Hematology part II
BLEEDING TENDENCYCOAGULATION PROCESS
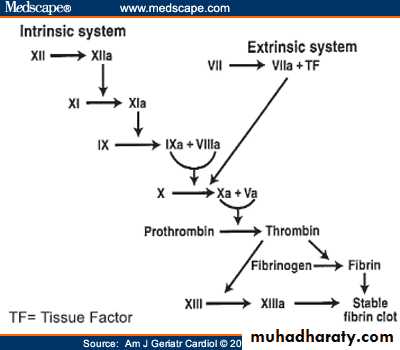
Normal mechanism are vascular response , tissue response, platelets plug formation, and activation of fibrin to stabilize the platelet plug. Following a vascular injury, vasoconstriction and platelets adhesion to the sub -endothelial exposed collagens by the effect of von willebrand factor vWF which is released from the endothelial cells .Platelets then with the help of tissue ADP aggregate and then it require fibrin for stabilization of the plug. This fibrin come from series of cascade coagulation by activation of the factors by intrinsic and extrinsic pathways. Usually the process is initiated by the tissue factor (extrinsic) pathway.
Coagulation cascade
Clotting cascade
Intrinsic pathway(APTT)Exrinsic pathway( PT)
FXII activateTissue Factor
FXI--FXIa
With help of Ca++..ACTIVATE
FXIa –activate;….FVII---FVIIa
FIX---IXa;Actvate ;….
FVIIa acivate FX
With help of FVIII………….FX---F Xa; activates; with help of Ca,&F V
Tested by APTT
Prothrombin (FII) to Thrombin (FIIa)activates;…..
COMMON PATHWAY TESTED BY PT,&APTT
Fibrinogen (F1
To …………………
Fibrin stabilize platelets plug
Clot stabilized with FXIII
coagulations
Coagulation factors of the plasma intrinsic and extrinsic are all produced by the liver except VWF which is released by the endothelial cellsBleeding is in many forms ;as purpura,petechiae,hemoarthrosis, intramuscular,epistaxis or GIT bleeding etc….
Family history of bleeding tendency, and age of onset and the physical examinations are important in the evaluation.
Presentations: Hemophilia is in males and usually detected during circumcision in the neonate and hemoarthrosis later on. Von willebrand disease VWD usually present later as in adolescent as epistaxis or menorrhagia. Idiopathic thrombocytopenia in childeren as purpura and petechiae.
Bleeding is either due to platelets deficiency or dysfunction,
or due to plasma coagulation factors deficiency,
or may be due to ; vessels defect in its integrity like vasculitis or meningococcemia.
Approach to the diagnosis
Child with bleeding as purpura or joints should be evaluated first by history and physical examination and then by investigations.Purpura is defined as bleeding into the skin ,as purple spot or become bluish which not blanch on pressure, either as pin point <2 mm called petechiae or purpura 2-10mm,or ecchymoses or bruises when>1cm diam. Purpura may be palpable as in case of vasculitis as in Henoch-schonlein purpura.
Investigations to start with are ;Full CBC and smear looking to platelets ,bleeding time BT (1-9min), prothrombin time PT (12-14 sec),and activated partial thromboplastin time APTT(32-38 sec).platelet function analysis PFA;is now replace the bleeding time. (BT,PT,APTT,platelets count)
Approach to the diagnosis
If the bleeding time or PFA is prolonged; then thrombocytes count or function ,or adhesion problem due to VWD is the cause of purpura. If platelets are low :it is ITPIf the BT is prolonged, platelets count normal,PT,APTT are normal then should go to platelet function analyser to see aggregation defect as in Glanzman disease(rare AR disease)
or drugs like aspirin. or adhesion defect as in VWD due to vWF deficiency.
If the bleeding time BT is normal, PT prolonged then suspect factorsX,VII,V,II, may be deficient ,as in liver disease or vit K deficiency or use of warfarin.
If BT , PT, are normal , APTT prolonged then think of factor of intrinsic pathway as hemophilia A(FVIII)& B (FIX),or FXI,def.
If BT normal,PT and APTT prolonged then think of FX,FV,FII,FI def.
Factor assay to detect the concerned factor to give exact factor deficiency.
Bleeding approach
Hemophilia A is sex linked due to FVIII deficiency. Present with recurrent bleeding in the joint and muscles, is more common than hemophilia B(FIX).may lead to crippling joints due to repeated hemoarthrosis.It has 3- types of severity.
Severe ;factor VIIIC (C:coagulant part), is<1% level in the plasma. spontaneous bleeding in joints and muscles
Moderate severe FVIII ; 1-5% bleed after minor trauma
Mild .FVIII 5-40% in the plasma. bleeds after surgery.
-----------------------------------------------------------------------
BT; is normal, PT is normal,But APTT is prolonged. Factor assay to estimate the level in plasma .
Management of hemophilia
Avoid intra muscular injections ,aspirin and NSAID.Mild cases can be treated by infusion of desmopressin(DDAVP) to stimulate the release of vwf from endothelial cells which hold the FVIIIC in the blood for a longer time.Can help in minor surgery.
In severe low level of FVIIIC, we needs to give recombinant FVIII concentrate to elevate the plasma factor level as needed according to the condition or surgery and the needed plasma level and the duration of elevated plasma level needed, and can be given as regular maintenance i.v infusion to keep the level above 2% to prevent recurrent hemarthroses. each 1 unit /kg, elevate the plasma level by 2% .
VON WILLEBRAND FACTOR ; VWF
Vwf is plasma big molecule produced by endothelial cells and is responsible for catching the FVIII (coagulant part:c ) in the plasma by one end and prevent its rapid degradation from plasma, and it also by another end it hold the platelet and bring it to the exposed subendothelial collagen to help for clot formation it can be detected by assay for vwf antigen VWFag. Its absence leads to adhesion defect in the platelets and so it prolong BT,and leads to the von willebrand disease VWD.and FVIIIC will rapidly disappears from plasma and may give prolonged APTT, and reduction in plasma level of FVIIIc .Low plasma level of vWF give low FVIIIag,but normal FVIIIc level.VWD von willebrand disease
It is autosomal disease, presenting as mucosal bleeding like epistaxis, menorrhagia or purpura or prolonged bleeding after surgery. No hemoarthrosis.BT is prolonged, APTT normal, PT normal ,vwf antigen assay; (estimate its concentration) decreased, ristocitin co-factor(RiCoF) (activity) reduced, FVIII normal or decreased. Many types of VWD as a result of different gene mutations. The commonest one is type 1(60-80 %) usually diagnosed later childhood and is autos. dominant.
Treatment is to give DDAVP ,for mild bleeding, or give plasma-derived FVIII concentrate ,which cannot produced by recombinant way ,it should be with FVIII because it hold it in the plasma.. Also same advice to the pt, not to have intramuscular injection or aspirin or NSAID.
Other coagulation factor deficiency are rare like FV,FVII,.
Idiopathic thrombocytopenic purpura(immune thrombocytopenia)
Defined as isolated low platelets count due to peripheral (splenic sequestration ) consumption with rapid reduction in its count , so its life span is reduced although bone marrow megakaryocytes are active and normal, as a result of autoantibodies against the platelets of IgG type, formed 2-3 weeks after of viral infections as URTI It presents as purpura and petechiae , epistaxis .Platelets count (normal count 150-250x10*9/l) leading to spontaneous purpura when its count reaches below20x10*9/l .Intracranial bleeding can occur if <10x10*9/l. other forms of bleeding is mucosal or intestinal. It is either form with spontaneous remission over 2 months or chronic form more than 6 months . It affect children above 2 years and older. More than 80% of children will remit within 2-8 weeks but others go into chronic condition.
Rate of intracranial hemorrhage is 0.5-1% of cases
Diagnosis of ITP
First history ,of previous viral infectionPhysical examination with otherwise healthy looking child and absence of hepatosplenomegaly or lymphadenopathy or anemia or bone pain that are clues for leukemia. so diagnosis by exclusion of other conditions like malignancy or bone marrow suppresion or SLE. SO first step is to be sure that thrombocytopenia present by blood test and second to be sure that it is isolated and idiopathic.
Complete blood count and blood film to see reduction in platelets and absence of immature leukocytes; as to exclude leukemia. Otherwise you may need bone marrow examination in atypical cases, and especially if we are going to treat by corticosteroids, because steroids lead to masking the diagnosis if it is used in case the condition is leukemia and not ITP, and it add more harmful morbidity to management of leukemia if steroid used. Thrombocytopenia when platelets count<150x10*9/l.
Normal range for platelets is 150-250 x10*9/l
Bleeding time; prolonged more than 9 minutes
Grades
Mild thrombocytopenia ;platelets 50-150x10*9/l.It has no obvious bleeding ,no risk unless operation or severe injury.Moderate;20-50 count, still low risk for spontaneous bleeding, but only in trauma or operation.
Severe thrombocytopenia; when count is less than 20 x10*9/l. high risk of spontaneous bleeding.
management
Abou 80% of cases are acute and benign self limiting and remitting within 6-8 weeks spontaneously.Treatment is indicated for; severe bleeding like intracranial, GI,bleeding or very low count like <20x10*9/l ,or some have distressing recurrent minor bleedings like epistaxis or menorrhagia.This treatment includes lines;
1.Steroids oral for 2 weeks or injection; for rapid increase in platelet count
2.Or IVIG , or anti-D,for Rh +ve patient unsplenectomized.all three drugs has side effects,as anti-D may cause hemolysis, IVIG,cause hemiplegia and immunosppresstion.
3.Third line is monoclonal antibody; Rituximab.
Platelet infusion in severe condition may be given to raise platelet count just for few hours.
4.Splenectomy in chronic cases, and in refractory to other lines of medical therapy.
5.Thrombopoeitin receptor agonist is now given to relapses after splenectomy; e.g; Romiplostim .
Disseminated intravascular coagulation DIC
Disorder of severe stress conditions like septicemia or hypoxia or poisoning or trauma characterized by intravascular thrombosis by multiple disseminated thrombi due activation of clotting process leading to diffuse fibrin depositions in small vessels and consumption of the fibrin and the clotting factors, ultimately leads to bleeding as purpura, from venous cannula, GI, intracranial, so on. With prolonged PT, APTT, and increased fibrin degradation products tested by D-dimer test. It is serous condition and needs prompt treatment of bleeding by; fresh frozen plasma and platelets and treat the underlying cause like the meningococcemia, shock….
thrombosis
Thrombosis in children is uncommon it may leads to venous thrombosis; are due to congenital inherited deficiency of anti thrombotic factors like;protein C def.
Protein S def.
Anti-thrombin def.
Factor V Leiden presence.
Acquires causes like;
Catheter insertion, DIC, congenital cyanotic heart disease, SLE.
Diagnosis is to do screening for congenital causes and acquired causes , after history and assessment of the thrombotic problem.
Malignancyleukemia and solid tumors
Uncommon, but affect 1 in 500 by 15 year of age. Over all 5-year survival is 75%.leukemia is the most common malignancy in children followed by brain tumors ,then solid tumors like, Neuroblastoma, Willms T. lymphoma, bone tumors and retinoblastoma .Preschool age ,< 5yr; ALL, Neuroblastoma,Willms retinoblastoma.
School age; ALL, brain tumor.
Adolescent; ALL, Hodgkin lymphoma, bone tumor
Presentation of malignancy
Raised intracranial pressure in brain tumor.White pupillary reflex in infant with retinoblastoma or squint.
Enlarged Lymphnodes in the neck and widenning mediastinum in lymphoma and may have abdominal masses or anemia.
Loin mass with hypertention or hematuria in otherwise healthy looking child as in willms tumor.
In neuroblastoma as loin mass ,pallor, bone pain.
Acute lymphoblastic anemia ALL.as pallor petechiae,bruises ,infection ,fever, bone pain,hepatosplenomegaly,lymphadenopathy,lethargy.
Aetiology of malignancy
Most cases the cause is unknown but environmental factors and genetic susceptibility as certain genes like in bilateral retinoblastoma with a gene mutation in chrom. 13 , in Down syndrome and leukemia, in neurofibromatosis and glioma of the brain,
Viral infections,genetic predisposition and exposure to radiation.
investigations
Bone marrow ex. for leukemia,neuroblastomaU.S , PAIN X-R,CT SCAN ,MRI SCAN,BIOPSY,
Nuclear medicine imaging methods; to localize bone, bone marrow, and lymph nodes metastases.
management
Chemotherapy, surgery,and radiotherapy. Child and parents should be seen and explained the problem in a realistic way and what to do and the expectations.chemotherapy and radiotherapy ; have side effects upon the immunity for infections specially measles and varicella. And have susceptiblity to opportunistic microorganisms like fungi, staph. coagulase-ve, pneumocystis carinii(fungus) in lung specially in leukemic pt. and may affect the fertility.
Bone marrow supression due to chemotherapy leads to; anemia,neuropenia,thrombocytopenia,so infections bleeding, Gut mucosal damage, alopecia, anorexia.
leukemia
Acute lymphoblastic L. account for 80%of leukemia in children. Other are acute myeloid L.,chronic myloid leukemia.Presentation of ALL peaks at 2-5 yr. as general ill-health,bruises,epistaxis, fever, pallor, either over several weeks or more rapid progression.
Full blood count is abnormal as low HB, thrombocytopenia, circulating blast cells.
Bone marrow is essential and to do immunological and cytological B.M. cell examination to identify the exact leukemia type, which give the idea about the prognosis.
CXR is required to see a mediastinal mass of T-cell leukemia .
Lumber puncture to detect CNS invasion by leukemic cells.
classifications
Both ALL and AML are calssified by morphology.immunological workup to further classify the cells into subtypes;
common ALL(c ALL);75%.T-cell leukemia. 15%,prognosis and clinical presentation, and response to therapy depend upon subtypes.
Prognostic factors in acute leukaemia ; high risk are;
age <1yr or >10 yr
Sex; male
Tumour load>50x10*9/l
Hypodiploidy <44 chromosomes in tumour cells
Persistence of leukemic blast cells in initial therapy.
Outline treatment
A)Induction ; by vincristine,dexamethasone,IT methotrexate for first 5 weeksB)Consolidation and CNS protection by intrathecal methotrexate, vincristine, steroids, for3 weeks,
C)Maintenance therapy for 2 yrs in girl and 3 yr in boys; by monthly vincristine,pulsed steroids for 5 days, daily 6- mercaptopurine, IT methotrexate, weekly oral methotrexate plus prophylactic
co-trimoxazole for pneumocystis carinii along the maintenance .
NON-HODGKIN LYMPHOMA
T- cell malignancy may be acue leukemia or lymphoma both characterised by mediastnal mass wih bone marrow infiltration.B-cell lymphoma present with cervical lymphadenopathy or abdominal mass. Abdominal disease present with pain or intussusception.Biopsy,radiological exam. by CT scan or MRI can localise the sites.Multiagents chemotherapy needed.80% survival for T-cell and B-cell lymphoma.Hodgkin lymphoma is rare ,and is commonly found in adolescent.
neuroblastoma
Tumor of neural crest from emberyonic cells in adrenal gland and sympathetic chain from neck to pelvis. Usually affect children <5 yr .It is highly malignant except in infant < 1yr spontaneous remission occur. Present with pallor, weight loss, abdominal mass in one side or crossing ,bone pain, hepatomegaly.It rapidly invade bone marrow and vertebrae,or LNs. Catecholamines can be detected in the urine and used as screening .Diagnosis is by bone marrow examination for metastatic invasion.Chemotherapy, surgery or radiotherpy help to cure 30% of cases.Wilms tumour(nephroblastoma)
Malignant ,affect children below 5 yr.Most pts present with a large abdominal mass discovered accidentally in otherwise well child. US.CT scan, MRI, needed for diagnosis showing renal mass confined within the renal capsule.
Metastasis to near tissues or lung or even other kidney. Usually chemotherapy started first followed by histological staging and delayed nephrectomy.Radiotherapy for advanced disease prognosis with treatment is good ;80% cure rate
Brain tumour
Always primary ,are the leading cause for death from solid tumors. It is 60% infra-tentorial.Astrocytoma40%,medulloblastoma20%,ependymoma8%,
brain stem glioma6%,craniopharyngioma 4%. Presentation with signs of intracranial hypertensions as; headache, seizures, vomiting, focal neurological signs.
Persistent back pain in children is significant and need MRI,due to spinal tumor or metastasis.
CT scan, MRI, of the brain is diagnostic .Lumber puncture should not be done if suspicion of brain tumor or intracranial hypertension.
Surgery is usually the first treatment but chemotherapy and radiotherapy may be used in certain type or tumour.