1
Fifth stage
Medicine
Lec-6
د بشار شاكر
3/11/2015
Brain SOL - 2
Meningiomas
Arise from the dura mater and are nearly always benign, well-demarcated lesions that
displace rather than invade the adjacent neural tissue as they grow.
These mesodermal tumors most often become clinically evident between the ages of 40
and 50. They are diagnosed by MRI or CT scanning which reveals marked, homogeneous
contrast enhancement. Meningiomas tend to appear in certain classic locations with
corresponding typical neurological manifestations. They often grow very slowly and are not
uncommonly discovered as an incidental radiological finding. The indications for treatment
must then be carefully considered: resection may be desirable in younger patients, but
unnecessary in older ones.
Common sites of meningiomas, and associated clinical features:
2
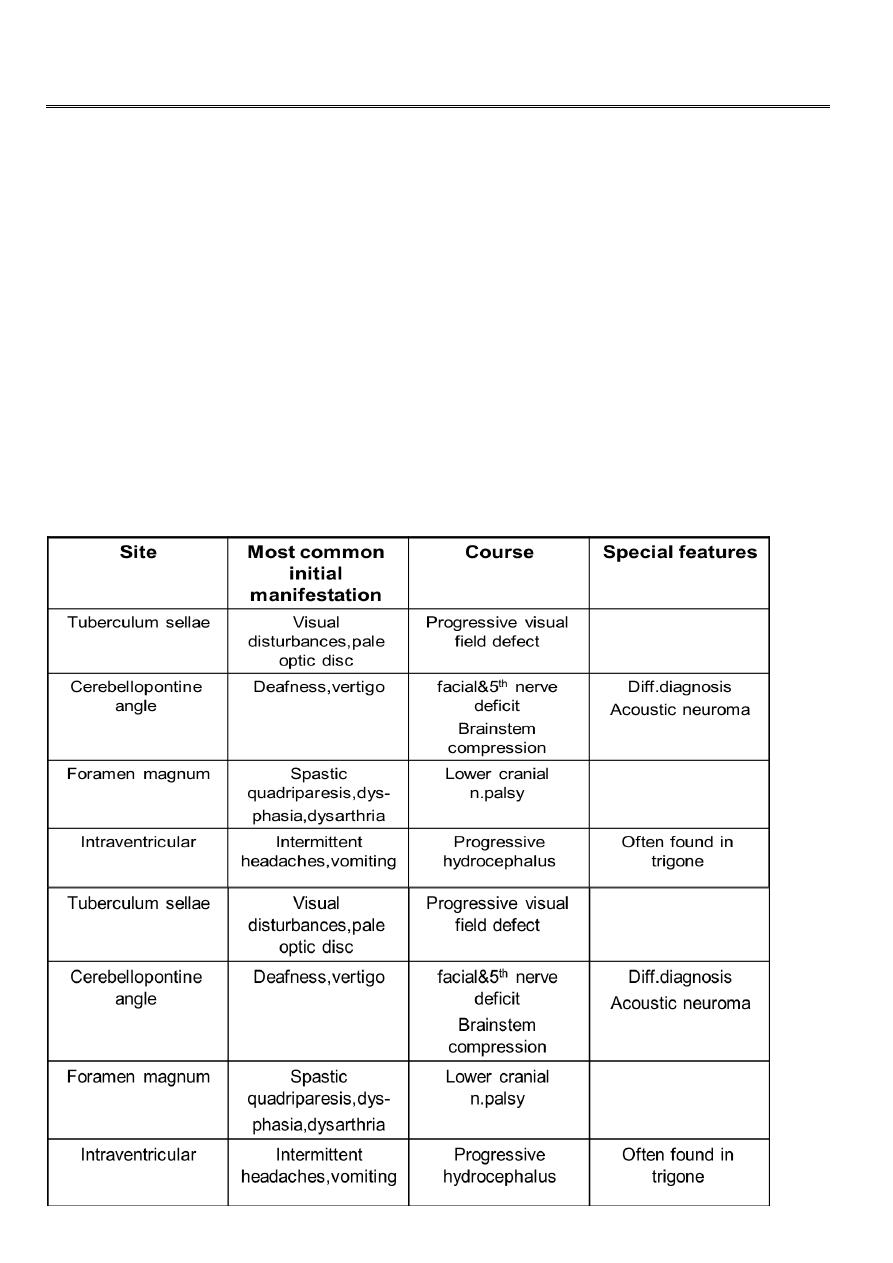
Meningioma of the left cerebral convexity Falx meningioma
Sphenoid wing meningioma
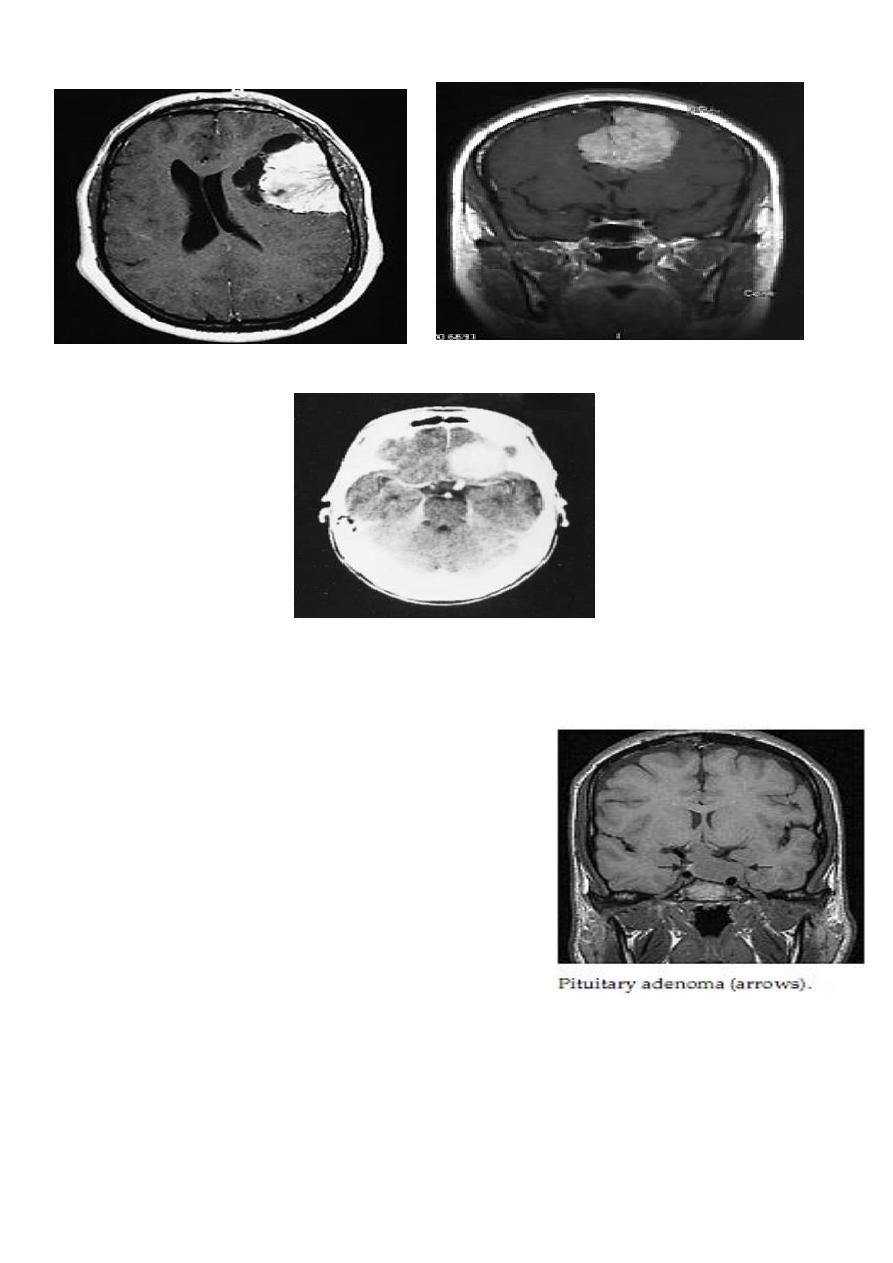
Pituitary tumors
Usually arise from the cells of the anterior pituitary
lobe.
Depending on their cells origin, they can produce
hormones in excess or cause hormone deficiency.
Thus, they present clinically with endocrine
disturbances and/or compressive effects on the
adjacent neural tissue .
They most commonly present between the ages of 30
and 50.
The rare eosinophil adenomas produce excessive growth hormone, causing
acromegaly,while basophil adenomas produce excessive ACTH, causing Cushing syndrome
(which ,when caused by a pituitary tumor, constitutes Cushing disease).
Prolactinomas produce galactorrhea and secondary amenorrhea in women and impotence
in men.

3
Although basophil adenomas and prolactinomas rarely cause mass effect, eosinophil
adenomas and, above all, the hormonally inactive chromophobe adenomas tend to grow
quite large, causing compression and dysfunction of the normal pituitary tissue, clinically
evident as hypopituitarism (multiple pituitary hormone deficiencies, including
hypothyroidism and secondary hypogonadism). Chromophobe adenomas can also
compress the optic chiasm, causing a visual field defect, usually bitemporal upper
quadrantanopsia or bitemporal hemianopsia. Compression of the optic nerves themselves
may impair visual acuity.
Prompt neurosurgical removal of the tumor can often reverse these visual difficulties if they
are still incomplete at the time of surgery.Most pituitary tumors do not present with signs
of mass effect (only one in 10 enlarges the sella turcica visibly on plain films of the skull).
Tumors that do cause mass effect should be neurosurgically removed, preferably by the
transsphenoidal route.
Hormonally active microadenomas can sometimes be treated with medication alone (e. g.,
prolactinoma can be treated with inhibitors of prolactin secretion, such as bromocriptine
and lisuride.
Craniopharyngioma
Arises in or above the pituitary fossa, often growing upward toward the diencephalon and
third ventricle.
This is a cystic tumor derived from epithelial remnants in Rathke’s pouch,
Generally containing calcifications as well as cholesterol crystals. It presents with
hypopituitarism , diencephalic manifestations (diabetes insipidus), and visual disturbances.
Like a pituitary tumor, it can cause hemi- or quadrantanopsia and impair visual acuity; it can
also cause occlusive hydrocephalus.
Craniopharyngioma is the most common suprasellar tumor in children and adolescents. It is
best treated by complete resection
ACOUSTIC NEUROMA
This is a benign tumour of Schwann cells of the 8th cranial nerve, which may arise in
isolation or as part of NF2 .
As an isolated finding, an acoustic neuroma occurs after the third decade and is more
frequent in females. The tumour commonly arises near the nerve's entry point into the
medulla or in the internal auditory meatus, usually on the vestibular division. Such lesions
make up 80-90% of tumours at the cerebello-pontine angle.

4
Clinical features
These depend on the site of the tumour along the acoustic or vestibular nerve. Similar
tumours arise rarely from the trigeminal nerve.
Hearing loss is almost invariable, although it may not be the presenting feature. Sensory
symptoms in the face and vertigo are also common at presentation. Distortion of the brain
stem and/or cerebellar peduncle may cause ataxia and/or cerebellar signs in the limbs.
Distortion of the fourth ventricle and cerebral aqueduct may cause hydrocephalus, which
may be the presenting feature .
Facial weakness is unusual at presentation, but facial palsy may follow surgical removal of
the tumour.
Investigation
MRI is the investigation of choice, CT being less useful in this region of the posterior fossa.
Management
This involves surgical removal. If this is complete, the prognosis is excellent. Deafness and
facial weakness, if not present before surgery, usually result from the operation.
Ependymoma
Is a benign tumor usually seen in children and adolescents.
On pathological examination, these tumors are often cystic and partly calcified. They
develop from the neuroepithelium of the walls of the cerebral ventricles and the central
canal of the spinal cord; as they grow, they displace, but do not invade, the adjacent neural
tissue. Ependymomas usually arise in the posterior fossa,most commonly near the fourth
ventricle, and in the conusmedullaris of the spinal cord.Their main clinical manifestations
are focal (often cerebellar) neurological deficits and signs of intracranial hypertension
secondary to compression of the CSF pathways and occlusive hydrocephalus. An unusually
persistent, continuous headache in children should arouse suspicion of an ependymoma or
other mass in the posterior fossa.
The treatment is by resection, followed by radiotherapy of the entire neuraxis. Seventy
percent of treated patients survive for 10 years or longer.
5
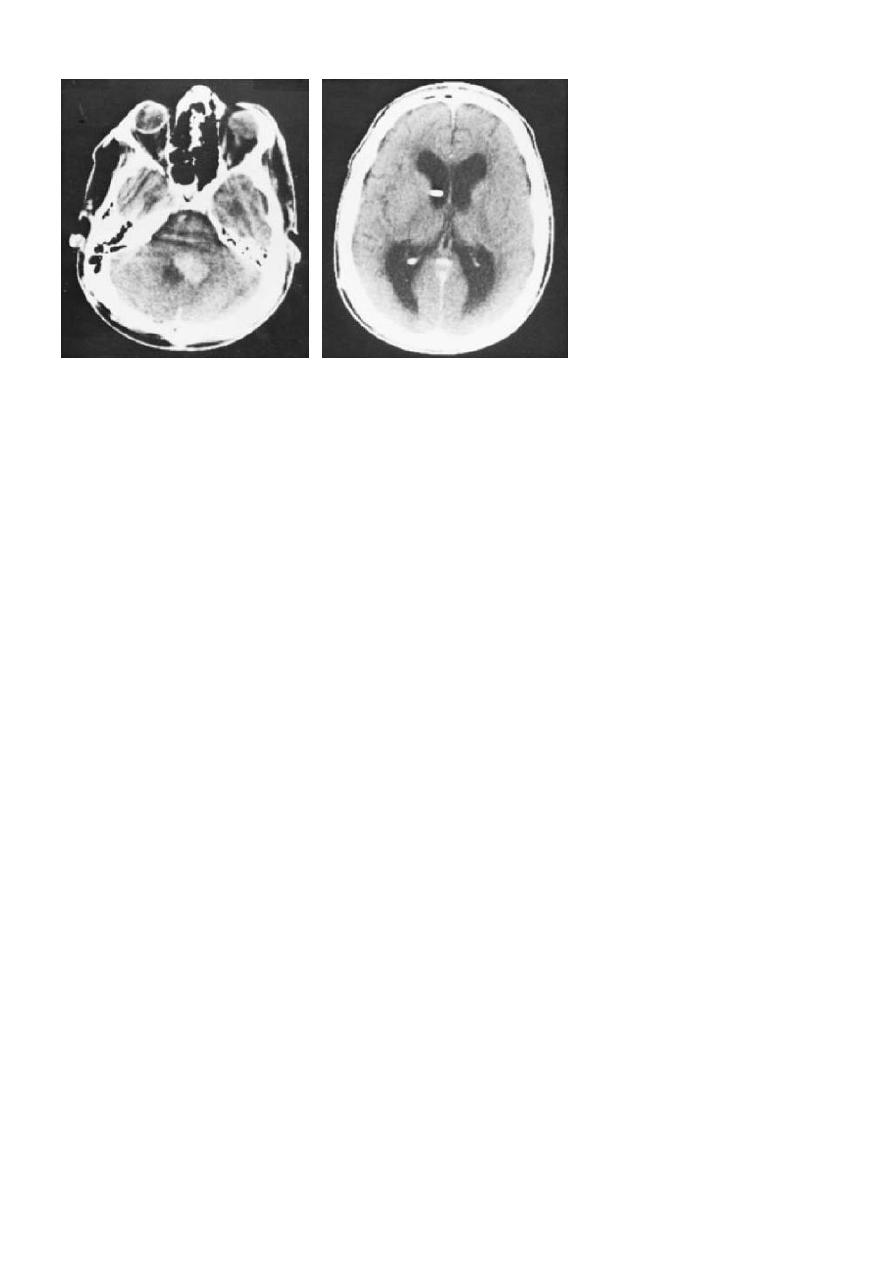
Ependymoma growing out of the fourth ventricle
Astrocytoma
the most common category of neuroepithelial tumor, has the following histological
subtypes
Glioblastoma multiforme
Is the most malignant grade of astrocytoma (grade IV astrocytoma). This most common and
most malignant tumor of the cerebral hemispheres usually arises between the ages of 40
and 60. It grows by infiltration into brain tissue and is thus nearly impossible to resect
totally, as nests of tumor cells nearly always remain beyond the margins of resection even if
all macroscopically evident tumor tissue is removed. Though it generally arises in a single
hemisphere, it can infiltrate across the corpus callosum into the opposite hemisphere,
creating a so-called butterfly tumor.
Glioblastomas grow rapidly, causing rapidly progressive clinical manifestations; they are,
therefore, usually diagnosed within a few weeks or (at most) months of the onset of
symptoms.
Focal neurological and/or neuropsychological deficits arise first, sometimes accompanied
by epileptic seizures, soon followed by general manifestations of intracranial hypertension .
The diagnosis can be made with a fair degree of confidence from the typical appearance in
neuroimaging studies , though this does not obviate the need for histological examination
of tumor tissue. CT characteristically reveals a central hypodense area, corresponding to
necrosis in the interior of the tumor. There may be hyperdense areas indicating
intratumoral hemorrhage. Peritumoral brain edema is often extensive, causing mass effect
and midline shift. Ringlike enhancement is seen after the administration of contrast
medium.
6
Even with the best currently available treatment, i. e., gross total resection of the tumor
with or without adjuvant radio- or chemotherapy, patients with glioblastoma survive only a
few months, or a few years at most, because of the nearly inevitable recurrences.
Grade III astrocytoma , is another type of histologically malignant astrocytoma. The
prognosis of patients with this type of tumor, though marginally better than that of
glioblastoma patients,is still poor.
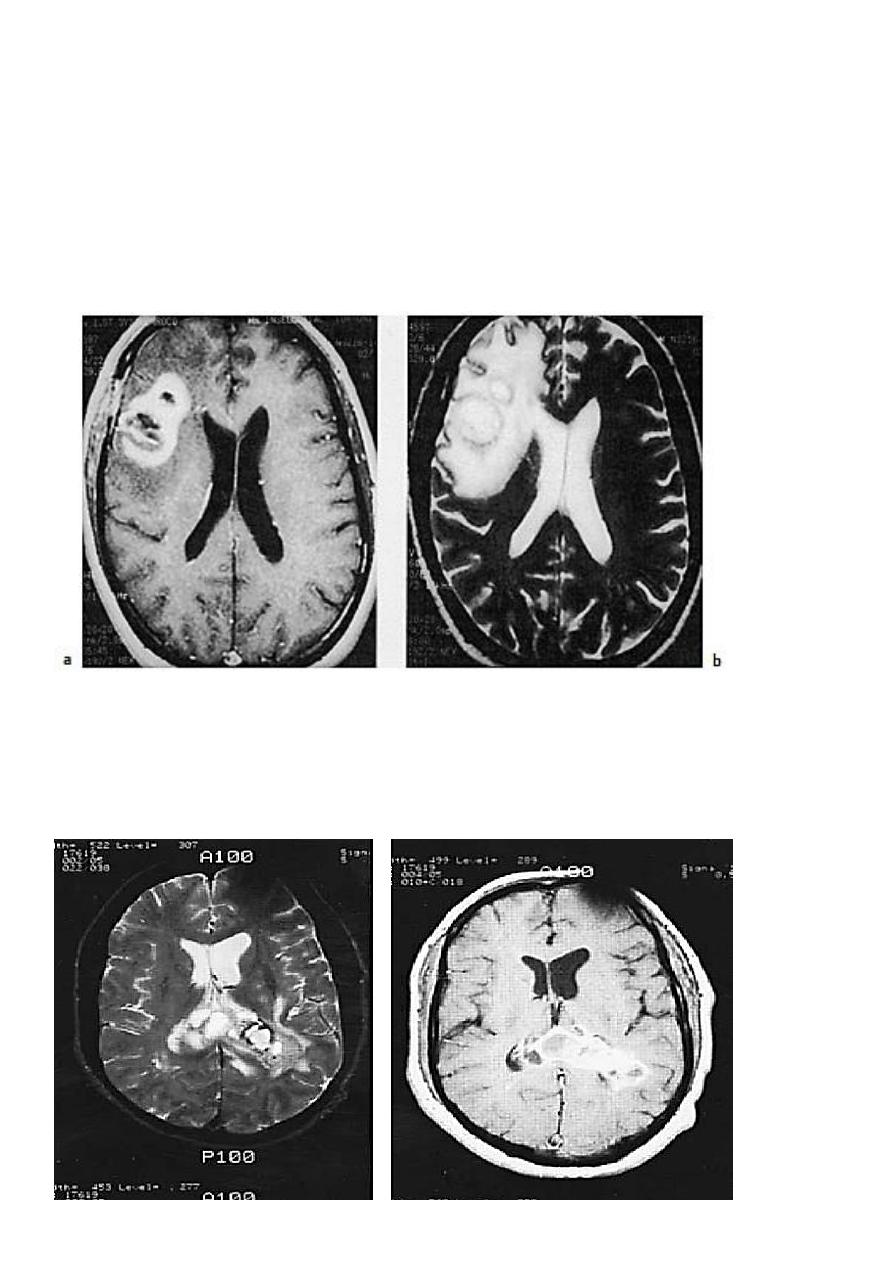
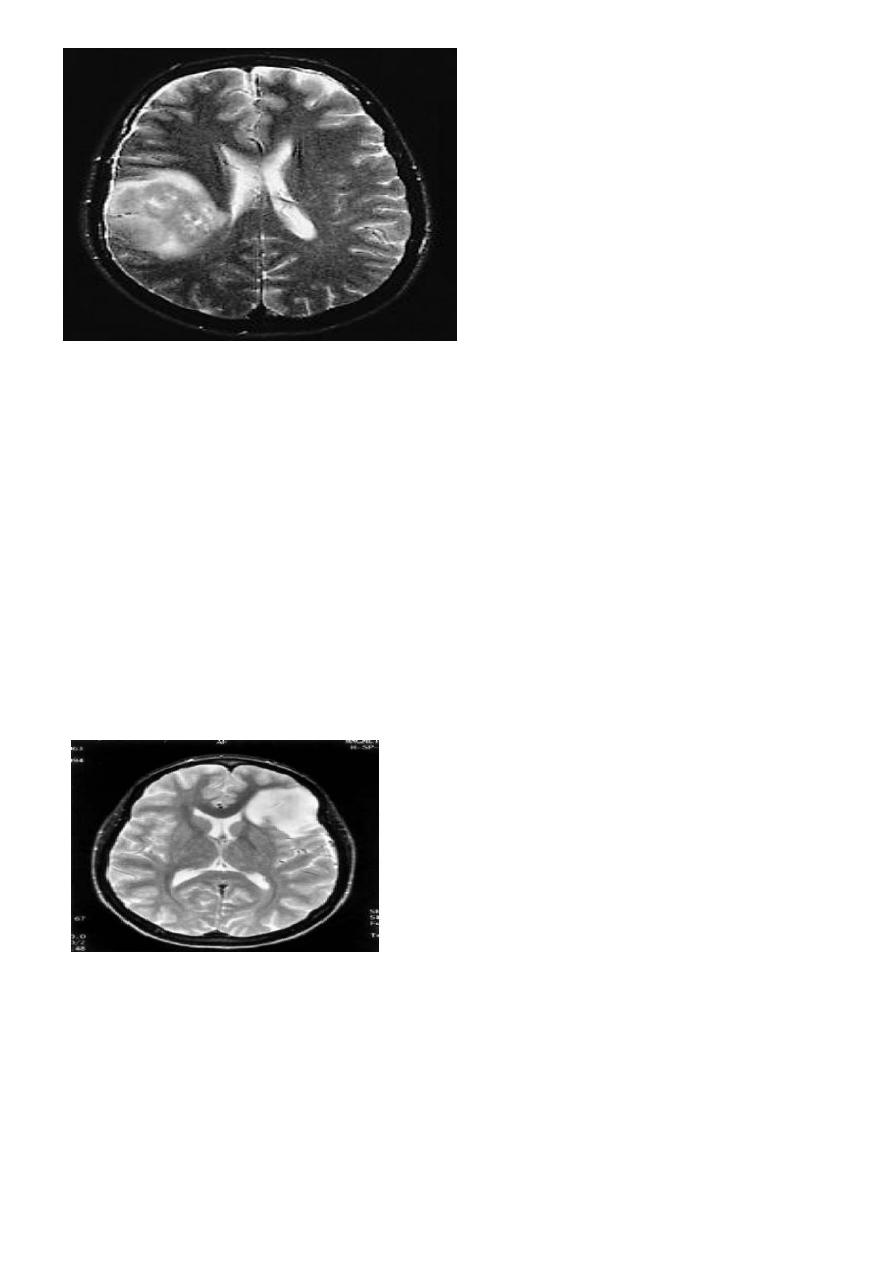
Glioblastoma multiforme in theright frontal lobe. The T1- and T2- weighted spin-echo
images (a and b,respectively) reveal a polycystic tumor surrounded by marked edema.
MRI illustrate a large tumor deep within the left cerebral hemisphere and extending
through the corpus callosum to the right hemisphere.
The black rim around a portion of the tumor (left) represents hemorrhage.
7
Grade III astrocytoma (partly cystic) in the
right parieto-temporal region, as revealed
by MRI.
Grade I and II astrocytomas
Generally affect adults aged 30 to 40. Though these tumors displace & infiltrate the
surrounding brain tissue, they are better demarcated from it than glioblastoma; they often
grow quite slowly, sometimes over many years. Their clinical manifestations include
behavioral and neuropsychological changes, increasingly severe focal neurological deficits
(e. g., hemiparesis), focal or secondarily generalized epileptic seizures, and signs of
intracranial hypertension.
If epileptic seizures are the only manifestation, tumor resection may be useful for seizure
control, if the location of the tumor permits. After a tumor is totally resected, it may not
recur until years later.
Astrocytoma of the left frontal lobe; the T2-
weighted MRI, shows an infiltrating tumor with
minimal mass effect and slight edema.
Cerebellar astrocytoma
Is considerably more benign than the other varieties, usually affects children aged 5 to 15
,and is well demarcated from the surrounding brain tissue. It is usually found in the
cerebellar hemispheres or vermis and may extend into the pons.
Its main clinical manifestations are thus ataxia, disequilibrium, nystagmus, and, often, signs
of intracranial hypertension (esp. papilledema) secondary to occlusive hydrocephalus.
8
Total resection often results in permanent cure. Brainstem astrocytoma is usually
inoperable, though tumors of this type are sometimes at least partly re-sectable in special
cases.
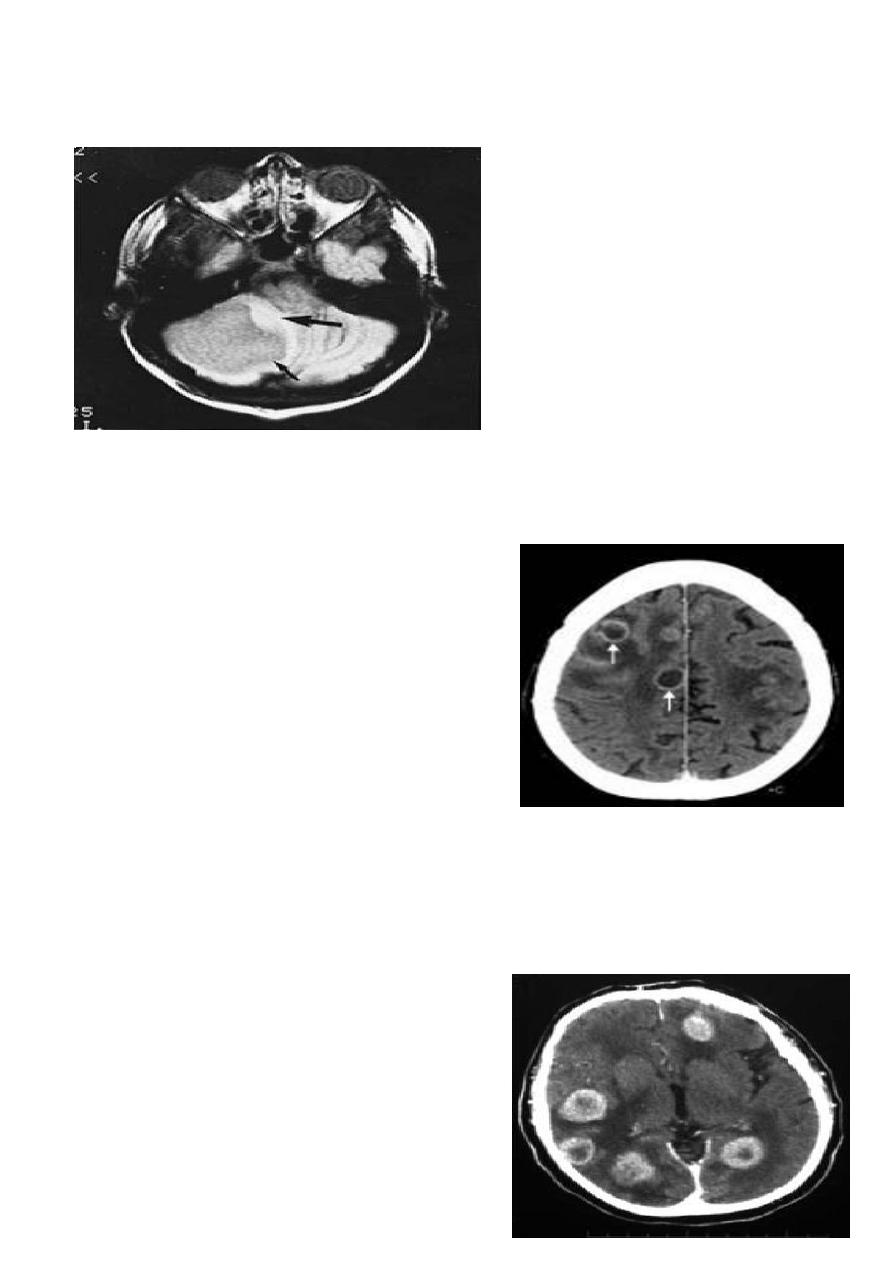
Cystic astrocytoma of the cerebellum.
MRI demonstrates the
large cystic component of the tumor
(smaller arrow) and the solid tissue
component (larger arrow)
Brain metastases
Account for about 15% of malignant brain tumors.
The most common source of a brain metastasis is
bronchial carcinoma in men and carcinoma of breast
in women.
Brain metastases sometimes produce symptoms
before the primary tumor does; in such
cases,multiple brain metastases are usually already
present, even if only a single one is apparent on the
neuroimaging study.
Generally speaking, surgical resection makes sense only for solitary metastases and the
surgical indication should always be carefully considered in the light of the extent of
disease. Only about 20% of patients so treated live more than five years after the operation
and postoperative radiotherapy, if they have not already died of the effects of their primary
tumor.Brain metastases usually produce extensive peritumoral edema and often cause
epileptic seizures; thus, corticosteroids and
antiepileptic drugs can be given for palliation. This
usually brings a substantial, if only temporary,
clinical improvement.
Multiple metastases from bronchogenic
carcinoma. Each lesion is surrounded by edema

9
Hydrocephalus
Obstruction to the CSF circulation leading to dilatation of the ventricular system.
Communicating H. :the obstruction lies outside the ventricular system.
Non-communicatin H. : the obstruction is within the ventricular system .
Causes of hydrocephalus
Communicating (obstruction outside
ventricular system)
Bacterial meningitis (especially tuberculous(
Sarcoidosis
Subarachnoid haemorrhage
Head injury
Idiopathic ('normal pressure)
Diversion of the CSF by means of a shunt procedure between the ventricular system and
the peritoneal cavity or right atrium may result in prompt relief of symptoms in obstructive
or communicating hydrocephalus.
NORMAL PRESSURE HYDROCEPHALUS
In this condition the dilatation of the ventricular system is caused by intermittent rises in
CSF pressure, which occur particularly at night.
It occurs predominantly in old age and is suggested by the combination of gait apraxia and
dementia, often with urinary incontinence as an early feature. This cause of dilatation of
the ventricles can be very difficult to distinguish from that occurring due to cerebral
atrophy, where the cortical sulci are also dilated.
The result of shunting procedures for normal pressure. hydrocephalus is unpredictable
Non-communicating (obstruction
within ventricular system)
Tumours
Colloid cyst
Arnold-Chiari malformation
Aqueduct stenosis
Cerebellar abscess
Cerebellar or brain-stem
haematoma

11
IDIOPATHIC INTRACRANIAL HYPERTENSION
This condition, previously known as 'benign intracranial hypertension' and 'pseudotumour
cerebri', usually occurs in obese young women. Raised intracranial pressure develops
without a space-occupying lesion, ventricular dilatation or impairment of consciousness.
The aetiology is uncertain but there may be a diffuse defect of CSF reabsorption by the
arachnoid villi.
The condition can be precipitated by drugs, including tetracycline, and rarely vitamin A,
retinoids.
Clinical features
The usual presentation is with headache, sometimes with transient diplopia and visual
obscurations. There are usually no signs other than papilloedema, which may be discovered
incidentally, but a 6th nerve palsy may be present.
Investigations
The CT is normal, with normal-sized or small ventricles. Once this has been demonstrated, a
lumbar puncture is safe and will allow confirmation of the raised CSF pressure and form
part of treatment.
MR angiography or cerebral venography will exclude cerebral venous sinus thrombosis or
stenosis of other cause. True papilloedema may need to be distinguished from other causes
of disc swelling by fluorescein angiography.
Management
Any precipitating condition should be sought, relevant medication should be withdrawn
and a weight-reducing diet started, if indicated.
The carbonic anhydrase inhibitor, acetazolamide, may help to lower intracranial pressure.
Repeated lumbar puncture can be considered, but is often unacceptable to the patient.
Patients failing to respond, in whom chronic papilloedema threatens vision, may require
optic nerve sheath fenestration or a lumbo-peritoneal shunt.
In patients with fixed stenosis of the transverse sinus, stenting may be helpful .
