
1
Fifth stage
Medicine
Lec-5
.د
فاخر
24/11/2015
Gout
Gout once called the “Disease of Kings” is also seen in Women, Especially after Menopause
Gout is a true crystal deposition disease. It can be defined as the pathological reaction of
the joint or periarticular tissues to the presence of monosodium urate monohydrate
(MSUM) crystals.
URATE, HYPERURICEMIA & GOUT
Urate: end product of purine metabolism
Hyperuricemia: serum urate > urate solubility) 6.8 mg/dl
The prevalence of gout varies between populations but is around 1% with a strong male
predominance (> 10:1). Prevalence increases with age and increasing serum uric acid
concentration. 'Primary' gout is almost exclusively a male disease and the most common
cause of inflammatory arthritis in men over the age of 40..
Hyperuricemia caused by 10% Overproduction 90% Underexcretion
Classification of Hyperuricemia:
1- Uric acid overproduction
Acquired disorders :
Ethanol
deficiencyMyeloproliferative disorders
Cytotoxic chemotherapy
Genetic disorders:
Deficiency HGPRT(hypoxanthine-guanine phosphoribosyl transferase), or superactivity
of PRPP(phosphribosyl pyrophosphate synthetase).
2- Uric acid underexcretion
Accounts for >90% of hyperuricemia
Diminished tubular secretory rate, increased tubular reabsorption, diminished uric acid
filtration

2
Hyperuricemia:
Serum uric acid levels are distributed in the community as a continuous variable Levels are
higher in men than women; they rise from the twenties in men and after the menopause in
women, positively correlate with obesity, and vary according to ethnicity.
Estrogen have a mild uricosuric effect; therefore, gout is unusual in premenopausal women
Higher renal clearance of urate in women possibly due to their higher plasma estrogen
levels
Pathogenesis of Gouty Inflammation
Urate crystals stimulate the release of numerous inflammatory mediators in synovial cells
and phagocytes
The influx of neutrophils is an important event for developing acute crystal induced
synovitis
GOUT RISK FACTORS
Male
Postmenopausal female
Older
Hypertension
Pharmaceuticals:
Diuretics, ASA, cyclosporine
Transplantation
Overproduction (10%)
Ethanol
HGPRT or G6PD deficiency
PRPP synthetase overactivity
Myeloproliferative disorders
Cytotoxic chemotherapy
Underexcretion (90%)
Renal insufficiency
Drugs and toxins
Diuretics
Ethanol
Cyclosporine A
Pyrazinamide
Lead nephropathy
Low-dose aspirin
Ketosis

3
Alcohol intake
Highest with beer
Not increased with wine
High BMI (obesity)
Diet high in meat & seafood
Clinical features
1- Acute gouty arthritis
extremely rapid onset, reaching maximum severity in just 2-6 hours, often waking the
patient in the early morning
severe pain, often described as the 'worst pain ever'
extreme tenderness-the patient is unable to wear a sock or to let bedding rest on the joint
marked swelling with overlying red, shiny skin
During the attack the joint shows signs of marked synovitis but also periarticular swelling
and erythema. There may be accompanying fever, malaise and even confusion, especially if
a large joint such as the knee is involved. As the attack subsides, pruritus and desquamation
of overlying skin are common. The main differential diagnosis is septic arthritis, infective
cellulitis or another crystal disease.
After an acute attack some people never have a second episode; in others the next episode
occurs after years. In most, however, a second attack occurs within 1 year and the
frequency of attacks gradually increases with time. Later attacks are more likely to involve
several joints and to be more severe
2-Chronic tophaceous gout
Large MSUM crystal deposits produce irregular firm nodules
('tophi') at the usual sites for nodules around extensor
surfaces of fingers, hands, forearm, elbows, Achilles tendons
and sometimes the helix of the ear. The white colour of
MSUM crystals may be evident and permits distinction from
rheumatoid nodules.
3- Progressive renal disease
is an important complication confined to untreated severe chronic tophaceous gout. This
results from MSUM crystal deposition in the interstitium of the medulla and pyramids with
4
consequent chronic inflammation, giant-cell reaction, fibrosis, glomerulosclerosis and
secondary pyelonephritis…
Renal stone ..
Investigations
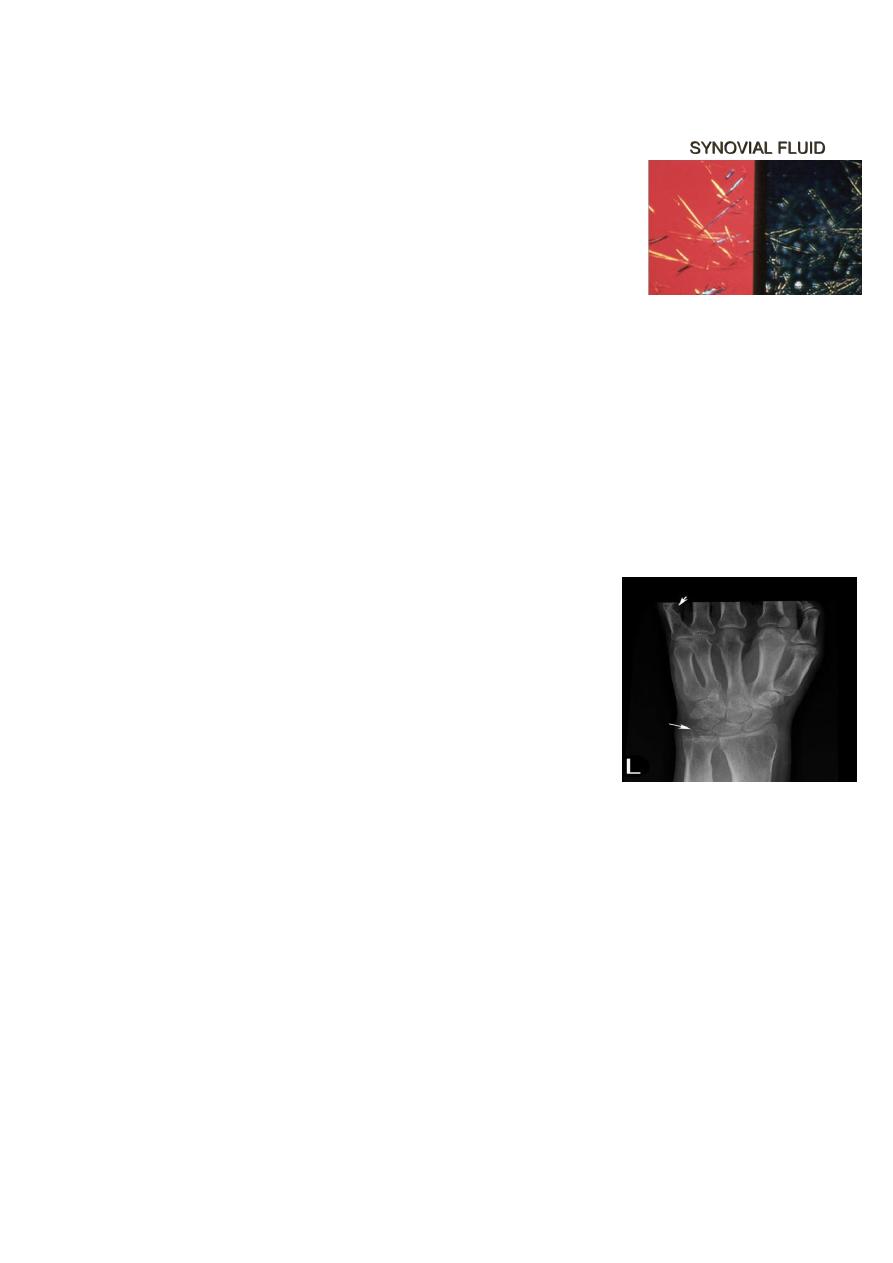
Definitive diagnosis requires identification of MSUM crystals in the
aspirate from a joint, bursa or tophus. In acute gout synovial fluid
shows increased turbidity due to the greatly elevated cell count (> 90% neutrophils..
Assessment of renal function (serum creatinine, urine testing), hypertension, blood glucose
and serum lipid profile should be undertaken. An FBC and ESR should detect
myeloproliferative disorders during remission of acute gout. During an attack a marked
acute phase response (elevated CRP, neutrophilia) is usual; the ESR is often modestly raised
in tophaceous gout
X-rays can assess the degree of joint damage. In early disease
they are usually normal, but narrowing of joint space, sclerosis,
cysts and osteophyte (changes of OA) may develop in affected
joints with time, or be present as a predisposing factor in
secondary gout. Gouty 'erosions' (bony tophi) are a less common
but more specific feature occurring as para-articular 'punched-
out' defects with well-delineated borders and retained bone
density. Tophi may also be visible as eccentric soft tissue
swellings..
Management
The acute attack
A fast-acting oral NSAID (. Indomethacin 50 mg 4hourly. naproxen, diclofenac,) can give
effective pain relief and is the standard treatment. Patients can keep a supply of an NSAID
with which they are familiar and take it as soon as the first symptoms are noticed,
continuing for the duration of the attack.
Oral colchicine (a potent inhibitor of neutrophil microtubular assembly) can be very
effective, but unfortunately often causes vomiting and severe diarrhoea at the doses
needed for rapid relief (1 mg loading dose, then 0.5 mg 6-hourly until symptoms abate).
The compromise is to try lower doses (0.5 mg 8-12-hourly) for a slower onset of benefit.
polarizing
microscopy

5
Aspiration of the joint will give instant relief and, when combined with an intra-articular
corticosteroid injection to prevent fluid reaccumulation, often effectively aborts the attack
Correction of any predisposing factors should always be attempted. Lifestyle alteration to
correct obesity and reduce excess beer consumption may significantly reduce
hyperuricaemia. Diuretics should be stopped if possible. Although a very high purine diet
(large amounts of seafood, red meat and offal) should be tempered, there is no need for a
specific highly restrictive diet.
and trigger acute attacks..
HYPOURICAEMIC DRUGS
INDICATIONS FOR HYPOURICAEMIC DRUGS
1-Recurrent attacks of acute gout
Tophi
2-Evidence of bone or joint damage
3-Associated renal disease
4-Gout with greatly elevated serum uric acid
ALLOPURINOL
Allopurinol: blocks conversion of xanthine to uric acid. works for underexcretors and
overproducers
The aim of treatment is to bring the serum uric acid level into the lower half of the normal
range to ensure dissolution of crystals and to prevent new ones forming. The serum uric
acid should therefore be measured every 3-4 weeks and the dose of allopurinol increased in
100 mg increments until this is achieved (maximum 900 mg daily).
