Fifth stage
pediatricLec-5
د.اثل
17/11/2015
Objective• To define FTT.• To know its causes.• To distinguish its manifestation.• Approach to investigate a child with FTT.• How you can manage a case.
Failure to Thrive (FTT)• FTT is a term given to malnourished infants andyoung children who fail to meet expected standardsof growth.• FTT is a common problem in pediatrics, affecting5% to 10% of young children and approximately 3%to 5% of children admitted to hospitals.• FTT is more common in children living in povertyand foster care and affects 15% of these group.
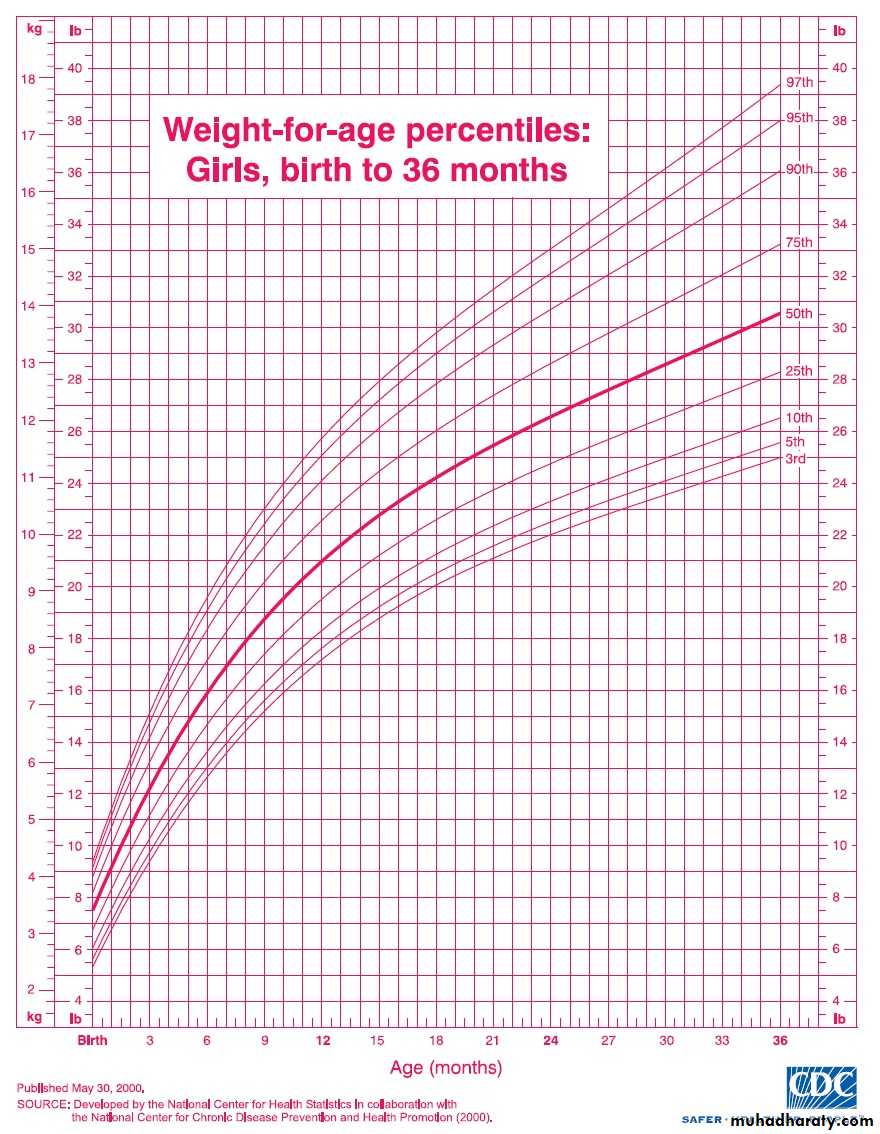
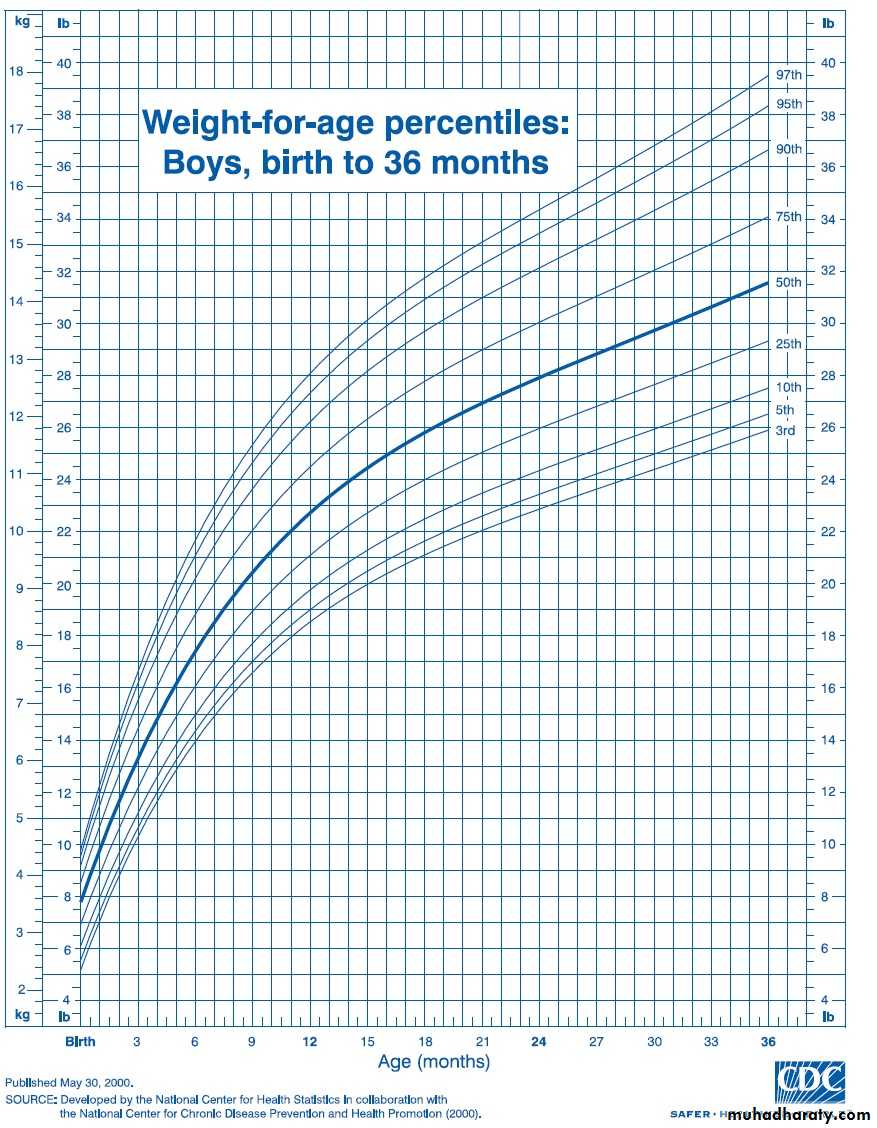
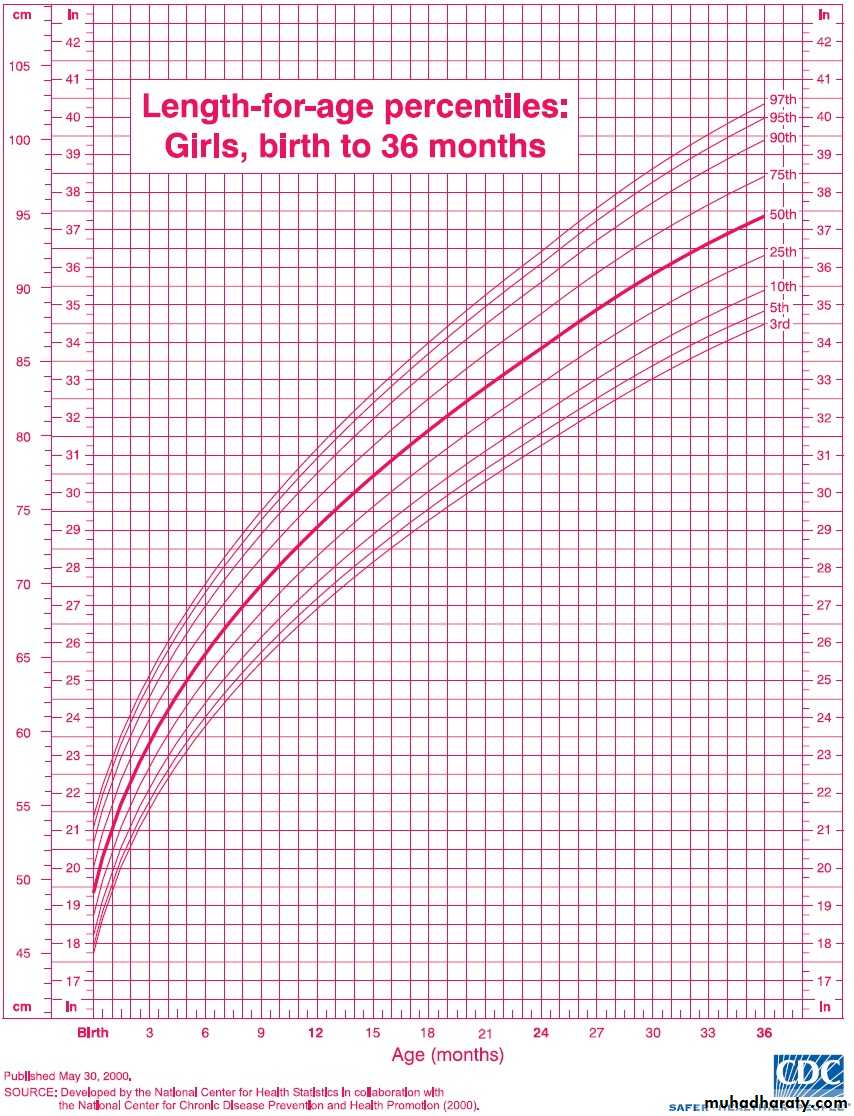
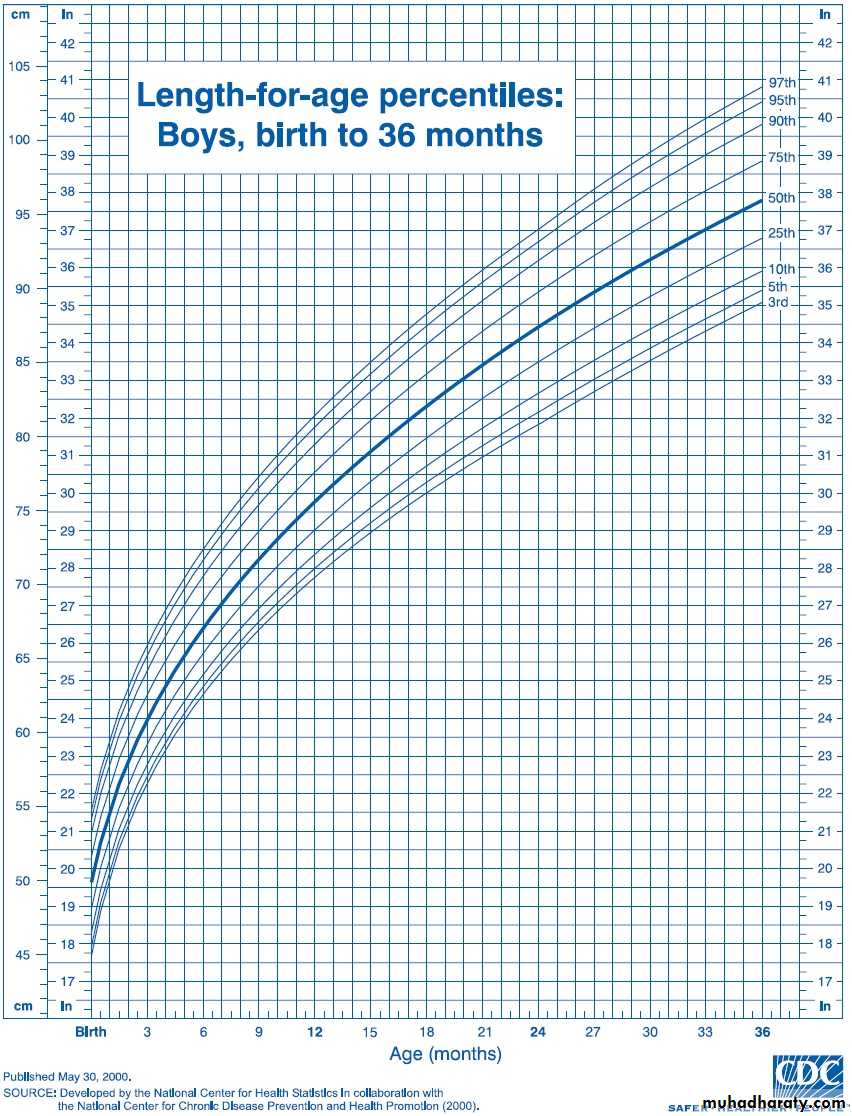
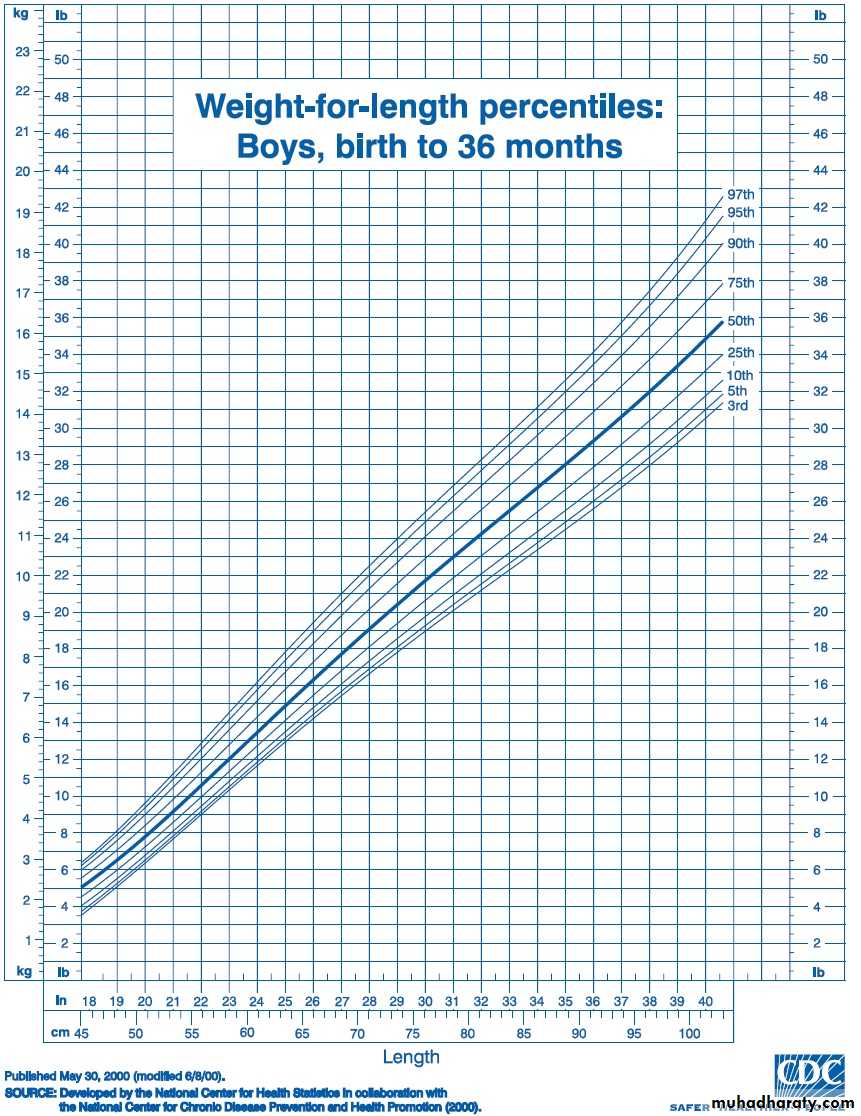
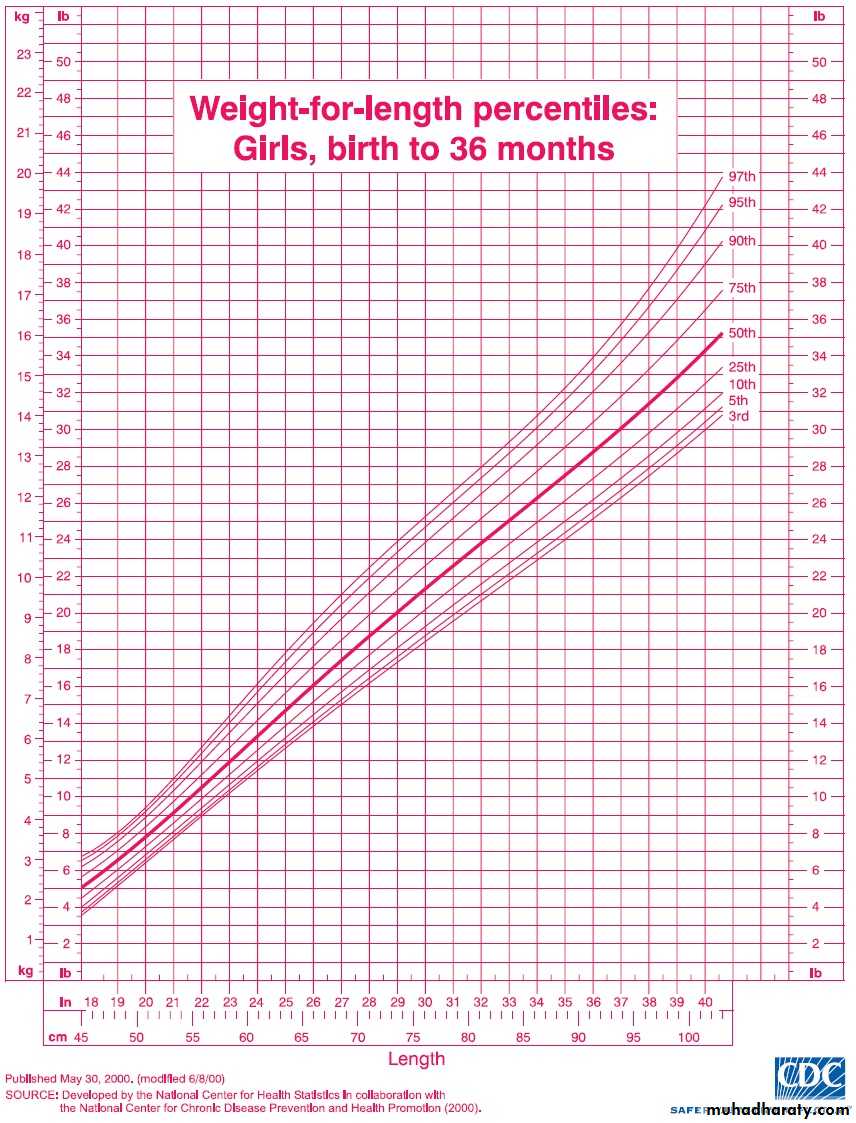
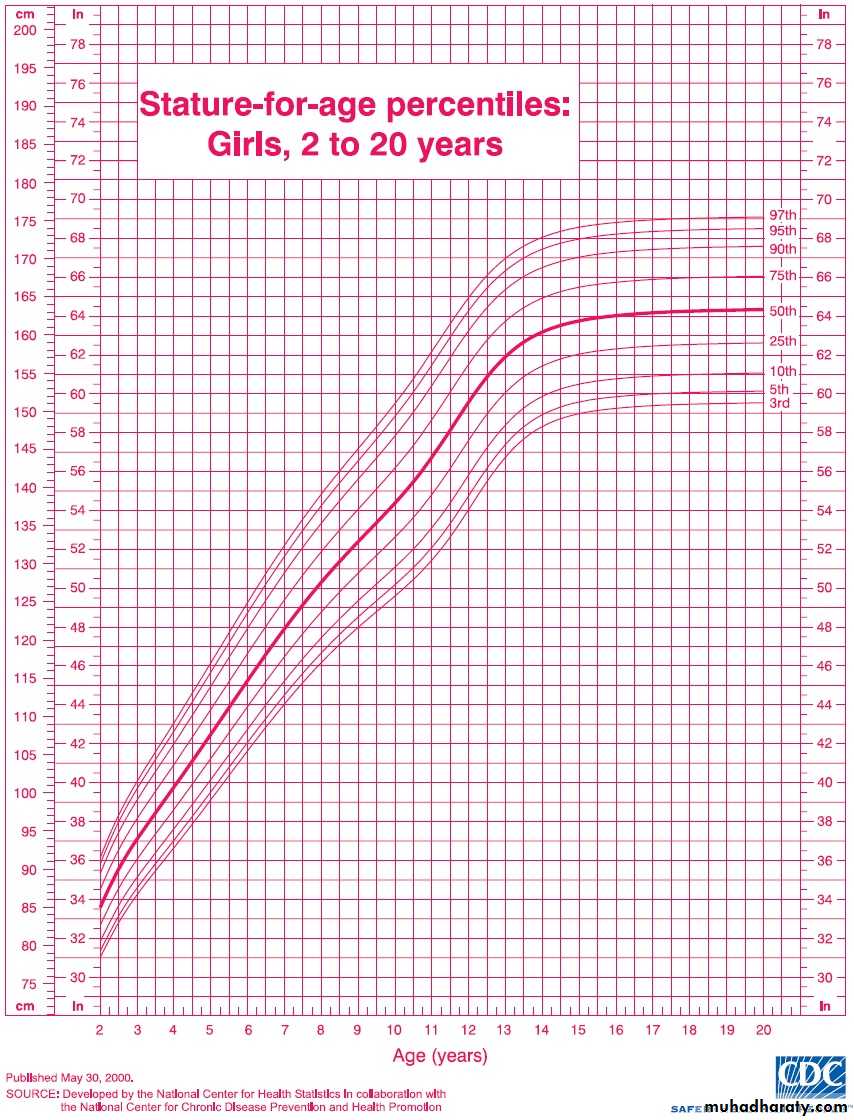
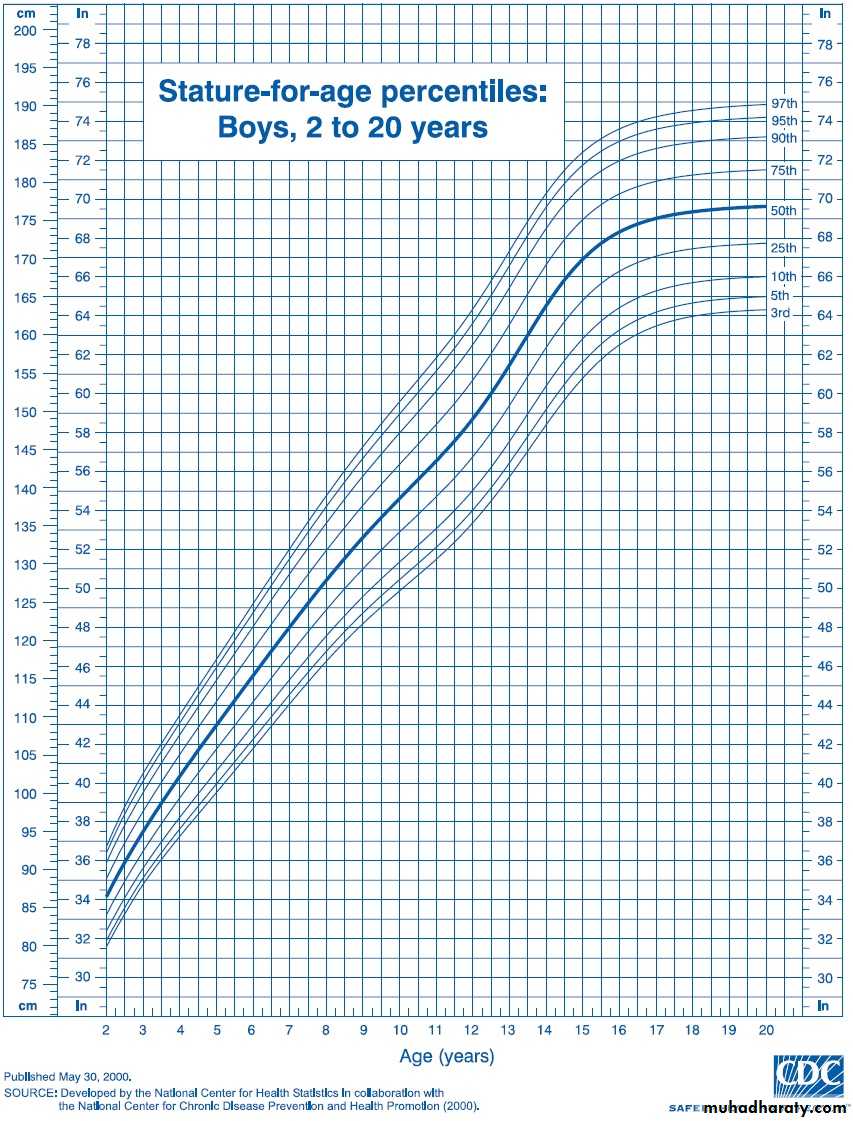
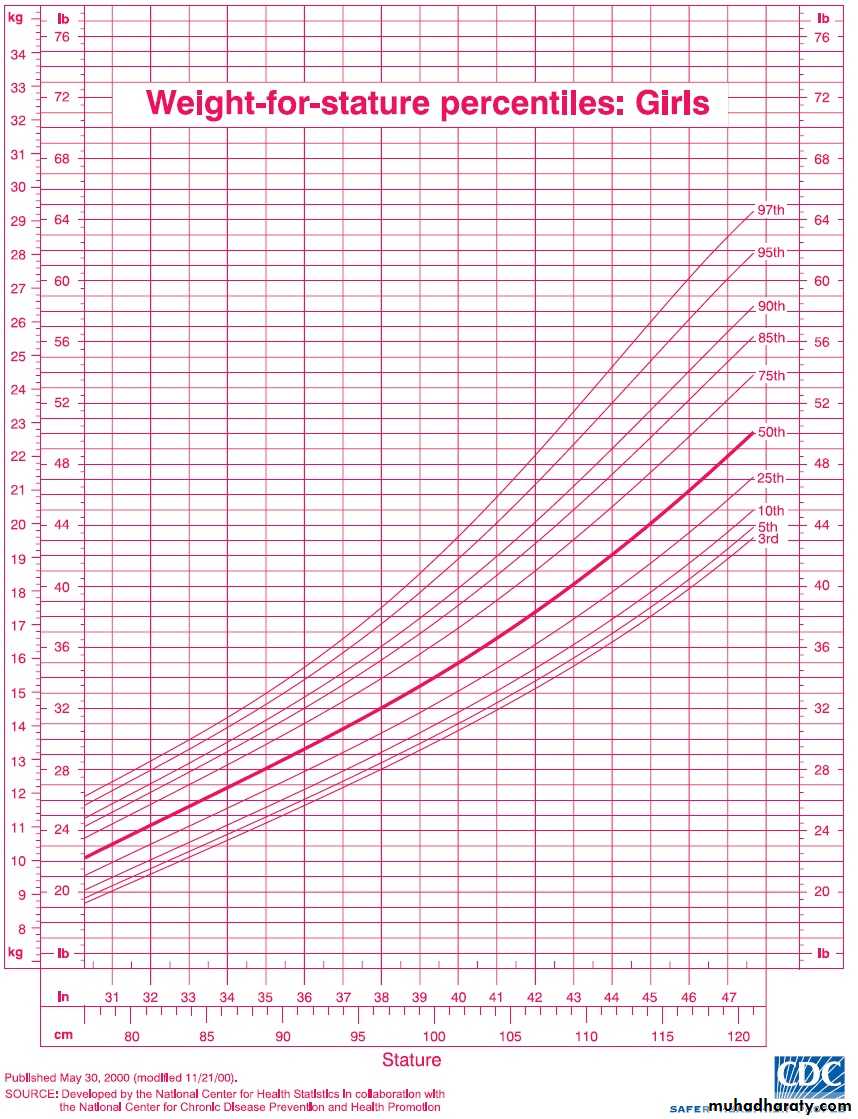
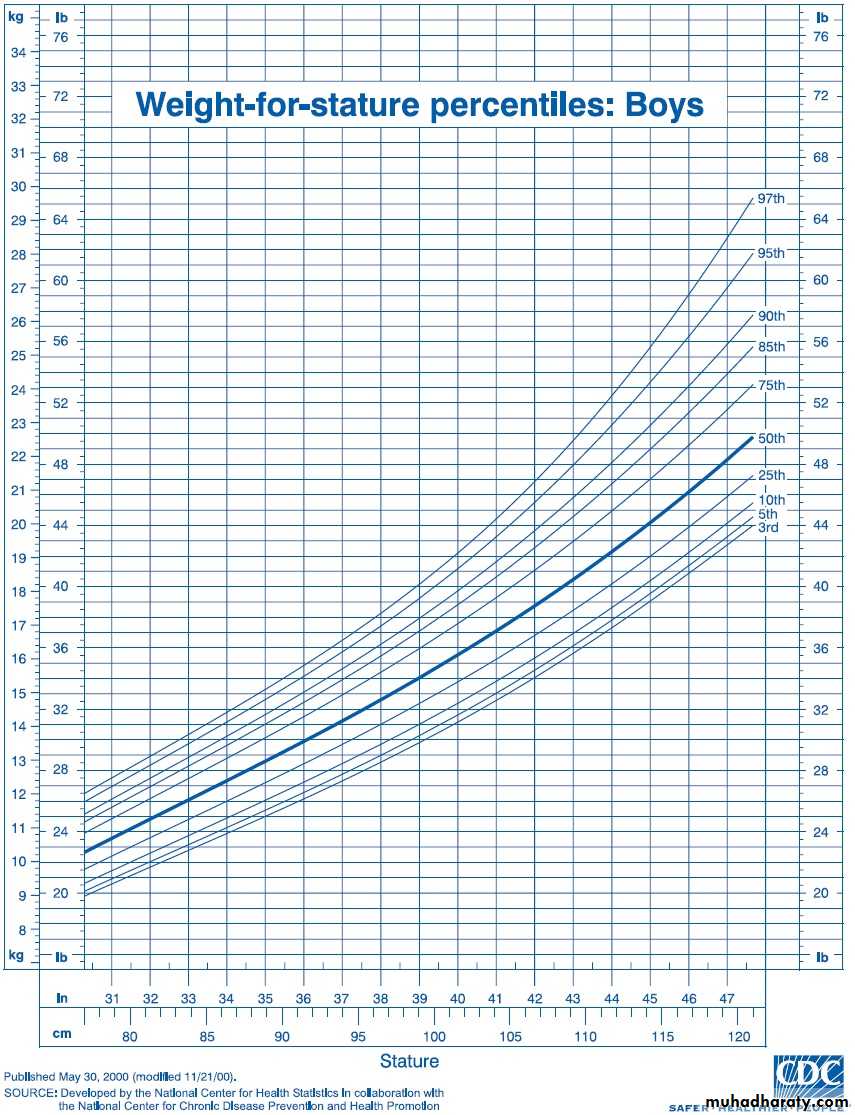
Definition of FTT• weight that falls or remains below the 5thpercentile for age.• weight that decreases crossing two majorpercentile lines on the growth chart overtime, (i.e., from above the 75th percentileto below the 25th)• weight that is less than 80% of themedian weight for the height of the childIn children with FTT, malnutritioninitially results in:• Wasting (deficiency in weight gain).then• Stunting (deficiency in linear growth)generally occurs after months ofmalnutrition.• Head circumference generally isspared except with chronic, severemalnutrition.The weight for age per cent of the standard value decreasesearly in the course of FTT, followed by a decrement of heightfor age. So:• Weight for height below the 5th percentile remains thesingle best growth chart indicator of acute undernutrition• Children with chronic malnutrition often have a normal weightfor height because both their weight and height are reduced.NOTE:Allowances must be made for prematurity;OFC corrections are needed until 18 months of age.weight corrections are needed until 24 months of age.height corrections are needed until 40 months of age.Causes of FTT:• Non organic ( psychosocial FTT).• Organic FTT is marked by anunderlying medical condition
Non organic or psychosocial FTT:It is far more common than organic FTT.Psychosocial FTT is most often due to poverty or poorchild-parent interaction.Causes of Non organic (psychosocial FTT):• Lack of food ( poverty)• Lack of knowledge, (poor feeding techniques,improper formula preparation, improper mealtimeenvironment)• Parental depression ,emotional deprivation, Child abuse or neglect .
Organic Causes of Failure to Thrive:Any chronic disease may lead to FTT• Gastrointestinal: GER, celiac disease, pyloric stenosis, cleft lip/palate, lactose intolerance, Hirschsprung's disease, milk proteinintolerance, hepatitis, cirrhosis, pancreatic insufficiency, biliarydisease, inflammatory bowel disease, malabsorption• Renal: UTI, RTA, DI, RF• Cardiopulmonary: Cardiac diseases leading to CHF, asthma, BPD, CF,anatomic abnormalities of the upper airway,• Endocrine: Hyperthyroidism, DM, adrenal insufficiency or excess,parathyroid disorders, pituitary disorders,• Neurologic: MR, CP, degenerative disorders, CNS tumors• Infectious: Parasitic or bacterial infections of the gastrointestinaltract, TB, HIV disease• Metabolic: IEM• Genetics, Congenital: Chromosomal abnormalities, congenital syndromes(fetal alcohol syndrome), perinatal infections• Miscellaneous :Lead poisoning, malignancy, collagen vascular disease,recurrently infected adenoids and tonsils
DIAGNOSIS AND CLINICAL MANIFESTATIONSHistory• prenatal and postnatal factors :That influence growth, including the history of prenatal care, maternalillnesses during pregnancy, to1. Identify fetal growth problems (IUGR), birth size (weight, length, and headcircumference).2. Identify prematurity• Indicators of medical diseases (review of systems):such as vomiting, diarrhea, fever, respiratory symptoms, etc• Careful dietary history is essential:The adequacy of the maternal milk supply or the precise preparation offormula should be evaluated.For older infants and young children, a detailed diet history is helpful,it is essential to evaluate intake of solid foods and liquids. Because of parentaldietary beliefs, some children have inappropriately restricted diets. Otherchildren with FTT drink excessive amounts of fruit juice, leading tomalabsorption or anorexia for more nutrient-dense foods..• Social environment: poverty, unemployment, illiteracy, conflict ,disruptive parent-child interactions
Physical examination :• Growth chart: weight, height, OFC• Systemic examination:– Physical findings related to malnutrition,such as dermatitis, pallor, or edema– Additionally, severely malnourished childrenare at risk for a variety of infections.• Depending on severity, the infant with FTT mayexhibit thin extremities, a narrow face, prominentribs, and wasted buttocks. Neglect of hygiene maybe evidenced by diaper rash, unwashed skin,untreated impetigo, uncut and dirty fingernails, orunwashed clothing. A flattened occiput with hairloss may indicate that the child has been lying on hisor her back. This flattening may be due to beingunattended for prolonged periods. Delays in socialand speech development are common. Other findingsmay include an avoidance of eye contact, anexpressionless face, hypotonia, and the absence of acuddling response.
Laboratory evaluation:There is no need for extensive laboratory search for medicaldiseasesSimple screening tests are recommended to screen for the commonillnesses that may cause growth failure and to search for medicalproblems that result from malnutrition.Recommended laboratory tests include:• CBP : type of anemia, WBC abnormalities (leucocytosis,lymphopenia)• Urinalysis, urine culture: UTI• Serum electrolytes & RFT• Serum protein: Degree of protein deficiency• Blood sugar: hpoglycemia• Stool sample for culture and ova and parasites may be indicatedfor children with diarrhea, abdominal pain, or malodorous stools.• PPD: screen for TB
TREATMENTMost children with FTT can be treated inthe outpatient setting.Hospitalization is required for– Children with severe malnutrition.– Children with underlying diagnoses that requirehospitalization for evaluation or treatment.– Children whose safety is in danger because ofmaltreatment( social issues of the family).
Nutritional management:✎It is the cornerstone of treatment ofFTT, regardless of the etiology.✎In general, the simplest and leastcostly approach to dietary change iswarranted.
Amount:✎ SLOW GRADUAL INCREMENT– Calories can be safely started at 20% above the childrecent intake– If no estimate of the caloric intake is available,50-75%of the normal energy requirement is safe.– Caloric intake can be increased 10-20% per day. withmonitoring for electrolyte imbalances, poor cardiacfunction, edema, or feeding intolerance. If any of theseoccurs, further caloric increases are not made until thechild's status stabilizes.✎ The final target is to provide 100 to 120 kcal/kgbased on ideal weight.
Type:according to age of the child & type of feeding :✎ Breast fed infant: continue breast feeding and may add cowmilk or special cows’ milk based formula (F75 or F100).✎ Bottle fed :Increased amount of cow milk ,or change to other types ifindicated like:– special cows’ milk based formula(F75 or F100)– calorically dense formula (for anorectic and picky eater)concentration of formula can be changed from 20 cal/oz to 24or 27 cal/oz– soy based (isomil) for lactose-intolerant child– hydrolyzed protein type (pregestemil) for cow milk proteinintolerant– home made (oil,butter,peanut butter, others)✎ Toddlers:– Dietary changes should include increasing the caloric densityof favorite foods by adding butter, oil, peanut butter, or otherhigh-calorie foods.– High-calorie oral supplements that provide 30 cal/oz are oftenwell tolerated by toddlers.Vitamin and mineral supplementation:It is needed, especially duringcatch-up growth. Vitamin and mineralintake in excess of the dailyrecommended intake is provided toaccount for the increasedrequirements; this is frequentlyaccomplished by giving an ageappropriate daily multiple vitamin.