
1
Fifth stage
Dermatology
كتابة الطالب
.د
عمر
2015/11/10
Important questions for dermatology
Lec1: للعملي
Q: Enumerate and define the primary and secondary lesions? من المحاضرة
=================================================================
Lec2:
Q: Define psoriasis?
Psoriasis is a genetic, immune-mediated skin and/or joint inflammatory disease in which
intralesional inflammation stimulates basal keratinocytes to hyperproliferate.
Q: Which drugs are contraindicated in psoriasis?
Lithium
Antimalarial agents
Beta blocking agents
Systemic steroids
Interferon
Q: What are the comorbidities associated with psoriasis?
Patients with psoriasis are at a higher risk for the following comorbidities than is the
general population:
1. Crohn’s dis. and UC (3.8 to 7.5 times); families with MS.
2. Cardiovascular disease
3. Metabolic syndrome???
4. Lymphoma (1.5 to 3 fold); non-melanoma skin cancer (250 PUVAs – 14 fold SCC)
5. Depression/suicide
6. Psychological/sexual dysfunction
7. Smoking
8. Alcohol

2
9. Obesity
10. Quality of life
Q: What are the clinical patterns of psoriasis? Write about most common one.
A. Variations in the morphology of psoriasis:
Chronic plaque psoriasis
Guttate psoriasis
Pustular psoriasis
Erythrodermic psoriasis
Light-sensitive psoriasis
HIV-induced psoriasis
Keratoderma blennorrhagicum (Reiter syndrome)
B. Variations in the location of psoriasis:
Scalp psoriasis
Psoriasis of the palms and soles
Pustular psoriasis of the palms and soles
Pustular psoriasis of the digits
Psoriasis inversus
Psoriasis of the penis and Reiter syndrome
Nail psoriasis
Psoriatic arthritis
The most common one is Chronic plaque psoriasis
Chronic, noninflammatory, well-defined plaques.
The plaques are irregular, round to oval.
Predilection for extensor surfaces such as the elbows and knees but any site can be
affected.
Silvery scale.
Tend to be symmetrically distributed.
Plaques enlarge and then tend to remain stable for months or years.
A temporary brown, white, or red macule remains when the plaque subsides.
Auspitz sign!!!
Q: What is the primary lesion in psoriasis?
Well demarcated, bright red, scaly, plaques.

3
Q: What are the precipitating factors of Erythrodermic psoriasis?
Precipitating factors include the administration of systemic corticosteroids; the excessive
use of topical steroids; use of tar and anthralin on acutely inflamed plaques; abrupt
discontinuation of systemic therapy; phototherapy complications; severe emotional stress;
infection.
Q: What are the nail changes in psoriasis?
Onycholysis separation of the nail plate from the nail bed.
Subungual hyperkeratosis
Pitting
Oil spot sign
Nail dystrophy
Q: Enumerate the clinical types of rheumatic psoriasis and talk about the most common
one?
Oligoarticular assymmetric arthritis
Polyarticular symmetric arthritis (RA-like)
Distal interphalangeal joint predominant
Destructive polyarthritis (arthiritis mutilans)
Ankylosing spodylitis and sacroiliitis
The most common one is Distal interphalangeal joint predominant: Mild, chronic, not
disabling, and associated with nail disease. Involves hands and feet. This is the most
characteristic presentation of arthritis with psoriasis.
Notes:
Skin is the largest organ in the body (17% of body weight).
There is no cure for psoriasis.
Psoriasis lead to inflammation in the skin, nails, and joints.
Psoriasis only lead to inflammation of nails in 30%.
Psoriasis + arthritis lead to inflammation o nails in 80%.
Auspitz sign عندما نحك مكان المرض يخرج دم elected by doctor.
Guttate psoriasis it is acute form of psoriasis and it is self-limited.
Erythrodermic psoriasis it is iatrogenic (caused by corticosteroids).
Penis is the most common site of psoriasis in male.

4
Hair lines is the most important site of psoriasis.
Kobner phenomena (slide 34) skin lesion that develops at the center of skin trauma.
=================================================================
Lec3:
Q: Write short notes about treatment of psoriasis:
If the affected body surface area below 20% use topical treatment like topical
steroids, pentocam, topical vitamin D3 analogue (Calcipotriene), Lubricants or lotions.
If the affected body surface area above 20% use systemic treatment like
Methotrexate, Acitretin, Cyclosporine, light therapy (lead to immunosuppression)
PUVA, UVB, UVA1.
You can use biological dugs infliximab, rituximab.
Also you can use immunosuppressive drugs (methotrexate).
Q: What are the side effects of PUVA?
Long term side effects (most of which are dose-dependant):
Skin tumors:
PUVA promotes skin aging, actinic keratoses, and squamous cell carcinoma (SCC).
Risk of genital tumors in males with exposure to PUVA and UVB.
Approximately 15 years after the first treatment with PUVA, the risk of malignant
melanoma increases, especially among patients who receive • 250 treatments or more.
Lentigines. Small black macules occur in PUVA-exposed sites.
Cataracts. The incidence seems to be very low if eye protection is used during the first
two days of PUVA treatment (from the time the drug is ingested until the end of the
following day).
Short-term side effects include dark tanning, pruritus, nausea, and severe sunburn.
Q: What are the drugs used in treatment of psoriatic arthritis?
Non-steroidal anti-inflammatory drugs
Intra-articular steroid injections
Methotrexate
Biologics
Cyclosporine
PUVA
5
Q: Write short notes about pityriasis rosea?
Pityriasis rosea (PR) is a common, benign, usually asymptomatic, distinctive, self-
limiting skin eruption of unknown etiology.
There is some evidence that human herpesvirus 6 (HHV-6) and 7 (HHV-7) may be
involved.
More than 75% of cases occur between 10 and 35 years of age with an age range of 4
months to 78 years.
Recurrence rate is about 2%.
The incidence is higher during winter time.
Upper respiratory tract infection occurs before the eruption in about 70% of cases.
Q: What is the primary lesion in pityriasis rosea?
Pink, ovale, plaques, scales.
Q: What are the Differential diagnosis of pityriasis rosea?
Secondary syphilis
Guttate psoriasis
Viral exanthems
Tinea corporis
Nummular eczema
Drug eruptions
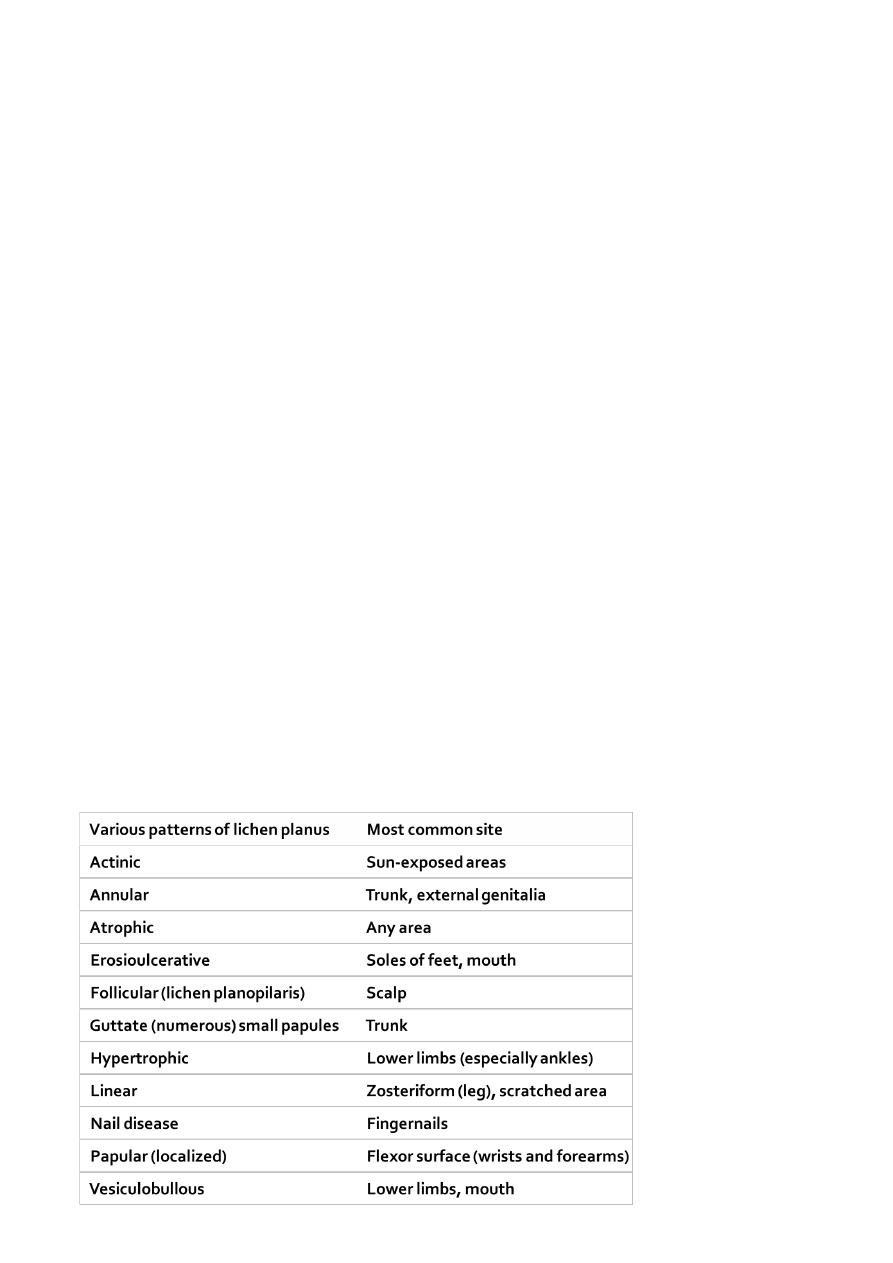
Q: Enumerate the clinical types of Lichen planus, and write about most common one?

6
Most common one is Localized LP:
• Papules are most commonly located on the flexor surfaces of the wrists and
forearms, the legs immediately above the ankles and the lumbar region.
• Itching is variable; 20% of patients with LP do not itch. Itch does not necessarily
correlate with disease severity.
• The course is unpredictable. Some patients experience spontaneous remission in a
few months, but the most common localized papular form tends to be chronic and
endures for an average of approximately 4 years.
Q: What is the treatment of lichen planus?
THERAPY FOR CUTANEOUS LICHEN PLANUS
Topical steroids
Intralesional steroids
Systemic steroids
Acitretin
Azathioprine
Cyclosporine
Antihistamines
Light therapy
PUVA (psoralen + UVA light) and broadband and narrow-band UVB therapy.
Tacrolimus ointment: Ulcerative lichen planus of the sole may respond to topical
tacrolimus 0.1% ointment.
THERAPY FOR MUCOUS MEMBRANE LICHEN PLANUS
The course of oral and vaginal lichen planus can extend for years.
Consider a biopsy to establish the diagnosis.
Most patients are asymptomatic (non-erosive type) and do not need treatment.
Tacrolimus ointment and pimecrolimus cream.
Corticosteroids (topical, systemic and intralesional)
Dapsone
Hydroxychloroquine
Azathioprine
Mycophenolate mofetil
Q: What is the primary lesion in lichen planus?
Th five Ps rule of lichen planus: pruritic, planar (flat-topped), polyangular, purple papules.

7
Notes:
Pytriasis rosea النخالة الوردية
Location of pytriasis rosea lesion it is located in the trunk and proximal extremities.
Etiology of pytriasis rosea is unknown.
Treatment of pytriasis rosea topical steroids + systemic anti-histamine.
Pytriasis rosea is self-limited.
Lichen planus حزاز منبسط
Lichen planus Affect skin, mucus membrane (mouth and vagina), nails.
Lichen planus 10 % familial predisposition.
Lichen planus self limited, may reoccur.
Slide 31 Wickham's striae.
Patient may remains with permanent hyperpigmentation (slide 34).
Mucus membrane in lichen planus mouth and vagina could be erosive (slide42),
or non-erosive (slide41).
Penis is very common site in lichen planus.
Psoriatic arthritis always affect the DIP joints.
=================================================================
Lec4:
Q: What is the active border of fungal infection?
One very characteristic pattern of inflammation is the active border of infection.
The highest numbers of hyphae are located in the active border, so samples are taken
from here.
Typically the active border is scaly, red, and slightly elevated.
Vesicles appear at the active border when inflammation is intense.
This pattern is present in all locations except the palms and soles.
Q: Enumerate the types of tenia pedis and discus the most common one?
The classic “ringworm” pattern
Interdigital tinea pedis (toe web infection)
Chronic scaly infection of the plantar surface
Acute vesicular tinea pedis
The most common types Interdigital tinea pedis (toe web infection)
The web between the fourth and fifth toes is most commonly involved.
Tight-fitting shoes are a predisposing factor.
8
The toe web can become dry, scaly, and fissured or white, macerated, and wet.
The bacterial flora is unchanged in the dry scaly pattern.
The macerated pattern occurs from an interaction of bacteria and fungus.
Extension out of the web space onto the sole or dorsum of the foot is common.
Q: Write short notes about second most common types of tenia pedis?
Chronic scaly infection of the plantar surface:
Plantar hyperkeratotic or moccasin-type tinea pedis is a particularly chronic form of
tinea that is resistant to treatment.
Clinically…
The hands may be similarly infected (two feet-one hand syndrome).
Q: Write short notes about treatment of tenia pedis?
Terbinafine 1% cream twice daily for 1 week in the interdigital type.
Econazole is excellent in the macerated interdigital TP.
Recurrence is prevented by wearing wider shoes and expanding the web space with a
small strand of lamb’s wool. Powders(not necessarily medicated) absorb moisture.
Oral terbinafine 250 mg daily for 2 weeks in the hyperkeratotic type and other types of
TP.
Acute vesicular tinea pedis responds to wet compresses, oral antifungal and oral
antibiotics.
Id reaction requires wet dressings, group V topical steroids, and occasionally systemic
steroids.
Q: Write about Tinea incognito?
Fungal infections treated with topical steroids often lose some (or sometimes all) of
their characteristics.
Tinea of the hand, body, face and groin are often misdiagnosed as eczema and treated
with topical steroids.
Topical steroids reduce inflammation giving false impression of improvement.
In the mean time, the fungus flourishes. Why?
Treatment is stopped, the rash returns, but by this time it has changed. How?
Intensity of itching is variable.
Hyphae are easily seen with KOH exam. several days after stopping the use of steroids
when scaling reappears.
9
Q: What are the clinical infection patterns of tenia of the scalp?
There may be multiple cases within a family, and each person may have a different infection
pattern which may be due to specific host T-lymphocyte response.
1. Noninflammatory grey patch pattern
Clinically…
DDx: Psoriaisis, atopic dermatitis, seborrheic dermatitis.
Negative Trichophyton Ag skin test.
2. Noninflammatory black dot pattern
Lack of inflammation may be explained by the fact that cell-mediated immunity to
Trichophyton antigen skin tests is negative in these patients.
Clinically…
DDx: Alopecia areata, trichotillomania.
3. Inflammatory tinea capitis (kerion)
Most patients have a positive skin test to the Trichophyton antigen, suggesting that the
patient’s immune response may be responsible for intense inflammation.
Clinically…
Lymphadenopathy
DDx: Abscess, neoplasm.
KOH mounts and fungal cultures are often negative because of destruction of fungal
structures by inflammation.
Scarring alopecia may occur.
4. Seborrheic dermatitis type
This type is the most difficult to diagnosis because it resembles dandruff.
Clinically…
DDx: Psoriasis, atopic and seborrheic dermatitis.
5. Pustular type
Follicular pustules may be sparse or numerous.
No scale or significant hair loss (slight).
Lymphadenopathy
DDx: Bacterial folliculitis, dissecting folliculitis.
Cultures and KOH wet mounts may be negative.
11
Q: What are the clinical patterns of Onychomycosis? Write about most common one?
1. Distal and lateral subungual onychomycosis:
2. Superficial white onychomycosis:
3. Proximal subungual onychomycosis:
4. Endonyx:
5. Total dystrophic onychomycosis (TDO)
The most common types 1. Distal and lateral subungual onychomycosis:
Is the most common pattern.
The distal parts of the nail plate to turn yellow, brown or black, usually close to the
lateral nail fold.
Subungual hyperkeratosis and onycholysis.
The infection can progress proximally forming linear channels which are highly
characteristic of onychomycosis.
Typically caused by T. rubrum.
Q: Write short notes about Chronic paronychia?
Chronic paronychia which is often associated with Candida.
Chronic paronychia occurs in individuals excessively exposed to moisture and
detergents.
Typically, many or all fingernails are affected at the same time.
The nail folds become inflamed and the cuticle detaches from the nail plate losing its
water-proof properties.
Yeasts get entry into the sub-cuticular area causing more inflammation and more
cuticular detachment.
Once the nail matrix is involved, horizontal ridges (Beau's lines) appear and the nail
plate becomes irregular, thickened, and convex, and if untreated nail dystrophy may be
the end result.
Treatment: Terbinafine, Itraconazole and fluconazole, Oral antifungals, Topical antifungals
(amorolfine 5% and cicolpirox olamine 8%), Ketoconazole and griseofulvin, Nail removal

11
Q: Write short notes about Diaper Candidiasis?
An artificial intertriginous area is created under a wet diaper, predisposing the area to
a yeast infection with the characteristic red base and satellite pustules.
Rx:
Dryness should be maintained. How?
Antifungal creams twice a day for approximately 10 days.
Residual erythema from irritation may be present after 10 days. What to do?
Mupirocin ointment 2% is effective for severe Candida and bacterial diaper dermatitis.
Treatment
topical ant-fungal -+ topical antibiotics -+ steroids creams.
Notes:
Fungal infection could be dermatophytes, molds, yeast.
Sites of fungal infection skin, nail, hair.
Fungal infection could be geophilic, zeophilic (very severe infection), anthrophilic
(less severe infection).
Tenia manium of sole differe from palm (slide 34,35).
Tinea incognito the active border not present, cannot be recognized.
Treatment of scalp (hair) and nail systemic -+ topical.
