1
Fifth stage
Dermatology
كتابة الطالب
.د
عمر
2015/11/28
Important questions for dermatology - 2
Lec5:
Q: What are the signs and symptoms of scabies in adults and infants?
In adults:
Rash present for 4 to 8 weeks has suddenly become worse.
Generalized, severe itching
Nocturnal itching
Pinpoint erosions and crusts on the buttocks
Vesicles in the finger webs
Diffuse eruption sparing the face
Nodules on the penis and scrotum
Patient becomes better, then worse, after treatment with topical steroids.
Rash is present in several members of the same family.
In infants:
Widespread involvement usually due to misdiagnosis and Rx.
Sometimes the face and scalp are affected.
Vesicles are common on the palms and soles (characteristic).
Secondary eczematization and impetiginization are common.
Burrows are difficult to find.
Nodules may be seen in the axillae and diaper area.
Q: How you treat scabies?
1- Permethrin (cream)
Is the drug of choice for the treatment of scabies in children and adults of all ages
including pregnant and lactating women.
Two applications 1 week apart, apply from head/neck to toe and wash after 8-12 hours
(for permethrin and lindane).
2- Lindane (cream, shampoo, and lotion)
3- BENZYL BENZOATE
4- CROTAMITON
2
5- SULFUR
The pharmacist mixes 5% to 10% precipitated sulfur in petrolatum.
The compound is applied to the entire body below the neck once each day for 3 days
and the patient is instructed to bathe 24 hours after each application.
These preparations are messy, have an unpleasant odor, stain, and cause dryness.
Sulfur in petrolatum is thought to be safe for infants <2 months old and pregnant and
nursing women.
6- Ivermectin
Q: Write short notes about Nits?
The female lays approximately six eggs, or nits, each day for up to 1 month, and then
dies.
Nits are 0.8 mm long and are firmly cemented to the bases of hair shafts close to the
skin to acquire adequate heat for incubation.
Nits are very difficult to remove from the hair shafts.
Q: How you treat pediculosis?
Permethrin (1% and 5%) is the most effective treatment. It paralyzes the nerves that allow
the lice to breathe.
Remains active for 2 weeks.
Only apply to dry hair.
It is insecticidal and ovicidal.
Two applications (10 min. each) one week apart.
Permethrin has a clinical efficacy of 95%.
Lindane and pyrethrin have cure rates less than 90%.
Malathion
Ivermectin
Co-trimoxazole (480mg twice daily for 3 days), and repeated after 1 week.
Shaving the head
Nit removal (Combing)
Fomite control
Eye infestation: Baby shampoo or Vaseline; Ivermectin.
3
Q: Management of leishmaniasis?
History:
History of travel (or living) to an endemic area in the previous weeks or months.
History of insect (sandfly) bites in the previous weeks or months.
History of high-risk activities such as sleeping outdoors.
Non-healing chronic nodular, violaceous ulcer for 4–6 weeks or longer.
Examination:
Chronic nodules – dusky red in color – ulcerated or crusted – non-healing – on exposed
body parts.
Investigations:
Demonstration of amastigotes in Giemsa-stained smears from infected skin by direct
microscopy.
Demonstration of intracellular amastigotes in the dermis of H & E skin sections.
Growth of promastigotes in Nicolle–Novy–MacNeal (NNN) culture medium from
lesional specimens
Demonstration of leishmanial DNA by PCR.
Treatment:
Try topical treatment methods for simple sores.
Reserve the systemic use of pentavalent antimonials for problematic sores: these
include:
1.Sores where scarring would be disabling or severely disfiguring.
2.Sores that will not heal easily (on shin or over a joint).
3.Sores involving mucosa or cartilage.
Weekly intralesional sodium stibogluconate PLUS daily oral itraconazole 100 mg (or
allopurinol) for 6 to 8 weeks.
IM sodium stibogluconate in a single daily dose of 20 mg/kg for 15–21 days.
Severe scarring may require plastic repair.
After healing, patients are normally immune to reinfection with the same species.
Lec6:
Q: Write short notes about impetigo?
A highly infectious skin disease, which commonly occurs in children.
The causative organism is usually Staphylococcus Aureus (>90% cases1), but less often
can be strep pyogenes.
Begins as a vesicle, which may enlarge into a bulla.

4
Weeping, exudative area with characteristic honey coloured or golden, gummy crusts,
which leave denuded red areas when removed.
May present as macules, vesicles, bullae or pustules
Bullae are more prominent in staphylococcal infection and in infants
Impetigo
Treatment:
Mild localised cases - use topical antibiotic Polyfax
Widespread or more severe infections – use systemic antibiotics, such as
flucloxacillin (or erythromycin if penicillin allergic)
Q: Write about viral warts?
Caused by human papilloma virus
Main types, common, plane and plantar
Very common
Disappear spontaneously eventually
If treatment is needed, options include:
Salicylic acid topically – needs daily treatment and can take months
Cryotherapy
Imiquimod cream
Note description = nodule, well circumscribed, round or oval shape, rough surface, dry,
cracked, black dots (thrombosed vessels).
Q: Write about shingles and post herpetic neuralgia?
Herpes Zoster (Shingles)
Caused by reactivation of the chickenpox virus which has lain dormant in the dorsal
root or cranial nerve ganglia
Rash is preceded by a prodromal phase of up to 5 days of tingling or pain
Then develop painful grouped vesicles/pustules on a red base in a dermatomal
distribution.
Most common in thoracic and trigeminal areas
Lesions become purulent, then crusted
Healing takes place in 3-4 weeks
Shingles treatment
Aciclovir 800mg 5 times daily, for 7 days
Rest, analgesia usually gabapentine.

5
Post-herpetic Neuralgia
Pain lasting longer than 3 months after the rash.
The followings are risk factors for developing post-herpetic neuralgia?
A: Older age
B: More severe pain during the eruption
C: Severely inflamed rash
D: Prodromal pain in dermatome
Lec7:
Q: Write about pathogenesis of acne?
Increased sebum production (androgens)
Abnormal keratosis (androgens)
bacterial proliferation (Propionibacterium acnes)
inflammation
Q: Enumerate the clinical manifestations of acne?
Closed comedone (whitehead)
Open comedone (blackhead)
Papules
Pustules (pimples)
Cysts and nodules
Q: Write about classification of acne?
Comedonal acne: Only comedons
Mild acne: Less than 20 pustules.
Moderate to severe acne: More than 20 pustules
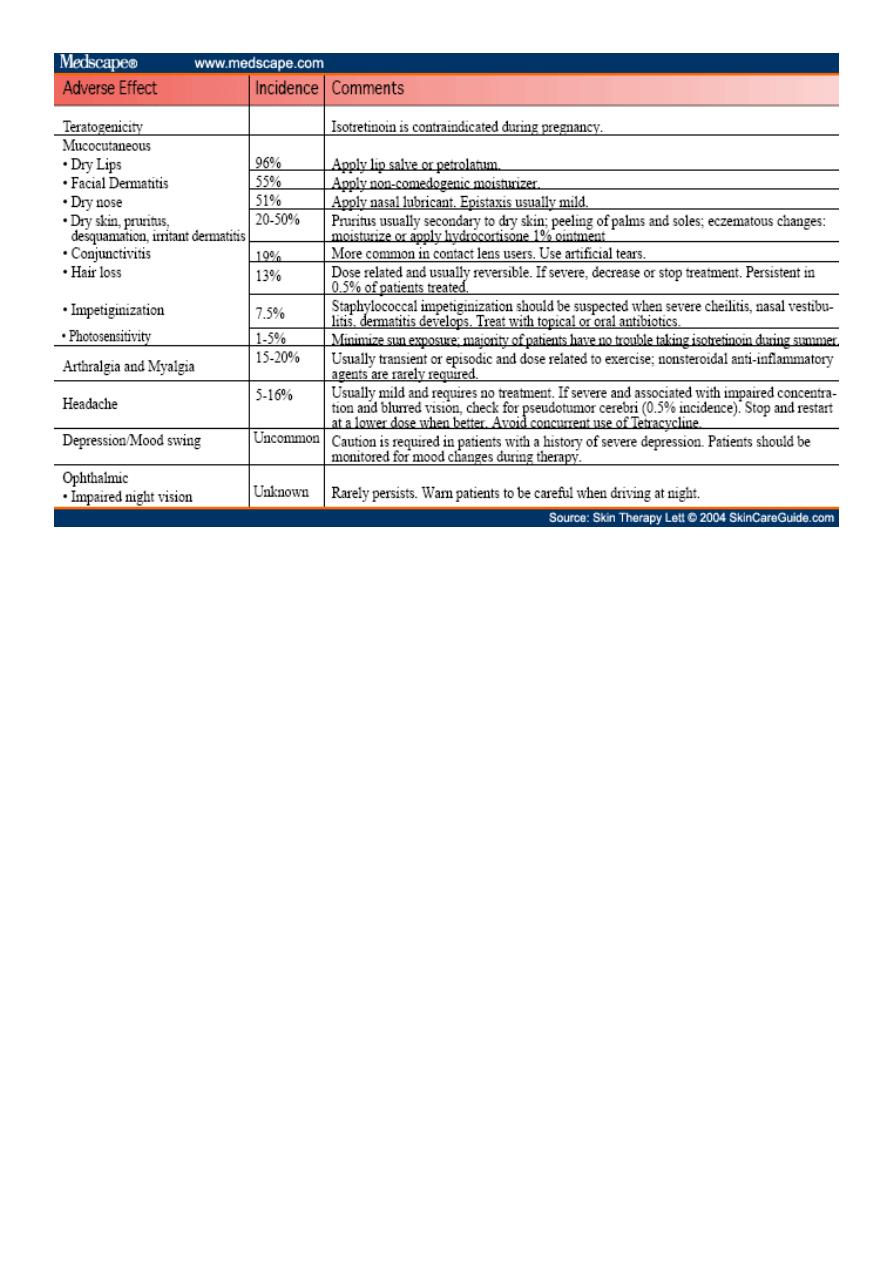
Q: Write about treatment of acne and side effects?
Antibiotics: Topical (clindamycin and erythromycin) and systemic antibiotics used in
the treatment of acne vulgaris are directed at Propionibacterium acnes.
Minocycline, Doxycycline (50 t0 200 mg / day for 3 months), Tetracycline, Lymecycline
Retinoids: These agents decrease the cohesiveness of abnormal hyperproliferative
keratinocytes.
Isotretinoin (systemic) 0.5 - 1 mg per kg over 4 to 6 months
Tretinoin (topical) cream (0.025%, 0.05%, 0.1%)
6
Notes:
Lesions of scabies:
o PRIMARY LESIONS Burrow, Vesicles, Papules
o SECONDARY LESIONS Pinpoint erosions, Pustules, Eczematous changes, Nodules
Scabies in elderly presented as itching, but they have normal skin.
Complications of scabies eczematous inflammation, pyoderma, post scabietic
pruritis, nodular scabies.
Folliculitis
o Inflammation of the hair follicle.
o Presents as itchy or tender papules and pustules at the follicular openings.
o Complications include abscess formation and cavernous sinus thrombosis if upper
lip, nose or eye affected.
Cellulitis
o Infection of the deep subcutaneous layer of the skin
o Presents as a hot, tender area of confluent erythema of the skin
o Can cause systemic infection with fever, headache and vomiting.
o Erysipelas is more superficial and has a more well demarcated border Erysipelas
o Streptococcus – Group A Strep Pyogenes.
o Treated by local and systemic antibiotics
