Carcinoma of the ovary
Carcinoma of the ovary is most common in the wealthy nations of the world. There are just under 6000 cases each year in the UK.While the incidence of ovarian cancer is similar to that of endometrium and of cervix, more women die from ovarian cancer than
from carcinoma of the cervix and body of the uterus combined
Aetiology
1-'Incessant ovulation' theoryEpithelial tumours are most frequently associated
with nulliparity, an early menarche, a late age at
menopause and a high estimated number of years
of ovulation
Oral contraceptive use reduces the risk
fourfold,However, even without oral contraceptives,
increasing age at first birth reduces the risk OF ovarian
cancer
2-Subfertility treatment
Subfertility, especially when it is unexplained, is associated
with both ovarian and endometrial cancer.
However, case-controlled studies have suggested that there might possibly be a link between ovarian cancer
and prolonged attempts at induction of ovulation
3-Genetic factors
Familial ovarian cancerThere is a family history in between 5 and 10 per cent
of women with epithelial ovarian cancers - usually
serous adenocarcinomas
A woman with one affected close relative has a lifetime
risk of 2.5 per cent, twice the risk in the general
population. With two affected close relatives, the lifetime
risk increases to 30-40 per cent
A particular feature of familial cancers is the relatively
early age at which they occur
Most of these families also have cases of breast or
colorectal cancer in the family. The defective genein the breast/ovary famil ies is most commonly the
tumour-supp ressor gene BRCAI (81 per cent).
BRCA2 is defective in about 14 per cent
Familial ovarian cancer
• Familial ovarian cancer is rare - 5-10%
• Suggestive history
• At least two first-degree relatives with ovarian, breast or colorectal carcinoma
• Cases usually diagnosed before 50 years of age
• Defective genes include BRCA 1 and BRCA2
• The risk of ovarian cancer (40%) in these families is
less than the risk of breast cancer (80%)
• Genetic testing cannot guarantee to detect all defective genes
Classification of ovarian tumours
Ovarian tumours can be solid or cystic. They may bebenign or malignant and in addition there are those
that, while having some of the features of malignancy,
lack any evidence of stromal invasion. These are
called borderline tumours.
Simplified histological classification ofovarian tumours
I Common epith elial tumours (benign, borderHne or ma'lignant)A. Serous tumour
B. Mucinous tumour
C. Endometrioid tumour
D. Clear cell (mesonephroid) tumour
E. Brenner tumour
F. Undifferentiated carcinomas
II Sex cord stromal tumours
A. Granulosa stroma cell tumour
B. Androblastoma: Sertoli-Leydig cell tumour
C. Gynandrobl'astoma
III Germ cell tumours
A. Dysgerminoma
B. Endodermal sinus tumour (yolk sac tumour)
C. Embryonal cell tumour
D. Choriocarcinoma
E. Teratoma
F. Mixed tumours
IV Metastatic tumours
Pathology of epithelial tumours
Well-differentiated epithelial carcinomas tend to more often associated with early-stage diseaseMucinous and endometrioid lesions are likely to be associated with an earlier stage and lower grade than
Serous cystadenocarcinomas
Borderline epithelial tumours
Ten per cent of all epithelial tumours of the ovary are of borderline malignancy.These show
*varying degrees of nuclear atypia
*an increase in mitotic activity,
*multi-layering of neoplastic cells
*formation of cellular buds,
*but no invasion of the stroma
*Most borderline tumours remain confined to the
ovaries and this may account for their much better
prognosis
Serous carcinoma
*Most serous carcinomas have both solid and cystic
elements but some may be mainly cystic.
*They often affect both ovaries.
*Well-differentiated tumours have a papillary pattern with stromal invasion.
*Psammoma bodies (calcospherules) are often present.
Mucinous carcinoma
Malignant mucinous tumours account for 10 per centof the malignant tumours of the ovary. They are usually
multilocular, thin-walled cysts with a smooth external
surface containing mucinous fluid
Mucinous
tumours are amongst the largest tumours of theovary and may reach enormous dimensions. A cyst
diameter of25 cm is quite common
Endometri oid carcinoma
These are ovarian tumours that resemble endometrialcarcinomas. Most are cystic, often unilocular, and
contain turbid brown fluid. Five to 10 per cent are
seen in continuity with recognizable endometriosis
It is important to note that 15 per,_ cent of
endometrioid carcinomas of the ovary are associated
with endometrial carcinoma in the body ofthe uterus.
In most cases these are two separate primary tumours
Clear cell carcinoma (mesonephroid)
These are the least common of the malignant epithelialtumours of the ovary, accounting for 5-10 per cent
of ovarian carcinomas
The appearance from which
the tumours derive their name is the clear cell patternbut, in addition, some areas show a tubulo-cystic
pattern with the characteristic 'hob-nail' appearance of
the lining epithelium.
Natural history
Some two-thirds of patients with ovarian cancerpresent with disease that has spread beyond the pelvis.
This is probably due to the insidious nature of the
signs and symptoms of carcinoma of the ovary, but
may sometimes be due to a rapidly growing tumour.
symptoms Diagnosis
*Abdominal pain or discomfort are~he commonest presenting complaints
*distension or
*feeling a lump the next most frequent.
*Patients may complain of indigestion,
*urinary frequency,
*weight loss r
*rarely, abnormal menses or postmenopausal bleeding
signs
*A hard abdominal mass arising from the pelvis ishighly suggestive, especially in the presence of ascites.
*A fixed, hard, irregular pelvic mass is usually felt best by combined vaginal and rectal examination
*The neck and groin should also be examined
for enlarged nodes.
investigations
*Haematological investigations include a full bloodcount, urea, electrolytes and liver function tests.
*A chest X-ray is essential.
* It is sometimes advisable to carry out a barium enema or colonoscopy to differentiate
between an ovarian and a colonic tumour and to
assess bowel involvement from the ovarian tumour
itself
An intravenous pyelogram (IVP) is occasionally
useful. Ultrasonography may help to confirm the
presence of a pelvic mass and detect ascites before it is
clinically apparent. In conj unction with CA 125 estimation,
it may be used to calculate a 'risk of malignancy
score
Markers for epithelial tumours
CA 125 is the only marker in common clinical use.It can also be raised in benign conditions such as
endometriosis. CA 125 is useful for monitoring women
receiving chemotherapy to assess response. A persistent
rise in CA 125 may precede clinical evidence
of recurrent disease by several months in some cases.
FIGO staging for primary ovarian carcinoma
FIGO definitionStage
Growth limited to ovaries
I
Growth involving one or both ovaries with pelvic extension
II
Growth involving one or both ovaries with peritoneal implants outside the
pelvis or positive retroperitoneal or inguinal nodes
Superficial liver metastases equals Stage III
III
Growth involving one or both ovaries with distant metastases 1
If pleural effusion is present, there must be positive cytology to allot a case to Stage IV
Parenchymal liver metastasis equals Stage IV
IV
treatment
Depends onStaging
Tumor type
Age
Desire for future fertility
Include surgery, chemotherapy and/or radiation therapy
Surgery for epithelial ovarian cancer
Primary surgery -to determine diagnosis and remove tumour• Total abdominal hysterectomy
• Bilateral salpingo-oophorectom
Infracolic omentectomy
Conservative primary surgery
• Young, nulliparous woman with Stage la disease• No evidence of synchronous endometrial cancer
• Unilateral salpingo-oophorectomy
Interval debulking surgery
• Women with bulky disease after primary surgery
• Must respond after two to four courses of chemotherapy
• Chemotherapy resumed after surgery
Second-look surgery
• At the end of chemotherapy
• No place in current management
Borderline tumours
• Ovarian cystectomy or oophorectomy adequate inyoung women
• Hysterectomy and bilateral salpingo-oophorectomy in
older women
Non-epithelial tumours
• Sex-cord stromal tumour• Granulosa cell tumour
• Theca cell tumour
• Sertoli-Leydig tumour
• Germ cell tumour
• Dysgerminoma
• Yolk sac (endodiermal sinus) tumour
• Teratoma
Sex-cord stromal tumour
Granulosa and theca cell tumours
The most common sex cord stromal tumours arethe granulosa and theca cell tumours.
They often produce steroid hormones, in particular oestrogens, which can cause *postmenopausal bleeding in older
women
*and sexual precocity in pre-pubertal girls.
Pathology
Granulosa cell tumours are normally solid, but cystic spaces may develop when they become largeLike most tumours of the sex cord stromal tumour group, the cut surface is often yellow because of neutral lipid related to sex
steroid hormone production.
Sertoli-Leydig cell tumours
Half of these rare neoplasia produce male hormoneswhich can cause virilization.
The prognosis for the majority who have
localized disease is good
Germ cell tumours
Dysgerminomas
Dysgerminomas account for 2-5 per cent of all
primary malignant ovarian tumours. Nearly all occur
in young women less than 30 years old. They spread
mainly by lymphatics
Pathology
Dysgerminomas are solid tumours which have asmooth or nodular, bosselated external surface
They may reach a considerable size: the mean diameter
is 15 cm. Approximately 10 per cent are bilateral
Elements of immature teratoma, yolk sac tumour or
choriocarcinoma are found in about 10 per cent of
dysgerminomas.l
Yolk sac (endodermal sinus) tumours
is the secondmost common malignant germ cell tumour of the
ovary, making up 10-15 per cent overall and reaching
a higher proportion in children.
The tumour is usually
well encapsulated and solid.
It often
secretes AFP, which can be used to monitor treatment
Teratoma
Immature teratomas are composed of a wide variety
of tissues and comprise about 1 per cent of all
ovarian teratomas
They are unilateral in almost all
cases and appear as solid masses
Metastatic Tumors of Ovary
Cancer from other sites may metastasize to the overies,there may be microscopic surface deposits or gross solid or cystic enlargement of the ovary.Endometrial carcinoma may spread to the ovary & other common primary sites are the colon,stomach&breast.
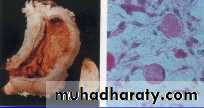
Krukenberg tumor
Is secondary growth from a mucus-secreting carcinoma arising in stomach or colon,in which both ovaries usually involved .The tumor histologically characterized by signet ring cells ,these have accumulated mucoid substance in the cytoplasm so the nucleus is displaced right to the edge of the cells.
METASTATIC TUMOR FROM GASTRIC CANCER (Krukenberg )
gastric carcinoma of the fundus, with secondary ovarian tumor (Mucus-secreting signet-ring cells)
Krukenberg Tumor:
METASTATIC TUMOR FROM BREAST CANCER
both ovaries replaced by pale, rather nodular tumor,
with breast cancer cells arranged in long linesperpendicular to the surface of the ovarian cortex