Fifth stage
Shoulder disorders
Lec-1
.د
مثنى
6/12/2015
Shoulder disorders
symptoms:
Pain; in tip of the shoulder from rotator cuff or acromioclavicular (AC) joint
disorders.
Referred pain; from neck (eg. Cervical spondylosis), mediastinum (eg. IHD).
Stiffness (eg frozen shoulder).
Swelling.
Instability.
Weakness; as in neurological disorders or tendon rupture.
Signs
Expose both upper limbs, neck and chest.
Exam from front, behind and axilla.
Look:
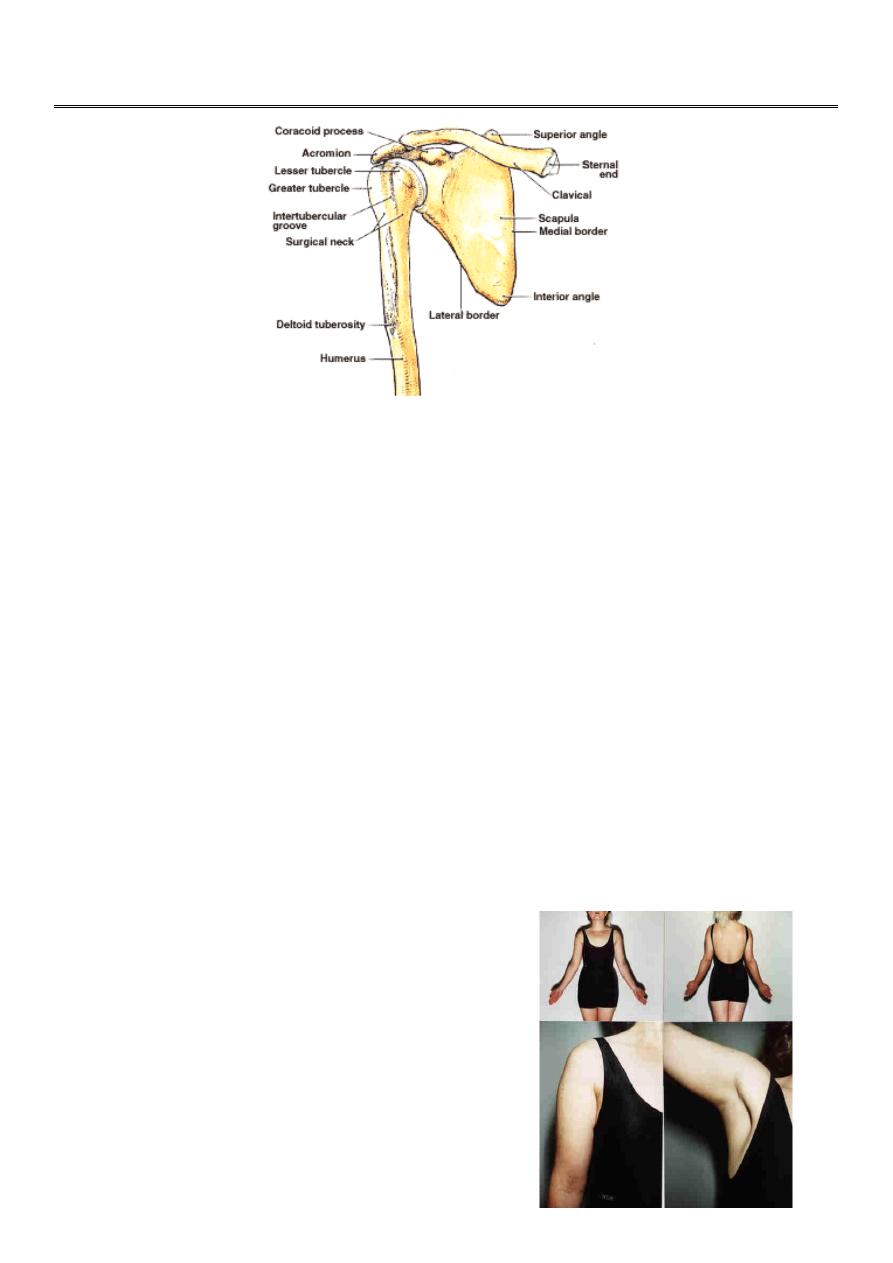
Skin; scar or sinus.
Shape; swelling,wasting or
deformity.
Position;
Swelling over acromioclvicular joint Echymosis
Wasting of the deltoid muscle
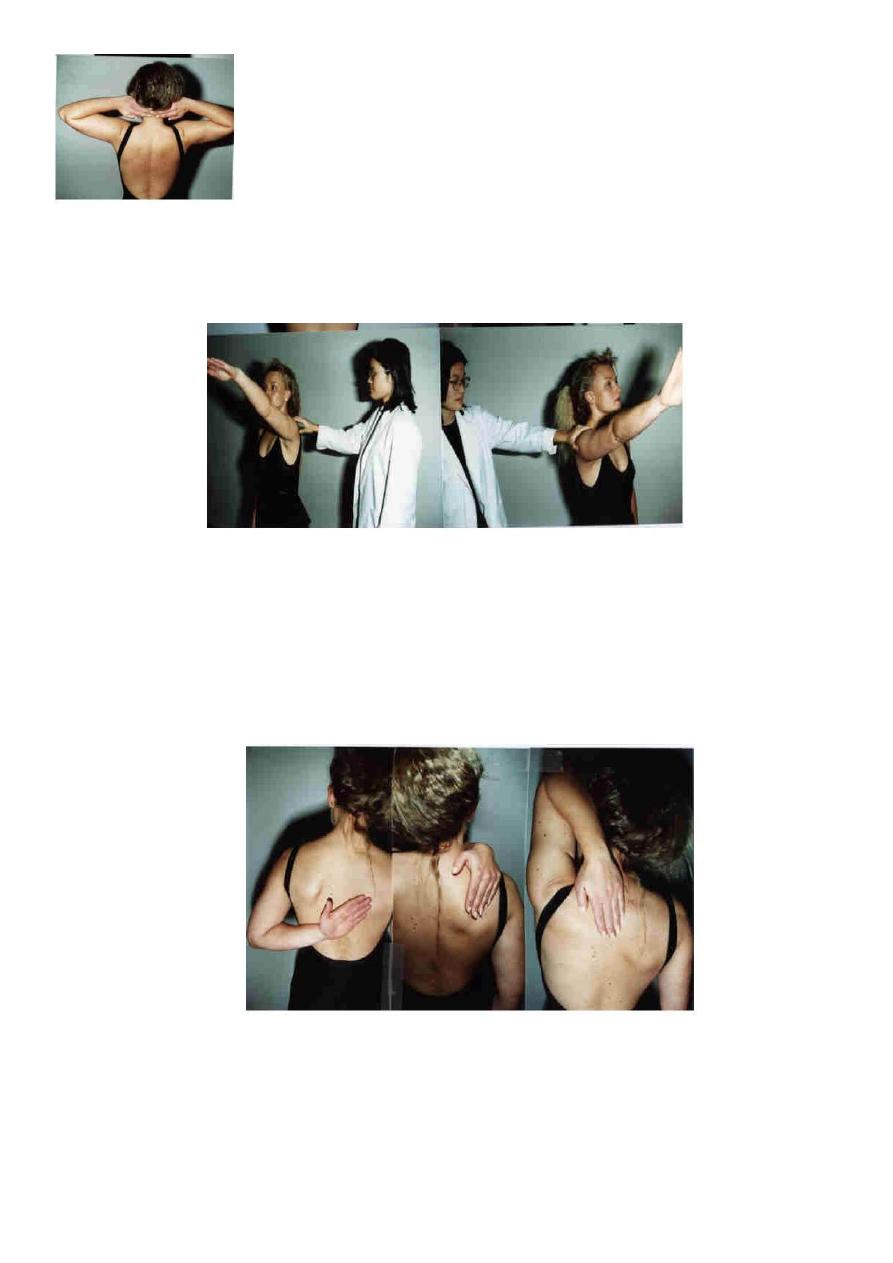
FEEL
Skin: temperature.
Bone and soft tissue points:
Sternoclavicular joint.
Acromioclavicular joint.
Bicipital groove.
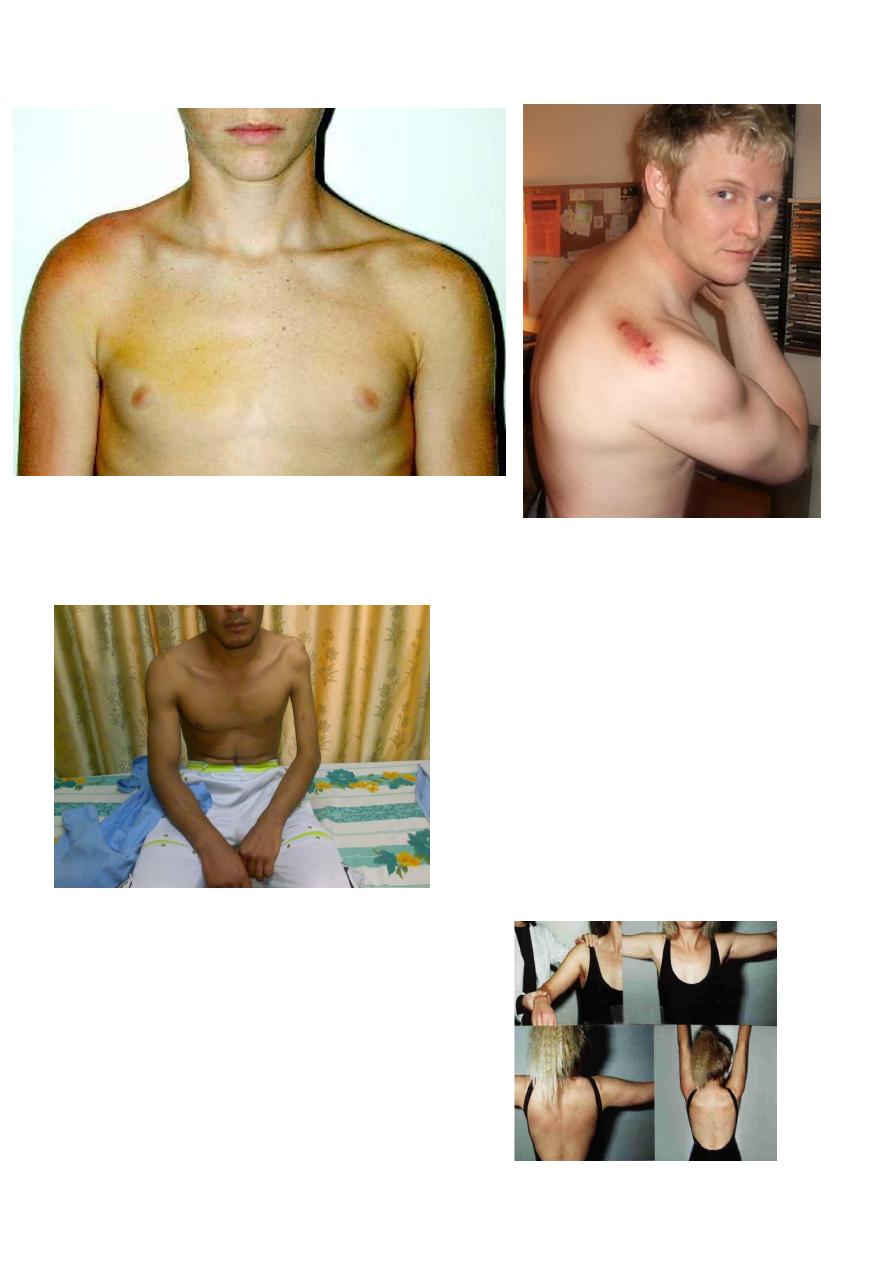
Move
Active movements:
Abduction: 0-90 degrees
glenohumeral movement. Last 60
degrees is scapulothoracic movement.
Flexion and extension: raise the arm
forwards and backwards.
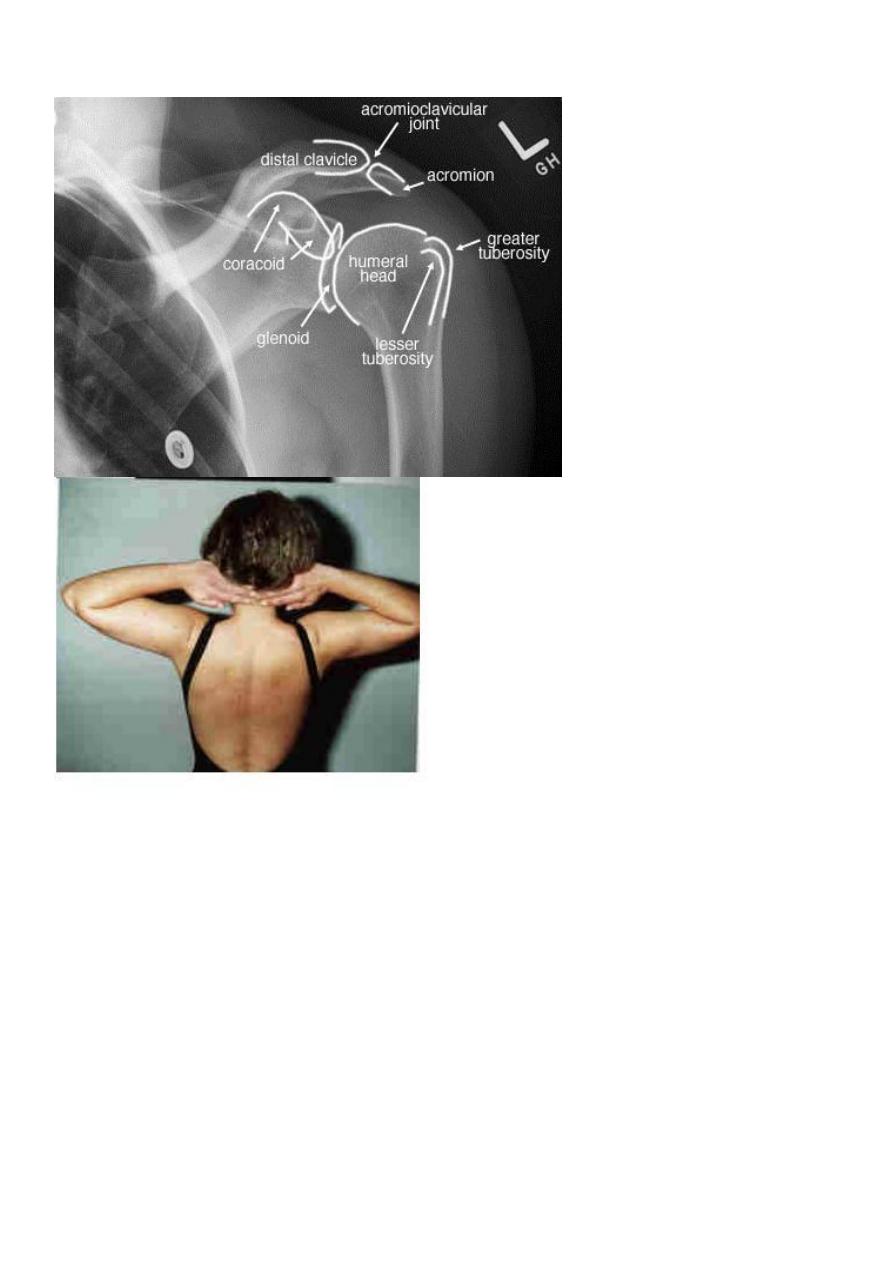
Rotation; external (ask the patient to clasp fingers behind the neck),
internal (reach up the back with fingers).
Disorders of the rotator cuff
The commonest cause of pain around the shoulder.
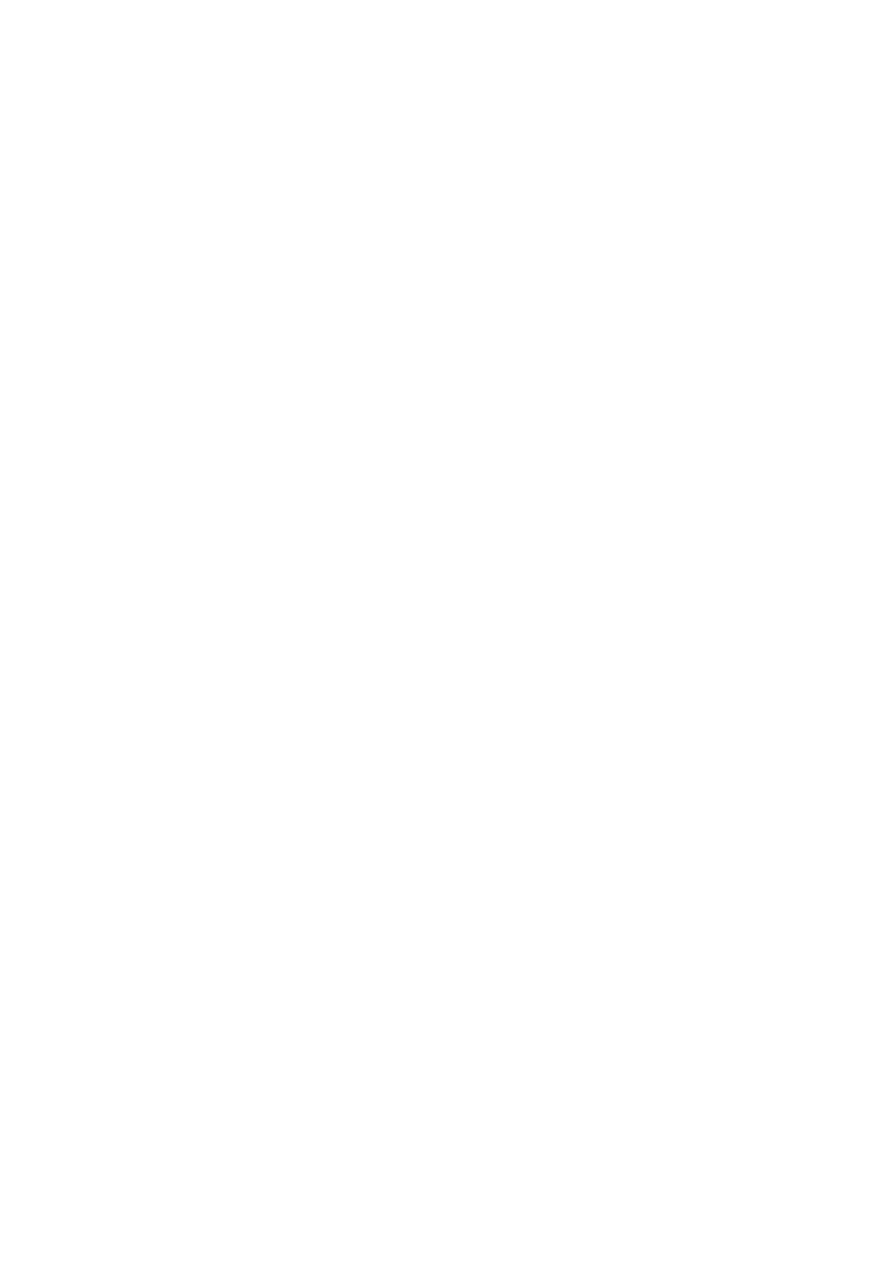
Rotator cuff anatomy
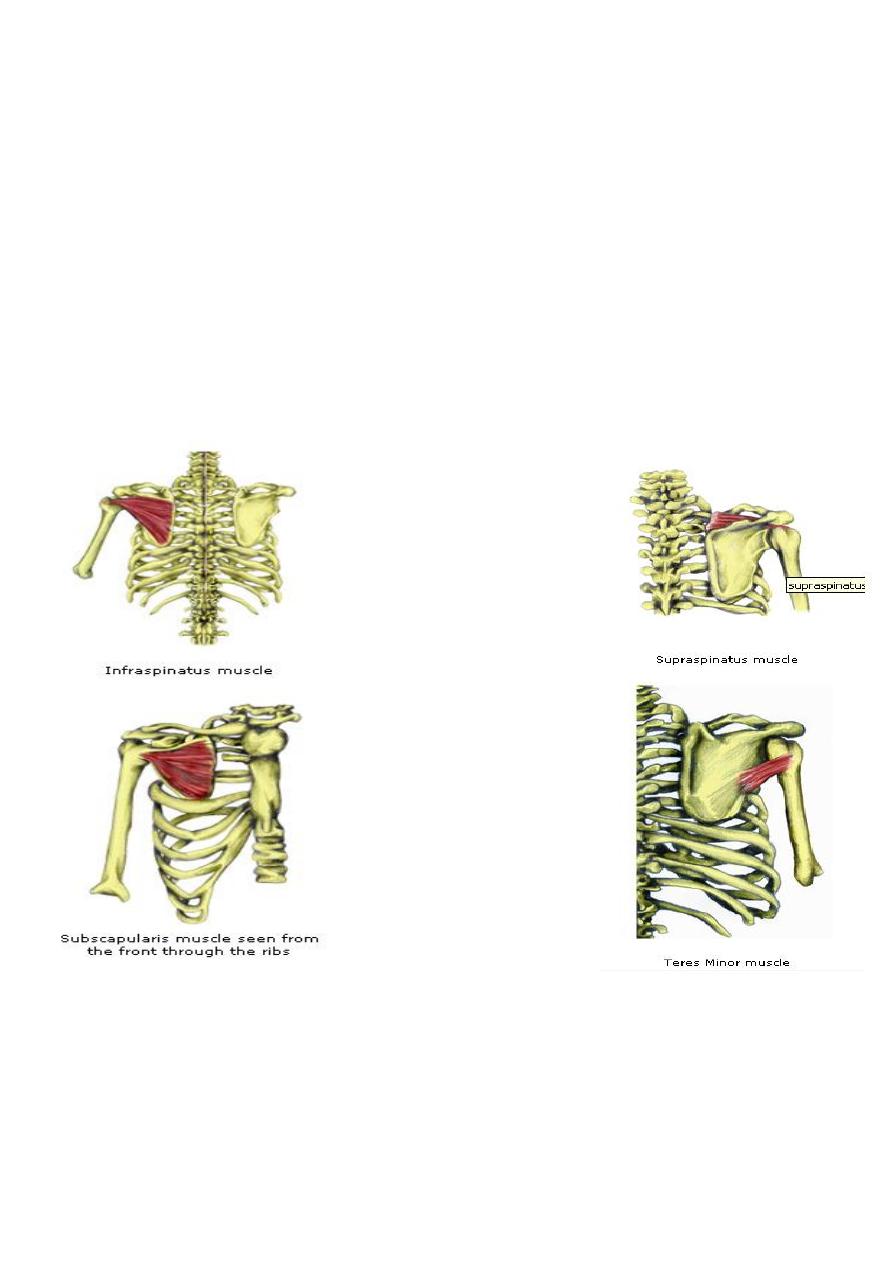
Consist of tendons of:
Supraspinatus.
Infraspinatus.
Subscapularis.
Teres minor.
Fused to the capsule of shoulder joint and insert around the greater
tuberosity.
Function: Abduction and stabilize the shoulder during movement.
Rotator cuff syndrome is caused by 5 conditions:
Supraspinatus tendinitis (impingement syndrome).
Rupture of the rotator cuff.
Acute calcific tendinitis.
Biceps tendinitis and /or rupture.
Adhesive capsulitis (frozen shoulder).
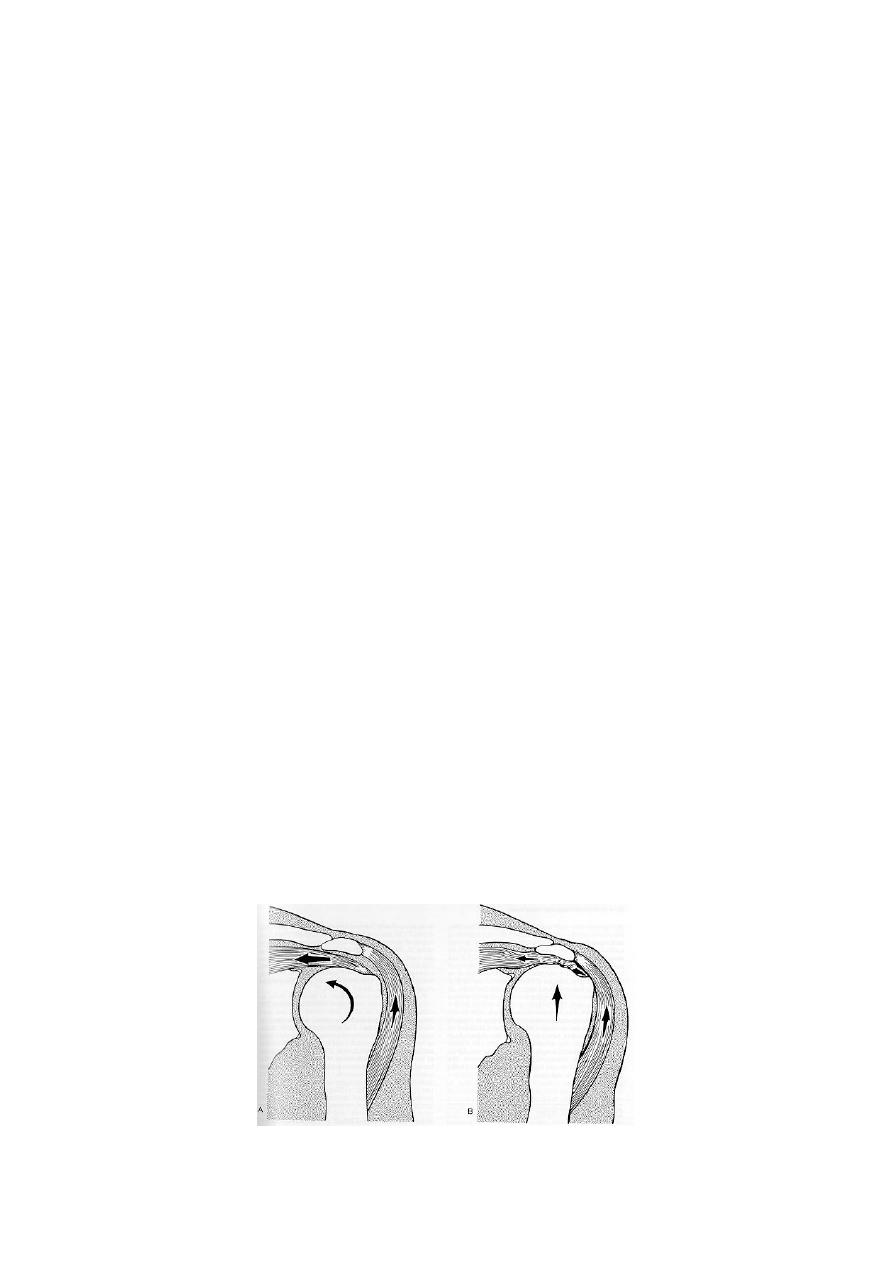
Impingement syndrome(supraspinatus tendinitis)
Cause: Repetitive compression or rubbing of the supraspinatus tendon
under the coracoacromial arch during abduction of the arm;
As in painting a wall or cleaning a window.
Other predisposing factors:
Acromiocalvicular joint OA,
Gout and rheumatoid arthritis.
Pathogenisis of supraspinatus tendinitis: (wear, tear and repair)
1. Edema and swelling,
2. Minute tears develop.
3. Scarring, fibrocartilagenous metaplasia or calcification in the tendon.
4. Healing or partial or complete tears.
5. The adjacent tendon of the long head of biceps often involved by
tendinitis or tear.
Clinical features 3 clinical patterns:
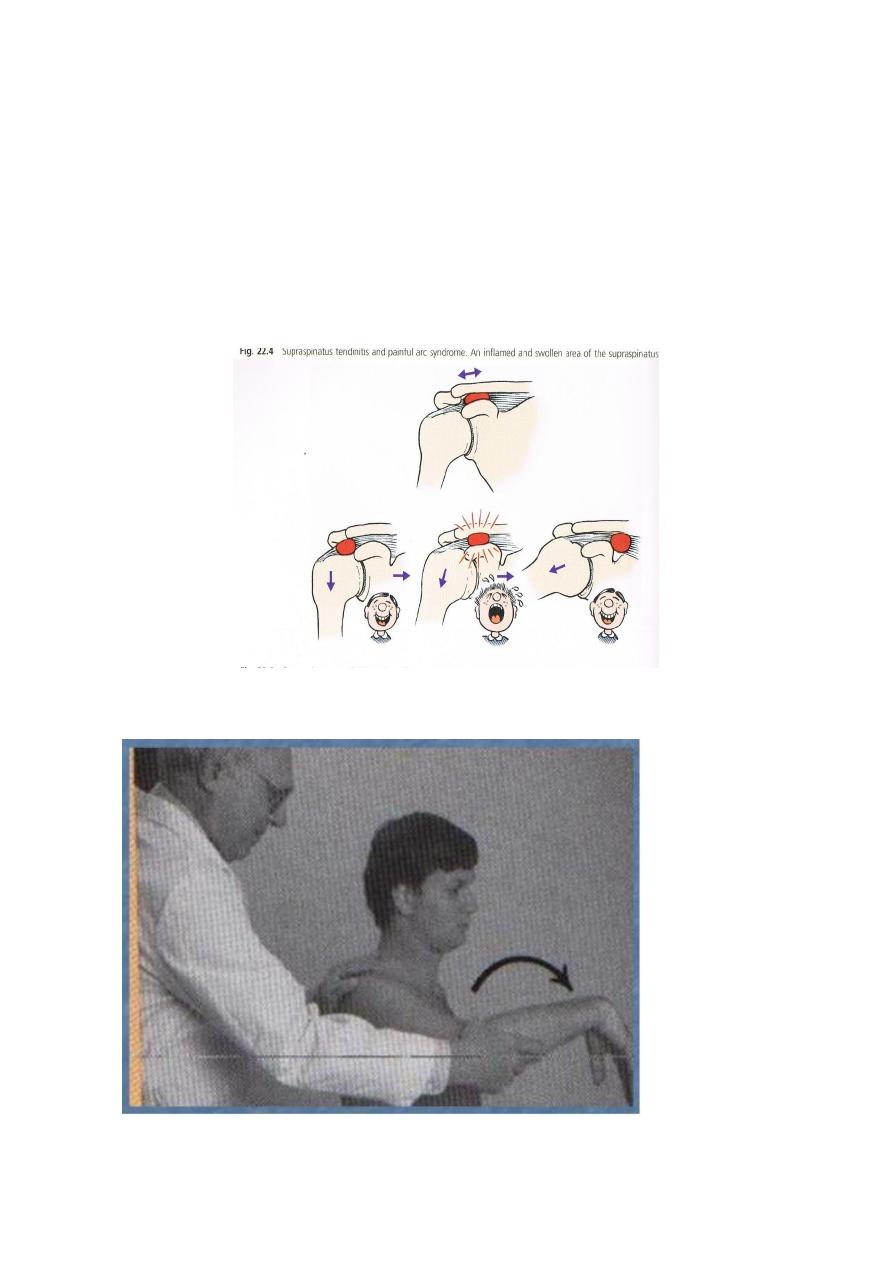
1. Subacute tendinitis (painful arc syndrome):
Age <40 years.
Anterior shoulder pain after vigorous or unaccustomed activity.
Tenderness over the anterior edge of the acromion.
The painful arc: pain on active abduction of the shoulder between 60
and 120 degrees.

2- Chronic tendinitis
Age 40-50 years.
History of recurrent attacks of subacute tendinitis.
Pain worse at night and on lying on affected side.
Slight stiffness.
Tenderness over the bicipital groove (biceps tendinitis).
3- Cuff disruption (partial or full thickness tear)
Age >45.
History of refractory shoulder pain with increasing stiffness and weakness.
Partial tears; abduction is possible but weak.
Full-thickness tear; abduction of the arm is not possible.
Full thickness RC tear
Treatment Conservative treatment
Uncomplicated impingement syndrome is often self-limiting by eliminating
the aggravating activity.
Avoid impingement position (abduction, slight flexion and internal
rotation).
Physiotherapy; ultrasound and active exercise.
NSAID. If fails,
Local injection of corticosteroid in the subacromial space.
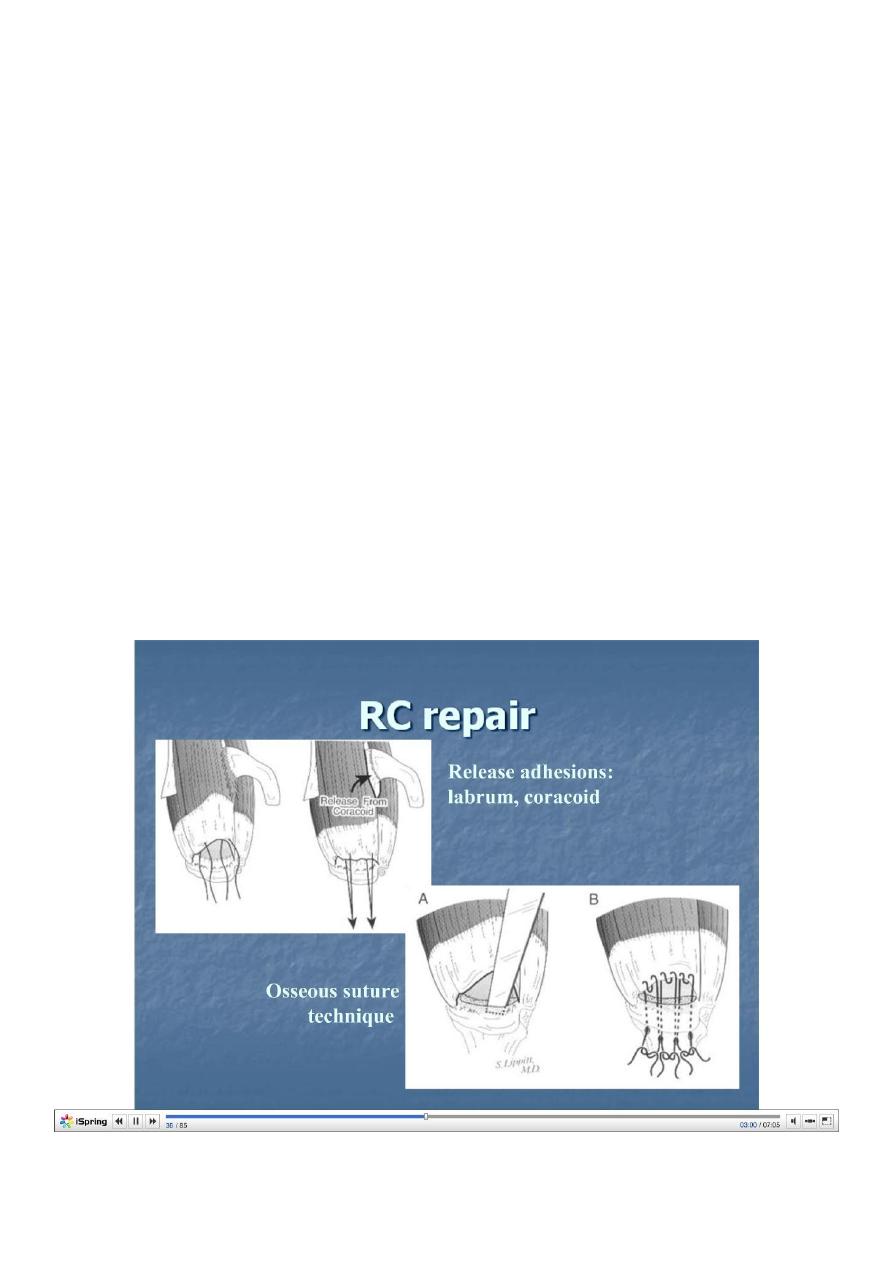
Surgical treatment
Indications:
Persistent symptoms >3months despite conservative treatment.
Younger patients with full thickness tear.
Open or arthroscopic acromioplasty.
Repair of rotator cuff tear.
Lesions of the biceps tendon-Tendinitis:
Usually associated with rotator cuff impingement.
Tenderness over
bicipital groove.
Treatment:
Rest.
Local heat and massage.
Corticosteroid injection in the bicipital
groove.
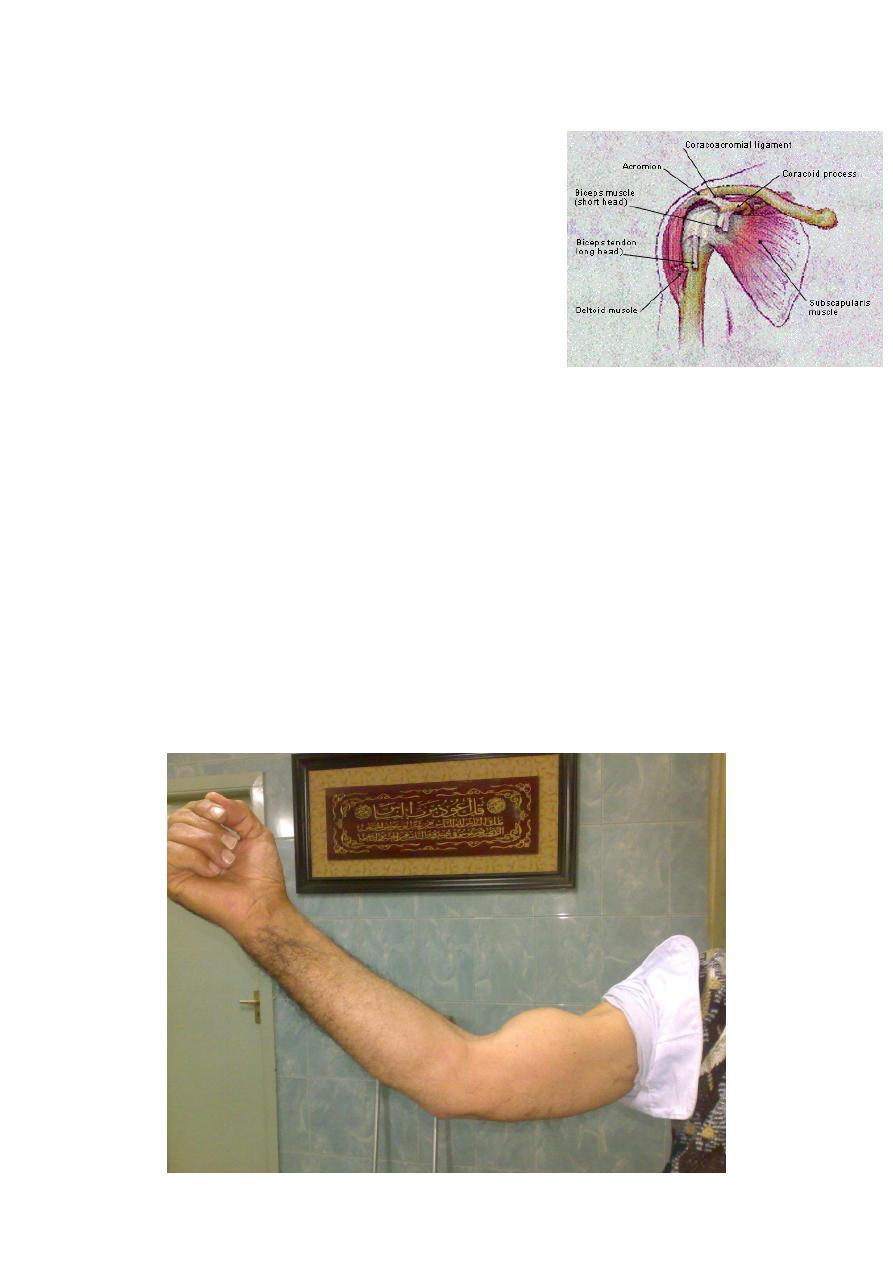
Rupture of long head of biceps
Usually accompany rotator cuff disruption.
Age >50.
Snap in the shoulder after lifting an object.
Lump in the lower arm on flexing the elbow.
Treatment; conservative.

Adhesive capsulitis (Frozen shoulder)
Progressive pain and stiffness of the shoulder which usually resolves
spontaneously after about 18 months.
Cause; unknown.
Pathology: fibroblast proliferation in the joint capsule.
Frozen shoulder
Associated with:
Diabetes mellitus.
Dupuytren’s disease.
Hyperlipidemia.
Hyperthyroidism.
Cardiac disease.
Hemiplegia.
Frozen shoulder Clinical features
Age: 40-60.
Pain; gradually increasing, disappear within 6 months.
Stiffness; gradually appears as the pain subside, persist for 6-12 months
then start thawing.
Passive and active movement is restricted in all directions.
Frozen shoulder Treatment
Conservaive: during the painful stage:
Reassurance.
Analgesics and antiinflammatory.
Exersice (pendulum).
After pain subside:

Manipulation under anesthesia with Steroid injection of
methyleprednisolone and lignocaine (risk of fracture neck of
humerus in porotic patients).
Surgical treatment
Surgical release is Indicated for persistent and disabling cases.