Fifth stage
PediatricLec-4
Dr. Athal Humo
7/12/2015
Cardiovascular SystemHeart Failure (HF)
Heart failure occurs when the heart is unable to pump blood at a rate proportionate with metabolic needs (oxygen delivery).
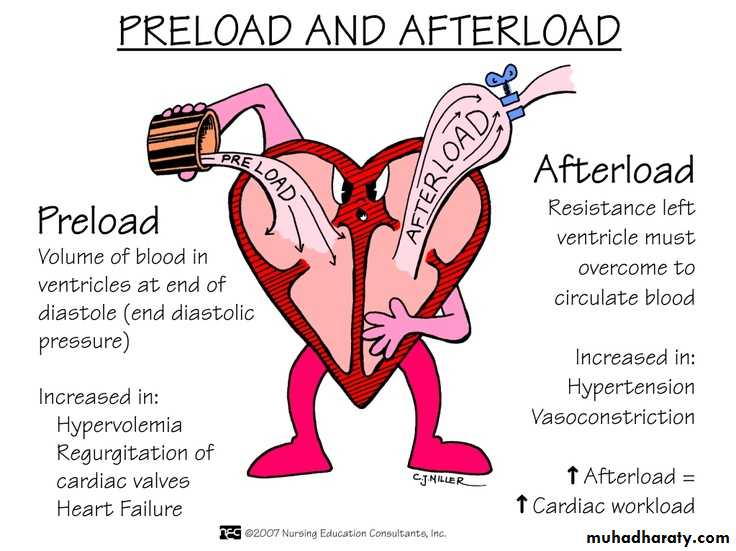
It may be due to:
change in myocardial contractility that results in low cardiac output.
abnormal loading conditions being placed on the myocardium.
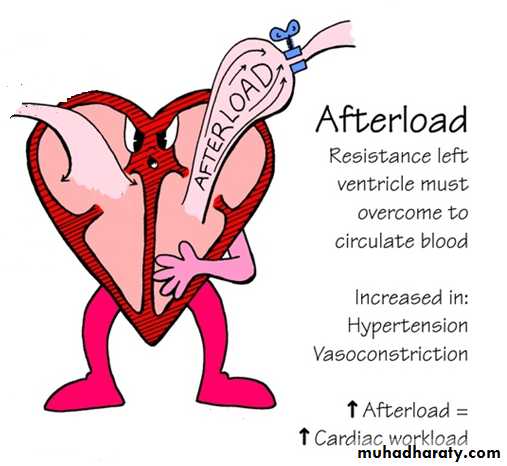
afterload (pressure overload, such as with AS, PS, or CoA).
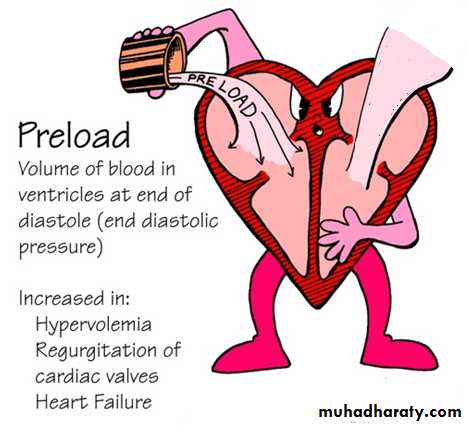
preload (volume overload, such as in VSD, PDA, or valvular insufficiency).
Volume overload is the most common cause of heart failure in children
ETIOLOGY:
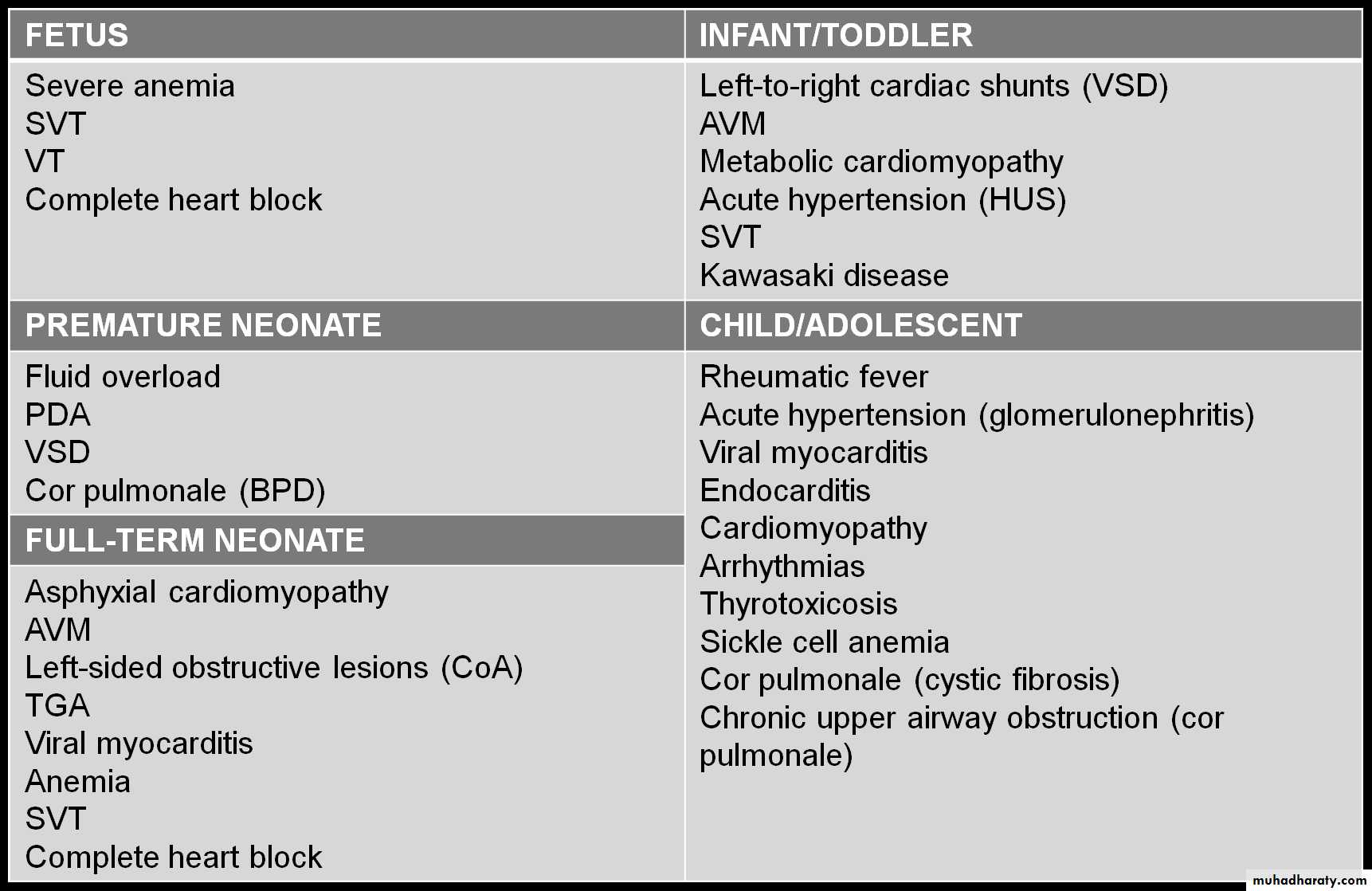
It is helpful to approach the differential diagnosis of heart failure based on age of presentation.
Etiology of Heart Failure by Age Group
Other Etiological Classification:
CARDIACcongenital structural malformations
● excessive preload
● excessive afterload
no structural anomalies
● cardiomyopathy
● myocarditis
● myocardial infarction
● acquired valve disorders
● hypertension
● kawasaki syndrome
● arrhythmia (bradycardia or tachycardia)
NONCARDIAC
● Anemia
● Sepsis
● Hypoglycemia
● Diabetic ketoacidosis
● Hypothyroidism
● Other endocrinopathies
● Arteriovenous fistula
● Renal failure
● Muscular dystrophies
CLINICAL MANIFESTATIONS
Symptoms
Children do not present with the typical features of CHF as seen in adults.
Age is very important when assessing child.
Infants:
Poor feeding
Failure to thrive
Tachypnea
diaphoresis with feeding.
Older children:
SOB
Easy fatigability
Edema.
Signs
Findings depend on whether pulmonary venous congestion, systemic venous congestion, or both are present.
Tachycardia, a gallop rhythm, and thready pulses may be present with either cause.
If LHF is predominant: tachypnea, orthopnea, wheezing, and pulmonary edema are seen.
If RHF: Hepatomegaly, edema, and distended neck veins.
Investigation:
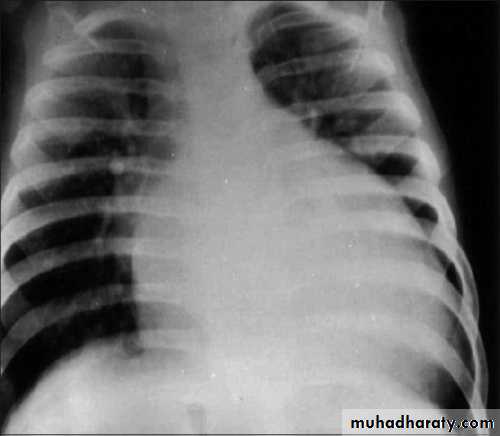
CXR: the absence of cardiomegaly on a chest x-ray usually rules out the diagnosis of heart failure.
Echocardiogram:
assesses the heart chamber sizes.measures myocardial function.
diagnoses CHD when present.
TREATMENT
The goals of medical therapy for CHF include the following:
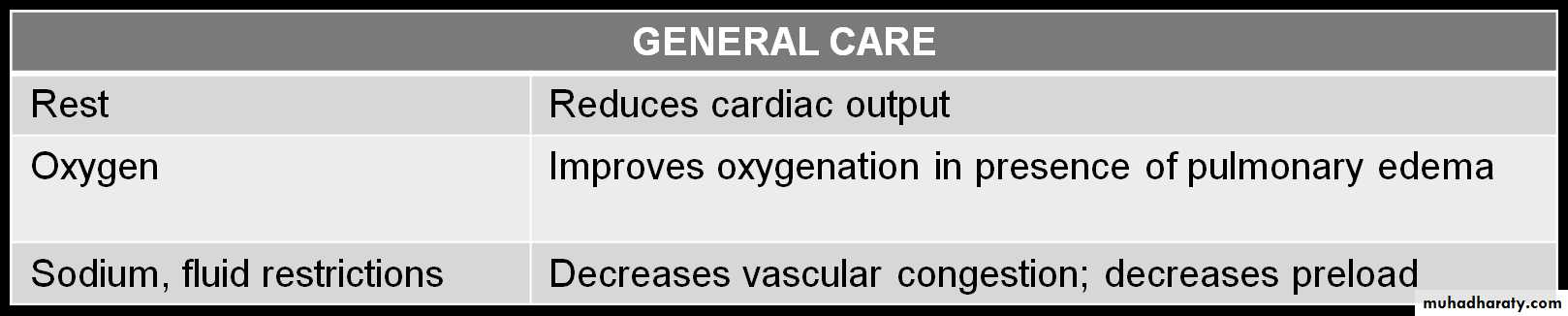
Reducing the preload
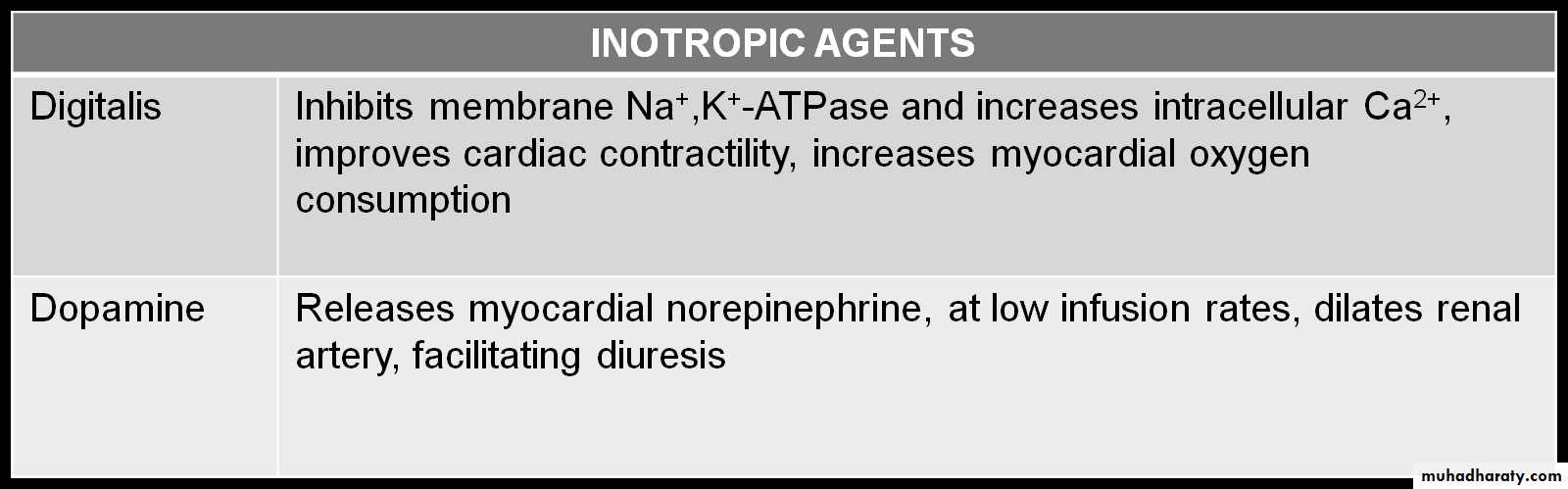
Enhancing cardiac contractility
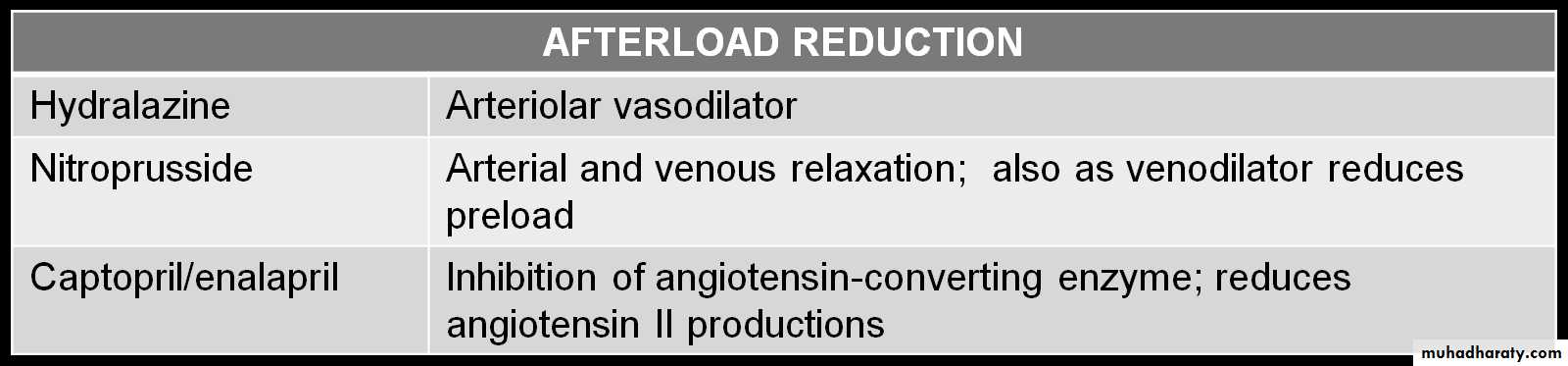
Reducing the afterload
Improving oxygen delivery
Enhancing nutrition
Remember
O2
Treatment underlying cause
+ 4Ds :
Diet: low salt and high calories
Digitals: Improve the cardiac contractility
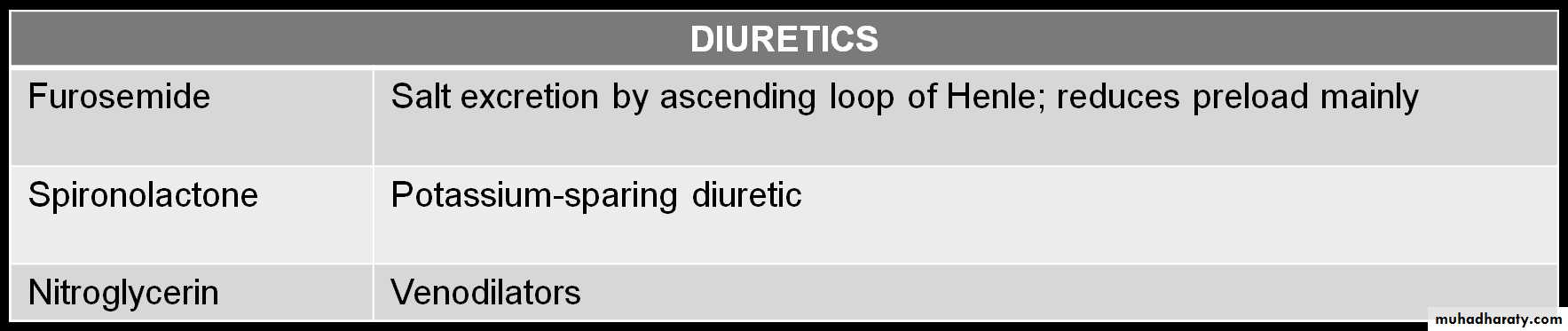
Diuretics: Reducing preload as frusemide
Dilators: Reducing afterload as ACE
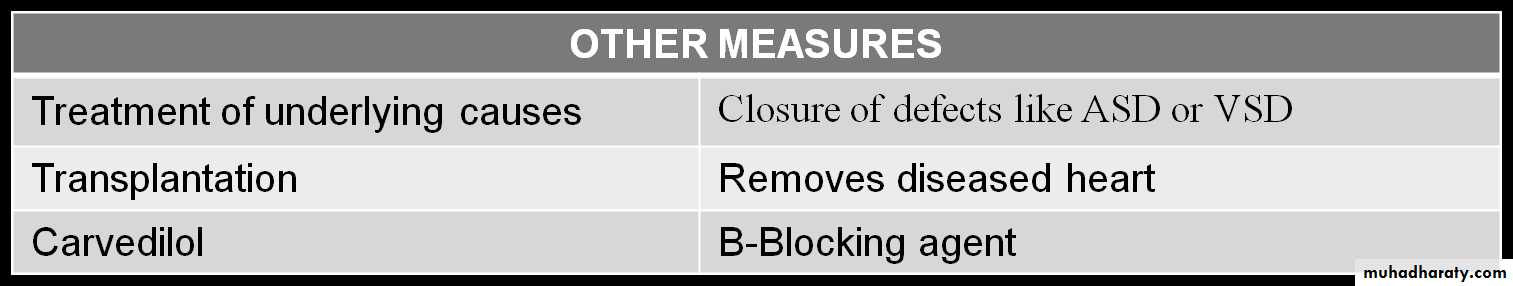
Treatment
Reducing preload
Improve the cardiac contractility
Reducing afterload
Doses:
Furosemide: 1 mg/kg/dose PO or IVHydrochlorothiazide: 2 mg/kg/d PO divided bid
Digoxin :TDD followed by maintenance.
IV Dopamine : 5-10 mcg/kg/min IV (usual dosage; maximal dosage May be up to 28 mcg/kg/min)
Dobutamine: 5-10 mcg/kg/min iv
Captopril: 0.1-0.5 mg/kg/d PO divided q8h
Enalapril: 0.1 mg/kg/d PO divided qd/bid, not to exceed 0.5 mg/kg/d
Carvidolol: 0.2-0.4 mg/kg/dose bid.
Spironolactone: 1-3 mg/kg/day.
DIGOXIN
Rapid digitalization can be achieved by administration of “total digitalizing dose (TDD) as follow:
Premature: 20 μg/kg
Full-term neonate (up to 1 mo): 20-30 μg/kg
Infant or child: 25-40 μg/kg
Adolescent or adult: 0.5-1 mg in divided doses
NOTE: These doses are PO; IV dose is 75% of PO dose Maintenance digoxin 5-10 μg/kg/day, divided q12h
Managing Acute Congestive Heart Failure (Acute Pulmonary Edema) in Children:
Admit to the ICU.
Head up position.
Oxygen.
IV furosemide: 1-2mg/kg.
Digoxin (TDD).
Dopamine if ↓BP: (5-10 mcg/kg/min) .
Nitrates (nitroprusside, nitroglycerin) as venodilators.
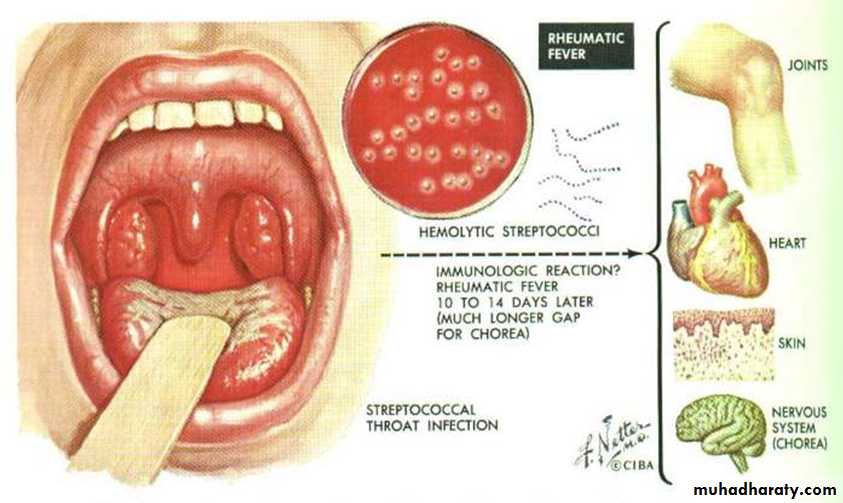
Rheumatic Fever
It is due to an immunologic reaction that is a delayed sequela of group A beta-hemolytic streptococcal infections of the pharynx.
A family history of rheumatic fever and lower socioeconomic status are additional factors.
It is most common in children 6 to 15 years of age.
Diagnosis:
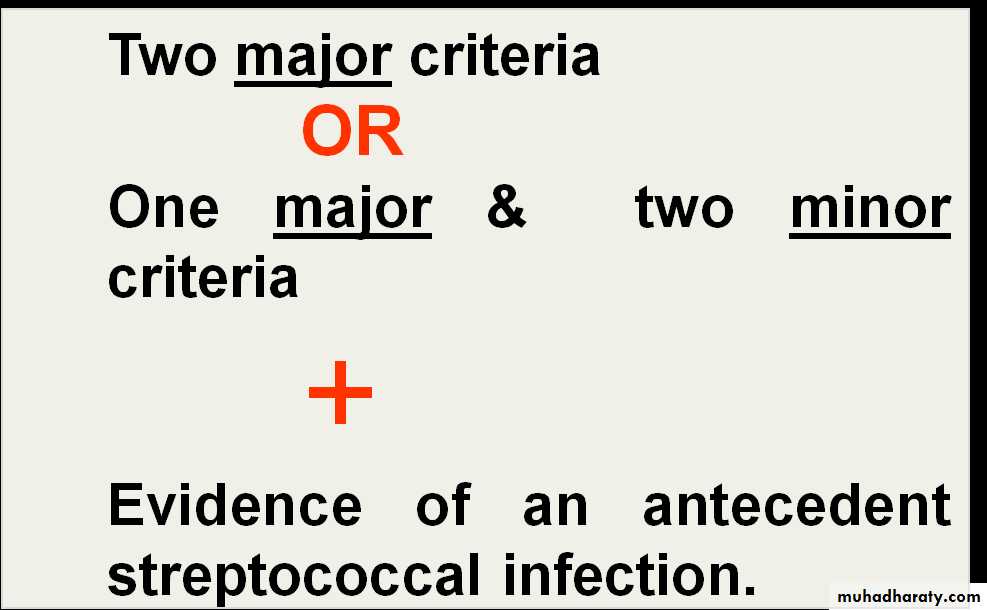
Acute rheumatic fever is diagnosed using the clinical and laboratory findings of the revised Jones criteria.
The presence of either :
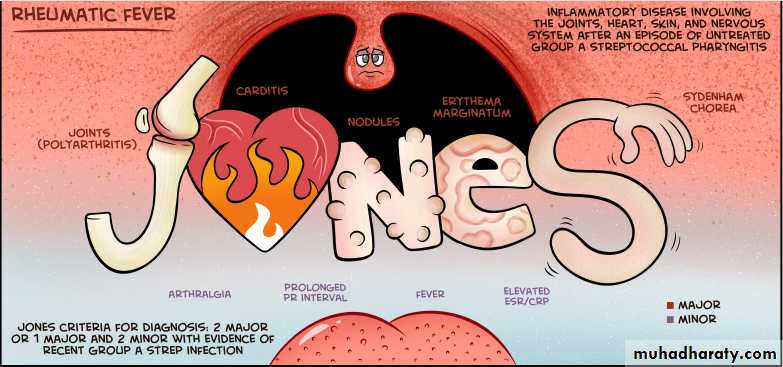
JONES CRITERIA
Major Jones Criteria for Diagnosis of Acute Rheumatic Fever
PolyarthritisCarditis
Subcutaneous nodules
Erythema marginatum
Chorea (Sydenham disease)
The presence of Sydenham’s chorea alone is sufficient for diagnosis
Minor Jones Criteria for Diagnosis of Acute Rheumatic Fever
Fever (temperatures 38.2°- 38.9°C).
Arthralgias.
Previous rheumatic fever.
Leukocytosis.
Elevated ESR/CRP.
Prolonged PR interval.
Evidence of recent group A streptococcal disease
The infection often precedes the presentation of rheumatic fever by 2 to 6 weeks.
Scarlet fever.
Positive throat culture.
Elevated antistreptolysin O or other antistreptococcal antibodies, it is the most reliable laboratory evidence of prior infection.
TREATMENT:
Management of acute rheumatic fever consists of:
Bed rest
Antibiotic:
Single dose benzathine penicillin 1.2 million unit im
Or 10 days of orally administered penicillin or amoxicillin
Salicylates after the diagnosis is established, 50-70 mg/kg/day in 4 divided doses PO for 3-5 days, followed by 50 mg/kg/day in 4 divided doses PO for 3 wk and half that dose for another 2-4 wk.
In severe carditis or CHF:
prednisone is 2 mg/kg/day in 4 divided doses for 2-3 wk followed by half the dose for 2-3 wk and then tapering of the dose by 5mg/24 hr every 2-3 days.
When prednisone is being tapered, aspirin should be started at 50 mg/kg/day in 4 divided doses for 6 wk to prevent rebound of inflammation.
Additional supportive therapy for heart failure or chorea may be necessary during the acute presentation.
PREVENTION
1ry prevention:
Appropriate antibiotic therapy of acute GAS pharyngitis is highly effective in preventing first attacks of acute rheumatic fever.
2ry prevention:
Benzathine Penicillin every 4 wk.
600,000 IU for children weighing ≤60 lb
1.2 million IU for children weighing >60 lb
Duration of prophylaxis for pt.
without carditis: 5years or until he is 21 years old.
With carditis : into adulthood and perhaps for life.
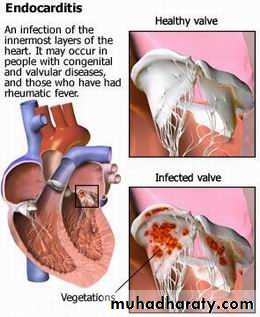
Infective Endocarditis
Infective endocarditis is an infection on the endothelial surface of the heart, including the heart valves.
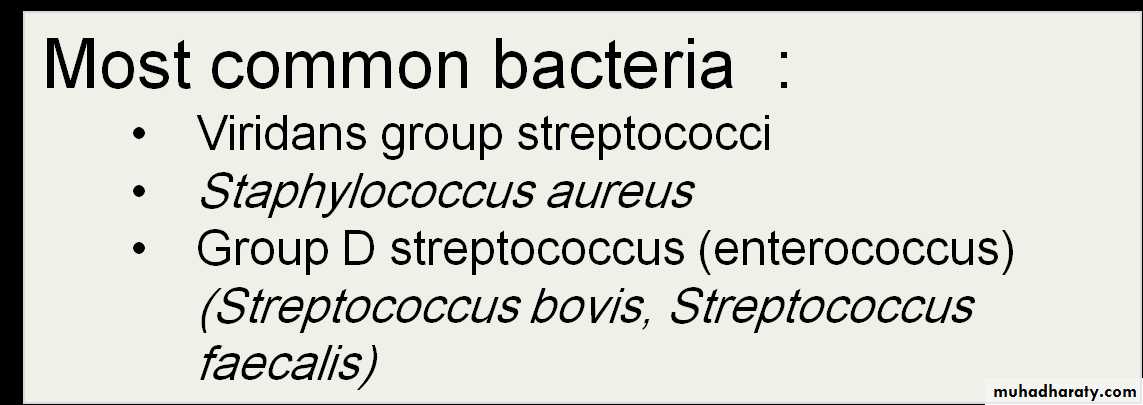
ETIOLOGY
Bacteria:Acute
Subacute
Non bacteria:
viruses, fungi, and other microbiologic agents.Staphylococcal endocarditis is more common in patients with no underlying heart disease.
Viridans group streptococcal infection is more common after dental procedures.
Group D enterococci are seen more often after lower bowel or genitourinary manipulation.
Pseudomonas aeruginosa is seen more frequently in intravenous drug users.
Fungal organisms are encountered after open heart surgery.
Coagulase-negative staphylococci are common in the presence of an indwelling central venous catheter.
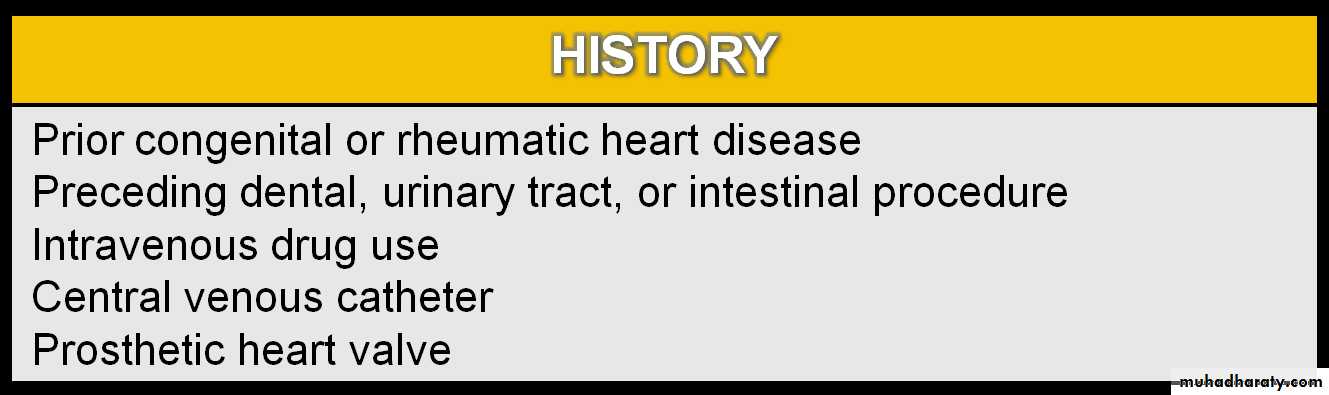
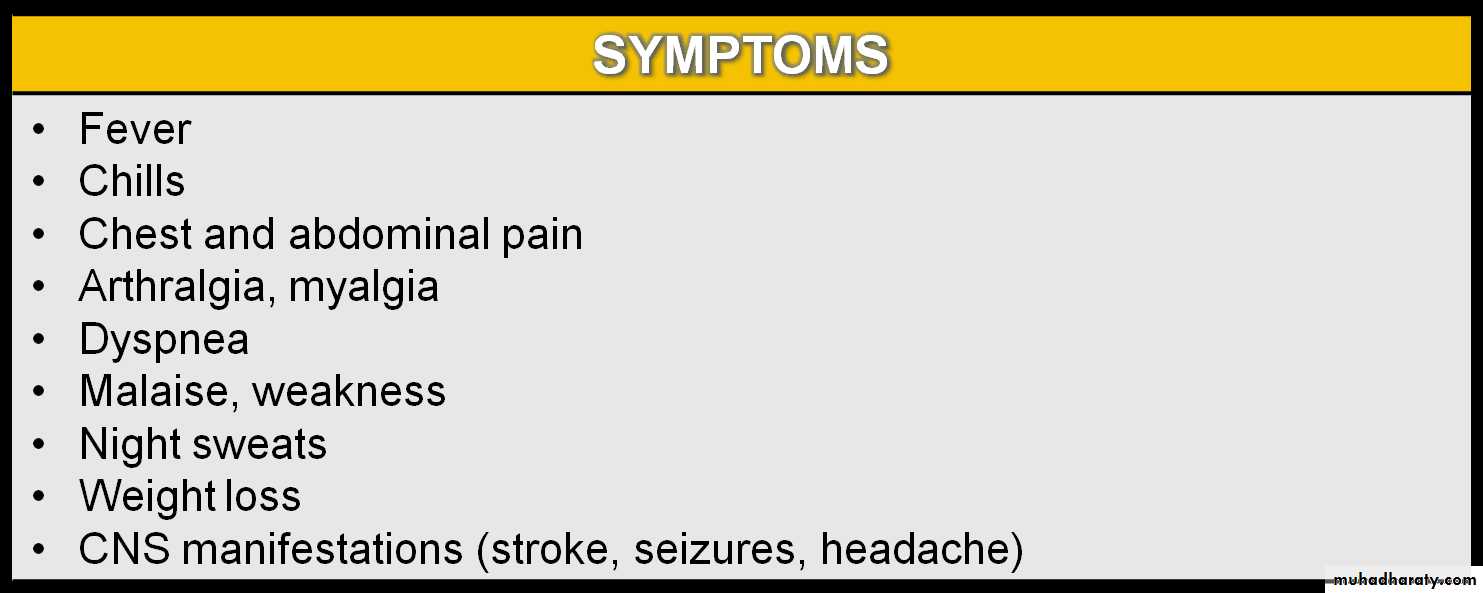
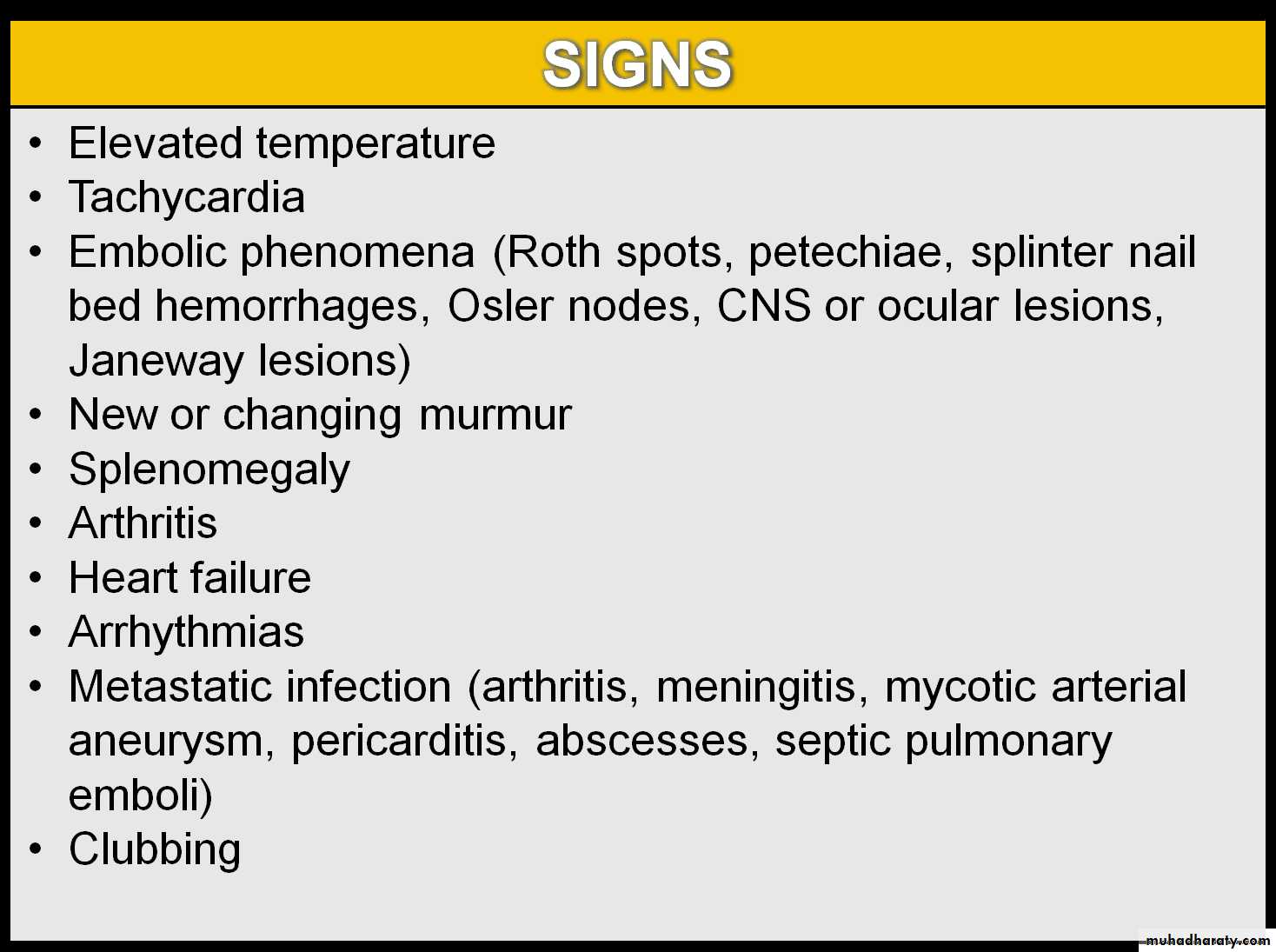
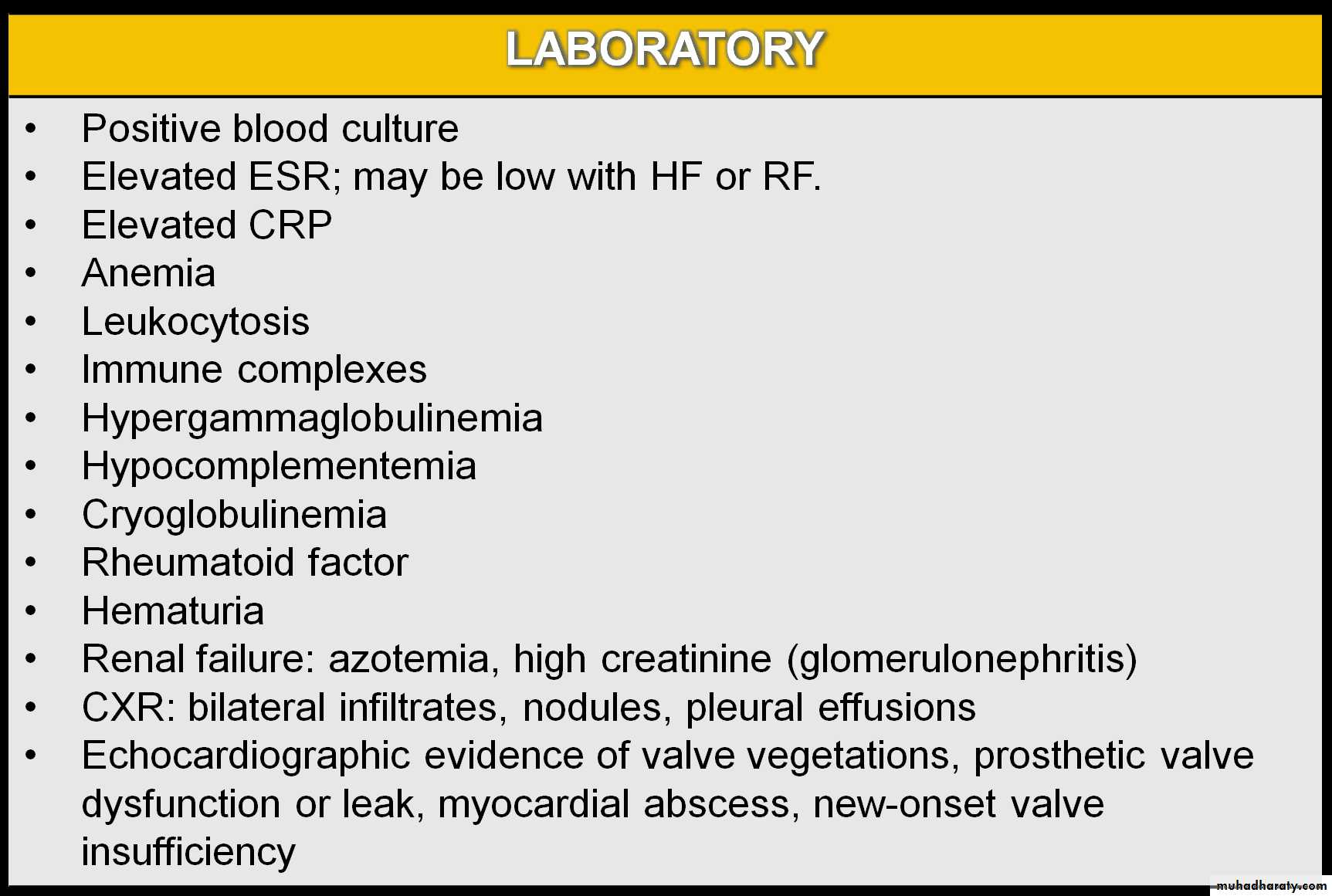
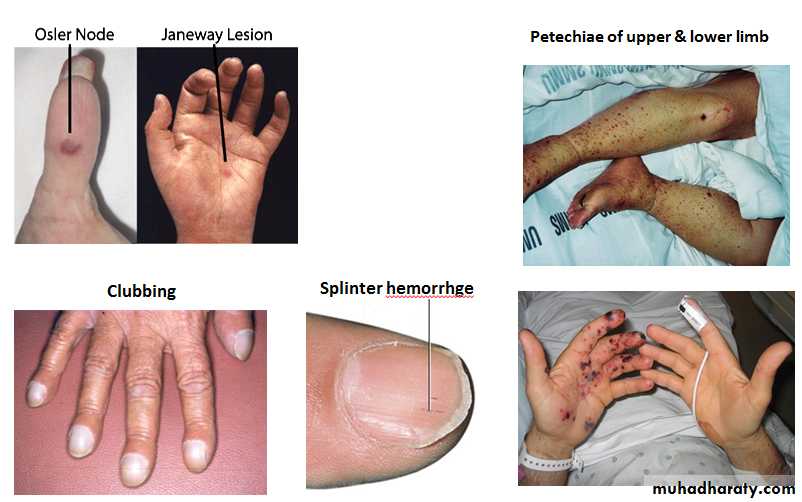
Manifestations of Infective Endocarditis
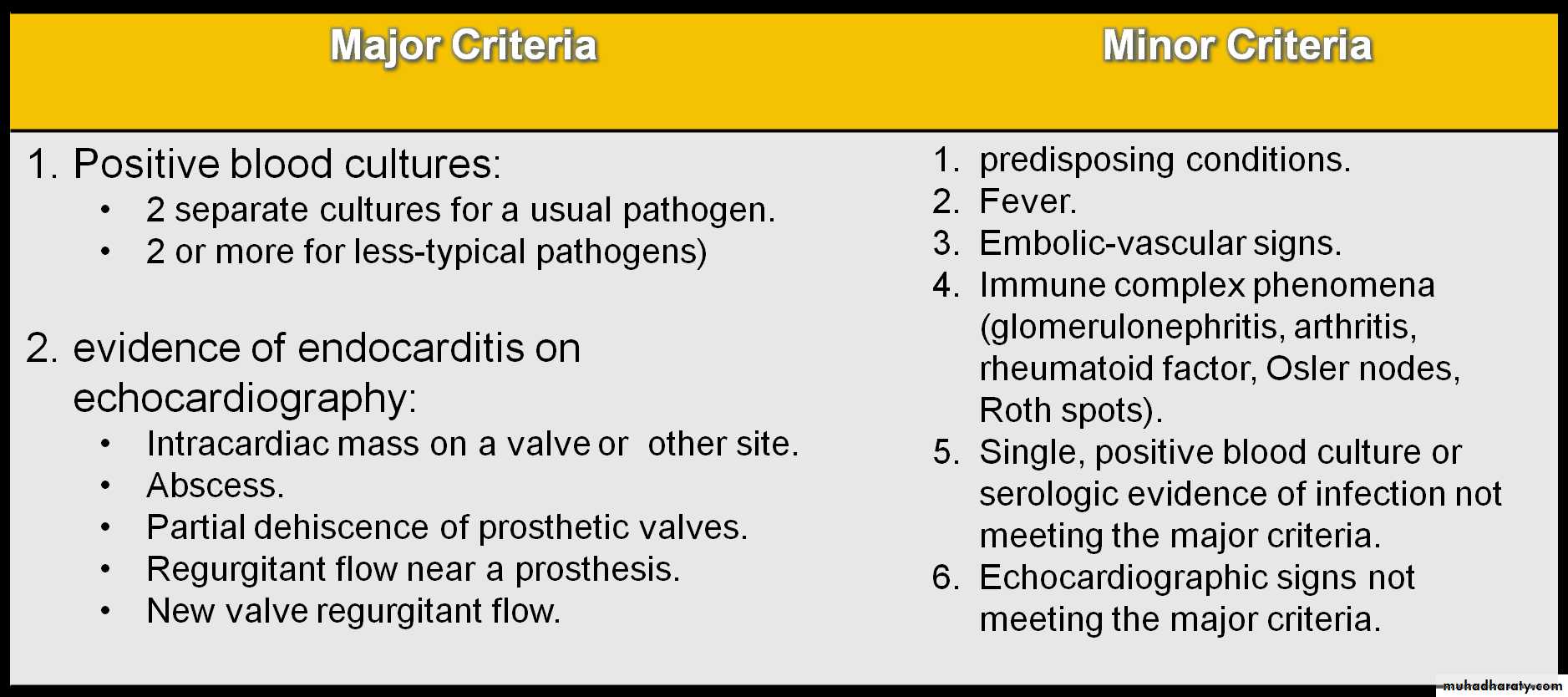
Duke Clinical Criteria for Diagnosis of Infective Endocarditis
Two major criteria or one major and three minor criteria or five minor criteria are needed for diagnosis of infective endocarditisCOMPLICATIONS
Most common: HF from aortic or mitral lesions.
Others:
Systemic or pulmonary emboli.
Myocarditis & myocardial abscess.
Acquired VSD
Valve obstruction secondary to large vegetations.
Heart block as a result of involvement(abscess) of the conduction system.
Meningitis.
Osteomyelitis & arthritis.
renal abscess & immune complex−mediated glomerulonephritisTREATMENT
Severely ill patients must be stabilized with supportive therapies for cardiac failure.
Empirical antibiotic therapy may be started for acutely ill persons after blood cultures are obtained.
High doses of bactericidal antibiotics are required for an extended period of treatment (4 to 8 weeks).
Vancomycin or a β-lactam antibiotic, with or without gentamicin, for a 6-week course is the most common regimen.
CARDIOMYOPATHY
A cardiomyopathy is an intrinsic disease of the heart muscle.There are three types of cardiomyopathy based on anatomic and functional features:
Dilated
Hypertrophic
Restrictive
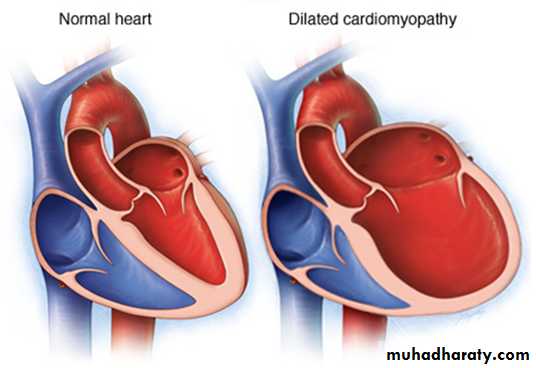
Dilated Cardiomyopathy (DCM)
DCM, the most common form of cardiomyopathy, is characterized predominantly by:
Left ventricular dilation.
Decreased left ventricular systolic function.
Etiology of DCM
Idiopathic: most common.Neuromuscular diseases: as duchenne muscular dystrophies.
Inborn errors of metabolism: as carnitine abnormalities.
Genetic mutations: familial or sporadic DCM.
Genetic syndromes: Alstrom syndrome.
infection: viral (coxsackievirus A and B), bacteria, fungi & parasite.
Endocrine: as hyothyrodism or hyperthyrodism.
Connective tissue disease: as SLE
Metabolic: as thiamine deficiency
Ischemic: most common in adults.
Chronic tachyarrhythmias.
CLINICAL MANIFESTATIONS
Initially nonspecific: (Irritability or lethargy, respiratory symptoms, FTT, abdominal complaints).
Then findings of HF:
Tachycardia, decreased pulse pressure, cool and pale skin, decreased pulses, increased jugular venous pressure, hepatomegaly, edema, rales.
Auscultation may reveal a gallop rhythm in addition to tachycardia and occasionally murmurs of mitral or, less commonly, tricuspid insufficiency may be present.
Investigation:
ECG: atrial or ventricular hypertrophy, nonspecific T-wave abnormalities, and, occasionally, atrial or ventricular arrhythmias.CXR: cardiomegaly and pulmonary congestion.
Echo:
dilatation of left atrium and left ventricle ± right ventricle.
decreased contractility.
decreased flow velocity across aortic valve.
mitral regurgitation.
PROGNOSIS:
Downward progression, ventricular arrhythmias & sudden death.
TREATMENT
The therapeutic approach to patients with DCM includes:
Careful assessment to uncover possible treatable etiologies.
screening of family members.
rigorous pharmacologic therapy.
Decongestive therapy for HF: diuretics, ACEI, digitalis are used. β-Adrenergic blockade with carvedilol or metoprolol is often used in patients with CHF.
Antiarrhythmic therapy.
Systemic anticoagulation
Mechanic ventilatory support, and on occasion, mechanical circulatory support, which may include ventricular assist devices, extracorporeal membrane oxygenation, and ultimately cardiac transplantation.
Trial of PO carnitine: for possibility of mitochondrial disorder)
By ЯĆĔŔ