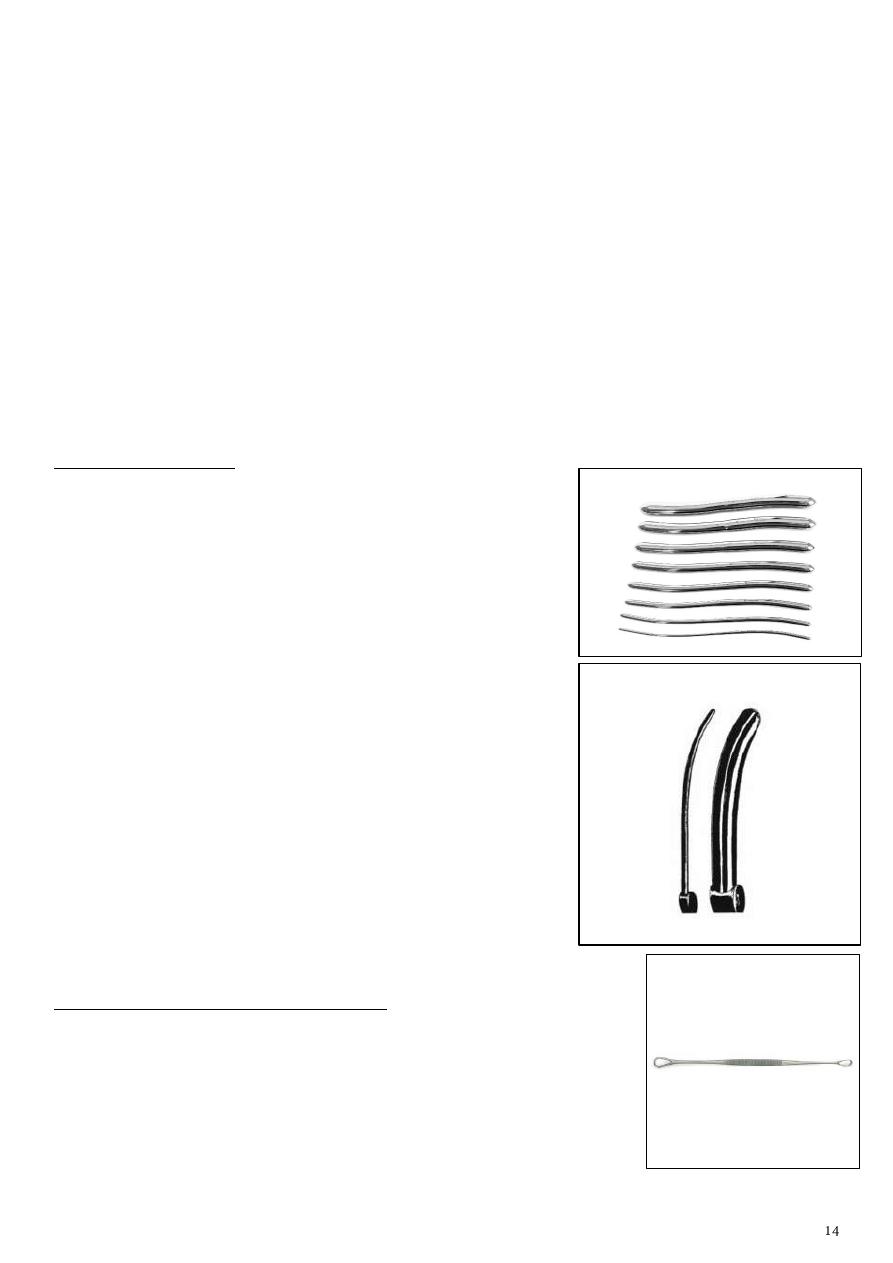
Could lead to uterine artery injury (severe bleeding).
Types Sim's curette, Sharp & blunt curette, Goldstein curette (nowadays it is not used
due to the risk of fluid embolism).
Uses:
o To curette out the products of conception in cases of missed or incomplete
conception.
o To curette out endometrium in cases of endometrial diseases for diagnostic and
therapeutic purposes (in case of infertility, postmenopausal bleeding, endometrial
cancer).
o For checking curettage: done 1 week after evacuation of H.mole.
Complications Hemorrhage, sepsis, perforation of the uterus, vigorous curettage lead
to amenorrhea due to total removal of endometrium (Asherman's syndrome).
7: Cervical dilator:
Types: Hegar's dilator, Hawkins Ambler's dilator.
Uses:
o Dilatation & curettage (D & C).
o Dilatation & evacuation (D & E).
o To diagnose incompetence os of cervix by passing
no. 8 Hegar's dilator in non-gravid uterus.
o In operation of cervix amputation of cervix,
repair and cauterization of cervix.
o For insufflations tests Insufflate means to
deliver air or gas under pressure to a cavity of
chamber of the body.
o To relive some causes of spasmodic
dysmenorrhea.
Complications sepsis, hemorrhage, perforation of the
uterus, cervical tear which cause cervical incompetence
or cervical dystocia at a later date.
8: Anterior vaginal wall retractor:
It has 2 loop-shaped ends with transverse serrations.
Uses it used with Sim's speculum to retract the anterior
vaginal wall for visualizing the cervix and anterior fornix.
Hegar's dilator
Hawkins Ambler's dilator
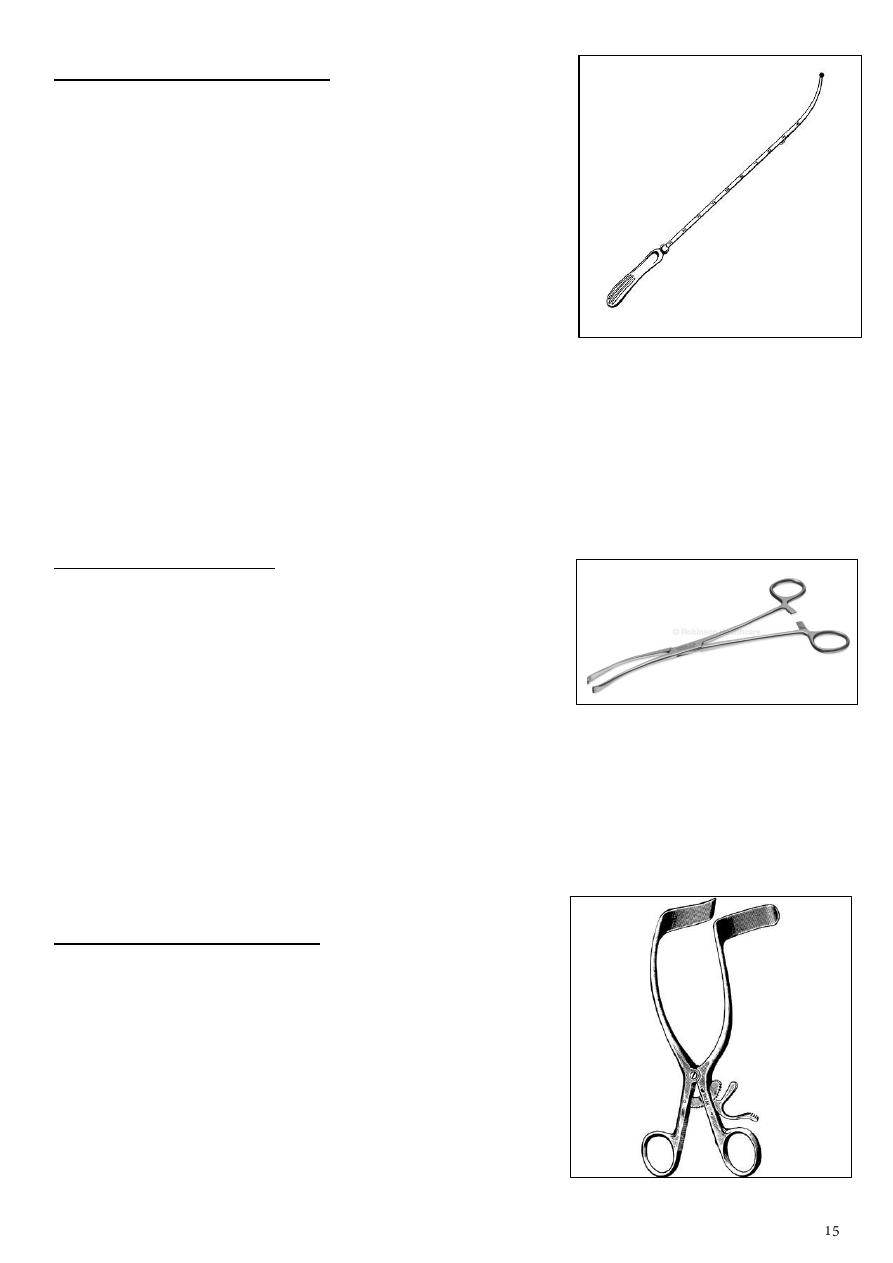
9: Simpson's uterine sound:
It is a granulated metallic rod about 12 inches long.
The distal end is curved at an angle of 60 degree and it
is 2 inches long (normal cervical length) and the tip of
the instrument is blunt.
Uses:
o To ascertain the size and direction of the uterus
before passing the cervical dilator.
o To ascertain the position of abnormal uterine
content like tumor, polyp, etc.
o For correction of the a mobile retroverted uterus (with precaution).
o For insufflations tests.
o The uterus is sounded routinely before operations on uterus or cervix.
It is not used when pregnancy is suspected, cervical infection is present.
Complications sepsis, perforation of the uterus.
10: Volsellum forceps:
It is used to hold the anterior lip of the cervix when it is
not friable that is in gynecological conditions.
It has got sharp teeth at the end which provide firm
grip.
Uses:
o For holding the anterior or posterior lip of cervix in various operations D & C,
cauterization of cervix.
o To test the mobility of cervix and laxity of ligaments in prolapse.
o To bring down fundus of uterus in vaginal hysterectomy.
o For small fibroids in myomectomy.
11: Self-retained retractor:
Used for retraction of abdominal wall.
Not need surgeon assistance.
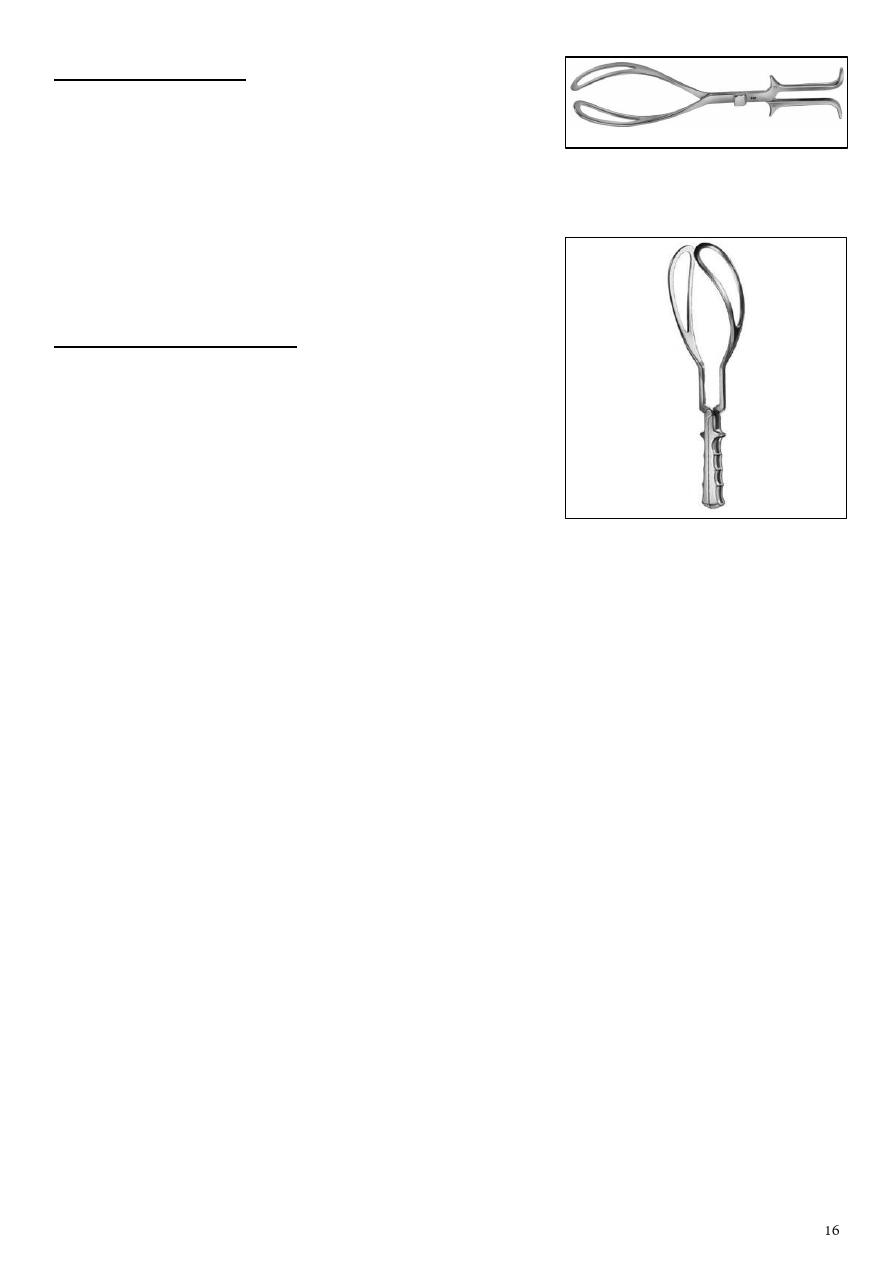
12: Killund forceps:
Has only one curve.
Cannot be locked.
Used for the rotation of the baby.
Need good experience physician.
It is not used widely nowadays because of its severe
complications.
13: Long curved forceps:
Has two curves, one for cephalic presentation, the
other for breech.
Can be locked.
Cannot be used for rotation.
Part4
: Important subjects
Subject1: Anatomy of female genital tract
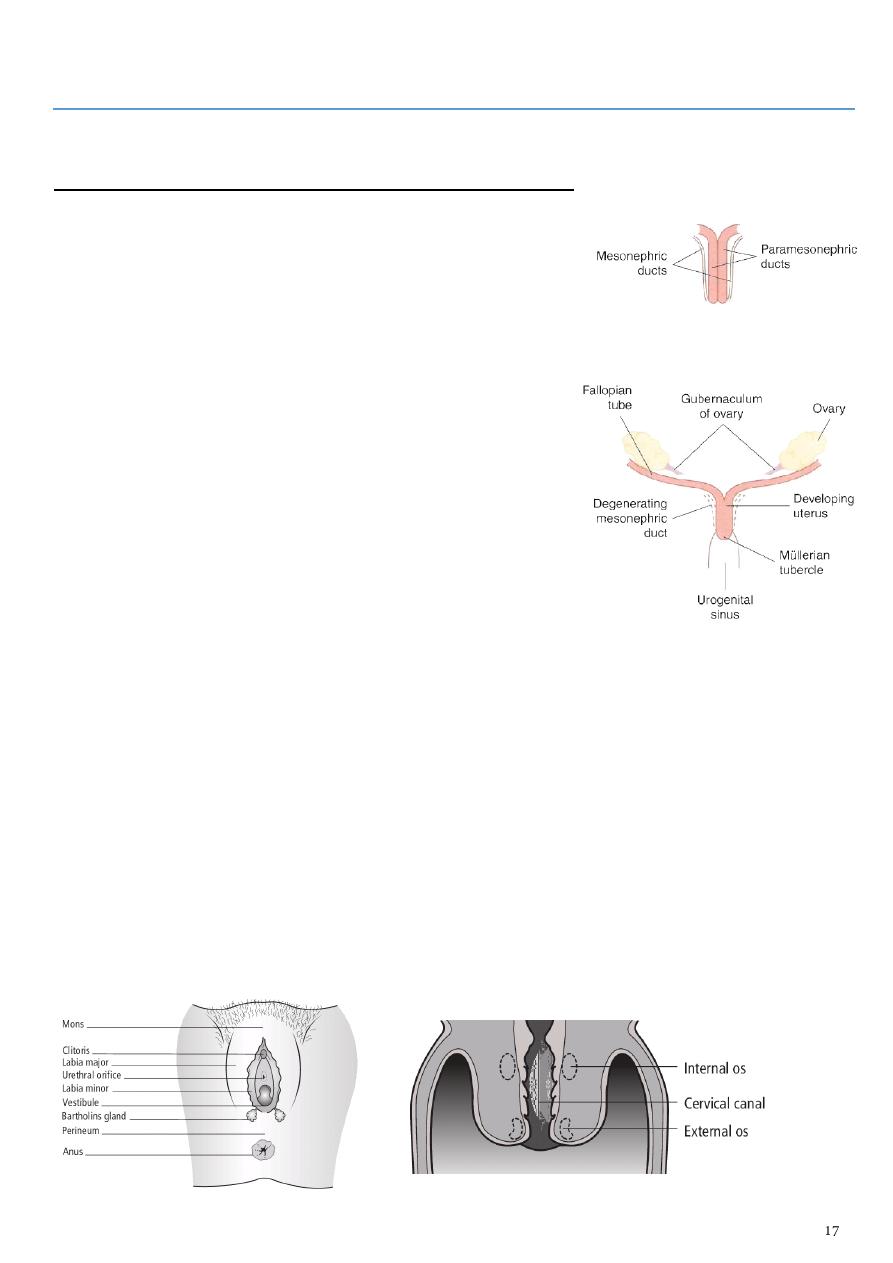
#Development of the genital organs:
Start by the 5
th
week.
The origin of all genital organs form Genital ridge,
mesonephric (wolffian) duct, para-mesonephric
(mullerian) duct.
Development of external genitalia:
o Genital tubercle clitoris.
o Genital folds labia minora.
o Genital swellings labia majora.
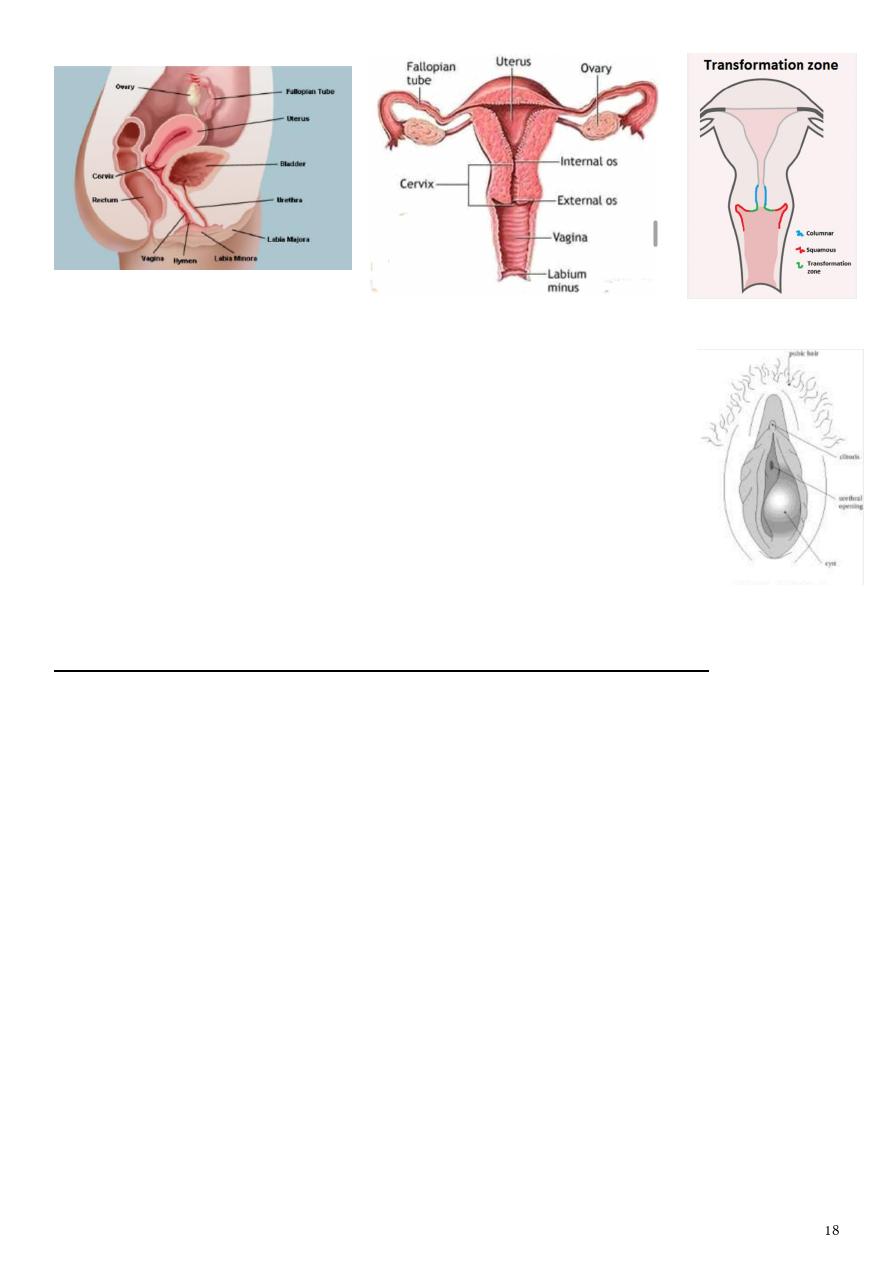
#Anatomy:
The vulva (external genitalia) include mons pubis,
labia majora, labia minora, clitoris, vestibule and vestibular orifice, greater vestibular
glands.
The vagina posterior wall (9cm), anterior wall (7cm), fornices (anterior, posterior,
two lateral), contain rugose, has no glands, Doderlein's bacillus (PH 4.5).
The uterus corpus (fundus, cornu, isthmus), anatomical internal os, anteversion and
anteflexion, layers (peritoneum, myometrium, endometrium), ligaments (cardinal,
round, uterosacral).
The cervix 2.5-3 cm, supra-vaginal part (columnar epithelium), vaginal part
(stratified squamous epithelium), transformation zone, anatomical external os.
The fallopian tube interstitial part, isthmus, ampulla, infundibulum.
The ovaries almond shape, solid, grayish pink, 3cm long, 1.5 cm wide, 1cm thick, 10
g weight, ligaments (ovarian, suspensory, mesovarian).
#Bartholin's gland:
Two pea size glands, lie at the base of each bulb and open via a 2 cm
duct into the vestibule between the hymen and the labia minora.
Sometimes the duct of this gland obstruct leading to Bartholin cyst.
If infection develop it may lead to Bartholin abscess.
Painless swelling (cyst), painful swelling (abscess).
Subject2: Normal and abnormal sexual development
#General information:
Puberty occur in girls between 8-14 years.
Puberty occur in boys between 9-14 years.
Puberty occur under control of hypothalamo-pituitary-ovarian axis.
Influencing factors genetic factors, enviromental factors (nutritional status), leptin
(regulates appetite & metabolism through hypothalamus), psychological factors,
geographic location.
#Female Pubertal stages (Tanner):
P1...prepubertal ( typically age 10 &younger )
P2... early development of subareolar breast bud+/- small amount of pubic & axillary
hair.
P3... increase in size of palpable breast tissue & areola, increased dark curled
pubic/axillary hair.
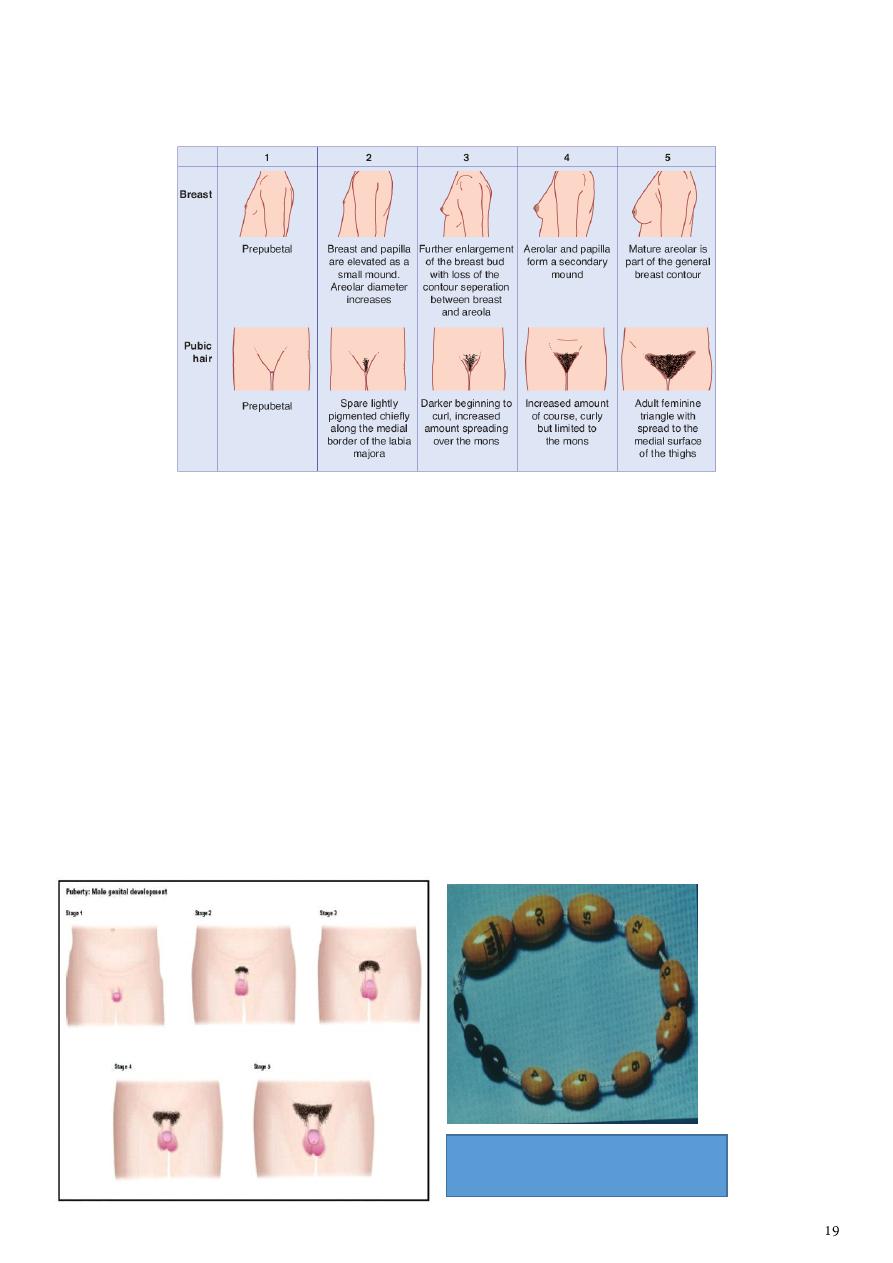
P4... breast tissue & areola protrude above breast level. Adult pubic hair but no spread
to medial thights.
P5... mature adult breast. Pubic hair extends to upper thigh.
#Male Pubertal stages (Tanner):
P 1...prepubertal (testicular volume < 2 ml, small penis) typically age 9 & younger.
P 2...enlargement of scrotum & penis, few long dark pubic hair.
P 3...lengthening of penis. Further growth of testes & scrotum. Pubic hair darker,
coarser & more curled.
P 4...penis increases in length & thickness. Increased pigmentation of scrotum. Adult
pubic hair but no spread to medial thighs.
P 5...genitalia adult in size & shape. Pubic hair spread to medial aspect of thighs.
Prader orchidometer used to measure
the size of testis during puberty
#Precocious puberty:
Refers to the development of secondary sexual characteristics <8yrs in girls & <9yrs in
boys.
Causes Gonadotrophin dependent (idiopathic,
congenital, irradiation, surgery, sever head
trauma, tumors) Gonadotrophin independent
(virilisation of female (CAH), feminisation of boy
(estrogen producing leydig tumor), adrenal tumor,
ovarian tumor, exogenous androgens, estrogen,
HCG-secreting tumor (teratoma)).
Treatment Psychological support, GnRH
agonists, treat systemic disease, surgery to
remove tumor.
#Delayed puberty:
Puberty delay if no breast development by age 13 in female, no menses by age of
15, testicular size <2.5 cm or 4 ml or pubic hair is not present by age of 14 in male.
Causes Hypogonadotrophic (idiopathic, renal failure, Crohns dis, malnutrition,
exercise, tumor of pituitary, hypothyroidism, hyperprolactinemia, PCOS, Kallman's
Syndrome), Hypergonadotrophic (Turner syndrome, Klinefelters syndrome, complete
androgen insensitivity, mixed gonadal dysgenesis, irradiation, chemotherapy, surgery,
testicular torsion, trauma, mumps orchitis, autoimmunity), Eugonadotrophic
(imperforate hymen, vaginal
Treatment Psychological support, Treat systemic disease, Promote puberty/ growth
if necessary, in male case (testosterone, hCG), in female case (estrogen replacement,
pulsatile administration of GnRH).
#Congenital Adrenal Hyperplasia (CAH):
Autosomal recessive, most common form is 21-hydroxlase deficiency.
Clinical presentation in new born female:
o Enlargement of clitoris.
o Excessive fusion of genital fold.
o Thickining
& rugosity of labia majora.
o Internal genital organs are present.
o Dangerous salt losing syndrome.

Affected male presented at age 0f 1-4 weeks with failure to thrive, reccurent
vomiting, dehydration, hypotension, shock.
Investigation Karyotype, 17a hydroxyprogesterone, Electrolyte abnormality, Pelvic
US.
Treatment of CAH Medical control of underlying disorder (Cortisol, correction of
electrolyte disorder) Surgical correction of underlying anatomical abnormality
(Reduction of clitoris, Clitoroplasty, Division of the fused labia)
#Turner's syndrome:
Karyotype 45XO, Phenotype female
Clinical signs edema of hand
& feet, Short stature, Absent
secondary sexual characteristics, Wide carrying angle of the arms,
Webbed neck, Broad chest with widly spaced nipples, Streak
ovaries, Normal internal genital organs.
Diagnosis Karyotype, Marked elevation of LH, FSH, Reduced
Estrogen, US (Cystic hygroma).
Treatment Induction of puberty by estrogen, Induction of
menstruation by progesterone, Growth hormone.
#Klinefelter syndrome:
Karyotype 47XXY
Phenotype..male
Small azospermic testis, abnormal secondary sexual characteristics,
Gynecomastia, infertile or reduced fertility.
Testosterone is low normal, raised FSH, LH, estrogen.
Treatment Androgen, Reduction mammoplasty.
Case of ambiguous genitalia the
most common cause is CAH.
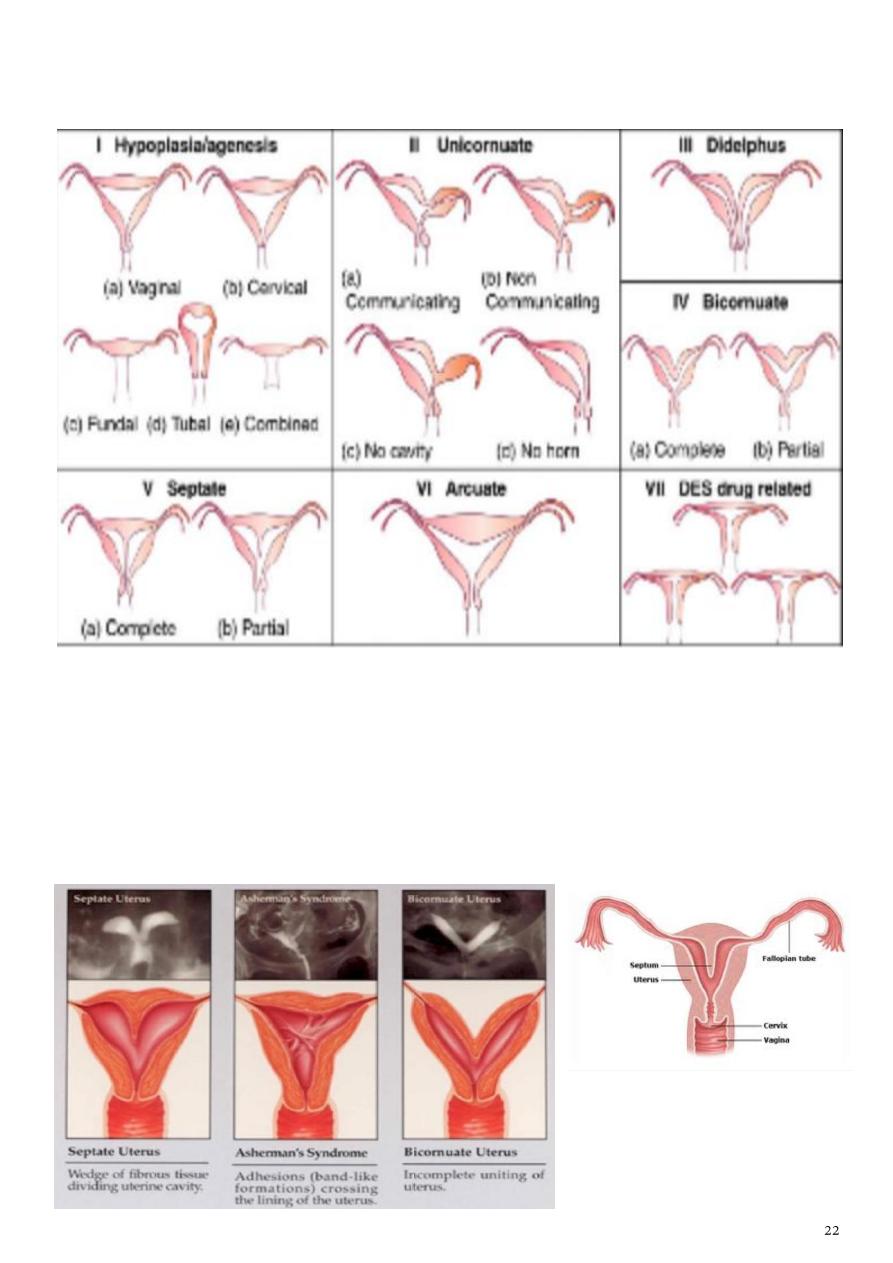
#Anomalies of internal genital organs (Mullerian Anomalies(:
Types:
Clinical manifestation Asymptomatic, Dysmenorrhoea, Dyspareunia, Pelvic pain,
Infertility, Recurrent miscarriage, Malpresentation, Preterm labour, Rarely ectopic
pregnancy.
Diagnostic evaluation pelvic US, CT, MRI, sonohistogram, HSG, hysteroscopy,
laproscopy.
Treatment many require no treatment, uterine septa can be excised with
hysteroscopy.
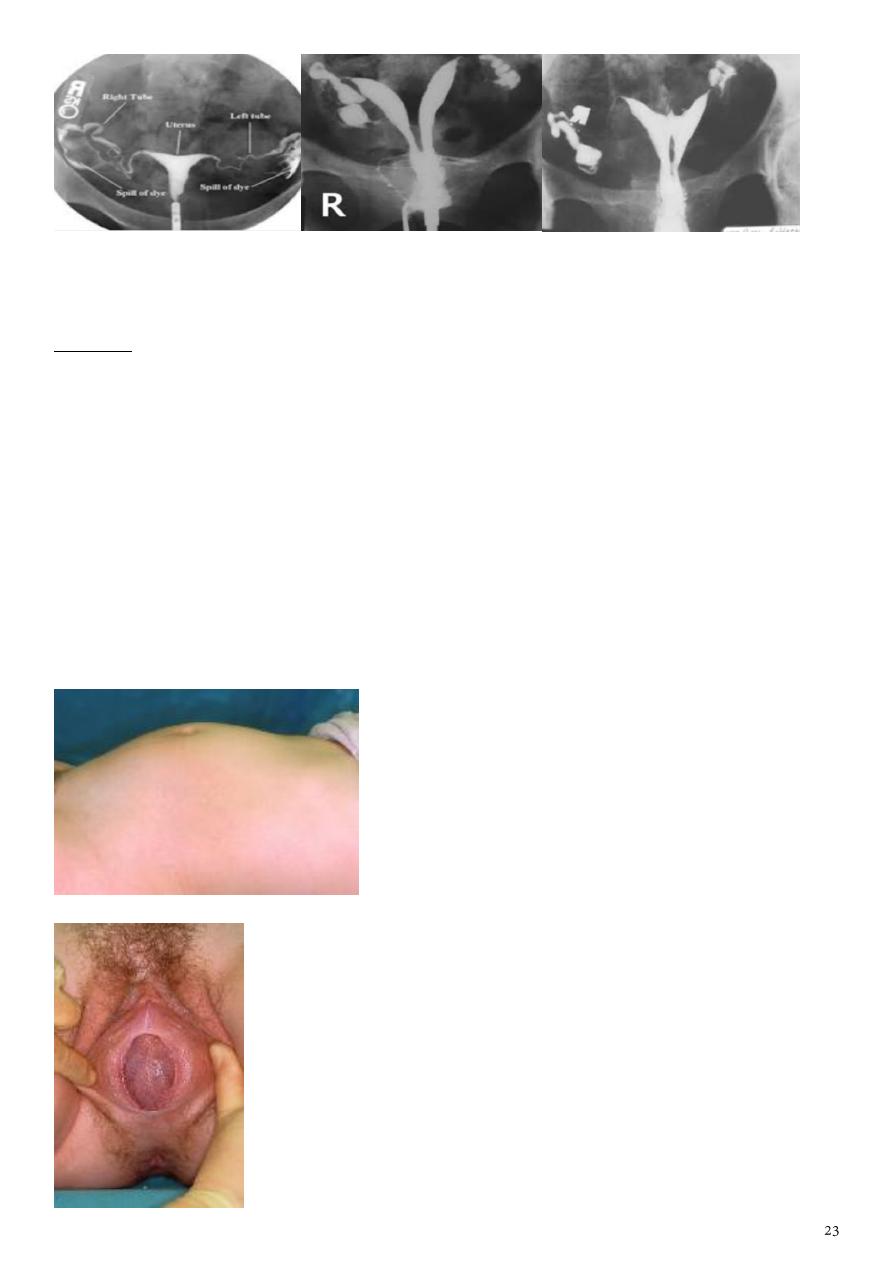
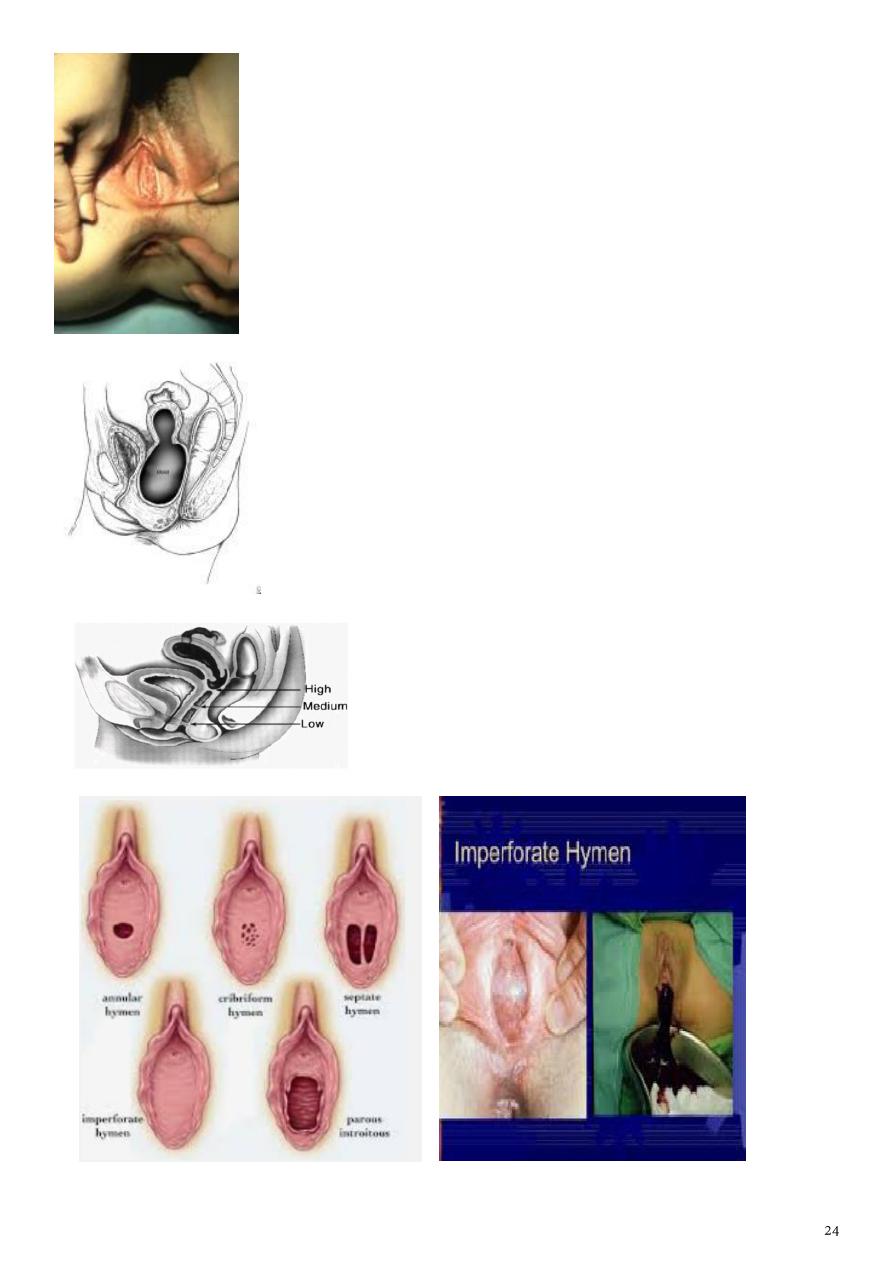
#Imperforated hymen:
Question
16 years old female presented with primary amenorrhea, on examination the
doctor see this picture, what is your diagnosis?
History primary amenorrhea, intermittent cyclical abdominal pain (dysmenorrhea),
difficulty with micturition and defecation, retention of urine in some cases.
Examination Normal stature and have normal secondary sexual characteristic,
abdominal mass, vulval inspection (tense bluish bulging membrane), rectal examination
(mass at the vagina).
Investigations US, Laparoscopy, Laparotomy.
Treatment After explanation of the condition and obtaining parents consent, a
cruciate incision (+) in the hymen allows drainage of the retained menstrual blood, also
give antibiotics. From medico-legal point of view, the girl must be given a report
confirm that the hymen was opened by surgical operation as treatment.
Abdominal mass with imperforate hymen
Observation of the introitus will display a tense bulging bluish
membrane which is the hymen.
Vaginal agenesis.
Not to be confused with imperforate hymen.
Diagram of hematometra and hematocolpos with imperforate
distal transverse vaginal septum.
Vaginal septum
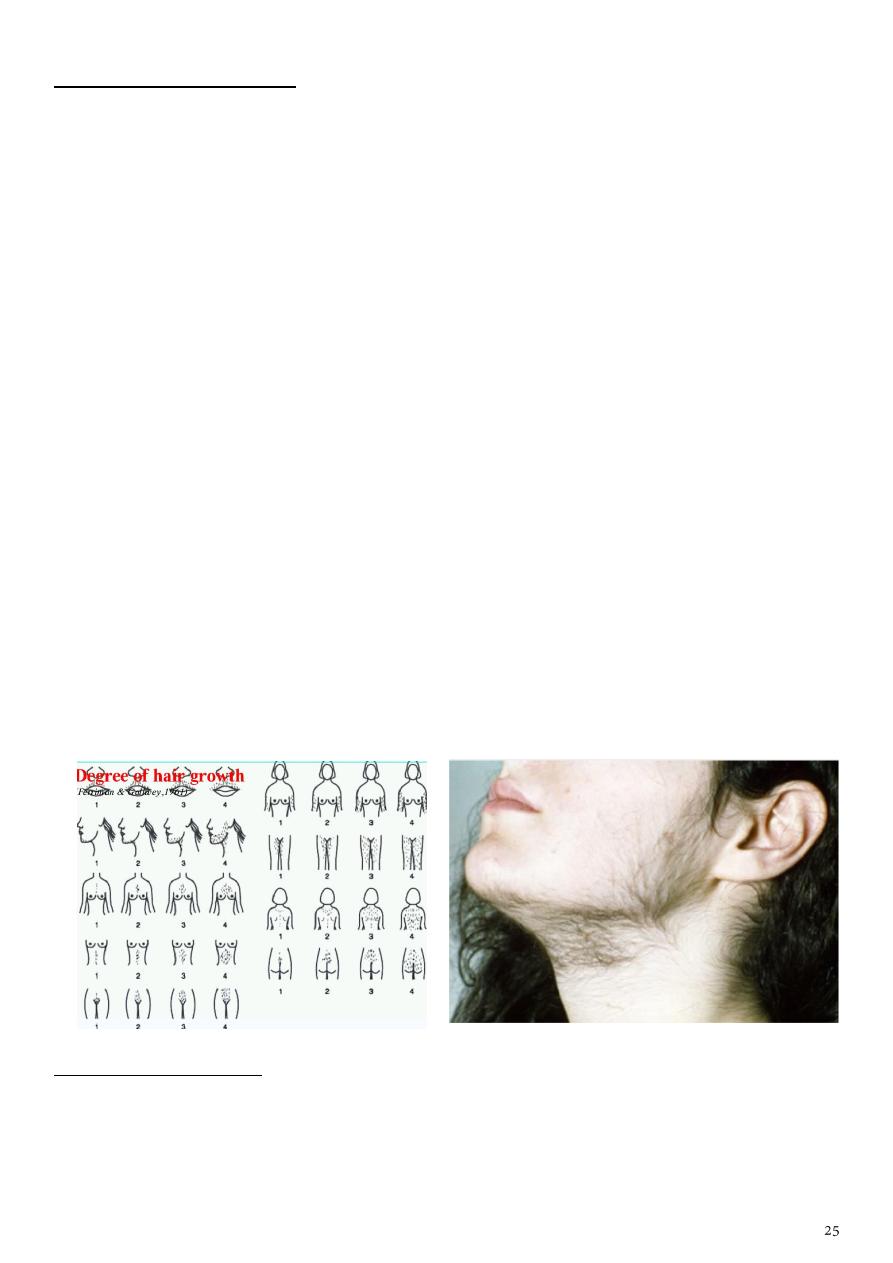
Subject3: Hirsutism
Definition: it is excessive growth of terminal (coarse) hair on the face, chest, back, inner
thigh in women following a male like patter.
Viriliaztion hirsutism + signs of androgen excess (acne, frontotemporal baldind,
deepening of the voice, a decrease in breast size, clitoral hypertrophy, increased
muscle mass, amenorrhea/oligomenorrhea.
Causes adrenal disorder (congenital or adult onset adrenal hyperplasia, adrenal
producing tumors), ovarian disorders (
PCOS
, androgen producing tumor, chronic
anovulation), pituitary disorders (cushing's syndrome, acromegaly), drugs (phenytoin),
intrinsic factors (genetic, racial, familial, idiopathic), intersex problem (turner's
syndrome).
Signs and symptoms male pattern of hair distribution, features of PCOS, thyroid
disease, Cushing syndrome, signs of virilization, signs of insulin resistance,
galactorrhea, pelvic mass.
Investigations free testosterone, 17 hydroxyprogesterone, LH:FSH ratio >3, 5a RA,
pelvic US, CT, MRI, Dexamethasone suppression test.
Treatment:
o General reassurance, stop smoking, weight reduction.
o Specific ovarian suppression (OCP), adrenal suppression (corticosteroids), anti-
androgens (spironolactone), 5aRA inhibitors (Finasteride), Insulin sensitizer
(Metformin).
o Local suppress hair growth, remove hair pigment, temporary depilation,
temporary epilation, permanent removal.
o Surgery.
Ferriman-Gallway score:
From 0 (no growth) to 4 (complete and heavy cover).
9 locations )upper lip, chin, chest, upper back, lower back, upper abdomen, lower
abdomen, upper arm, thigh).
In white races, a score of 8 and above is considered indicative of androgen excess.
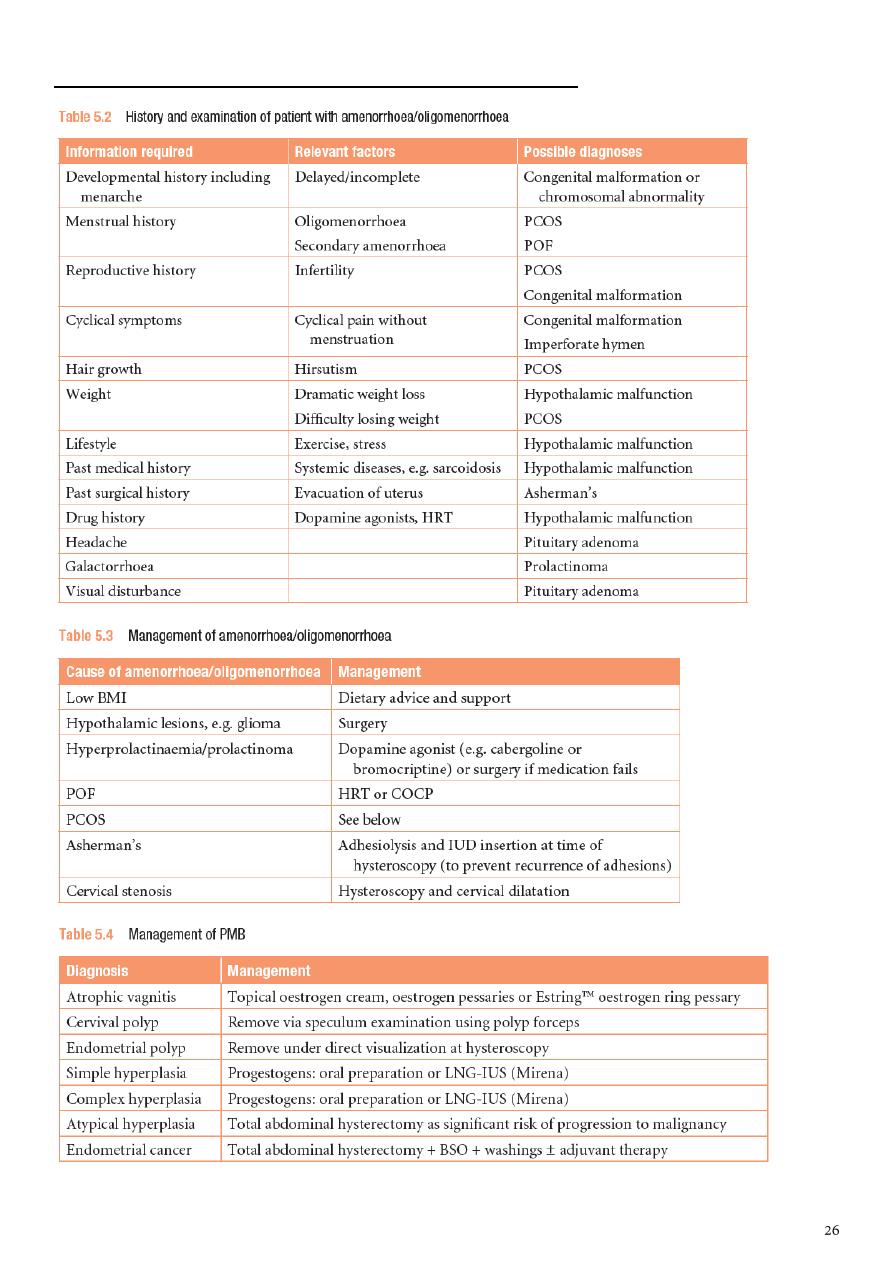
Subject4: Disorders of the menstrual cycle
Subject5: Genital infections
Disease
How you get it
Symptoms
Treatment
Partners
Diseases that are transmitted sexually
Chlamydia
Infection of mucous
membranes lining
the genitals can lead
to inflammatory
disease (PID) in
women and infertility
in men and women.
By having vaginal
or anal sex without
a condom with
someone who has
the infection; from
mother-to-baby
(eye and chest
infection)
Women often
have no
symptoms or may
have pain with
sexual
intercourse, lower
abdominal pain,
changes in
bleeding pattern.
Men may have no
symptoms or may
have watery or
thick discharge
from penis, pain or
urinating.
Antibiotics.
Recent sexual
partners need
treatment. Don't
have sex until 7
days after starting
treatment and until
sexual contacts
have been treated.
Gonorrhoea
Bacterial infection of
genitals, throat or
anus, can lead to
infertility
particularly in
women.
By having vaginal,
anal or oral sex
without a condom
with someone who
has the infection;
from mother-to-
baby (eye
infections).
Women usually
have no
symptoms, but
may have pain
with sex, vaginal
discharge, lower
abdominal pain.
Men may have no
symptoms or
discharge from
penis, discharge
from anus, pain in
testicles, pain on
urinating.
Antibiotics.
Sexual partners
must be tested and
treated if positive.
Avoid sex until
seven days after
treatment is
completed.
Condoms provide
some protection,
but not total.
Syphilis
Bacterial infection
entering the body
through breaks in
skin or linings of the
By having vaginal,
anal or oral sex
without a condom
with someone who
has the infection;
Painless ulcer
(chancre) usually
on genitals; later
Antibiotics with follow-
up blood tests.
Sexual partners
must be tested and
treated if positive.
Current health
regulations advise
Disease
How you get it
Symptoms
Treatment
Partners
genital area; over
time, goes on to
damage internal
organs (heart, brain,
spinal cord)
from mother-to-
baby across
placenta during
pregnancy
(congenital
syphilis).
swollen glands,
rash, hair loss.
no sex until you are
cleared.
Genital warts
Human
papillomavirus (HPV)
causes fleshy or flat
lumps
– may be
present even if not
visible
HPV transmitted by
direct skin-to-skin
contact, usually
during sex; from
mother-to-baby.
Sometimes no
identifiable source
of transmission.
Fleshy or flat
lumps on or
around genitals,
anus, groin or
thigh.
Visible warts can be
treated, but the
infection cannot be
cured. Discuss
vaccination with your
general practice.
Condoms provide
some protection,
but not total.
Genital herpes
Herpes simplex virus
causes skin infection
usually on mouth
and lips (cold sores)
or on genitals.
Close skin contact
with someone with
the virus; from
mother-to-baby.
Painful, red
blisters, little sores
or ulcers, flu-like
symptoms, and
sometimes a
discharge.
Anti-herpes drugs and
pain relief can be given
to treat symptoms, but
the infection cannot be
cured. Some may need
medication to prevent
further outbreaks.
Partners may or
may not catch
herpes. Do not
have sex when
open sores are
present. Condoms
provide some, but
not complete,
protection.
Non-specific
urethritis (NSU)
Infections that cause
inflammation of the
urethra.
Can be caused by
chlamydia or by
bacteria, viruses or
other organisms.
Women usually
have no
symptoms. Men
have discharge
from the penis,
pain on urinating,
but sometimes
there are no
symptoms.
Antibiotics.
Partners need to be
examined and
treated.
Disease
How you get it
Symptoms
Treatment
Partners
Trichomoniasis
Trichomonas
vaginalis
, a small
parasitic organism,
causes irritation in
the vagina in women
and can cause an
irritation inside the
penis in men.
During sexual
intercourse with an
infected person.
Women may have
no symptoms, but
there may be a
yellowy-green
frothy vaginal
discharge. Men
usually have no
symptoms.
Antibiotic tablets and/or
vaginal pessaries.
Treat with
antibiotics to avoid
re-infection. Don't
have sex until 7
days after starting
treatment and until
sexual contacts
have been treated.
Diseases that can be transmitted sexually or may be transmitted in other ways
Hepatitis A
Viral infection which
affects the liver.
Mainly through
contaminated food
or water or not
hand-washing after
toilet/before food
etc. Can be through
anal sex and oral-
to-anal contact
(rimming).
Often no
symptoms, or may
have mild flu-like
illness, or
vomiting,
abdominal pain,
dark urine and
yellowing of the
skin and whites of
the eyes.
Immunisation for
prevention. Good
hygiene and hand-
washing. Avoid alcohol
and drugs. Eat a well-
balanced low-fat diet.
Immunisation for
prevention and
avoid anal sexual
practices until
recovered.
Hepatitis B
Viral infection which
affects the liver.
By having vaginal,
anal or oral sex
without a condom
with someone who
has the infection;
form mother-to-
baby. By sharing
needles, syringes,
toothbrushes,
razors and
unsterilized
instruments that
pierce the skin.
Blood transfusion in
countries that do
May have no
symptoms or mild
flu-like illness or
vomiting,
abdominal pain,
dark urine and
yellowing of the
skin and whites of
the eyes.
Rest, exercise and
avoid alcohol, drugs
and smoking. Eat a
well-balanced low-fat
diet. Check any
prescribed or over-the-
counter medicines are
safe to take.
Always use a
condom if partner is
not immunised.
Protection is
offered to babies
on the
immunisation
schedule and to
children under 16
years. Free
immunisation is
available for
household and
sexual contacts.
Disease
How you get it
Symptoms
Treatment
Partners
not pre-test blood
for transfusion.
Hepatitis C
Viral infection which
affects the liver.
After contact with
infected blood or by
sharing needles or
syringes or possibly
through sexual
contact. Blood
transfusion in
countries that doe
no pre-test blood
for transfusion.
Often no
symptoms or may
have mild, flu-like
illness or vomiting,
abdominal pain,
dark urine and
yellowing of the
skin and whites of
the eyes.
Rest, exercise and
avoid alcohol, drugs
and smoking. Eat a
well-balanced low-fat
diet.
Sexual and needle-
sharing partners
can have a blood
test to check for
Hep C antibodies.
HIV
Human
Immunodeficiency
Virus
attacks the
white blood cells and
causes damage to
the immune system
so that it can be
difficult to fight off
infections.
HIV is transmitted
through blood,
semen and vaginal
fluids, sharing
needles and from
mother-to-baby.
Blood transfusion in
countries that do
not pre-test blood
for transfusion.
Usually no
obvious symptoms
for many years.
No immunisation or
cure available although
some secondary
infections can be
treated or prevented.
Keeping well for longer
is possible with good
care. Women with
HIV/AIDS need a
cervical smear yearly.
Practice safer sex
to prevent
transmission.
Partners should
ask for an HIV test.
Pelvic inflammatory
disease (PID)
An infection of the
womb and fallopian
tubes that can cause
infertility.
Usually by having
vaginal sex without
a condom with
someone who has
gonorrhoea or
chlamydia.
Pain during sex,
sore abdomen or
back, heavy,
irregular or painful
periods, spotting,
high temperature,
feeling sick;
sometimes no
symptoms.
Antibiotics and rest.
Need to check for
STIs and be treated
to avoid
reinfection. No sex
until treatment is
completed and until
sexual contacts
have been treated.
Pubic lice
– crabs
Small lice that live in
the pubic hair and
By close body
contact, usually
during sex with an
Intense itching in
the pubic area,
Special shampoo,
cream or spray applied
Treat partners of
the last 3 months in
Disease
How you get it
Symptoms
Treatment
Partners
cause irritation.
infected person.
Can be spread via
infected bedding
and clothing.
small nits (eggs)
on pubic hair.
to pubic area. Wash all
clothing and bed linen.
the same way at
the same time.
Scabies
Small mites that
burrow into the skin
cause irritation.
By close body
contact, sometimes
during sex. Can be
spread by sharing
clothes or bedding.
Itching, worse at
night, and a rash
on the body.
Special lotion, cream or
ointment. Wash all
clothing and bed linen.
Treat partners of
the last 3 months in
the same way at
the same time.
Infections that are not sexually transmitted but can affect the genital area
Thrush or
candidiasis
Irritation of mucous
membranes from a
yeast organism. It
can occur in or
around the vagina,
and on the tip of the
penis.
Yeast overgrowth
may occur when
antibiotics are
used, during
pregnancy, with
diabetes, or when
immunity is
lowered. It can
occur after sex, but
also without sex.
Women have
vaginal or vulval
itching and a thick,
whitish vaginal
discharge. Men
have itching and
may have a red
rash on the head
of the penis or a
discharge under
the foreskin.
Creams and pessaries
for local treatment.
Anti-fungal tablets may
be given in severe
cases. Salt water baths
for men are usually
effective.
Need treatment if
showing symptoms.
Cystitis
Bacteria cause
inflammation of the
bladder lining; can
spread to kidneys
and cause damage
to kidney function.
Bacteria from
around the anus
getting into the
urethra and
bladder, not
emptying the
bladder properly.
Much more
common in women
than men.
Burning sensation
when urinating,
needing to urinate
urgently and more
often than usual,
cloudy,
bloodstained or
smelly urine,
aching in lower
abdomen or back.
Antibiotics after urine
test if symptoms last
longer than a day, drink
plenty of water, use
pain relief and using
alkalisers, e.g. Ural,
Citravesent
Disease
How you get it
Symptoms
Treatment
Partners
Bacterial vaginosis
If the control of the
normal bacteria in a
healthy vagina fails,
an overgrowth of
certain bacteria can
occur. The
acid/alkaline balance
is upset and irritation
results.
It may be brought
on by anything that
changes the
balance in the
vagina, eg, new
sexual partners,
increased sexual
activity.
Greyish white,
smelly vaginal
discharge.
Oral tablets and/or
vaginal pessaries.
Amsel's criteria
for diagnosis of bacterial vaginosis in which at least three out of four
should be present and these are:
• Thin, gray, homogenous discharge.
• Clue cell on microscope (vaginal epithelial cells so heavily coated with bacteria that the
border is obscured).
• PH of vagina> 4.5 (usually between 4.7-5.7).
• The addition of KOH to the vaginal secretions (the “whiff” test) releases a fishy, amine
like odor.

Subject6: Fertility control and contraception
#The ideal contraceptive method should:
Highly effective
No side effects
Cheap
Rapidly reversible
Widespread availability
Acceptable to all cultures and religions
Easily distributed
Can be administrated by non- health care personnel.
#Combined oral contraceptive pills (COCP):
Once daily pill, easy to use, very high degree of protection
against pregnancy, with many other beneficial effects, it is
mainly used by young, healthy
Formulation Synthetic Estrogen (Ethinyl estradiol) +
Synthetic progestogens (norethindrone, levonorgestrel,
gestodene).
COCP contain 21 pills that contain the active ingredient, one pill to be taken daily,
followed by a 7 placebo pills.
Method of use The patient begins taking the pills on the first day of menstrual cycle
then in the next cycles they are administered in fifth day of the cycle and continue for
21 days, each day at the same time, then discontinued for 7 days to allow for
withdrawal bleeding that mimics the normal menstrual cycle which occur after 3-5 days
from stopping pills.
Mode of action centrally inhibition of ovulation, Peripheral effects (Making
endomtrium atrophic and hostile to an implanting embryo, altering cervical mucus to
prevent sperm ascending into the uterine cavity).
Absolute Contraindication Circulatory diseases (IHD, CVA, HT, arterial or venous
thrombosis), Acute or severe liver disease, Oestrogen-dependent neoplasms (breast
cancer), Breastfeeding <6 weeks post-partum, Smoking ≥15 cigarettes/day and age
≥35, Focal migraine.
Relative contraindications Generalized migraine, Long-term immobilization, •
Irregular vaglinal bleeding, Less severe risk factors for cardiovascular disease (obesity,
heavy smoking, diabetes).
Side effects Venous thromboembolism, Arterial disease (hypertention, myocardial
infarction and thrombotic stroke), Mortality, Carcinogenic effect (Breast cancer,
Cervical cancer, Liver cancer), CNS (Depression, Headaches, Loss of libido),
Gastrointestinal, Genitourinary system, Chloasma, Leg cramps.
If pills are missed Less than 12 hours late (Don't worry. Just take the delayed pill at
once, and further pills as usual), More than 12 hours late (Take the most recently
delayed pill now + Use extra precautions (condom, for instance) for the next 7 days).
Positive health benefits treat heavy or painful periods, improve premenstrual
syndrome(PMS), reduce the risk of pelvic inflammatory disease(PID), decreased
incidence of benign breast lump, decrease number of functional ovarian cyst, *less
endometriosis, against both ovarian and endometrial cancers, treatment for acne.
Important questions during history taking parity, family history, menstrual history,
any medical disease.
Causes of failure rate (get pregnant) in COCP missing pills, low dose of active
ingredient, irregular taking of pills or different time of administration, taking another
drug like ampicillin, gastroenteritis (defect in absorption).
#Combined oestrogen and progesterone vaginal ring:
It is soft ring that a woman can insert into vagina.
Women who use Ring leave the ring in place for 3 weeks during a month.
During the 4th week, the ring is removed for 7 days.
A new ring is used for each cycle.
#Combined hormonal patches:
Contain Oestrogen and progestogen
Patches are applied weekly for 3 weeks, after which there is a patch-free week.
Contraceptive patches have the same risks and benefits as COC.
They are relatively more expensive, may have better compliance.
#Progesterone only contraception:
Methods progestogen-only pill (mini-pill), subdermal
implant (Implanon), injectables, hormone-releasing
intrauterine system.
Mechanism of action central effects (inhibit ovulation)
peripheral effects (local effect on cervical mucus making it
hostile to ascending sperm, Local effect on the endometrium making it thin & atrophic
thereby preventing implantation, cause decreased tubal and endometrial motility).

Side effects Menstrual disturbances, Functional ovarian cyst, ectopic pregnancy.
Indications of Progestogen-only pills breastfeeding, older age, cardiovascular risk
factors, diabetes.
#Injectable progestogens (Depo-Provera):
Given by deep intramuscular injection.
Most women who use it develop very light or absent
menstruation.
Depo-Provera will improve PMS and can be used to treat
menstrual problems such as painful or heavy periods.
It is particularly useful for women who have difficulty
remembering to take a pill
Single IM injection every 3 months.
Side effects weight gain, delay in return of fertility, persistent menstrual irregularity,
irregular vaginal bleeding or amenorrhea, risk of osteoporosis.
Indications contraindication to estrogen, Following rubella vaccination in
puerperium, -Husband waiting for effect of vasectomy, Mental retarded women,
Breast-feeding, population control in developing countries.
#Subdermal implants
:
Implanon consists of a single silastic rod that is inserted
subdermally under local anaesthetic into the upper arm.
It releases the progestogen etonogestrel 25-70 Mg daily.
Norplant, which is withdrawn from the market It lasts for
3 years and thereafter can be easily removed or a further implant inserted.
Implanon is particularly useful for women who have difficulty remembering to take a
pill and who want highly effective long-term contraception.
There is a rapid return of fertility when it is removed.
It works for 1 year.
#Copper Intrauterine device:
Mechanism of action Induce inflammatory reaction
within the endometrium, toxic to the sperm and oocyte and
the embryo, interfere with the fertilization, interfere with
sperm motility and oocyte capability of fertilization and
implantation.
Complications Bleeding and pain, Infection(PID), Perforation, Expulsion, Intrauterine
pregnancy, Ectopic pregnancy.
Contraindications Nulliparity and infertility, Active infection, Uterine anomalies
increase risk of expulsion and perforation, gynecologic malignancy, genital bleeding of
unknown cause, gestational trophoblastic disease.
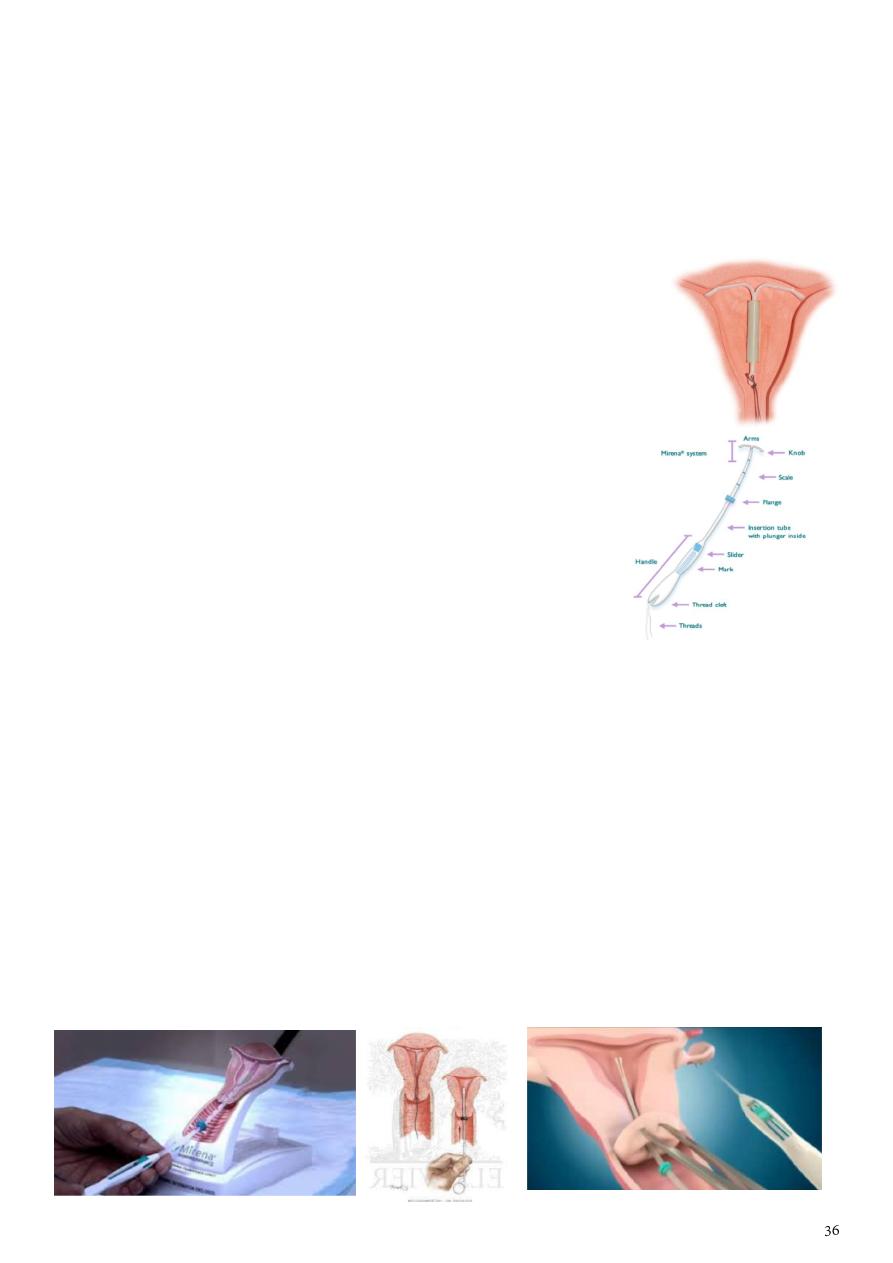
#Levonorgestrel releasing IUD "merina":
The LNG IUS is made of flexible plastic
Mechanism of action Thickens cervical mucus, Inhibits sperm
function in uterus, Reduces monthly growth of the lining of the
uterus, lessen menstrual blood loss in women who have heavy
menstrual flow.
What are the most common side effects of the LNG IUS?
o 10+ in every 100 women are likely to experience the
following Headache, Abdominal/ pelvic pain, Bleeding
changes, Vulvovaginitis, Genital discharge.
o 1 to 10 in every 100 women are likely to experience the
following Depression, Migraine, Nausea, Acne,
Hirsutism, Back pain.
Merina available, expensive, white color, larger, not
metallic.
Time of insertion of both types of IUD day 3-5 of the cycle because there is no
pregnancy and the cervix is patulous during this period.
#Method of insertion of ICD:
How to check that the device is in the uterus? Thread in place, by US.
Causes of thread not in place expulsion, perforation in myometrium, thread is coiled
in so you can localize it by examination or US or abdominal X-ray.
Complications at time of insertion infection, pain, bleeding, trauma (perforation).
Copper still for 5 years, Merina still for 10 years,
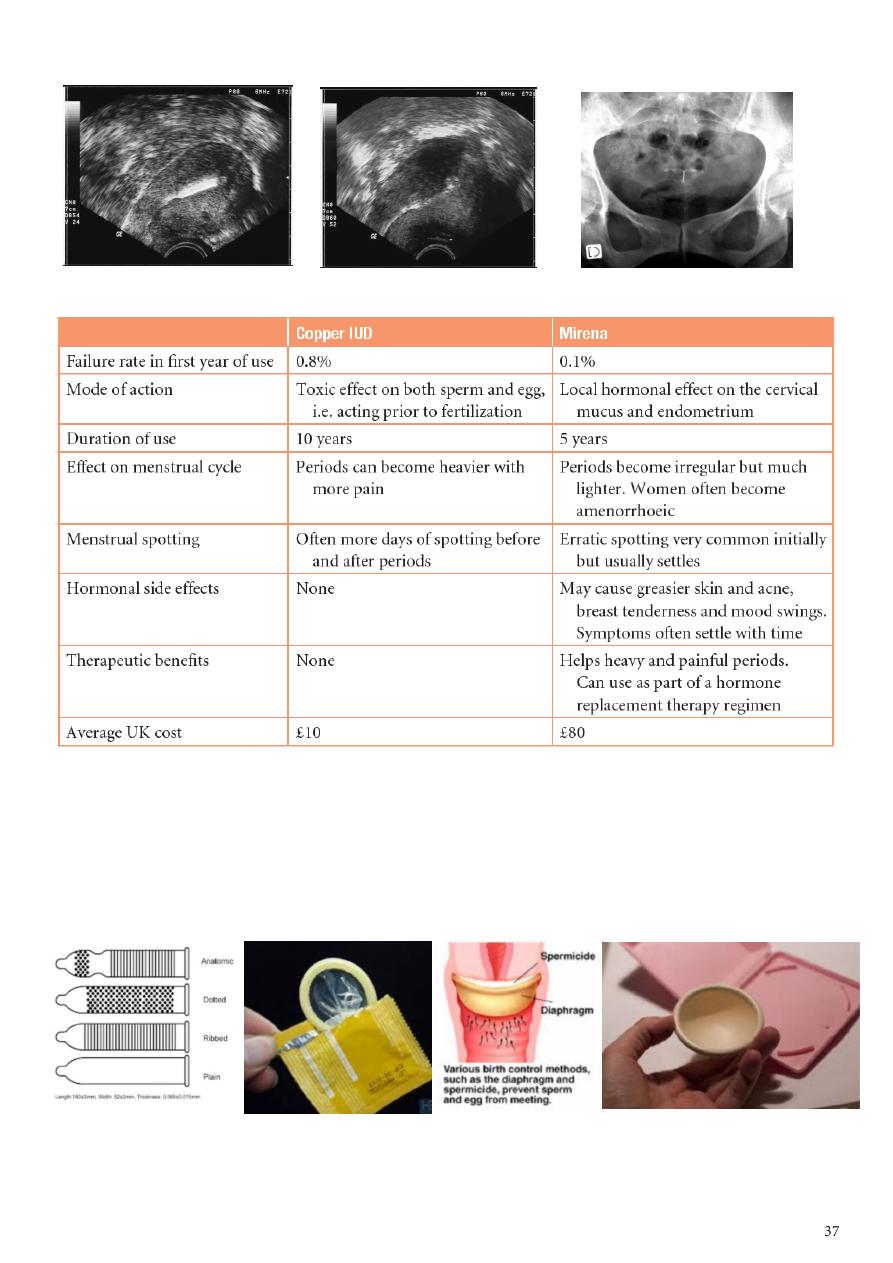
Copper IUD LNG IUD X ray with LNG IUD
#Mechanical contraception:
Male condom protective against STDs.
Female diaphragm application at cervix with spermicidal effect.
Complications allergy, rash, failure.
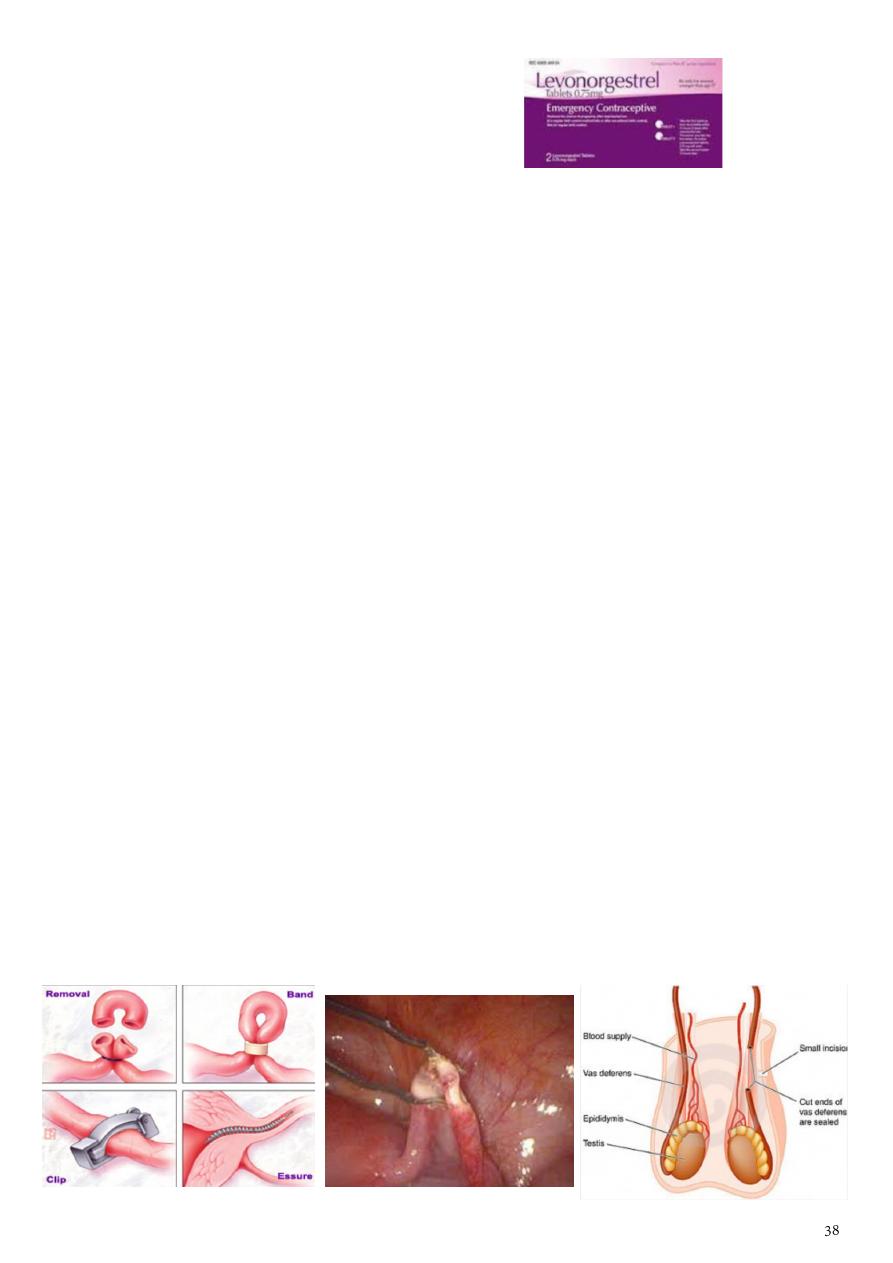
#Emergency contraception:
Levonorgestral 0.75 mg, take 2 tablets.
IUCD within 5 days of sexual intercourse.
#Natural family planning:
Avoid intercourse 5 days before and after ovulation.
To know the time of ovulation:
1- Temperature increase in ovulation, so calculate the body temperature every
morning for 3 months.
2- At time of ovulation there is localized abdominal pain and breast tenderness.
3- Spotting few drops of blood.
4- Cervical mucosa become thin and watery and colorless.
5- US size of mature follicles (18-20).
Other type called withdrawal no ejaculation in female genital tract.
#Permanent contraception:
Bilateral tubal ligation:
o Should ligate both uterine tubes.
o Types removal, clips, band, essure.
o Essure screw in the uterine tube lead to local inflammatory ration and block
the tube.
o If the female want to become pregnant again do IVF.
Bilateral male vasiectomy:
o Incision in the scrotum.
o Cut the vas deferens.
o The male become infertile after 3 months.
o Should do semen analysis for at least 3 times to confirm the success of the
operation.
Subject7: Infertility
Definition:
It is failure to get pregnant after 1-2 years with regular unprotected sexual activity.
Causes:
Ovulatory factor PCOS.
Tubal factor Obstruction.
Endometrial factor.
Unexplained.
Testicular factor.
History in female:
Age:
o Natural conception declines significantly in the female after 35 years of age. This is
due to the decline in oocyte quality and numbers.
o Ask about mirage before menarche.
History of getting pregnant before to know if it is primary or secondary infertility.
Duration of infertility to know the cause, to know if it is primary or secondary
infertility.
Body weight Over or under weight can affect ovulation (irregular cycle, PCOS);
women with a body mass index (BMI) of >29 or <19 will have difficulty conceiving.
Hair distribution Hirsutism (PCOS).
Body temperature elevated due to progesterone.
Menstrual cycle regular or irregular (indicate ovulatory cause), LMP, mid-cyclic pain.
Gynecological history pap smear, ectopic, PCOS, inter-menstrual bleeding.
Type of contraception Injectable (lead to increase period of non-pregnant), IUCD
(infection), OCCP (can get pregnant early).
Occupational hazards exposure to chemicals and radiation adversely affects male and
female fertility.
Smoking reduces fertility in females and semen quality in males.
Alcohol excessive alcohol is harmful to the fetus, and can also affect sperm quality.
Drugs:
o Non-steroidal anti-inflammatory drugs (inhibit ovulation).
o Chemotherapy (destroys rapidly dividing cells e.g. gametes).
o Cimetidine, sulphasalazine, androgen injections (affects sperm quality).
Sexual history:

o Coital frequency stress and anxiety may affect libido and coital frequency and
thus impact on fertility. Recommended coital frequency is two to three times per
week.
o Post-coital bleeding.
o Sexual transmitted diseases (STDs).
Medical history chronic diseases, IBD.
Surgical history appendectomy could lead to adhesion of the uterine tube, trauma
like car accident.
Family history infertility, PCOS, congenital abnormalities.
History in male:
Age fertile up to 80 years.
Number of wives.
Occupation radiation, excessive heat, away from house.
History of illegal relationships STDs lead to tubal diseases.
Medical history trauma, DM, hypertension.
Surgical history hydrocele, torsion.
History of undescended testes or mumps.
Drugs that lead to impotence.
Examination:
General examination weight, hirsutism, vital sings, sign of any medical diseases
(thyroid, DM, autoimmune diseases).
Abdominal examination striae (indicate previous pregnancy), mass (ovarian or
fibroid), scar, hair distribution.
Genital examination abnormal discharge, pus.
Bi-valve speculum excoriation, redness, ulcer, erosions, abnormal discharge, high
vaginal swap, endo-cervical swap.
Digital examination (bi-pelvic examination) uterus (size, shape, mobility, consistency),
cervix (mass, ectopic, infection, movement lead to severe pain = cervical excitation
test), fornex (feel the adenxae -ovary and tube- normally not palpable).
Examination in male:
o General examination sign of any medical diseases.
o Local examination of the genitalia.
Investigations:
Ultrasound in regular cycle do US before day 14 (in day 12 or 13) to see the follicles
before rapture // By US see ovarian cyst, size of ovaries in mid-cyclic time, rapture of the
follicles.
Hormonal assay LH and FSH (do at day 2 or 3 -this is baseline-), do Prolactin test at
any time (irregular cycle, unovulatory cycle), Progesterone (do it at the end of the cycle
at day 22 in the mid-luteal phase, high level of progesterone confirm the presence of
corpus luteum).
Laparoscope diagnostic and therapeutic, see endometriosis or tubal adhesion.
hHistosalpingography inject radiopaque dye then take x-ray, normally see white tube
with spillage at the end of the tube>
For ovary cause do US and hormonal assay.
For tubal cause do laparoscope and histosalpingography (filling defect, obstruction,
other diseases).
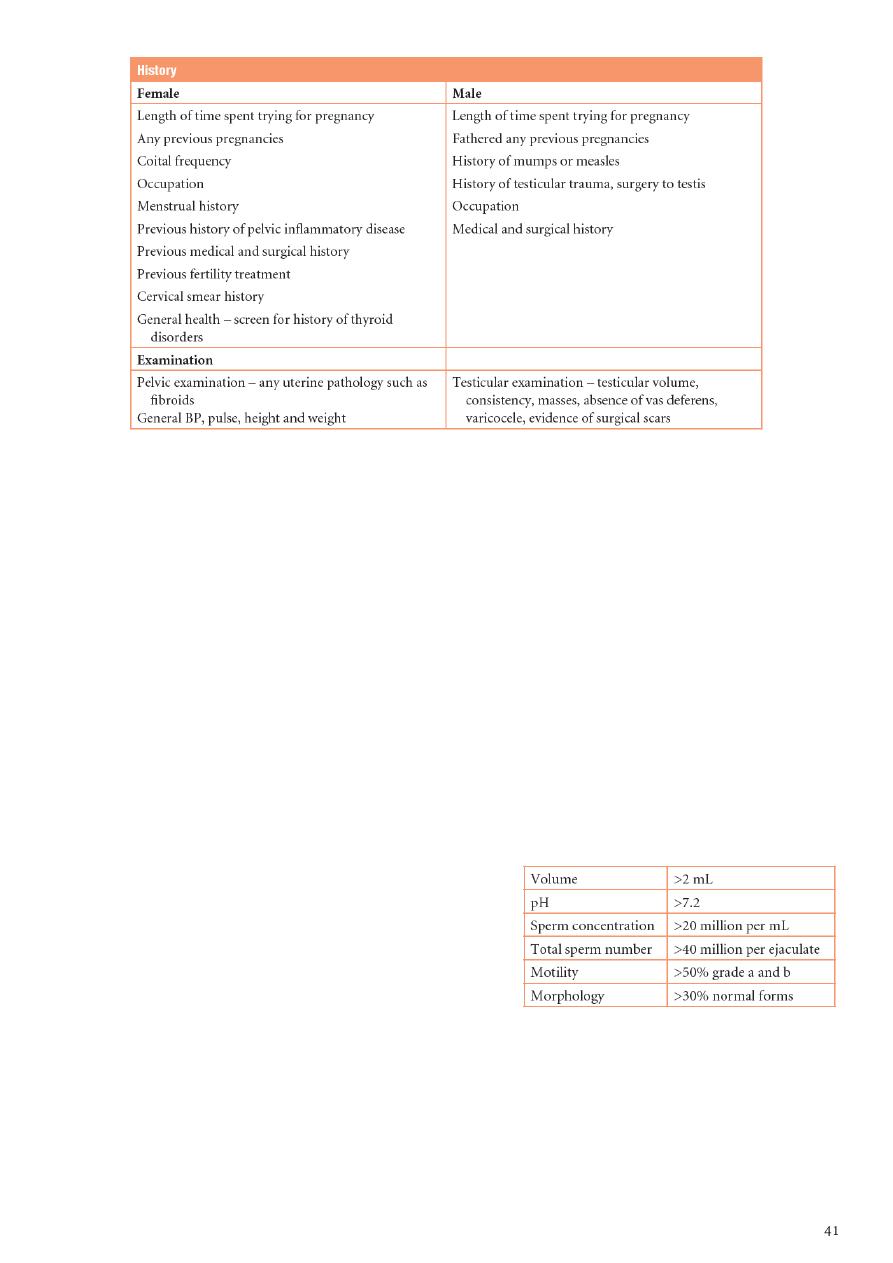
In male seminal analysis see this table
about normal parameters for semen analysis
according to WHO criteria.
Treatment:
If there is ovulatory cause stimulate the ovulation by clomiphene citrate give it at
day2 of the cycle and continue for 5 days, start by low dose, follow up by US.
If the cause is ovulatory use pregnin lead to LH surge, called ابرة مفجرة, lead to
rapture of follicles, give it when follicles are well-developed, its action begin after 48
hours.
Life style modification nutrition, weight, exercise.
Subject8: Fibroid
Information:
A fibroid is a benign tumor of uterine smooth muscle, termed a ‘leiomyoma’.
2 of 10 females have fibroid.
The gross appearance is of a firm, whorled tumor.
The typical whorled appearance may be altered following degeneration; three forms of
which are recognized: red, hyaline and cystic.
Fibroids are estrogen dependent.
Risk factors for clinically significant fibroids nulliparity, obesity, a positive family
history, African racial origin (three times higher risk).
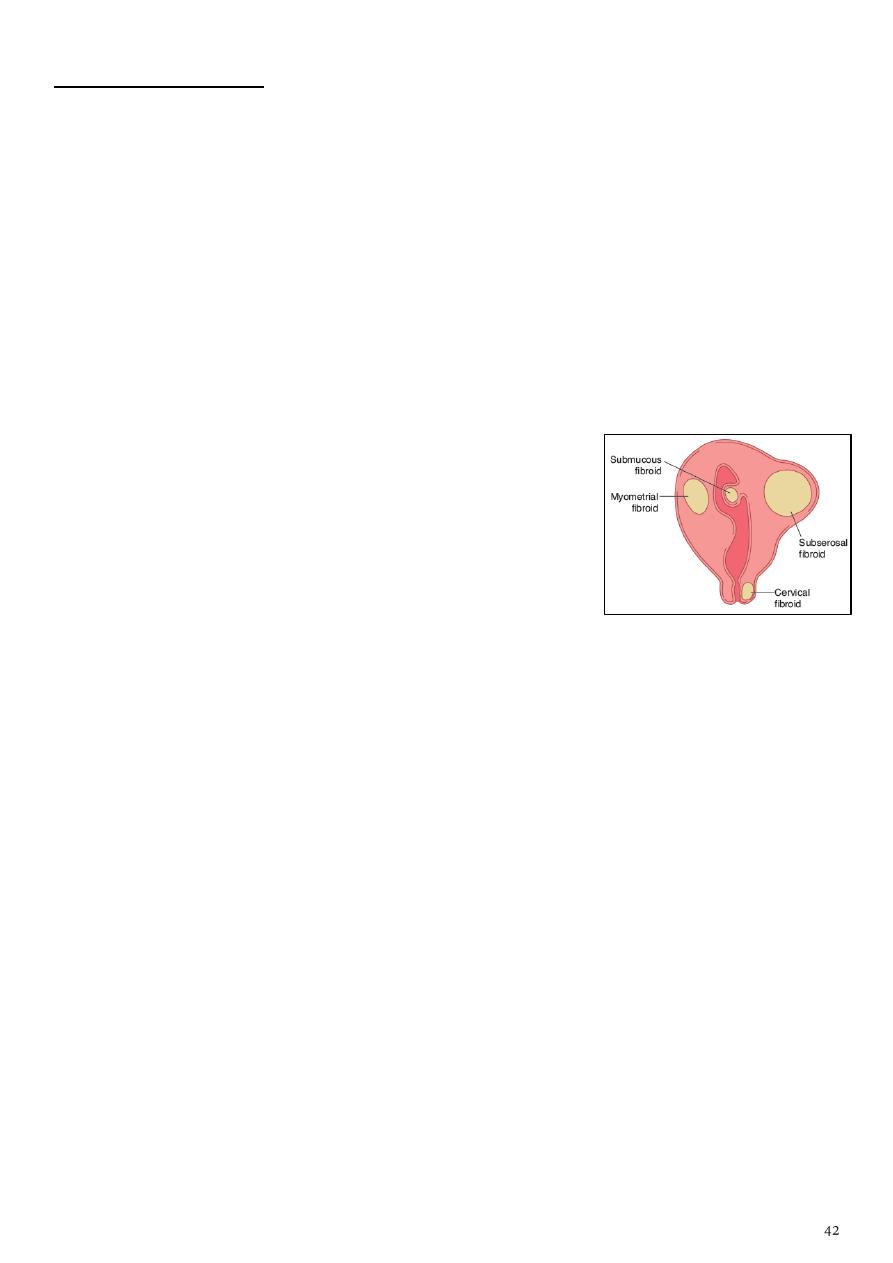
Types:
Submucous fibroid Located adjacent to and bulging into
the endometrial cavity.
Intramural fibroid Located centrally within the
myometrium.
Subserosal fibroid Located at the outer border of the
myometrium.
Pedunculated fibroid Attached to the uterus by a
narrow pedicle containing blood vessels.
Cervical fibroids arise from the cervix.
History:
In non-pregnant women:
Asymptomatic when the fibroid is small.
History of abnormal vaginal bleeding like menorrhagia, inter-menstrual bleeding (if
pediculated), dysmenorrhea.
Vaginal discharge if infected.
Pressure symptoms pressure on bladder lead to frequency, retention of urine /
pressure on the veins lead to varicose veins / pressure on genitalia lead to prolapse.
Subfertility may result from mechanical distortion or occlusion of the Fallopian tubes.
Anemia (if there is vaginal bleeding).
Polycythemia (if there is pressure on the broad ligaments).
In pregnancy:
Could lead to abortion.
Pre-term labor.
Placental abruption.
Mal-position, mal-presentation.
Obstructed labor.
Post-partum hemorrhage due to inefficient uterine contraction.
Pain due to complications like red-degeneration.
Examination:
Abdominal mass by bi-manual examination (adnexa examination if mobile it is
ovarian mass – if fixed to the uterus it is fibroid).
Different by pregnancy there is fundal height like pregnancy but there is no fetal
heart (fetal heart = double maternal pulse).
Investigations:
Hemoglobin concentration will help to indicate
anemia if there is clinically significant
menorrhagia.
Ultrasonography is the mainstay of diagnosis to
distinguish between a fibroid and an ovarian
mass.
In the presence of large fibroids,
ultrasonography is helpful to exclude
hydronephrosis from pressure on the ureters.
Treatment:
Conservative management is appropriate where asymptomatic fibroids are detected
incidentally.
The main types of medical treatment for heavy menstrual bleeding (tranexemic acid,
mefenamic acid, combined oral contraceptive pill) tend to be ineffective.
The only effective medical treatment is to use gonadotrophin releasing hormone (GnRH)
agonists.
Mifepristone (an antiprogestogen) has been shown to be effective in shrinking fibroids
at a low dose, but is currently not available for use as it causes endometrial hyperplasia.
Menorrhagia associated with a submucous fibroid or fibroid polyp should be treated by
hysteroscopic removal.
Where a bulky fibroid uterus causes pressure symptoms, the options are myomectomy
with uterine conservation, or hysterectomy.
Myomectomy will be the preferred option where preservation of fertility is required.
Uterine artery embolization (UAE) is a newer technique performed by interventional
radiologists.
Hysterectomy and myomectomy can be facilitated by GnRH agonist pretreatment over a
three-month period to reduce the bulk and vascularity of the fibroids.
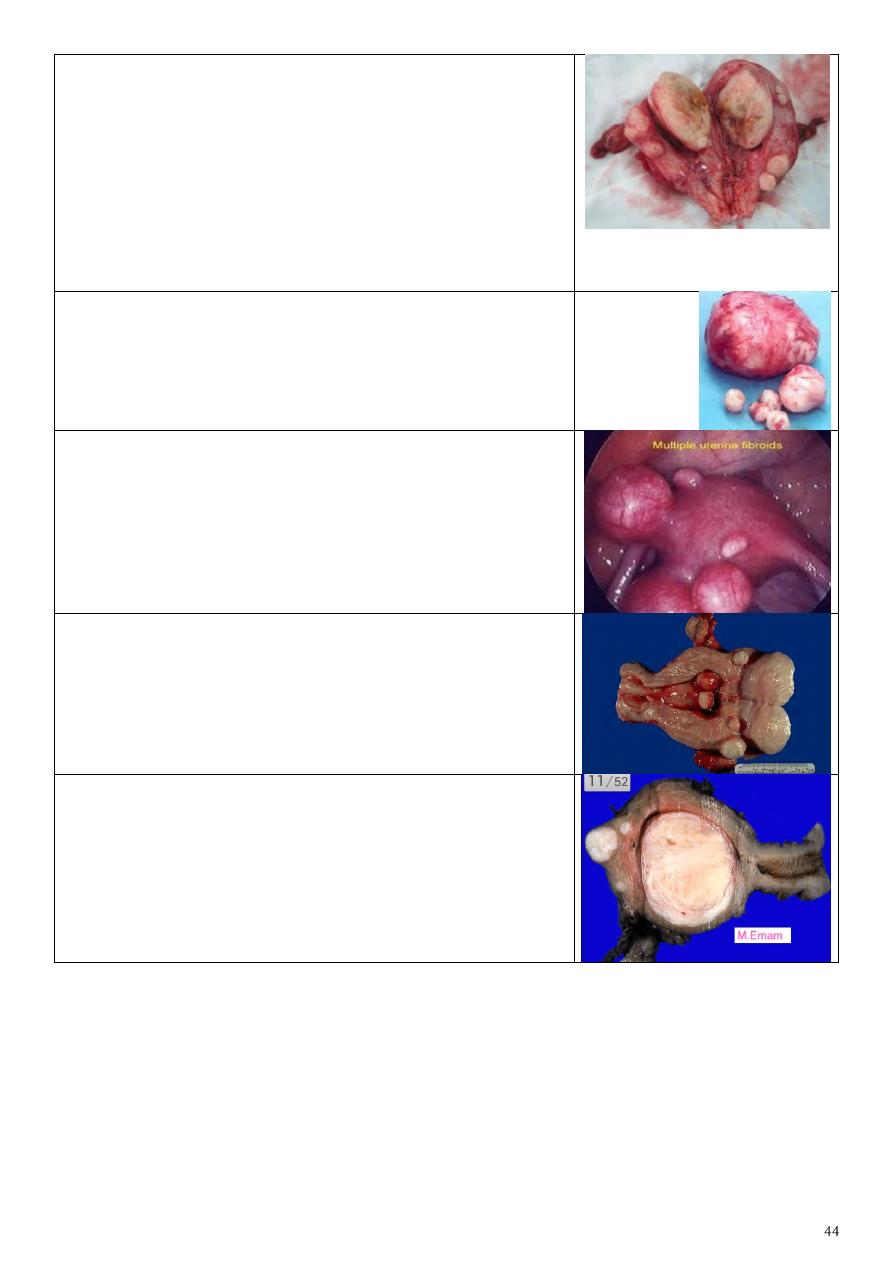
Description White yellow, no blood inside, round,
regular, different in size.
Types of fibroid that interfere with pregnancy
submucus, intrameural.
Symptoms vaginal bleeding, infertility, spontaneous
abortion, pain, pressure effect.
Treatment hysterectomy, myomectomy.
Treatment depend on type of fibroid, number of
fibroid, symptoms, patient wish, family number.
Multiple fibroid of different size.
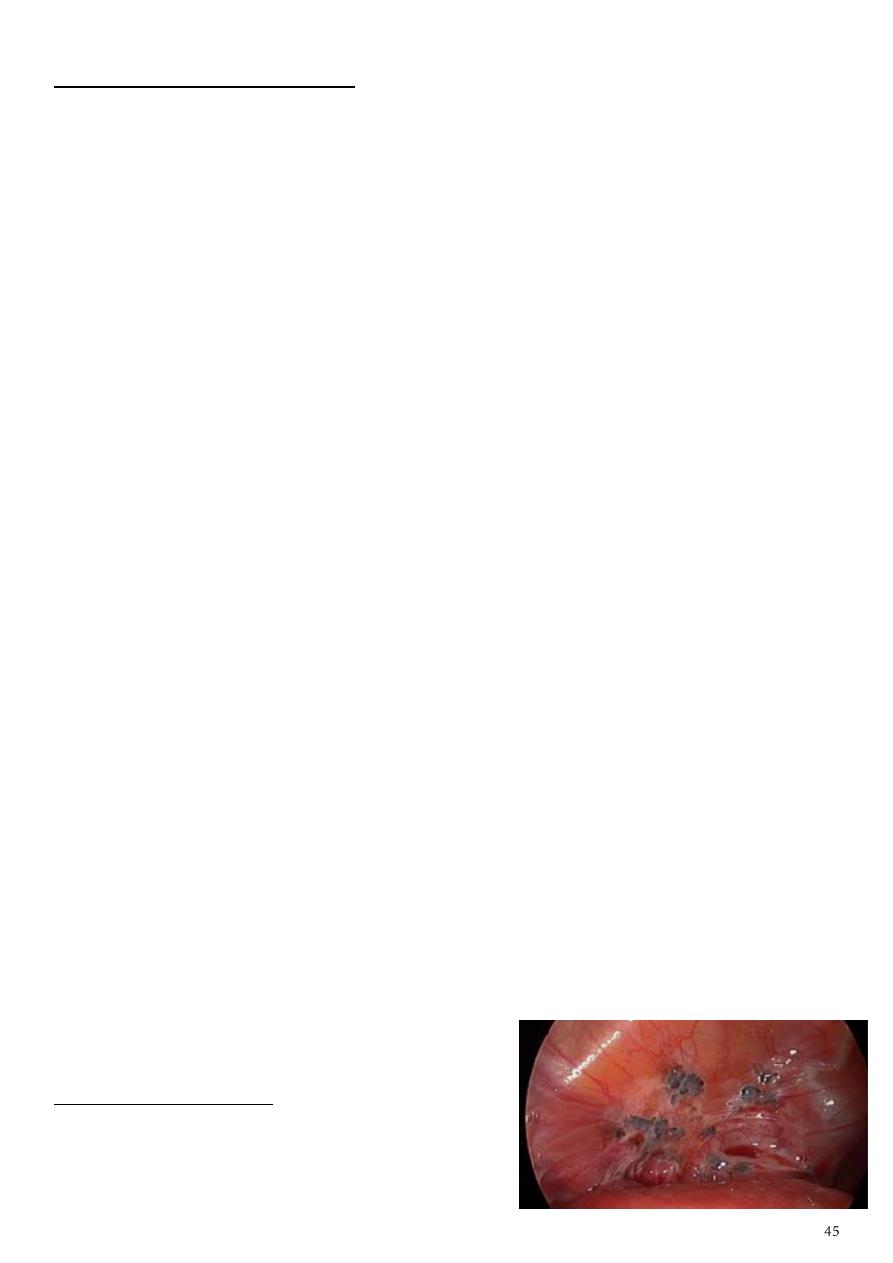
Laparoscopy showing multiple fibroids.
Multiple – round – regular outline – from uterus.
Big submucus fibroid – lead to infertility.
Small subserous, intramural.
Tx: by myomectomy.
Subject9: Endometriosis
Endometriosis is the presence of endometrial-like tissue outside the uterine cavity,
which induces a chronic inflammatory reaction. It can occur in various pelvic sites such
as on the ovaries, fallopian tubes, vagina, cervix, or uterosacral ligaments or in the
rectovaginal septum.
It can also occur in distant sites including laparotomy scars, pleura, lung, diaphragm,
kidney, spleen, gall bladder, nasal mucosa, spinal canal, stomach, and breast.
Symptoms Dysmenorrhea, Heavy or irregular bleeding, Pelvic pain, Lower abdominal
or back pain, infertility, Dyschezia, Bloating, nausea, vomiting, Inguinal pain, Pain on
micturition and/or urinary frequency, Pain during exercise.
Physical examination nonspecific pelvic tenderness, Ovarian involvement may
present with adnexal tenderness or masses, fixed uterine retroversion.
Risk factors Family history of endometriosis, Early age of menarche, Short menstrual
cycles (<27 d), Long duration of menstrual flow (>7 d), Heavy bleeding during menses,
Inverse relationship to parity, Delayed childbearing, Defects in the uterus or fallopian
tubes, Hypoxia and iron deficiency may contribute to the early onset of endometriosis.
Investigation Laparoscopy with biopsy is the only definitive way to diagnose
endometriosis.
Differential diagnosis Chronic salpingo-oopheritis, Ovarian cyst, malignant ovarian
tumours, Small myoma, Acute abdomen.
Medical treatment NSAID, Oral contraceptive pills, Danazol, Gestrinone,
Progestagens, Gonadotrophine releasing hormone agonists.
Surgical treatment conservative surgery (LASER, Co2 diathermy, Drainage of
endometriotic cyst), Definitive surgery (TAH + BSO).
Adenomyosis:
It is a disorder in which endometrial glands are found deep within the myometrium.
Patients are usually multioparous, in their late thirties or early forties.
Present usually with severe congestive dysmenorrhoea menorrhagia.
On examination the uterus is bulky, tender.
USS: altered ecchogenisity in myometrium, similar to uterine fibroid.
Treatment: danazole, GnRHa.
TAH.
Question form the doctor Patient presented with
irregular bleeding, dyspareunia, on examination she
had a fixed extroverted uterus:
Dx: endometriosis.
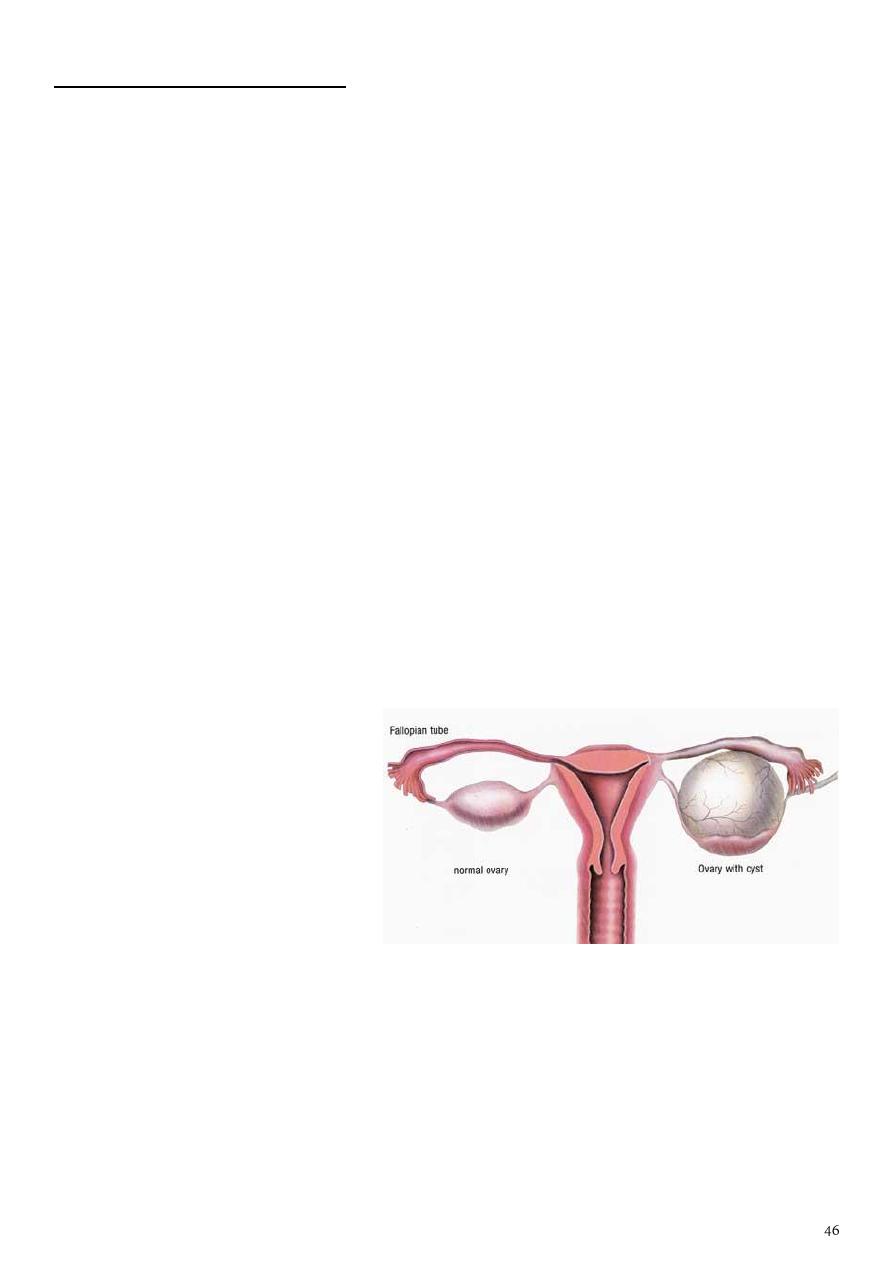
Subject10: Ovarian cyst
Types:
1- Benign (95%):
Could be pre-menopausal or post-menopausal.
Follicles not raptured then increase or decrease in size and called graafian follicular cyst,
and it is contain fluid.
Rapture of the follicles lead to corpus luteal cyst, it contain fluid, this cyst can disappear
in the next few cycles.
Hemorrhagic cyst which contain blood.
2- Malignant: like ovarian carcinoma.
3- Pathological: like polycystic ovarian syndrome (PCO).
Clinical manifestations of benign cyst:
Small cyst is asymptomatic.
Gradual abdominal distention.
Lower abdominal pain.
Irregular cycles (due to hormonal disturbances).
Breast tenderness (due to hormonal disturbances).
Frequency.
Altered bowel habits.
Hirsutism.
Easily fatigability.
Weight gain.
Examination:
1- General examination.
2- Vital signs.
3- Pelvic examination: fullness of the fornices.
4- Abdominal examination:
Inspection: distention, dilated veins, hair, striae.
Palpation: small cyst is not palpable, large cyst like mass and it is big and regular.
Percussion and Auscultation.
Investigations:
Hb level differentiate between cyst and cancer (which lead to anemia).
Blood group and Rh.
Ultrasound of the abdomen ultrasound features of the benign cyst are: regular
outline, smooth, no sepitation, no nucleation, no hemorrhage, no calcifications, thin
wall, contain homogenous radiolucent fluid.
CT / MRI MRI is better because this cyst is soft mass.
Hormonal investigations LH and FSH level.
Cancer markers CA-125.
Treatment:
Less than 3 cm resolve spontaneously during 2-3 months (cycles).
Persistent for 2-3 months use combined oral contraceptive pills (COCP) which reduce
the breast tenderness and suppress the ovulation so decrease the number of follicles
and cysts.
Cyst with symptoms like pain, give pain killer and COCP.
Large symptomatic cyst surgical removal by laparotomy and take biopsy to exclude
malignancy.
Malignant cyst surgery with radiotherapy or chemotherapy.
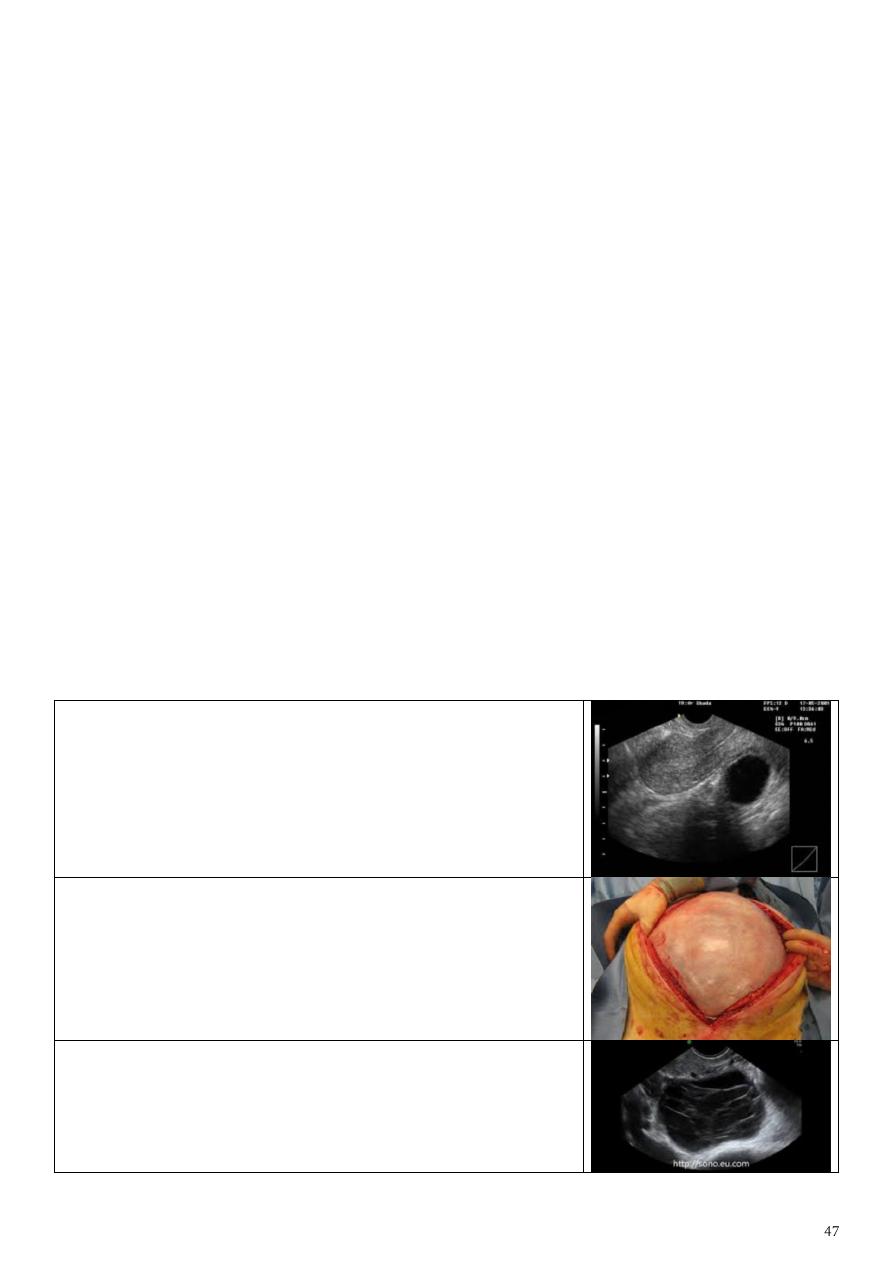
US sound of uterus:
Thickness of endometrium = 3-4 mm.
Regular, thin wall.
Single echogenicity.
No blood inside, only fluid.
Dx simple ovarian cyst.
Huge simple ovarian cyst.
Cancer not reach this size.
Cyst:
Multilocular, thick wall, sometimes bleeding inside.
Could be cancer.

Subject11: Polycystic Ovarian Syndrome (PCOS)
Introduction:
PCOS is a syndrome of ovarian dysfunction along with the cardinal features of
hyperandrogenism and polycystic ovary morphology.
The etiology of PCOS is not completely clear, but there is often a family history. It seems
likely that a gene is important in its development.
Proliferative phase of the cycle follicles increase in size to become mature (16-18
mm) under the effect of FSH.
LH lead to rapture of follicles give oocyte + follicular fluid.
Follicular fluid could lead to peritoneal irritation and presented as mid-cyclic pain.
In PCOS follicles not reach maturity (biggest follicle is less than 8 mm) so it lead to un-
ovulatory cycle and infertility.
PCOS follicles doesn’t contain ova or oocyte so discover it surgically or during IVF (in
vitro fertilization).
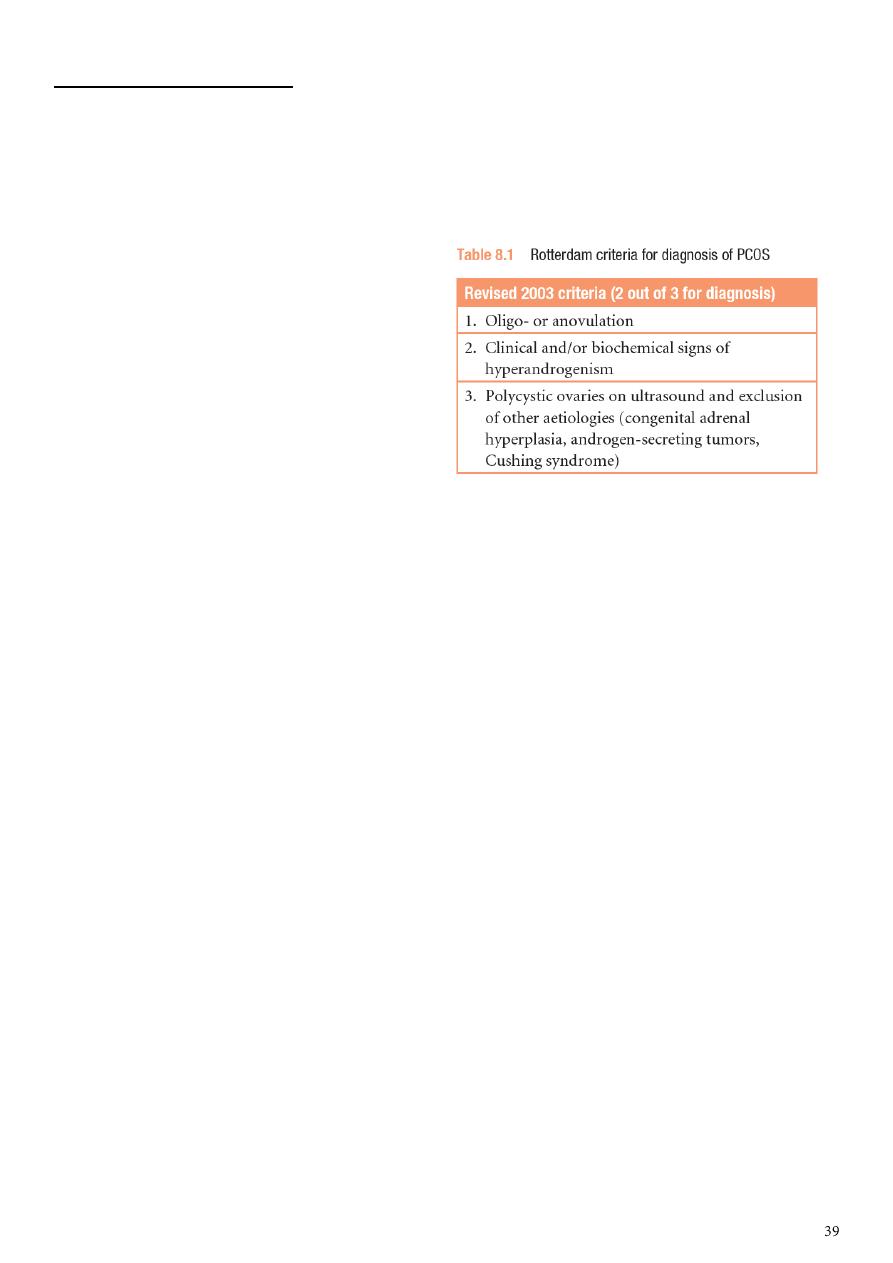
Diagnosis of PCOS:
Patients must have two out of the three features below:
1- Clinical features:
May be asymptomatic.
Endocrine and metabolic symptoms could lead to D.M.
Menstrual abnormality oligomenorrhoea, amenorrhoea,
Hirsutism and acne and balding.
Subfertility in up to 75 per cent of women.
Weight gain and Obesity.
Recurrent miscarriage.
Acanthosis nigricans areas of increased velvety skin pigmentation occur in the axillae
and other flexures.
2- Biochemical features:
Increased free testosterone.
LH/FSH more than 3 (reversed ratio).
Increase insulin (impaired glucose tolerance).
Decrease level of sex hormone binding globulin.
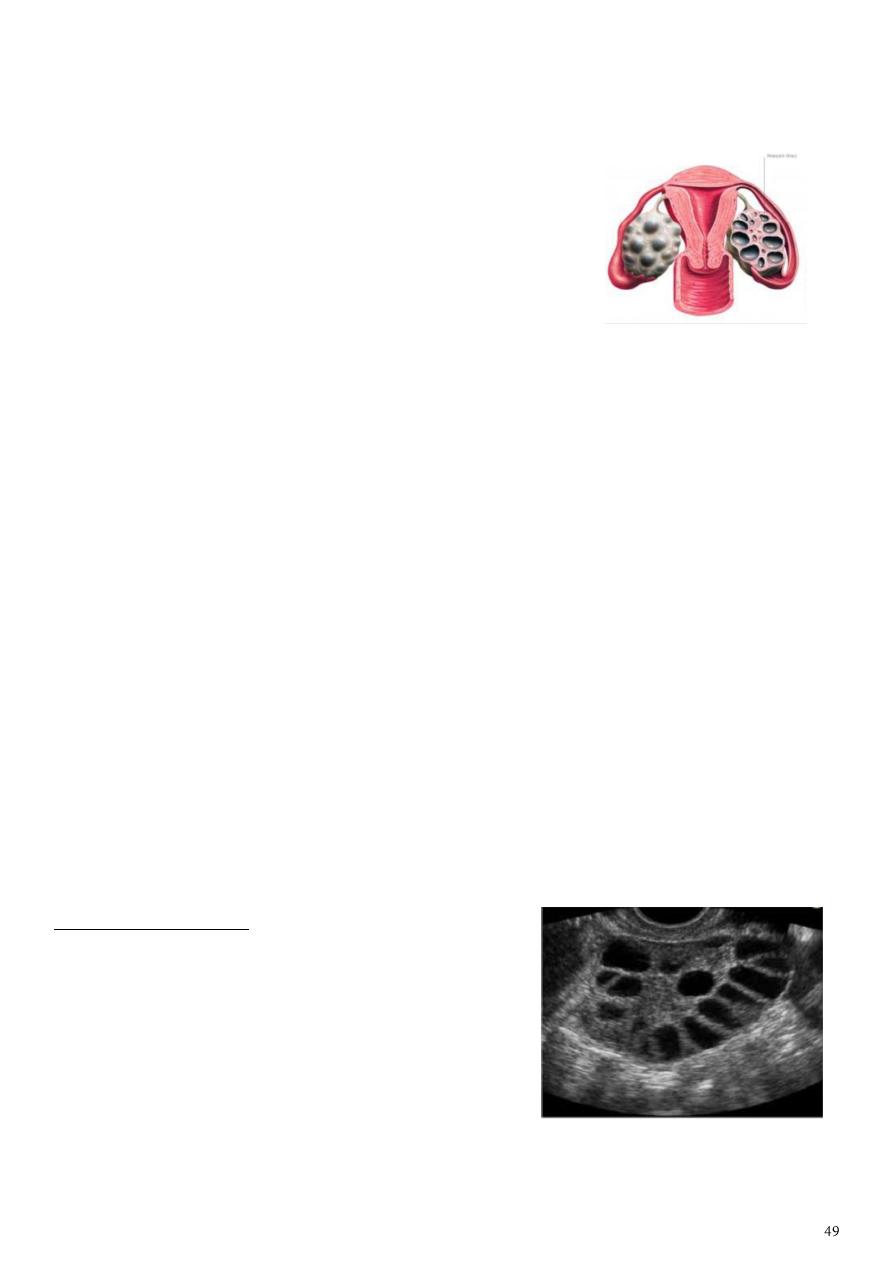
3- Image features:
Ultrasound more than 10 hypoechoic follicles, each measure 6-8 mm in diameter,
with or without increase ovarian volume.
Laparoscopy big size ovary, could be bilateral.
Investigation:
Investigate for same hormones mentioned above.
Glucose tolerance test.
Imaging study.
Treatment:
1- Education of patient.
2- Conservative:
Contraception: give OCCP.
Metformin: for D.M.
Weight reduction: to reduce to peripheral conversion in adipose tissue decrease
androgen can lead to increase size of follicles Pregnancy can occur.
3- Medication:
Symptomatic relieve by anti-androgens.
Ovulation induction (to get pregnant) by giving clomifine citrate 50-150 mg/day, start
from mid of the cycle and still for 5 days. // side effect of ovulation induction is OHSS
"ovarian hyper-stimulation syndrome" which need hospital admission.
Note: give OCCP rest the ovary for 3 months then do ovulation induction.
4- Surgery:
Cut part of the ovary wedge resection.
IVF remove all follicles then make IVF and give fixator.
=============================================
Question form doctor:
Patient presented with irregular bleeding and have this
sonography:
Sonography: bliateral ovaries contain more than 10
follicles each measure 2-5 mm arranged in necklace
apperance, and there is increased ovarian stroma
with or without increased of ovarian volume more
than 10 cm3.
Diagnosis: polycyctic ovarian syndome.
Other symotms: hirsutism, obesity, acne.
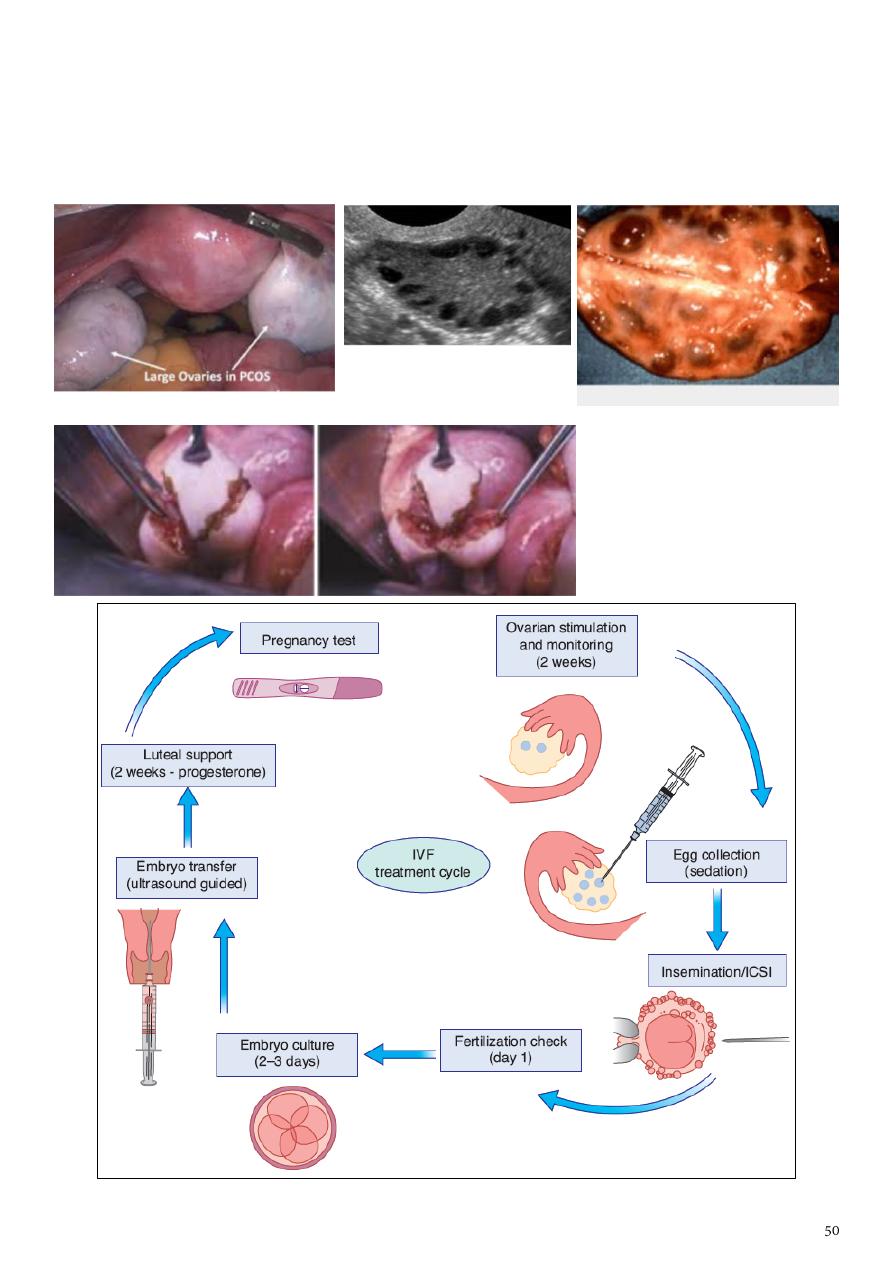
Other menstural abnormality: oligomenorrhea or amenorrhea.
Investigations: Increased free testosterone, LH/FSH more than 3 (reversed ratio),
Increase insulin (impaired glucose tolerance), Decrease level of sex hormone binding
globulin.
Treatment: medical (COCP, ovulation induction), surgical, weight reduction.
What is this procedure :
wedge resection part of
surgical tx in case of PCOS
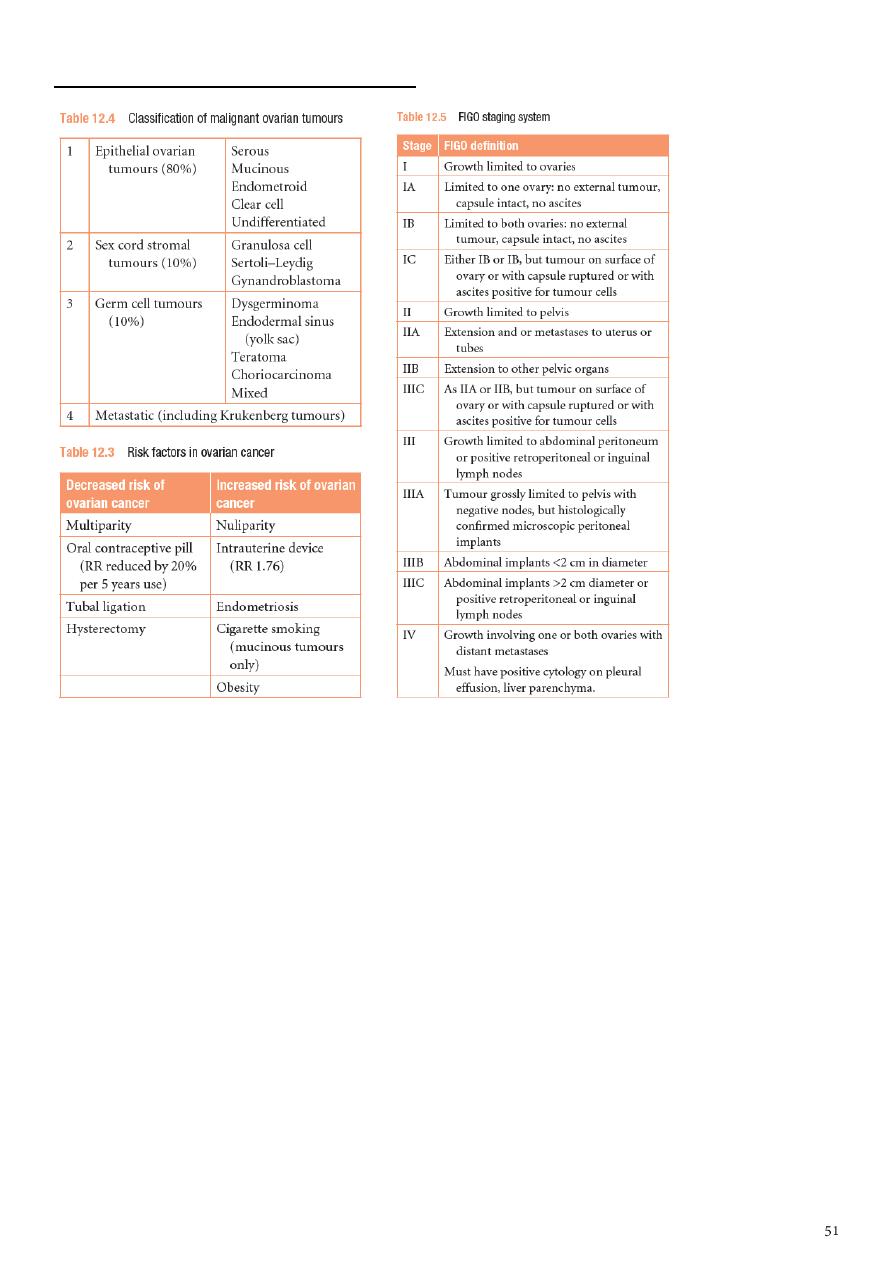
Subject12: Ovarian neoplasia
Investigations:
TVS –masses and mass characteristics
Tumor markers – CA-125, LPA (plasmalysophosphatidic acid)
CT – assess spread to LN, pelvic and abdominal structures
MRI – best for distinguishing malignant from benign tumors
Symptoms:
Functioning tumors.
Nonfunctioning tumors swelling, pressure symptoms, pain, menstrual disturbances,
ovarian cachexia
The following suggest malignancy:
age: mostly postmenopausal

pain: chronic and persistent
rapid course
bilaterality
Solidity ( variegated consistency )
fixity
metastases :nodules in DP, lymph nodes
ascitis
edema LL
cachexia
Treatment:
Depends on Staging, Tumor type, Age, Desire for future fertility
Complete surgery: TAH/BSO + omentectomy + lymphadenectomy:
o other cases of stage Ia
Conservative surgery: unilateral adnexectomy indicated:
o stage Ia: intact capsule, negative peritoneal washing, free omentum,
o well differentiated T,
o young patient with low parity
o Stage Ib,c
Cytoreductive surgery: TAH/BSO + omentectomy + lymphadenectomy + may be bowel
resection & anastomosis:
o for all other stages
Chemotherapy.
Radiotherapy.
Subject13: Endometrial carcinoma
Risk factors for Endometrial Cancer:
high levels of estrogen
endometrial hyperplasia
obesity
hypertension
polycystic ovary syndrome[citation needed]
nulliparity (never having carried a pregnancy)
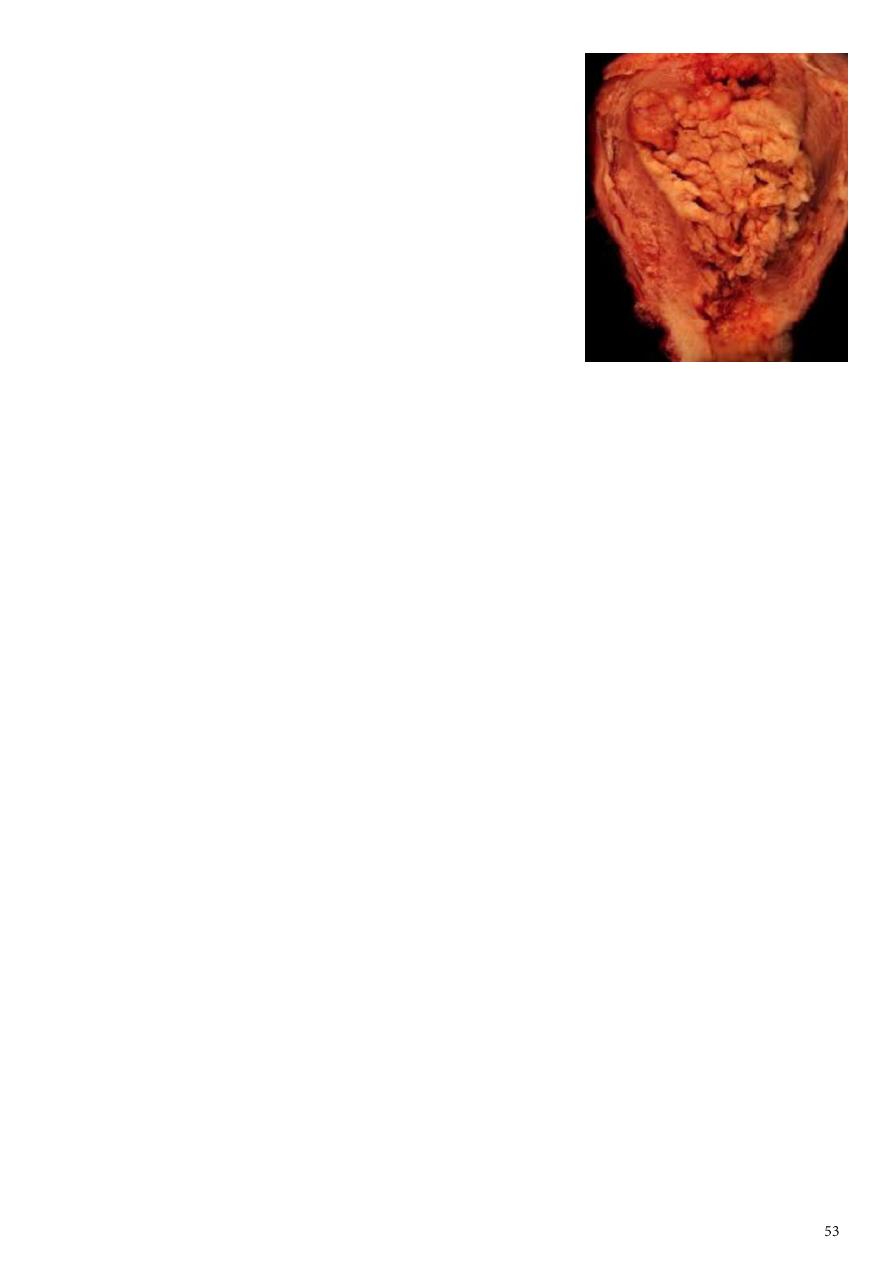
infertility (inability to become pregnant)
early menarche (onset of menstruation)
late menopause (cessation of menstruation)
endometrial polyps or other benign growths of the
uterine lining
diabetes
Tamoxifen
high intake of animal fat[citation needed]
pelvic radiation therapy
breast cancer
ovarian cancer
heavy daily alcohol consumption (possibly a risk factor)
Factors reduce risk of endometrial carcinoma
:
Oral contraception.
Progestogens.
Smoking.
Clinical presentation
Post-menopausal bleeding, Intermenstrual bleeding,
menorrhagia, Watery or purulent vaginal discharge (blood stained), Pain, Abnormal
screening test.
Pap smear, Endometrial curettage, dilation and curettage (D&C),
Hysteroscopy, Endometrial biopsy or aspiration, Transvaginal ultrasound,
Sonohysterography, Pipelle biopsy curettage, TruTest, Magnetic resonance imaging (MRI).
Spread Patterns
Direct extension, Transtubal, Lymphatic, Hematogenous (Lung most
common, Liver, brain, bone)
Treatment:
Stage IB or less: total hyst/BSO/PPALND, cytology
Stage IC to IIB: total hyst/BSO/PPALND, cytology, adjuvant pelvic XRT
Stage III: total hyst/BSO/PPALND, cytology, adjuvant chemotherapy
Stage IV: palliative XRT and chemotherapy

Subject14: Premalignant condition of the cervix
Screening for cervical intraepithelial neoplasia (CIN):
Medical screening method
o Detect premalignant and malignant processes of cervix.
o Prevent progression of abnormal cells to cancer.
o This is NOT a diagnostic test!
Cervical cancer screening with cytology provides the opportunity for early effective
intervention and has reduced morbidity and mortality
Papanicolaou
Cervicoscopey
Visual inspection with acetic acid (VIA)
Visual inspection with acetic acid and magnification (VIAM).
Colposcopy
Cervicography
Automated pap smears
Molecular (HPV/DNA) tests.
Co-testing using the combination of cytology plus HPV DNA testing is an appropriate
screening test for women older than 30 years (applied in some places).
Papanicolaou (Pap) smear test:
Is a screening test for asymptomatic Women to detect treatable pre-invasive squamous
abnormalities of the Cervix
Not diagnostic-rather screening test to detect early changes on the cervix.
It is a simple and painless test that may cause minor discomfort.
Cervical Smear aims to prevent cancer, not to detect cancer.
Cervical cancer screening should begin at age 21 years and not before age 21 because it
may lead to unnecessary and harmful evaluation and treatment in women at very low
risk of cancer.
Women who have been immunized against HPV-16 and HPV-18 should be screened by
the same regimen as non-immunized women because it doesn’t prevent against all
high risk HPV viral type.
Frequency of cervical cytology screening:
Annual cervical cytology screening is recommended for women aged 21–29 years.
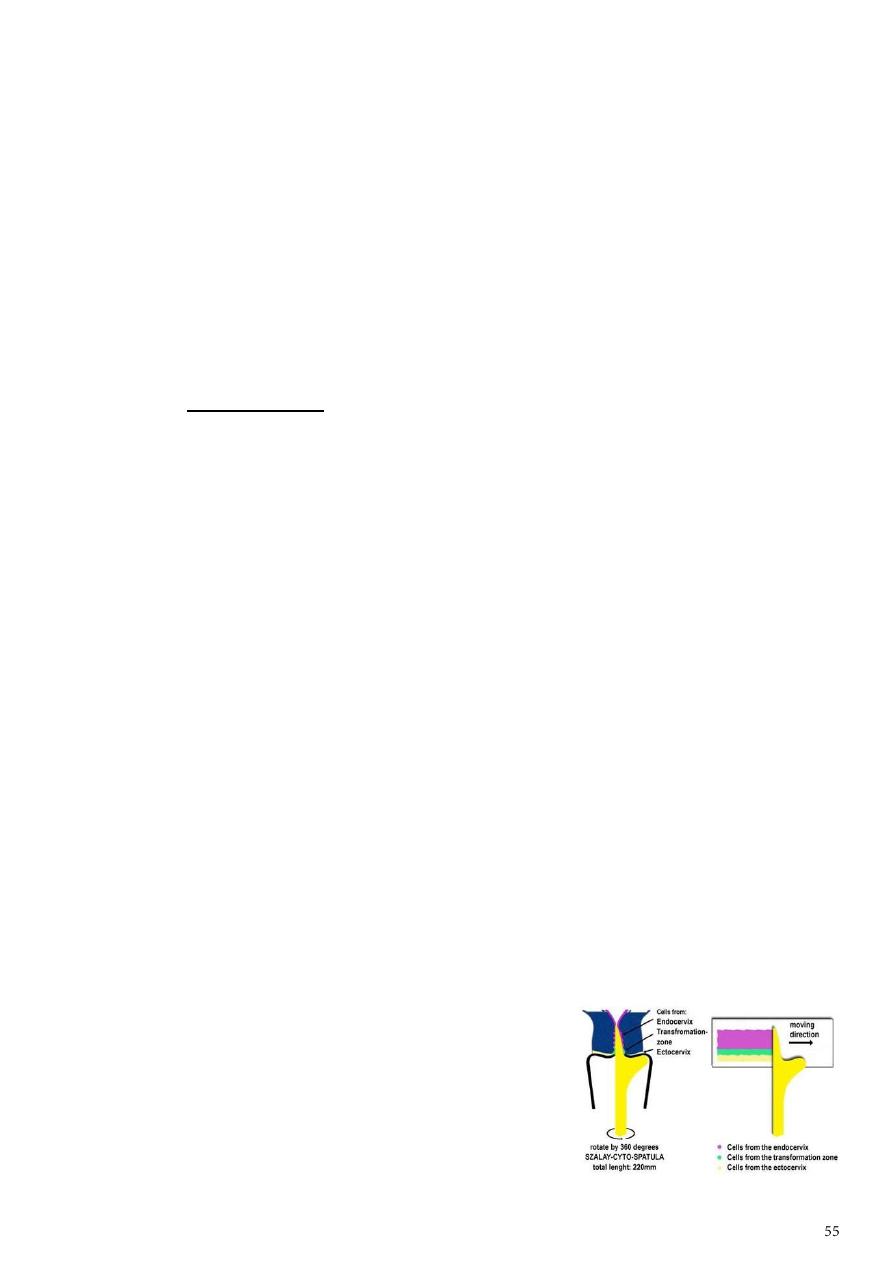
Women aged 30 years and older who have had three consecutive cervical cytology test
results that are negative for intraepithelial lesions and malignancy may be screened
every 2-3 years.
women with any of the following risk factors may still require more frequent cervical
cytology screening:
o Women who are infected with human immunodeficiency virus (HIV)
o Women who are immunosuppressed (such as those who have renal transplants).
o Women who were exposed to diethylstilbestrol in utero.
o Women previously treated for CIN 2, CIN 3, or cancer (continue to have annual
screening for at least 20 years).
Pap Smear is not necessary in women in these categories:
Virgin patient.
Total Hysterectomy for benign disease.
Recent result of pap smear.
Age over 65 and over 10 benign Pap Smears.
Preparation:
To prepare for the Pap test, for two days before the test ,women should avoid:
o Vaginal Douching .
o Using tampons.
o sexual intercourse.
o Using birth control foams, creams, or jellies or vaginal medications or creams.
The ideal time for a woman to have a Pap Smear is five days after her menstrual period
has ended.
Exfoliated cells are collected from the transformation zone of the cervix by Use spatula
of different size or brush.
There are two methods of preparing and processing cervical smear slides:
1. Conventional cervical (Pap) smear test:
Collecting the cells smears on a microscope slide and
applies a fixative.
The slide is sent to a laboratory for evaluation.
The Spatula with the optimal shape and size is
chosen.
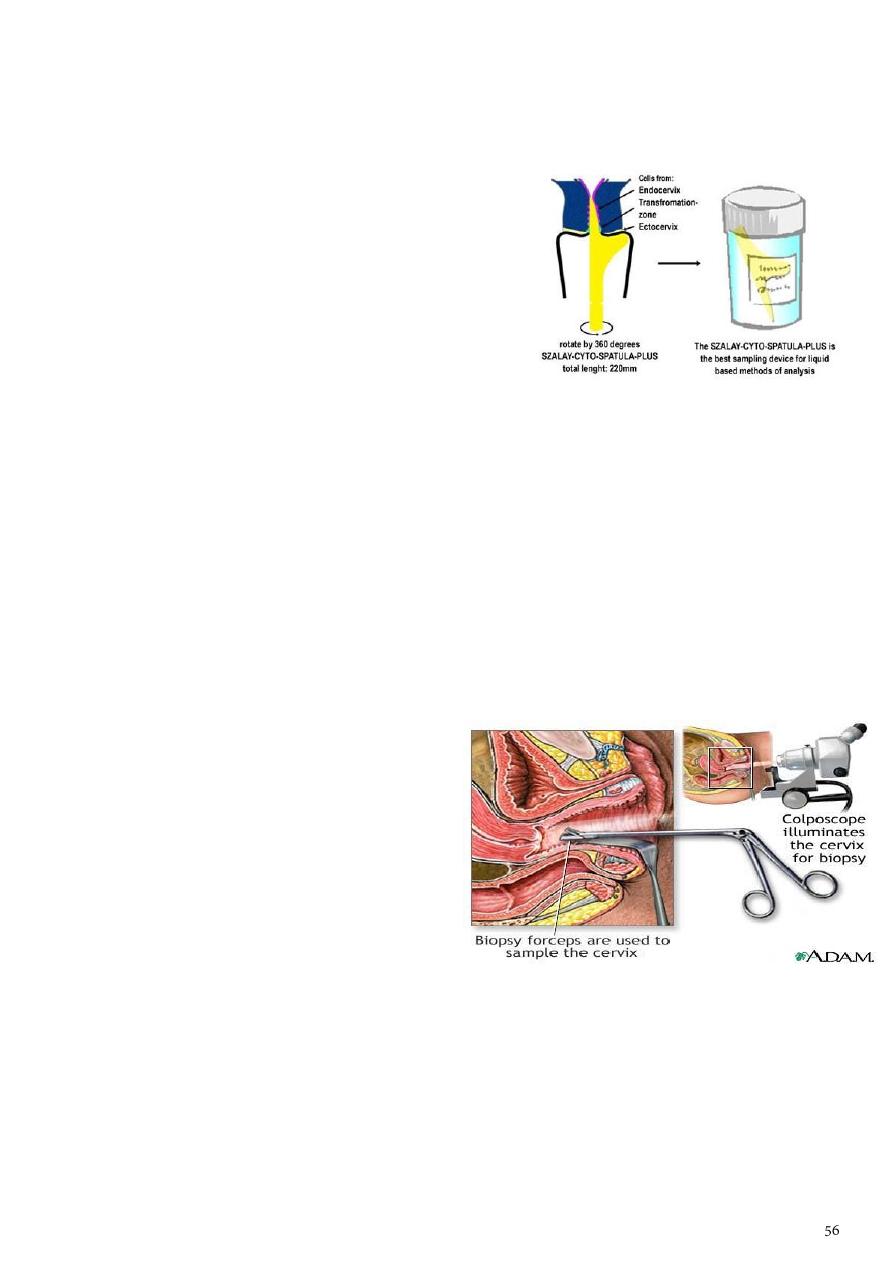
The 'tongue' of the spatula is introduced into the canal, whilst its 'shoulder' is
positioned on the 3 o'clock position of the ectocervix at the beginning of the
procedure . With gentle pressure the spatula is rotated in a clockwise direction.
2. Liquid based cytology (LBC) test.
Cell transferred to a vial of liquid preservative
that is processed in the laboratory to produce a
slide for interpretation by light microscopy.
Classification of CIN:
CIN classification
CIN 1 (mild dysplasia) involvement of the inner one-third of the epithelium.
CIN 2 (moderate dysplasia) involvement of inner one-half to two-third
CIN 3 (severe dysplasia/carcinoma in situ) full thickness involvement.
Or can be classified as:
Low grade lesions (CIN1 and HPV-associated changes) in which there is a significant
chance of regression and low progressive potential.
High grade lesions (CIN 2 and CIN 3) are likely to behave as cancer precursors.
Colposcopy:
It is a binocular operating microscope
with magnification of 5-20 times.
Indicated for further investigation of
smear abnormalities.
It has been used to examine the cervix in
detail to:
*Identify dysplastic abnormalities on the ectocervix.
*Detect changes in the cellular pattern and vascularity of the covering epithelium.
*Allow the accurate localization of the abnormal epithelium.
*Exclude an invasive process.
Methods:
*Saline method.
*Classical or extended method.
*Iodine test.
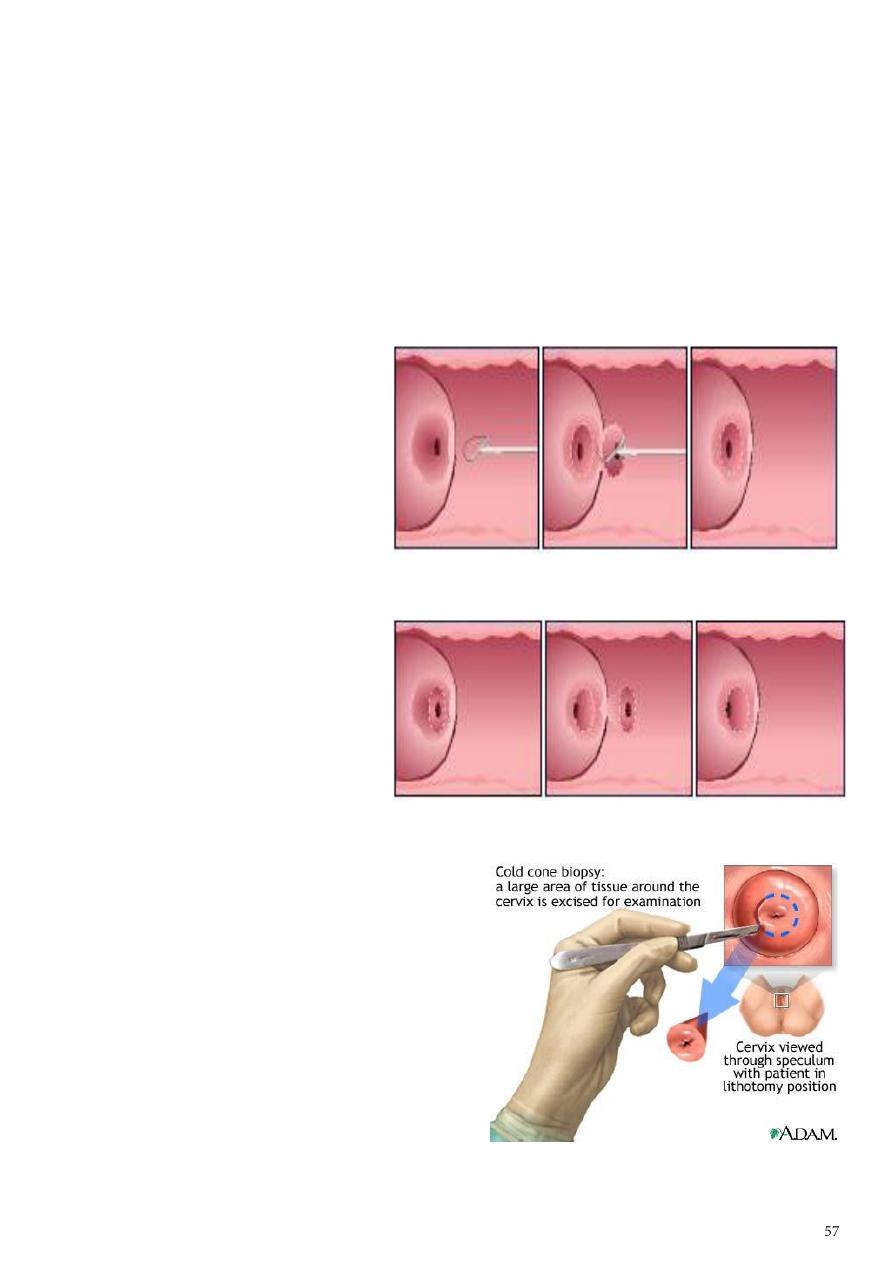
Treatment of CIN:
Destroying the abnormal epithelium (cryosurgery, laser vaporization).
Excisional techniques:
a. local excision
b. loop electrode excision procedure (LEEP).
c. cone biopsy.
d. trachelectomy (excision of cervix).
e. hysterectomy.
LEEP (loop electrosurgical
excision procedure(: After
freezing the area with local
anesthetic, an electrical wire
loop is inserted into the vagina
and all the abnormal tissue is
removed. This procedure is also
done in the physician's office.
A cone biopsy: refers to
removal of a cone-shaped
piece of tissue. The tissue
removed provides a more
extensive sample for diagnosis
than a simple biopsy. A cone
biopsy is usually done in the
operating room.
The cold cone biopsy is a surgical
procedure requiring general anesthesia
and is indicated by the presence of
precancerous changes in the cervix .
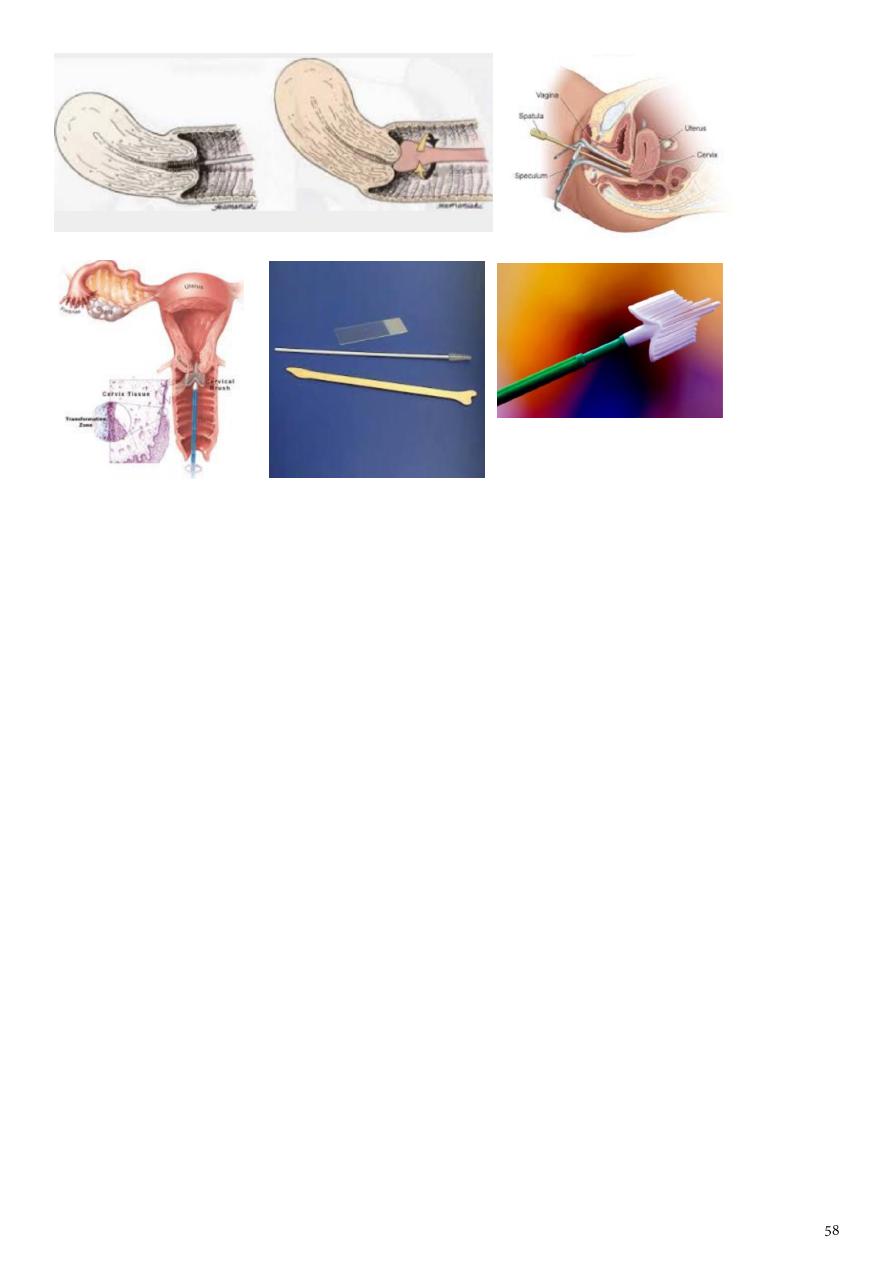
Notes form doctor:
Tools
spatula or cytobrush, slide, cusco speculum, gloves.
Indications of pap smear:
o For screening of malignant and premalignant conditions.
o For checking degree of infection (HPV- 16-18-31-35).
What are the pre-request of doing pap-smear:
o Avoid intercourse for at last 24-48 hours.
o Avoid use of any vaginal wash or douche.
o Do pap smear at day 12 of the cycle.
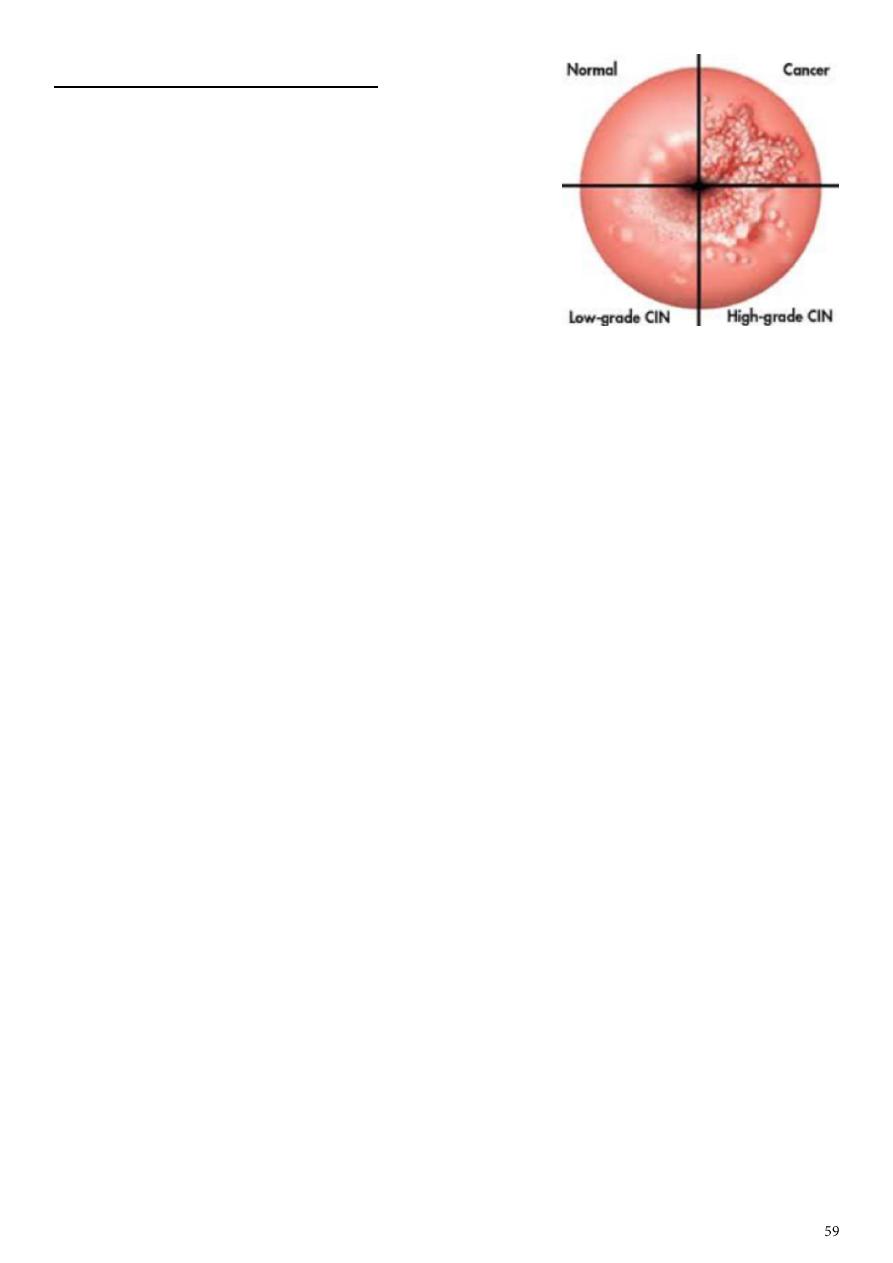
Subject15: Cervical cancer
Causes for cervical cancer:
human papillomavirus (HPV) infection,
HIV infection.
chlamydia infection.
stress and stress-related disorders.
dietary factors.
hormonal contraception.
multiple pregnancies.
exposure to the hormonal drug diethylstilbestrol (DES) .
Smoking.
family history of cervical cancer.
There is a possible genetic risk associated with HLA-B7.
Risk groups for cervical cancer:
Young age at first coitus(20years)
Multiple sexual partners.
Young age at first pregnancy.
High parity .
Low socioeconomic state.
Smoking.
Clinical presentations:
Asymptomatic.
Vaginal bleeding, contact bleeding.
Profuse vaginal discharge.
Cervical mass.
Moderate pain.
Fistula formation (leak age of urine or feces).
Symptoms of distant metastases may be present as enlarged inguinal and
supraclavicular L.N. metastases in the abdomen, lungs or else where in case of
advanced disease.
Systemic manifestation of advanced malignancy as: loss of appetite, weight loss,
fatigue, pelvic pain, back pain, leg pain, single swollen leg, heavy bleeding from the
vagina, leaking of urine or feces from the vagina, and bone fractures.

Differential diagnosis:
Cervicitis.
Cervical ectropion.
Endometrial carcinoma.
Pelvic inflammatory disease (PID).
Vaginal cancer.
Metastatic cancer to cervix (rare).
Tuberculosis.
Syphilitic chancre.
Choriocarcinoma.
Investigations:
Diagnosis should be based on histology and appropriate biopsies.
After the diagnosis is established, investigation which needed are:
Complete blood cell count
Renal functions test
Hepatic functions test
Imaging Studies: for staging
Chest radiograph should be obtained to help rule out pulmonary metastasis.
CT scan of the abdomen and pelvis is performed to look for metastasis in the liver,
lymph nodes, or other organs and to help rule out hydronephrosis/ hydroureter.
Barium enema (sometimes).
Intravenous urogram.
Treatment:
Conization or simple hysterectomy (removal of the uterus) - microinvasive cancer
Radical hysterectomy - removal of the uterus with its associated connective tissues, the
upper vagina, and pelvic lymph nodes. Ovarian preservation is possible.
Chemoradiation therapy
Surgery should only be considered an option for early disease (stage 1 and stage
11a).
Early cervical cancers (stage I and IIA) may be treated by either procedure.
Radiotherapy is the treatment of choice once the disease has spread beyond the
confines of the cervix and vaginal fornices, when surgery is not effective. Stage Ib2-IVa
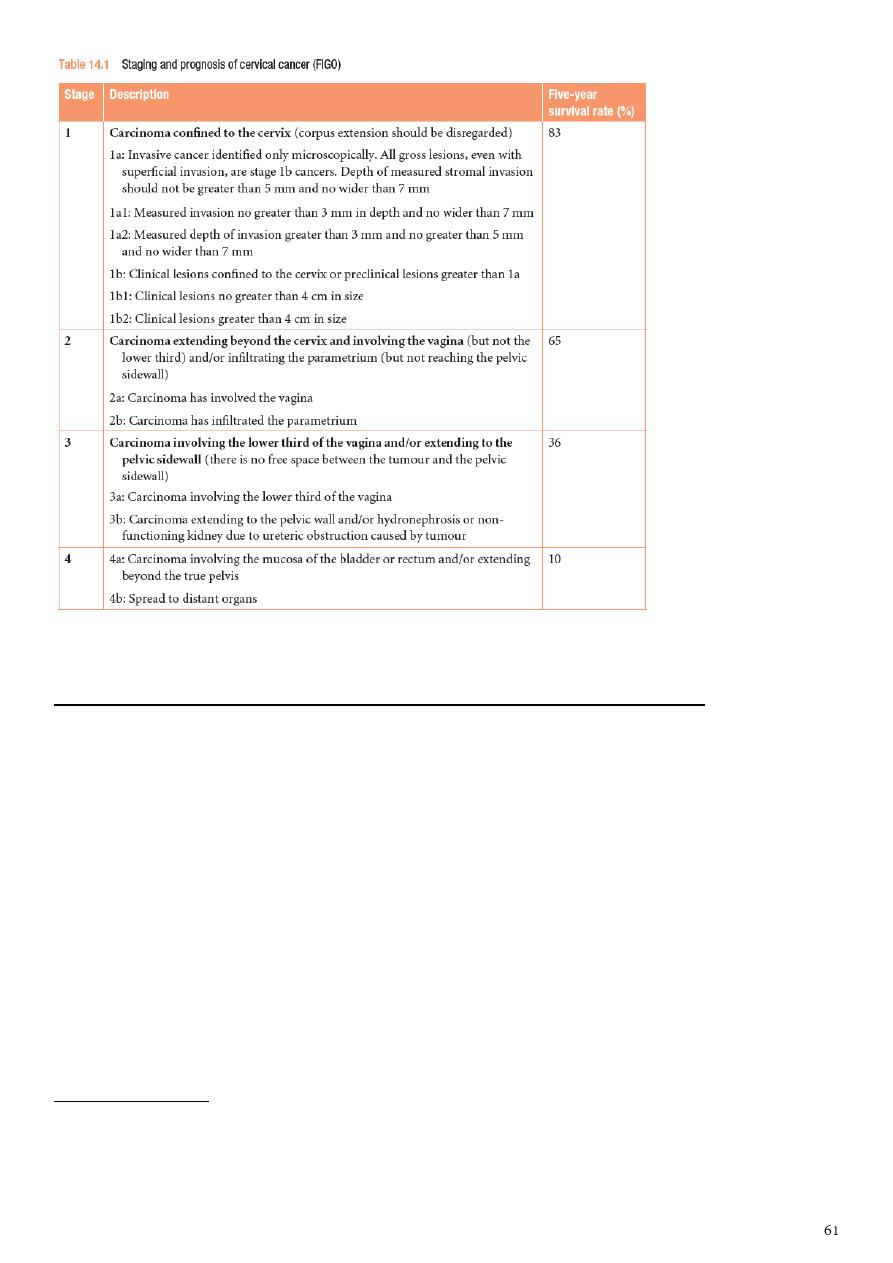
Subject16: Conditions affecting the vagina and vulva
Causes of vulvar conditions:
Infection: candida, Trichomonas vaginalis.
Inflammation: Lichen planus, Lichen sclerosis.
Trauma: sexual or asexual.
Drugs.
Premalignant and malignant conditions.
Autoimmune: Crohn's disease, Paget's disease.
Infections:
Candida infection:
Candida albicans dimorphic yeast.
Symptoms pruritus, vaginal discharge (white, cheesy, adherent to vaginal skin).
Signs redness, erythema, swelling, macerated skin.
Investigation swab.
Treatment symptoms control (give alarmin for pruritus), local care, antifungal
(local and systemic).
Trichomonas vaginalis:
It is protozoa, consider as STD.
Symptoms pruritus, discharge (green gray, frothy), soreness which lead to
dyspareunia.
Signs redness, swelling, strawberry lesion of vagina and cervix (2% of patients).
Investigation wet smear (saline).
Treatment for patient and husband, screening for other STD, metronidazole for 2
weeks, local care.
Herpes simplex:
Genital herpes caused by HSV-2 and increasingly by HSV-1 (due to oro-genital
sex).
There is primary and recurrence phases of infection.
Primary is most severe.
Symptoms pain, ulcer, dyspareunia, retention of urine, systemic manifestation
(fever, tired).
Signs multiple small elevated ulcers, swelling, erythema.
Investigations swab.
Treatment local care, analgesia, normal saline path, acyclovir.
Recurrent infection less severe and it is prolonged by stress, fever, sexual
intercourse, menstruation.
Human papilloma virus:
Condition called condyloma acuminatum (DDx: condyloma lata).
Presentation skin lumps different in size.
Treatment medical or surgical.
Other infections:
Syphilis.
Lymphogranuloma venereum.

Inflammatory:
Lichen sclerosis:
Inflammatory destructive skin valvar condition.
Could be associated with other skin lesions.
Cause is unknown but it could be autoimmune.
In young self-limited.
In elderly premalignant condition, destructive, not self-limited.
At beginning (erythema, ecchymosis) then (fissuring) then (scaring).
Signs narrowing of vaginal opening lead to dyspareunia, scaring of labia minora,
amputation of citreous.
Investigations biopsy (indications erosion, pigmentation, persistent ulcer).
Treatment:
o Valvar care: barriers, path.
o Local steroids (long term) gradual rate increase.
o Follow up (because it is premalignant).
o Rarely need surgery (if narrowing not improved by steroid.
Lichen planus:
Autoimmune condition.
Other associated autoimmune diseases pernicious anemia, type1 DM, thyroid
diseases, Addison's disease.
Associated with other skin conditions.
Symptoms pain, itching, dyspareunia, apareunia, bleeding (post-coital).
Signs velvety, Koebner's phenomenon.
Investigation biopsy for histopathology (indications erosion, pigmentation,
persistent ulcer).
Sometimes it involved the upper respiratory tract, esophagus, external auditory
meatus.
Treatment steroid, valvar care.
Hyperkeratosis:
Cause is chronic trauma.
Rarely pre-malignant.
Symptoms pain, pruritus, dyspareunia.
Signs white plaques.
Investigation biopsy.
Treatment care, removal of cause, steroid.

Dermatitis (eczema):
Types Contact dermatitis (only area of contact), allergic dermatitis (any area in the
body).
Causes of contact dermatitis soap, bubble path.
Causes of allergic dermatitis drugs, hair removal medication (sometimes lead to
contact dermatitis also).
Symptoms pain, redness, pruritus, dyspareunia.
Investigations skin test (patch test).
Treatment:
o Removal of affecting agent.
o Skin care (barrier).
o Antihistamine (alarmin).
o Iodine bicarbonate wash.
o Steroids.
Psoriasis:
Occur in flexion of body.
Features like psoriasis of other parts in the body.
Premalignant conditions:
Lichen sclerosis in elderly.
Human papilloma virus infection.
Valvar intra-epithelial neoplasm:
Vulval intraepitheial neoplasia (VIN) is a premalignant skin condition which is
increasing in incidence.
VIN can be either associated with human papilloma viruses (HPV) or with lichen
sclerosis.
Stages (dysplasia, one, two, three) like that of cervical cancer.
Presentation pain, pigmentation, pruritus, dyspareunia.
Investigations biopsy.
Treatment palliative therapy (laser cryotherapy), surgical removal and biopsy,
immunotherapy.
Do assessment of vagina and cervix.
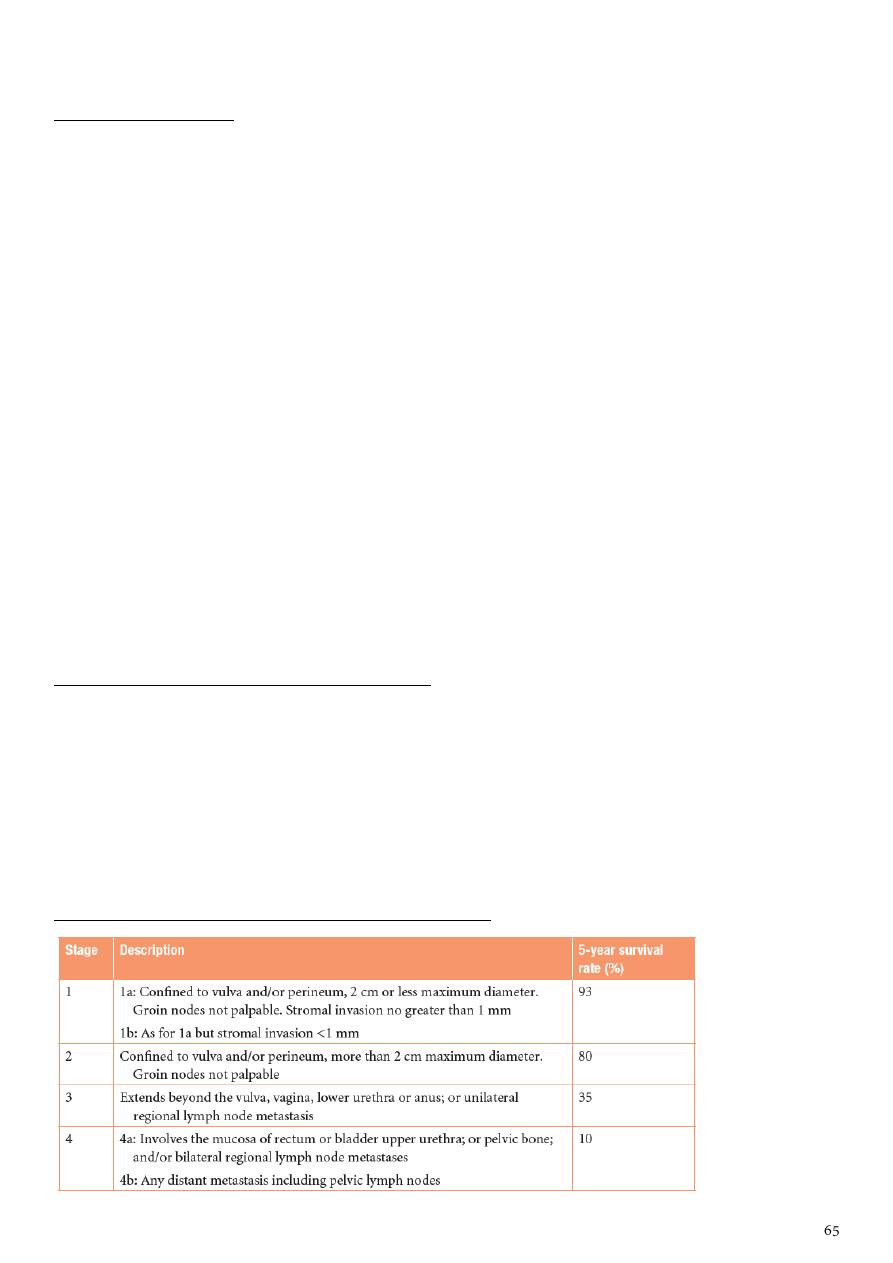
Vulval cancer:
Clinical presentation:
Vulval cancers usually present with vulval symptoms.
Patients may present with a lump (noticed when washing), vulval pain (some
tumours are ulcerating) and post-menopausal bleeding (some tumours bleed on
touch). Some patients are frequently unaware of vulval cancer.
While most tumours are small on examination, it is surprising how large some
tumours can be on initial presentation.
The tumours are usually clinically obvious and are often cauliflower-type growths on
the vulva.
Some tumours, however, can ulcerate and some may produce a subtle skin
thickening.
The most common sites are the labia majora and clitoris and the tumours may be
uni- or multifocal so it is important to examine the patient thoroughly (include the
anal area, vagina and cervix).
Vulval cancer spreads regionally to the groin nodes (inguinal and femoral) and
palpation of these nodes is important to exclude clinically obvious malignant nodes.
Patients should also have the cervix inspected to make sure that there is no
involvement by cancer or cervical intraepithelial neoplasia (CIN).
Investigation and the importance of staging:
A biopsy is essential for diagnosis and a chest x-ray is useful to exclude obvious lung
metastases.
Staging of the cancer is essential for prognostic information and planning adjuvant
treatment.
Poor prognostic factors include large (greater than 4 cm) primary tumours, sphincter
involvement and metastases to the groin nodes.
Staging and prognosis of vulval cancer (FIGO 2009):
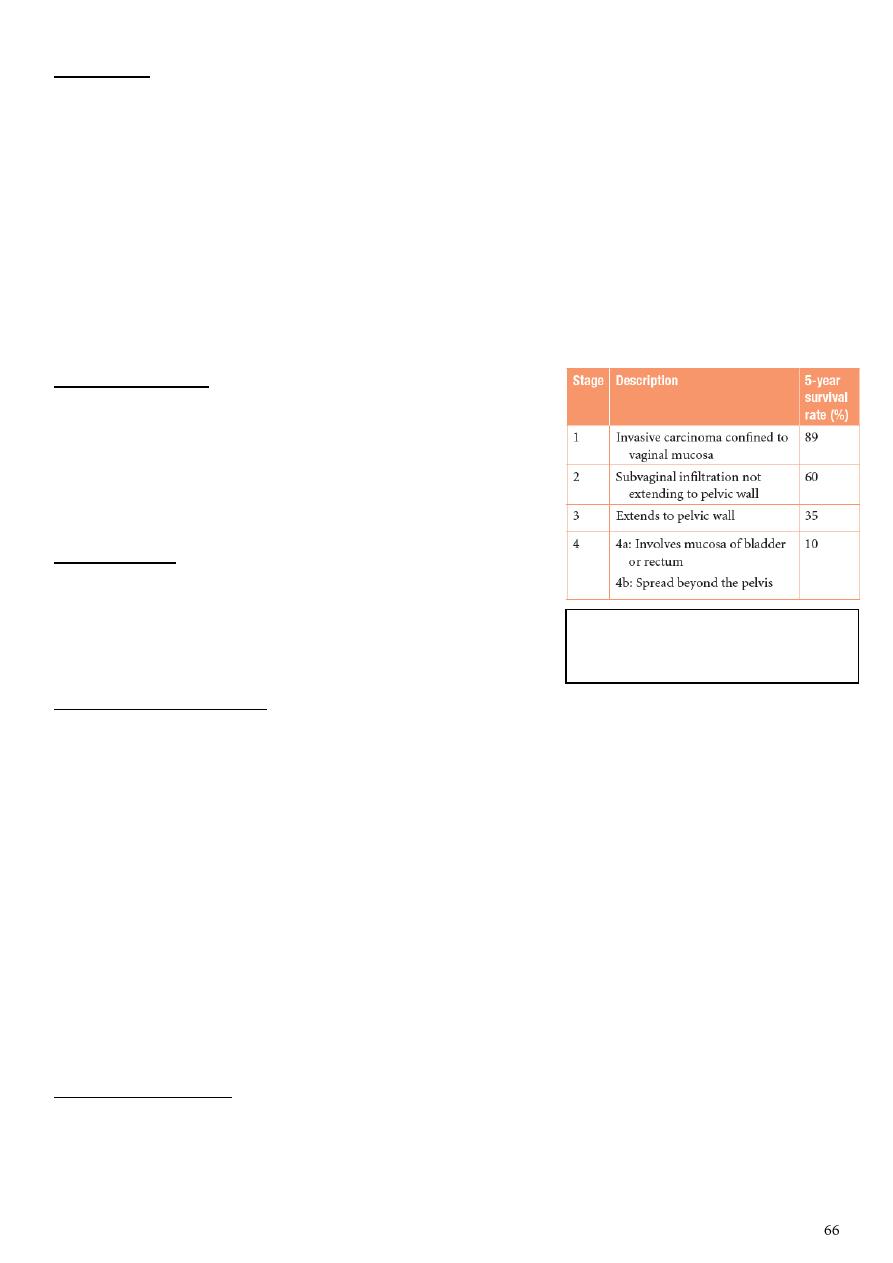
Treatment:
Surgical radical vulvacetomy which include removal of vulva, blilateral L.N
(inguinal and femoral L.Ns).
Complication of surgery poor wound healing, wound breakdown, bleeding,
lymphedema, DVT, psychological and sexual problems.
Radiotherapy if L.N is involved.
Sentinel L.N if involved give radiotherapy, if not involved do surgery only.
Early stage tumor wide local excision.
Conditions that affect vagina:
Vaginal discharge:
Infection bacterial vaginosis, Trichomonas,
candida.
Tumors of vagina, cervix, uterus.
Other F.B, trauma.
Lichen planus:
Involve vagina.
Give steroids suppositories and vaginal cream.
Lichen sclerosis: not involve the vagina.
Premalignant conditions:
Intraepithelial neoplasia can affect the genital tract (CIN and VIN).
Premalignant and malignant disease of the cervix.
The vaginal area can also be affected (called vaginal intraepithelial neoplasia, VAIN).
This is usually as a result of extension of CIN from the cervix.
VAIN is asymptomatic.
Treatment can involve cauterization, surgical excision, radiotherapy and
observational follow up depending on the patient, grade of disease and size of the
lesion.
VAIN assessment and treatment can be complicated and is best managed by
specialist teams.
There is a risk of vaginal cancer in untreated patients, but this risk remains unclear.
Malignant condition:
Will be missed so presented later and in metastatic state.
Treatment: radiation.
FIGO staging and prognosis of
vaginal cancer
Subject17: Urinary incontinence
Classification:
Stress incontinence (most common): involuntary loss of urine with physical effort
(cough, jump).
Urge incontinence: involuntary loss of urine associated with urgency.
Overflow incontinence: precede by contraction then full of bladder then
incontinence.
Continuous incontinence: always loss of urine without provoking factors.
Symptoms:
Symptoms before voiding (storage phase):
Stress incontinence.
Urge incontinence.
Urgency: intense desire to void.
Frequency: urination more than usual voiding rate.
Decrease or increase bladder sensation of fullness.
Symptoms during voiding (void phase):
Poor stream (voiding difficulty).
Intermittent stream.
Hesitancy.
Symptoms after voiding (post voiding phase):
Post voiding drippling of urine (most common cause is urethral diverticulum).
Feeling of incomplete emptying.
Dysuria, hematuria, pyuria.
Investigations:
1- Local:
Mid-stream urine examination (infection treat it).
Urinary diary test (chart for input and output, episodes of incontinence, provoked
factors).
Pad test (weight the pad then do physical activities that lead to incontinence for 4
hours then weight the pad, if increased by 1 g it considered as significant
incontinence).
Three swab test:
o Put three swabs in the vagina, inject the methylene blue in bladder, then wait for
time.
o Upper swab stain vesico-vaginal fistula.
o Middle swab stain urethra-vaginal fistula.
o Lower swab stain incontinence or contamination.
o Wet but not stain urethra-vaginal fistula.
2- Urodynamic study:
Flowmetery:
o Voiding (ml) per time (min).
o Normal half of bladder = 50 ml/sec.
o Detrusor pressure = pressure inside bladder – intra-abdominal pressure.
o Storage phase first desire to void = half of bladder capacity = 150-200 ml
normally.
o Bladder capacity = 400-600 ml normally.
o Detrusor pressure = less than 15 ml of water.
o No involuntary loss of urine.
o Ask the patient to void normally 50 ml/sec and detrusor pressure during voiding
= 70.
o Residual volume = less than 50 ml normally.
o Benefits know the bladder capacity, stress incontinence, detrusor pressure,
obstruction, residual volume.
o Indications of flowmetery:
Before operation.
Neurogenic bladder.
Multiple symptoms (urge and stress).
Multiple sclerosis.
Voiding problems.
Fail of operation.
Vedio-cystourethrography:
o Radioactive material and take colored films.
o Useful to see diverticula, fistula, reflux, same indications of flowmetery.
3- Radiological tests:
US Residual volume, bladder (stones, mass), diverticulum, mass in abdomen,
kidney.
IVU.
MRI problems in pelvic floor or sphinceter.
4- Tests for sphincter:
Nerve conduction study.
Urethral pressure profiometery.
Management:
1- Overflow insentience:
Treated by urologist and neurologist.
End by continuous catheter.
2- Stress incontinence:
Pelvic floor exercise.
Pelvic floor muscle stimulation.
Vaginal cone.
Drugs: SSRI (lead to nausea and vomiting).
Surgery:
o Colpo suspension.
o TPT.
o Artificial sphincter.
o Local injection of strengthening materials like collagen.
3- Detrusor overactivity:
Bladder training:
Drugs:
o Selective anticholinergic.
o TCA.
o Anti-diuretics (decrease urine output).
o Gabapentin (for neurogenic bladder).
Surgery:
o Sacral nerve stimulation.
o Tibial nerve stimulation.
Use pat or catheterization (suprapubic or self).
Subject18: Prolapse
Introduction:
It is protrusion of uterus or pelvic organs (bladder, rectum) in to or outside the vagina.
It occur due to lack or weakness of supporting structures like connective tissue, muscles,
ligaments that support the pelvic organs.
You can use Sim's speculum to see anterior and posterior vaginal wall see the
protrusion.
Causes:
Childbirth and raised intra-abdominal pressure

Aging the process of ageing can result in loss of collagen and weakness of fascia and
connective tissue.
Multiple parity lead to increase laxity of the ligaments.
Obstructed labor lead to weakness of the supporting structures.
Congenital connective tissue defects like collagen diseases.
Lack of estrogen lead to atrophy and increase laxity.
After hysterectomy because we cut the ligaments.
Types:
Cystocele prolapse of the urinary bladder.
Urethrocele prolapse of the urethra.
Rectocele prolapse of the rectum.
Enterocele prolapse of the part of the small intestine.
Uterine prolapse prolapse of the uterus.
Symptoms:
Non-specific:
o Lump, local discomfort, backache, bleeding/ infection if ulcerated, dyspareunia or
apareunia.
o Rarely, in extremely severe cystourethrocele, uterovaginal or vault prolapse, renal
failure may occur as a result of ureteric kinking.
Specific:
o Cystourethrocele – urinary frequency and urgency, voiding difficulty, urinary tract
infection, stress incontinence.
o Rectocele: incomplete bowel emptying, digitation, splinting, passive anal
incontinence.
Symptoms
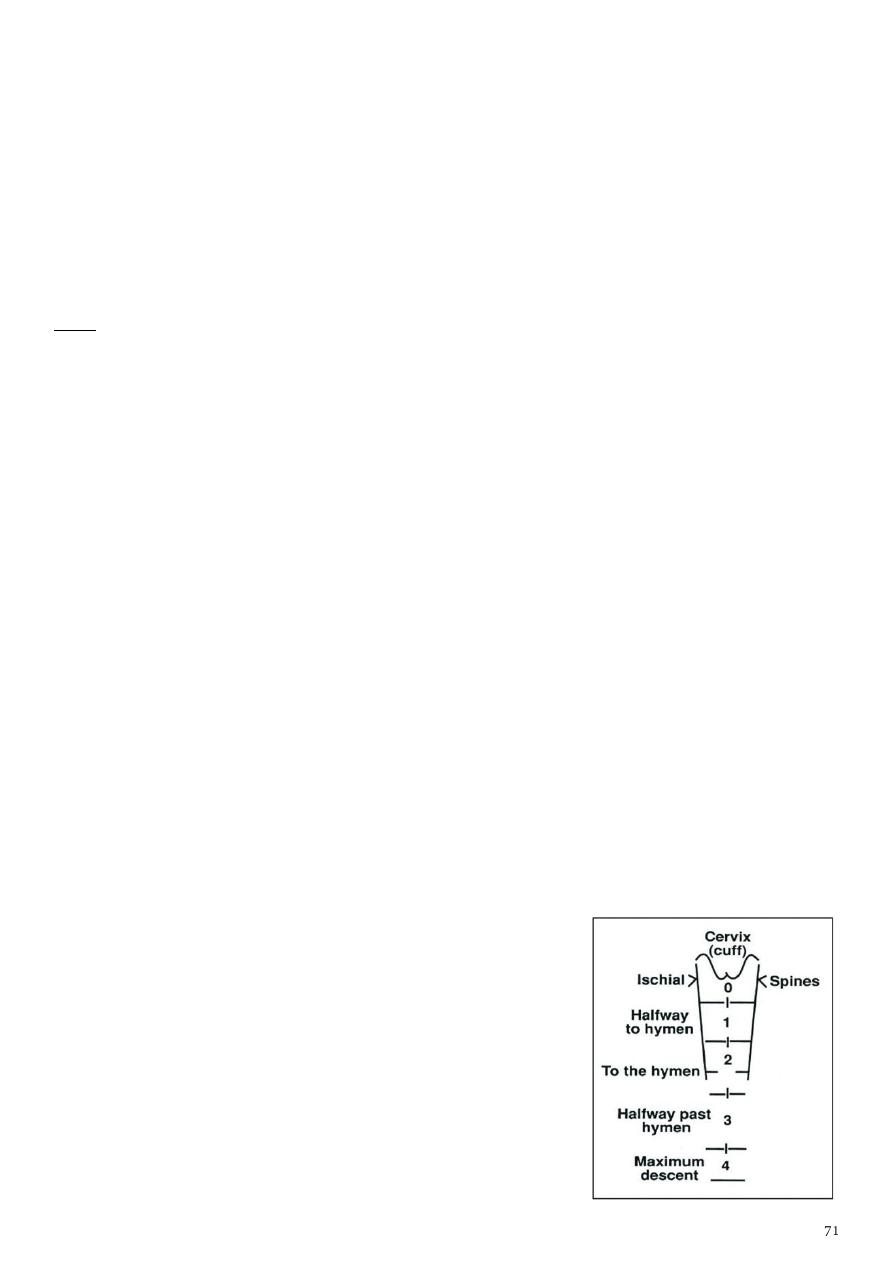
Cystocele or urethrocele:
Could be due to frequent pregnancies.
Lead to urinary symptoms like urgency, frequency, infection (cystitis, UTI).
General and abdominal examination show nothing important.
Pelvic examination ask the patient to come with full bladder, examine the patient in
dorsal position, good lightening, use sim's speculum see bulging ask patient to
cough and this lead to increase the bulging of cystocele and see few drops of urine pass
through the urethra.
Note: lithotomy position means labor position, dorsal position means patient lye on her
back.
Rectocele or enterocele:
Protrusion lead to bulging in the posterior vaginal wall.
Symptoms: difficulty in defecation, stasis, constipation, painful defecation.
Uterine protrusion:
Usually presented in menopause.
Not affect the cycle.
Symptoms: felling of heaviness in the pelvis, friction lead to ulceration and infection,
bleeding on touch.
Grades:
Grade1: the uterus reach the vagina.
Grade2: the uterus reach the introitus.
Grade3: uterus and cervix outside the vagina.
Procidentia = complete prolapse = Grade3
Score:
Baden Walker Hoffman score (2013)
Zero station at the level of Ischial spine ((there is no
prolapse at this point))
Grade1 descend in half way to the hymen.
Grade2 Reaching the hymen.
Grade3 half way behind the hymen.
Grade4 further descend.
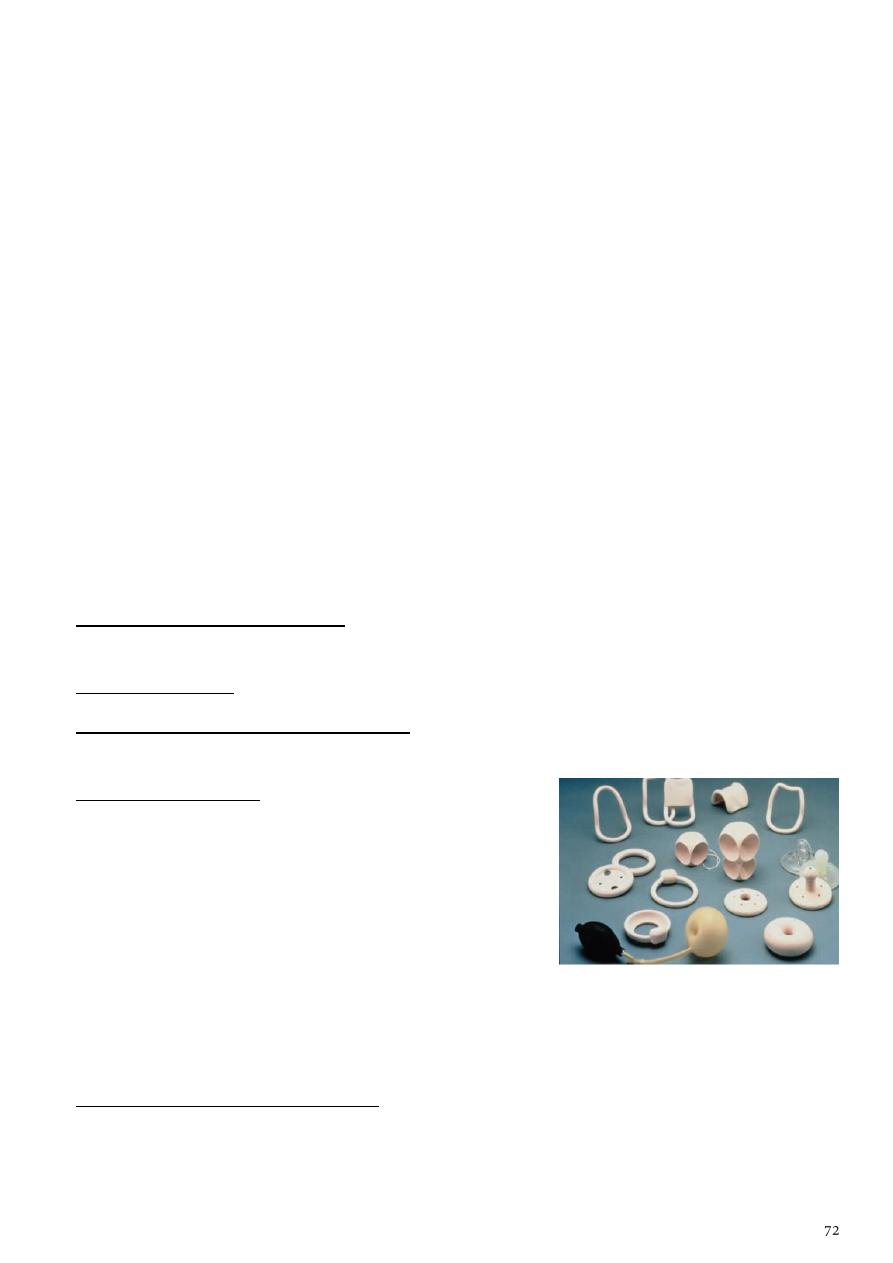
Differential diagnosis:
Anterior wall prolapse congenital or inclusion dermoid vaginal cyst, urethral
diverticulum.
Uterovaginal prolapse large uterine polyp.
Management:
History.
Examination.
Investigations:
o Cystocele general urine examination, urine microscopy, cystometry,
cystoscopy, urethroscopy, urodynamic study.
o Rectocele sigmoidoscopy (DDx tumor like fibroma), anoscopy.
o Uterine prolapse ulcer swab.
Treatment.
Treatment:
1- Hormonal replacement therapy give low dose tab of estrogen used in minor
prolapse.
2- Treat the infection.
3- Electrical stimulation of the pelvic floor will strength the floor used in minor
prolapse.
4- Pessary (ring pessary):
There are multiple types and shapes color and sizes of
pessary.
Used if patient above 60 years and not fit for
anesthesia or have multiple diseases.
Push the uterus to its normal site then fit the ring
between the anterior and posterior vaginal wall.
The ring pessary still 3-6 months then take it off and clean and sterilize it and put it
again.
Prolonged period of pessary lead to infection, ulcer, pressure.
5- Vaginal or abdominal hysterectomy used for patient complete her family, fit for
surgery, has procidentia (complete prolapse).
6- Patient young age, not complete her family, has uterine prolapse or other types of
prolapse:
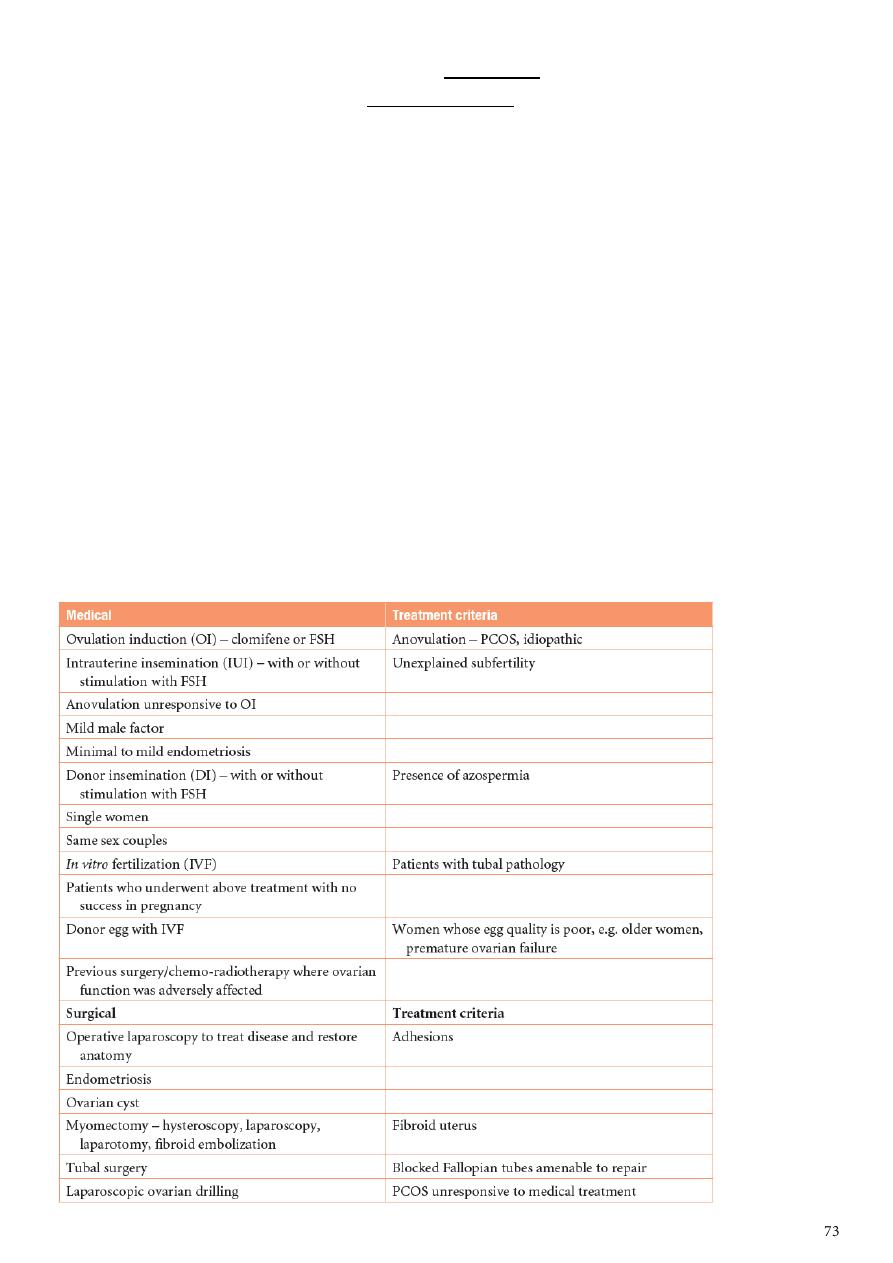
Repair of wall like anterior or posterior colporaphy or both.
Surgery fixing the ligament by uterosacral fixing (use mish between sacrum and
uterus).
Prophylaxis:
Exercise after delivery (pelvic flow examination).
Avoid prolongation of labor especially during second stage of labor.
Reduce the number of traumatic delivery.
General notes:
Bartholin cyst it is swelling of the bartholin duct which open between labia minora
and hymen + infection bartholin abscess. Treated by drainage and
marsupialization.
The pregnancy is confirmed by blood test in 3-5 days and by blood test in 10 days.
ICUD = used for 5 years carry risk of bleeding (menorrhea), infection (in first 2
weeks), pregnancy (when fall).
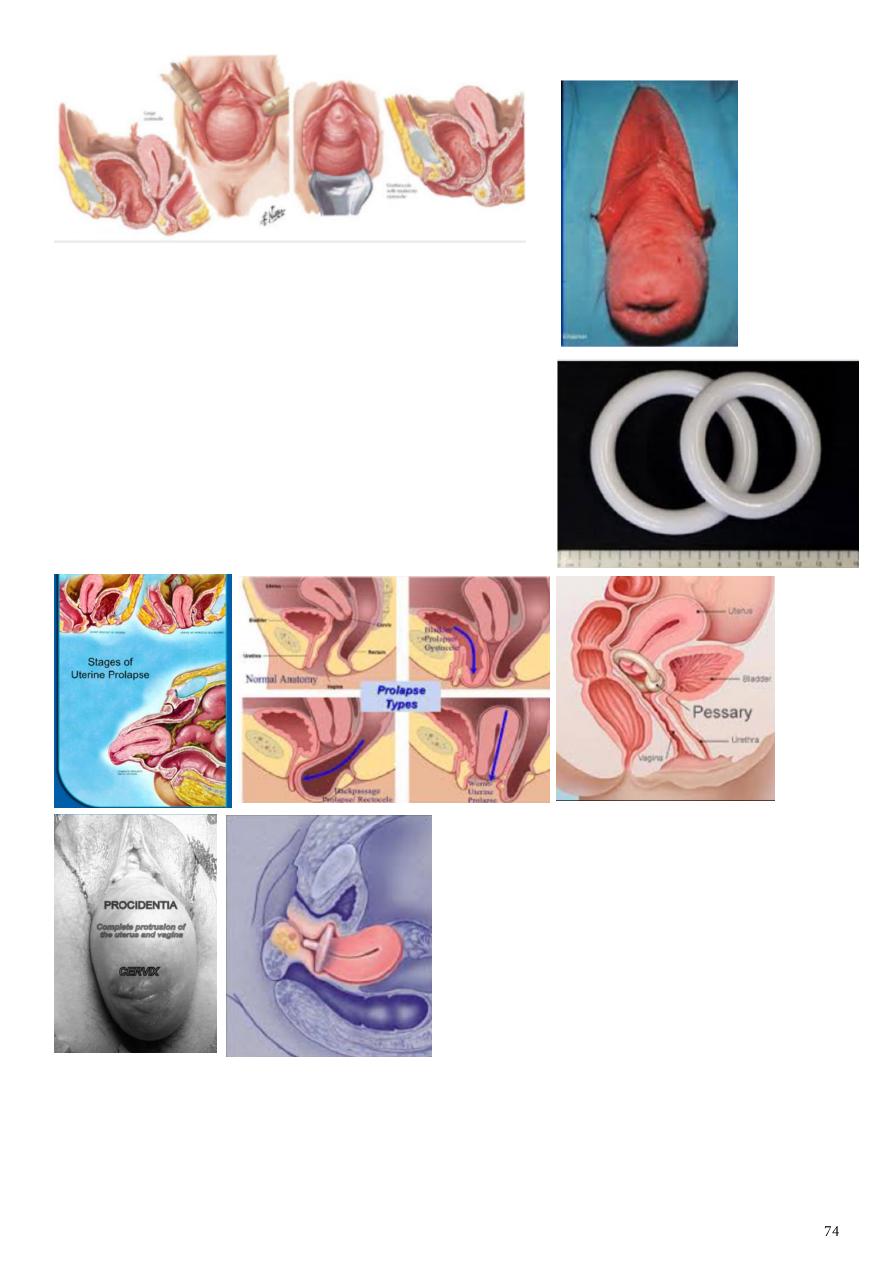
Notes form doctor:
Cystocele:
o Occur in old age.
o History of incontenince.
o Ask patient to come with full bladder.
o Ask the patient to cough.
Ring pessary:
o Used to treat prolapse.
o Put for 6 months.
o Complications ulceration, infection.

Subject19: Abnormal vaginal discharge
Infection:
Upper and lower genital tract infection.
Most of abnormal vaginal discharge is due to lower infection because it is more
common.
Infection of lower genital tract candida albicans (vulvo-vaginal candidiasis),
Trichomnias vaginals, bacterial vaginosis.
Candida discharge (white color, malodor, thick like cheese, adherent and difficult to
separate form vulvar skin) – itching – soreness.
T. vaginalis discharge (gray-greenish in color, frothy) – itching – soreness.
Bacterial vaginosis discharge (whitish-gray in color, bad fishy odor) – no itching – no
soreness.
Examination:
Candidiasis red macerated skin of vulva and vagina.
T. vaginalis red inflamed and strawberry vagina.
Bacterial vaginosis normal (because it is not inflammation, but there is only chage in
the bacterial flora).
Upper genital tract infection (pelvic inflammatory diseases PID):
Symptoms fever, abdominal pain, deep dyspareunia (superficial in lower infection),
diarrhea, vomiting, dysuria, frequency, abdominal tenderness, toxic state, adnexal mass
(abscess), vaginal discharge (without any characteristics), inter-menstrual bleeding,
menorrhagia, dysmenorrhea.
Diagnosis:
Candida culture and sensitivity.
T. vaginalis wet filed using normal saline and microscope to see tichomonus with its
four flagella and undulant membrane.
Bacterial vaginosis Criteria Discharge (whitish-gray, fishy odor), Ph (high, more
than 4.5), KOH (fish odor), Clue cell (by microscope).
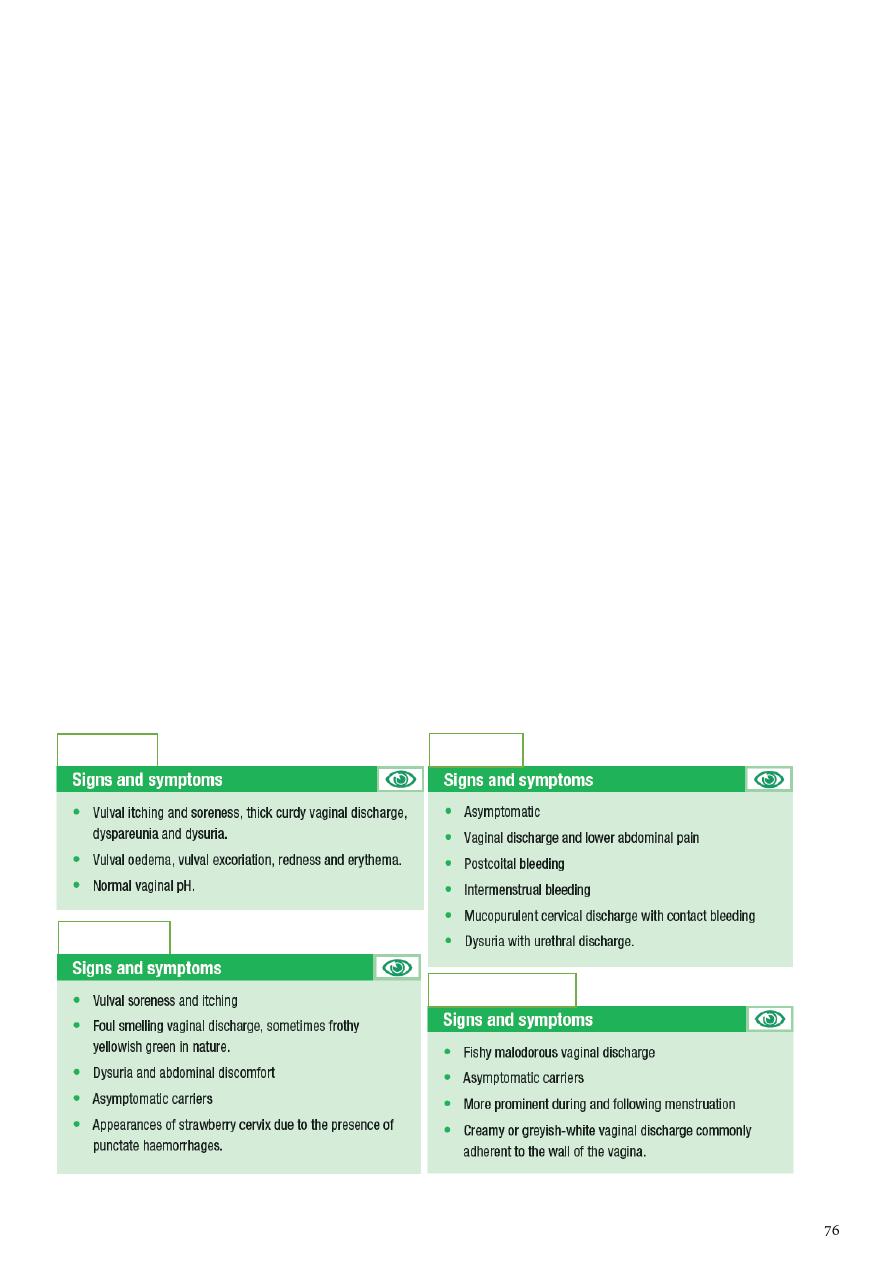
Management:
Candida nystatin, clotrimazole antifungal.
Trichomias metronidazole.
Bacterial vaginosis metronidazole.
Upper genital tract any antibiotic.
Symptomatic treatment analgesic, anti-piratic.
Bed-rest.
STDs prevent sexual intercourse, treat the partner, search for partner infected,
search for other STDs.
Key Points:
Acute PID can be life threatening.
Other differential diagnosis should be kept in mind (ectopic pregnancy, appendicitis).
Detailed sexual history should be taken.
Incomplete treatment of sexually transmitted infections should be avoided as there is a
high chance of recurrence.
Surgical treatment should not be delayed if patient’s general condition is not improving
with conservative treatment.
Thorough counselling regarding the implications of infection with regards to subfertility
and risk of ectopic pregnancy should be offered.
All attempts to contact present and previous partners should be encouraged and made.
Patients should be advised to use barrier contraception until the infection is completely
cured. Test of cure should be done.
Candidiasis
Trichomonas
Bacterial vaginosis
Chlamydia
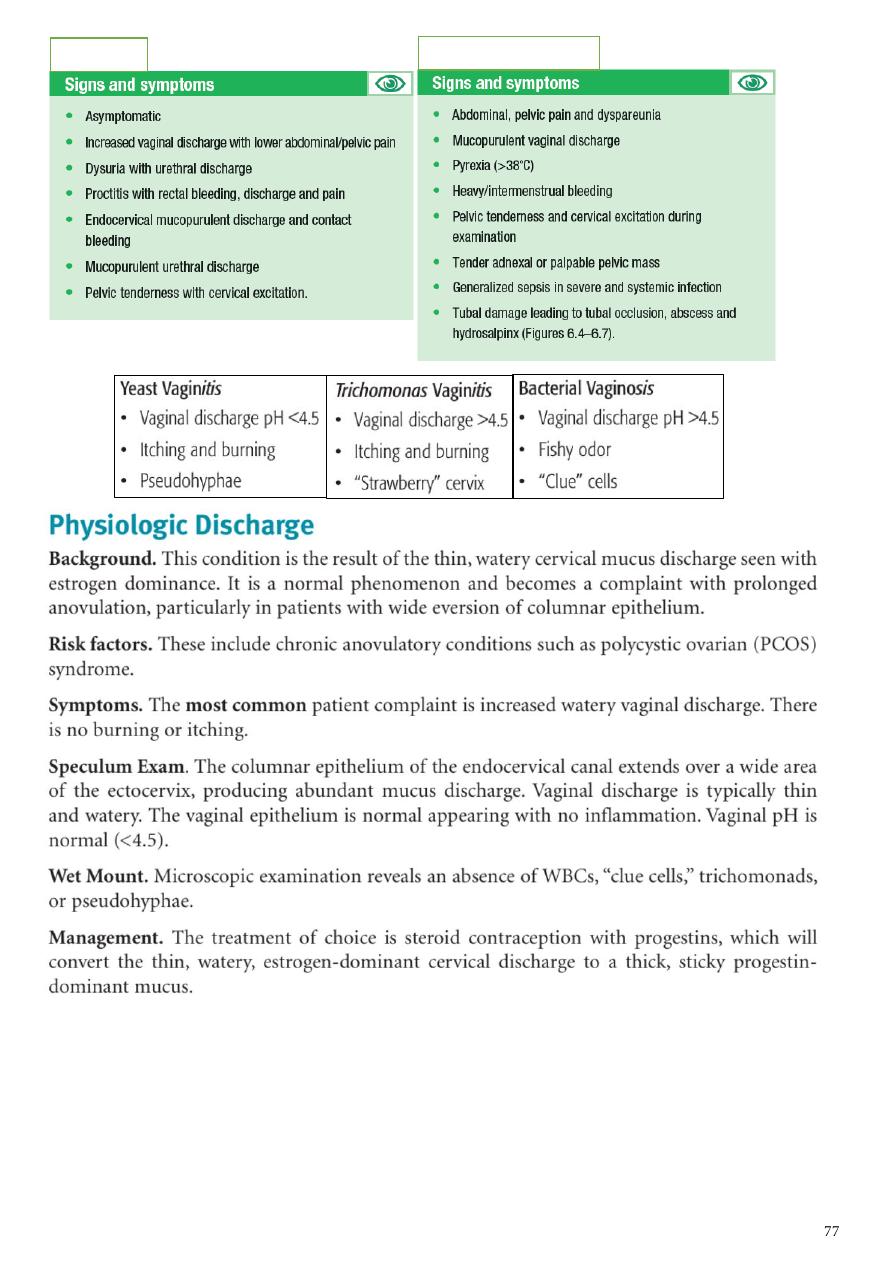
Gonorrhea
Upper genital infection

Subject20: Gestational trophoblastic disease
Association:
Younger age group less than 16 years and more than 40 years.
Areas: Asians.
History of previous mole.
Nutritional factors: carotene deficiency.
Partial mole:
Triploid (3 sets of chromosome = 69).
Due to fertilization of 2 sperms to one ovum or fertilization of one divided sperm to one
ovum.
Fetal vessels and placenta present.
There is focal hydropic degeneration in placenta.
Presentation: abortion.
Diagnosed by histopathological study.
Need for chemotherapy (0.5%).
H.mole:
46 chromosome.
Only paternal chromosome (2 sperms or one divided sperm).
Usually xx.
No feral vessels.
Presence of villi with hydropic degeneration.
Presentation: excessive symptoms of pregnancy like pre-eclampsia, thyroid
enlargement, large uterus.
50% need chemotherapy.
Diagnosed by US snow storm appearance due to excessive cystic lesions.
Management of partial mole and H.mole:
Evacuation:
Preparation: prepare blood, investigation (CBC, Hb, blood group, cross match, B-hCG).
General ansthesia.
Suction method if evacuation.
If bleeding occur not use oxytocin but use ergometrine at the end of evacuation.
Follow up:
Twice weekly for 6 months.
Avoid pregnancy to avoid confusion.
Better not use COCP cause slower lowering of B-hCG.
Better not use IUCD or progesterone they lead to bleeding and confusion.
Best method is condom.
Contraception for 6 months if not use chemotherapy.
Contraception for 1 year if use chemotherapy.
Chemotherapy.
Figo scoring or staging:
Age of patient less than 40 years is low risk, more than 40 years is high risk.
Previous pregnancy before the mole H.mole (low risk), abortion (moderate risk),
normal pregnancy (high risk).
Duration between H.mole and pregnancy less than 3 months (low risk), more than 1
year (high risk).
Level of B-hCG 1000 (low risk), 1000000 (high risk).
Site of metastasis lung (low risk), brain (high risk).
Number of metastasis large number (high risk), low number (low risk).
Size of metastasis small size (low risk), large size (high risk).
Previous chemotherapy if not take (low risk), if take (high risk).
=== Figo scoring: less than 6 (give one chemotherapy), more than 6 (give multiple
chemotherapy).
Photos:
www.muhadharaty.com/lecture/7827
www.muhadharaty.com/lecture/7888
