Fifth stage
PediatricLec-3
Dr. Athal Humo
17/11/2015
ACUTE GLOMERULONEPHRITISACUTE GLOMERULONEPHRITIS
Acute glomerulonephritis is characterized by hematuria, hypertension, and edema. The hematuria is usually grossly evident as tea-colored or cola-colored urine. In some children, however, the hematuria may be microscopic only.
Diseases commonly manifesting as acute nephritic syndrome include:
Acute postinfectious glomerulonephritis:Bacterial infections: as poststreptococcal glomerulonephritis & Mycoplasma pneumoniae
Viral infections: as influenza virus, EBV & mumps virus.
Immunoglobulin A (IgA) nephropathy
Membranoproliferative glomerulonephritis
Henoch-Schonlein purpura (HSP) nephritis
Systemic lupus erythematosus (SLE) nephritis
Wegener granulomatosis
Microscopic polyarteritis nodosa
Goodpasture syndrome
Hemolytic-uremic syndrome.
Glomerulonephritis Associated with Infections
Acute Poststreptococcal Glomerulonephritis:
Acute poststreptococcal glomerulonephritis (APSGN) is a classic example of the acute nephritic syndrome characterized by the sudden onset of gross hematuria, edema, hypertension, and renal insufficiency. It is one of the most common glomerular causes of gross hematuria in children.
Etiology
APSGN which is immune mediated glomerular injury follows infection of the throat or skin by certain “nephritogenic” strains of group A β-hemolytic streptococci (GAS).
Poststreptococcal GN commonly follows streptococcal pharyngitis during cold-weather months and streptococcal skin infections or pyoderma during warm-weather months.
Clinical Manifestations
APSGN is most common in children aged 5-12 yr and uncommon before the age of 3 yr.The typical patient develops an acute nephritic syndrome 1-2 wk after an antecedent streptococcal pharyngitis or 3-6 wk after a streptococcal pyoderma. The history of a specific infection may be absent, because symptoms may have been mild or have resolved without patients receiving specific treatment or seeking the care of a medical provider.
The severity of kidney involvement varies from asymptomatic microscopic hematuria with normal renal function to gross hematuria with acute renal failure.
Depending on the severity of renal involvement, patients can develop various degrees of edema, hypertension, and oliguria.
Patients are at risk for developing encephalopathy and/or heart failure secondary to hypertension or hypervolemia. Hypertensive encephalopathy must be considered in patients with blurred vision, severe headaches, altered mental status, or new seizures.
Encephalopathy can also result from the direct toxic effects of streptococcal antigens on the central nervous system.
Respiratory distress, orthopnea, and cough may be symptoms of pulmonary edema and heart failure.
Peripheral edema typically results from salt and water retention and is common; nephrotic syndrome develops in a minority (<5%) of childhood cases.
Nonspecific symptoms such as malaise, lethargy, abdominal pain, or flank pain are common.
The acute phase generally resolves within 6-8 wk. Although urinary protein excretion and hypertension usually normalize by 4-6 wk after onset, persistent microscopic hematuria can persist for 1-2 yr after the initial presentation.
Diagnosis
Urinalysis :RBC
RBC cast
polymorphonuclear leukocytes
Proteinuria
Mild normochromic anemia may be present from hemodilution and low-grade hemolysis
The serum complement:
C3 level is significantly reduced in >90% of patients in the acute phase and returns to normal 6-8 wk after onset.
CH50 is commonly depressed
C4 is most often normal in APSGN, or only mildly depressed.
Confirmation of the diagnosis requires clear evidence of a prior streptococcal infection:
A positive throat culture report might support the diagnosis or might represent the carrier state
a rising ASO titer confirms a recent streptococcal infection. But it is commonly elevated after a pharyngeal infection & rarely increases after streptococcal skin infections.
anti- (DNase) B level is best single antibody titer to document cutaneous streptococcal infection.
a positive streptozyme screen (which measures multiple antibodies to different streptococcal antigens) is a valuable diagnostic tool.
Serologic evidence for streptococcal infections is more sensitive than the history of recent infections and far more sensitive than positive bacterial cultures obtained at the time of onset of acute nephritis.
MRI of the brain is indicated in patients with severe neurologic symptoms and can demonstrate reversible posterior leukoencephalopathy in the parieto-occipital areas
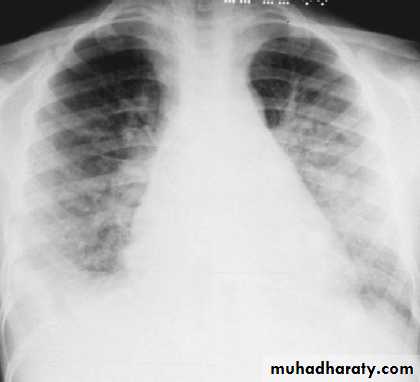
CXR is indicated in those with signs of heart failure or respiratory distress.
Renal biopsy should be considered only in the presence of:
ARF
NS
absence of evidence of streptococcal infection
normal complement levels.
when hematuria and proteinuria, diminished renal function, and/or a low C3 level persist more than 2 mo after onset. (Persistent hypocomplementemia can indicate a chronic form of postinfectious GN or another disease such as membranoproliferative GN.)
Complications
Acute renal failure can require treatment with dialysis.
Hypertension is seen in 60% of patients and is associated with hypertensive encephalopathy in 10% of cases.
Electrolytes disturbance: hyperkalemia, hyperphosphatemia, hypocalcemia.
Heart failure.
CXR of a patient with poststreptococcal glomerulonephritis showing pulmonary edema
Treatment
Management is directed at treating the acute effects of renal insufficiency and hypertension.Although a 10-day course of systemic antibiotic therapy with penicillin is recommended to limit the spread of the nephritogenic organisms, antibiotic therapy does not affect the natural history of GN.
Sodium restriction, diuresis usually with intravenous furosemide, and pharmacotherapy with calcium channel antagonists, vasodilators, or angiotensin-converting enzyme inhibitors are standard therapies used to treat hypertension.
Clinical course and prognosis
Majority of children with APSGN make a full recovery without significant long-term consequences.Recurrences of APSGN are rare.
Progression to CKD & ESRD may occur in severe cases.
Follow up of AGN is important to document full recovery:
Proteinuria associated with APSGN usually resolves by 6–8 weeks. Prolonged proteinuria for more than 3 months may indicate irreversible renal injury, and should be viewed with concern.
Gross hematuria usually improves within 1–3 weeks but microscopic hematuria can persist for up to 1 year and is not an indicator of poor prognosis.
Recovery of serum complement C3 to normal usually takes 6–8 weeks. Persistent hypocomplementemia beyond 8 weeks requires a careful search for other diagnoses, such as MPGN and SLE nephritis.