1
Fifth stage
Pediatric
Lec-1
.د
بسام
23/11/2015
EXAMINATION OF THE NEWBORN BABY
The objective of doing an examination of the newborn baby is to do an early detection of any
abnormality which may needs urgent intervention & treatment shortly after birth, or to
detect any other abnormalities which may need follow up or been able to be treated later
on. Also to answer the naturally anxious parents after delivery to know if their baby is all right
and appear normal.
The exam should be carried out twice or preferably 3 times during the 1st few days of life.
The first exam done in the hospital delivery room to:-
Identify any obvious major or minor malformations.
To asses gestational age, nutrition and vigor.
To determine how well the baby handles the transition from intra to extra uterine life,
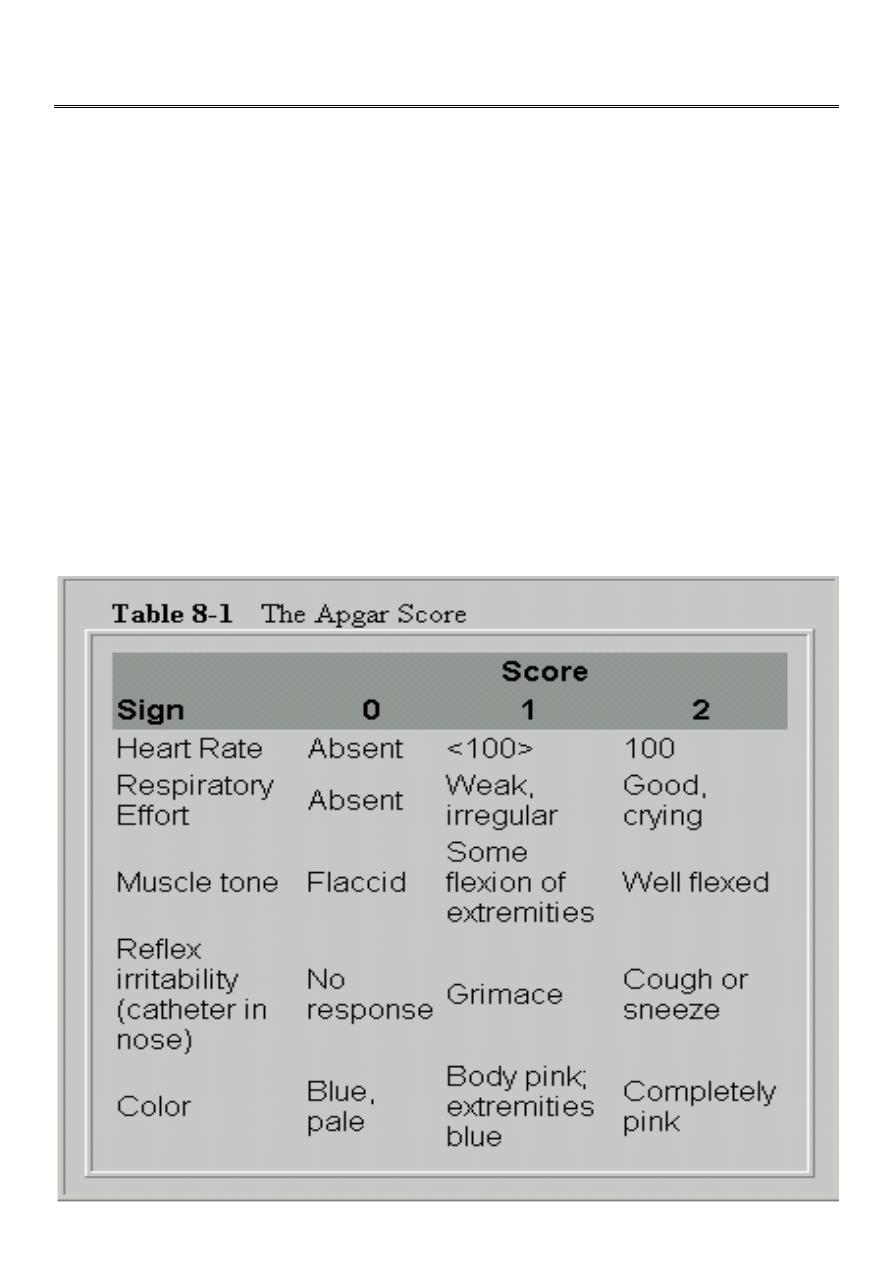
this can be done by assessing what is called the APGAR scoring which is assessed at 1
and 5 min after birth and as follows:

2
The 2nd examination performed in the hospital newborn nursery and during the 1st 24 hours
of life.
The 3rd examination is carried out just before the family discharge to home. Its main purpose
is to discover any postnatally acquired problems such as infection or excessive jaundice & to
detect any malformations that were not apparent at the 1st examination such as forms of
congenital Heart diseases whose murmur were not audible on the 1st day of life.
To have successful examination of the NBB the baby should be naked, warm, well illuminated,
and stable. The ideal time to examine the baby is a couple of hours after feeding, when the
baby is not too deeply asleep as they often are after feeding, nor awake and screaming as
just before a feeding.
General examination:
First of all does the baby looks normal or abnormal, do the body proportions, head, face and
neck appears grossly normal, are there any obvious deformities or unusual appearance, is
the baby in distress or resting comfortably. Also you have to look for signs of prematurity and
post maturity.
What is the color of the skin is it pink or it is pale which may represent asphyxia, anemia,
shock or edema. If he is cyanosed is it involving the hands and feet known as
(acrocyanosis) especially when they are cold which is a normal phenomenon due to
vasomotor instability, or the cyanosis is central one due to cardiac pulmonary or CNS disease.
The extremities may be mottled with a net like pattern if they are cool. Generalized mottling
may signify acidosis or vasomotor instability. Another variation in skin color is the so called
harlequin color change mostly seen in LBW infants where the baby’s skin is dark pink or
reddish on the dependent half of the body while the upper half appears pale the two colors
sharply demarcated along the midline (it is not pathological).
Look for petechiae which can be associated with increased intravascular pressure during
labor or due to thrombocytopenia.
Mongolian blue spots: are blue well demarcated areas of pigmentation are seen over the
buttocks, back and sometimes other parts of the body, they tends to disappear within the
first year of life.
Fine soft immature hair lanugo hair frequently covers the scalp and may cover the face &
shoulders in premature infants.
Salmon patch (nevus simplex): are small pale pink ill-defined flat vascular lesions that occur
mostly on the glabella, eye lid upper lip & nuchal area in 30-40% of normal NBB, they may
persist for several months & become more visible with crying.

3
Erythema toxicum: benign self-limited, the lesion are firm yellow white, 1-2 mm papule or
pustules with a surrounding erythematous flare they may be sparse or numerous peak
incidence is in the 2nd day of life. Aspirate from the lesion show eosinophils infiltrate &
absence of M.O. on a stained smear.
Milia: superficial epidermal inclusion cysts, the lesion is firm papule of 1-2 mm in diameter
and pearly opalescent white, they are most frequently scattered over the face, gingiva and
on the midline of the palate called Epistein pearl, it disappear spontaneously.
Miliaria: erythematous minute papulovesicular lesions may impact a prickly sensation the
lesions are usually located to sites of occlusion or to flexural areas such as the neck, groin,
and axilla. It is due to retention of sweat in occluded sweat ducts.
Port-wine stain (nevus flammeus): dilated dermal capillaries macular sharply demarcated
pink to purple, vary in size, head and neck are most commonly involved, usually unilateral. It
can be an isolated phenomenon or it is part of sturge weber syndrome (portwine stain with
intracranial calcification).
Strawberry nevus: bright red capillary hemangiomas protuberant, compressible, any part of
the body can be affected. It can regress spontaneously within the first 2-3 years of life, if not
it require treatment.
Cavernous hemangioma: ill define & more diffuse, cystic, compressible, the overlying skin
color either normal or bluish.
Head
: may be molded particularly if the baby is the 1st born. A rounded symmetrical head
is seen if a baby is born by caesarian section or breach delivery, whereas babies born by
vaginal vertex delivery usually has a head that is elongated occipitally with some overriding
of the sutures & possibly a caput succedaneum or cephalhematoma.
Caput is a collection of subcutaneous edema fluid caused by pressure during passage through
the birth canal disappear within the 1st few days of life.
Cephalhematoma is a sub periosteal collection of blood limited by the sutures of the skull it
is soft to fluctuant it lasts for several weeks gradually gets smaller.
The anterior fontanel should be flat or slightly sunken when the baby is held in the upright
position & is quite, the size of the anterior fontanel 1-3 cm in diameter, post fontanel is either
closed at birth or it is closed during the 1st 4 months of life.
Causes of large anterior fontanel:
Prematurity. Hydrocephalus. Achondroplasia.
Intrauterine growth retardation. Osteogenesis imperfecta. Congenital rubella.
Hypophosphatasia. Trisomies (21, 18, 13).
Rickets (in older infants). Hypothyroidism.

4
Eyes
: subconjunctival or retinal hemorrhage are not significant, occur during difficult labor.
Pupillary reflex should be present, the iris should be inspected for colobomas or
heterochromias
Presence of bilateral red reflex exclude cataract or other intraoccular pathology. But white
pupillary reflex (leukocorea) is seen in:-
Cataract
Tumor (retinoblastoma),
Chorioretinitis
Retinopathy of prematurity
Persistent hypeplastic
Primary viterious.
A cornea of more than 1cm (megalocornea) suggest congenital glaucoma.
Mouth
: natal tooth in the lower incisor position may be seen, these teeth are usually shed
before the eruption of the deciduous teeth. The hard & the soft palate should be inspected
for a cleft palate. Epstein pearl may be seen on the hard palate.
Neck:
It is relatively short in the newborn, there may be goiter, cystic hygroma,
sternomastoid tumor, webbing of the neck in female suggest Turner syndrome, and both
clavicles should be palpated for fractures.
Chest:
breast hypertrophy is common & milk may be present. Asymmetry, erythema,
tenderness and induration suggest abscess formation. Widely spaced nipples suggest turner
syndrome.
Also observe the respiratory rate which is normally between 30-40/min in full term baby and
in resting state, a rate of >60 is abnormal. The respiratory rate in preterm baby is higher, the
premature infant may have a periodic breathing.
Heart:
localize the heart to exclude dextro-cardia & there may be transitory murmur in
normal heart and cong heart dis may not initially produce a murmur that will be present later.
The rate may vary from 100 per min in relaxed sleep to 180 per min during activity, the pulse
should be palpated in the upper & lower extremities to detect coarctation of the aorta.
Abdomen:
the liver is usually palpable sometimes as much as 2cm less commonly the
spleen tip may be felt, the abdominal wall is usually weak especially in premature infant, and
umbilical hernia is a common finding.
Omphalitis: Is an acute local inflammation of the periumbilical tissue that may extent to the
abdominal wall, the peritoneum, the umbilical vein and portal vessels, or the liver and may
result in later portal hypertension.
5
Abdominal masses
: may be cystic as in:
1. Hydronephrosis.
2. Polycystic kidney.
3. Adrenal hemorrhage.
4. Intestinal duplication.
5. Choledocal cyst.
6. Ovarian, omental, or pancreatic cyst.
Or the abdominal masses are solid as in:
1. Neuroblastoma.
2. Hepatoblastoma.
3. Teratoma.
4. Renal vein thrombosis (flank mass).
Abdominal distention at or shortly after birth suggests either intestinal obstruction or GIT
perforation. Later distention suggests lower bowel obstruction, sepsis, or peritonitis. A
scaphoid abdomen suggests diaphragmatic hernia.
Omphalocele is an abdominal wall defect through the umbilicus where a herniation of the
abdominal viscera which are covered by the peritoneum.
Gastroschisis: The abdominal defect lies to the right of an intact umbilical cord, and the
intestine lie exposed without a covering sac, free in the amniotic fluid.
Genitalia: look for ambiguous genitalia, vaginal discharge or bleeding may occur normally
after birth, it is transient due to the effects of maternal hormones.
Anus: should be examined for unperforated anus although not all the cases are visible you
may need to have gentle insertion of the little finger or a rectal tube.
Extremities: hands &feet for polydactyly or syndactyly, nerve injury or fracture seen by
observing spontaneous or stimulated movements of the extremities.
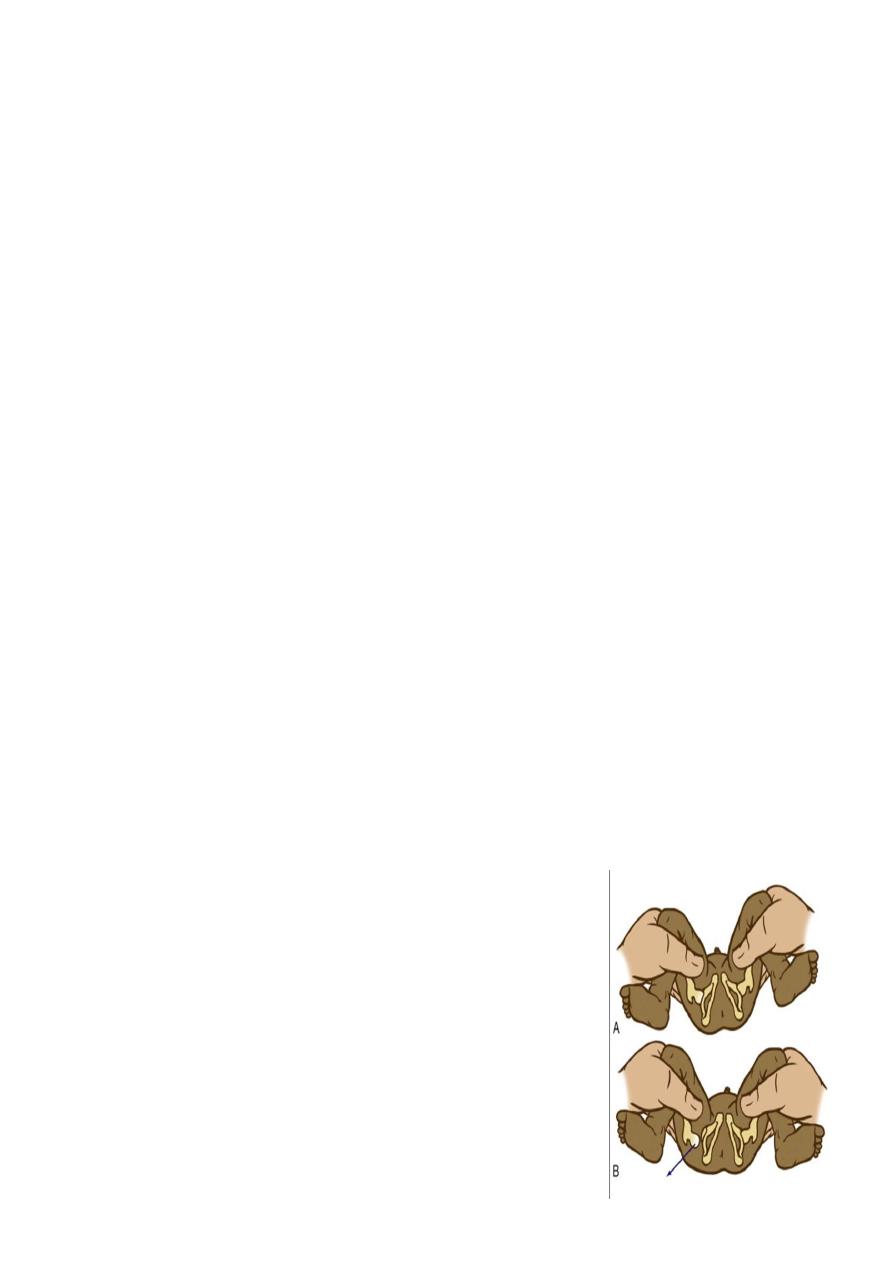
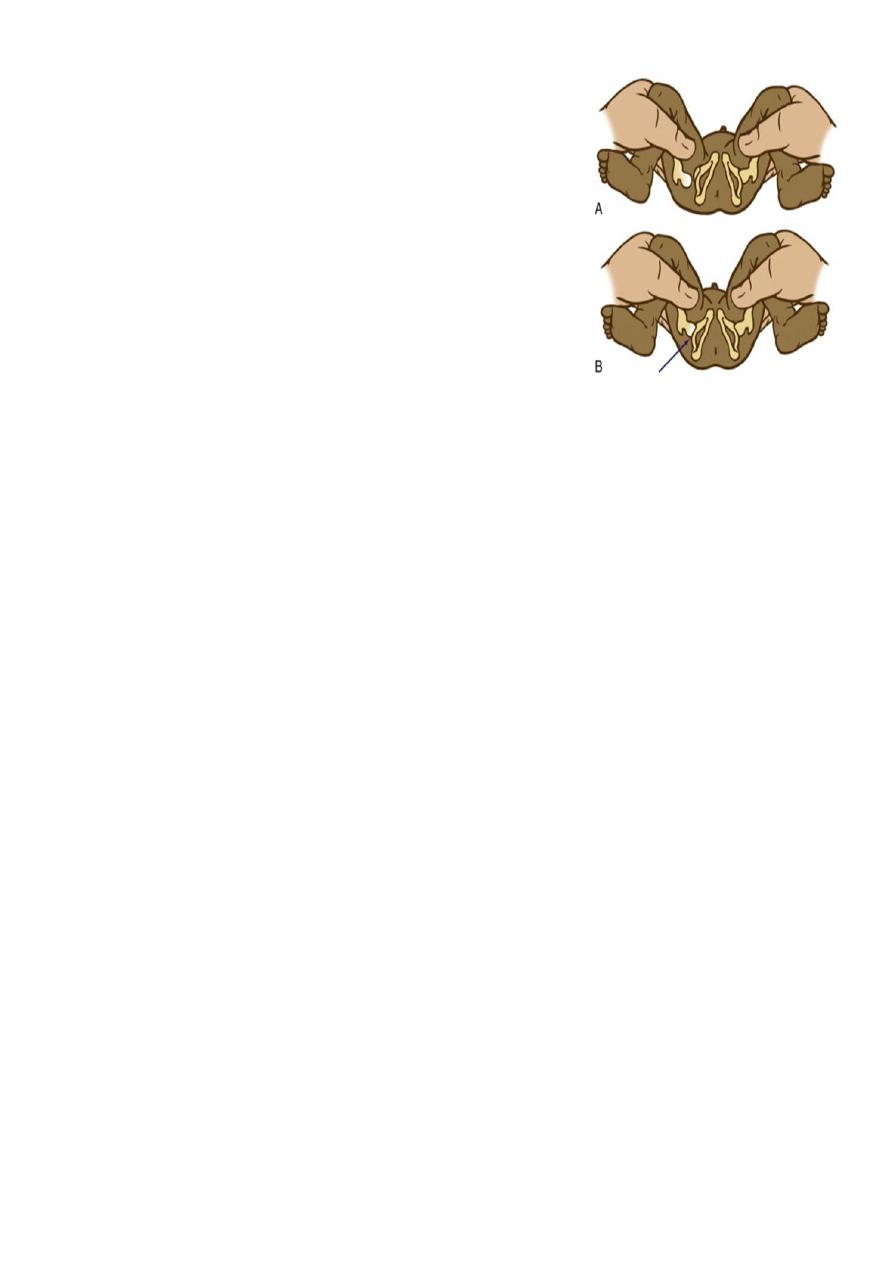
Examine for developmental dysplasia of the
hips:-
The examiner adducts the flexed hip and gently pushes the thigh
posteriorly in an effort to dislocate the femoral head. In a
positive test, the hip is felt to slide out of the acetabulum.
((Barlow Test))
6
The Ortolani test
is the reverse of Barlow test: The
examiner attempts to reduce a dislocated hip. The examiner
grasps the child's thigh between the thumb and index finger
and, with the 4th and 5th fingers, lifts the greater trochanter
while simultaneously abducting the hip. When the test is
positive, the femoral head will slip into the socket with a
delicate clunk that is palpable but usually not audible. It
should be a gentle, non-forced maneuver.
Primitive neonatal reflexes
Moro reflex: To elicit the reflex, the head is supported and allowed to drop to the level of
the bed. There will be initial extension response of the upper limbs, followed by flexion and
crying.
Grasp reflex: it is elicited by placing a finger or object in the open palm, the normal infant
will grasp the object and with attempted removal the grip is reinforced.
Rooting reflex: The infant opens the mouth and turns the head towards the pacifier or the
examiner finger stimulating the cheek.
Sucking reflex: Vigorous sucking movements are initiated when an object is placed in the
infant's mouth.
Tonic neck reflex: when manually turning the head to one side while supine, extension of the
arm occurs on that side of the body corresponding to the direction of the face while flexion
develops on the contralateral extremities.
