1
Fifth stage
Gynecology
Lec-5-6
د. آمنة
2/12/2015
Puberty
Its physiological transition from childhood to adolescence, associated with growth spurt & appearance of secondary
sexual characteristics .
-Occur between 8-14 yrs in girls.
-Occur between 9-14 in boys.
Normal puberty
Endocrine control
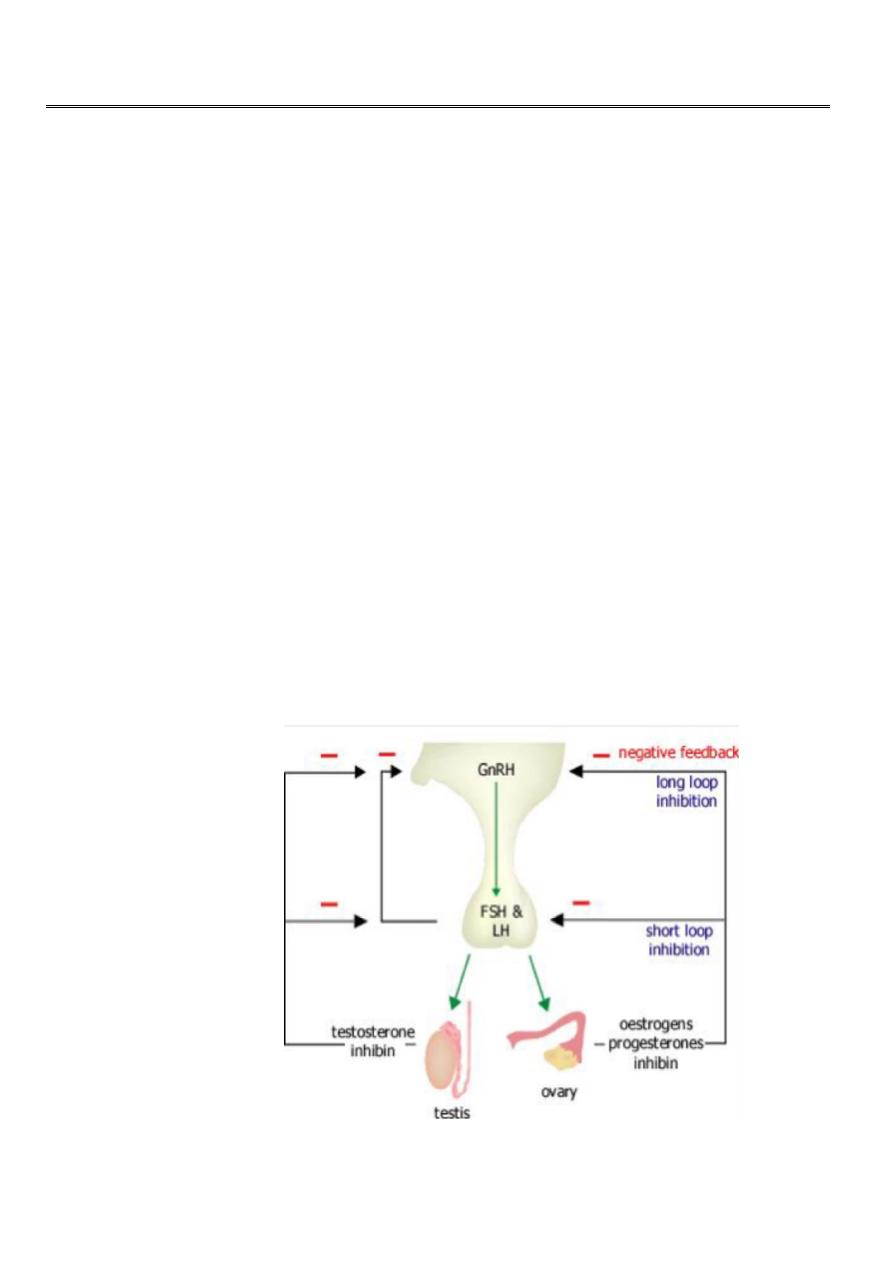
*Onset of puberty signalled by the secretion of pulses of GnRH from hypothalamus.
*Prior to puberty: hormonal feedback/ central neural supression of GnRH release suppress onset of puberty.
*The hypothalamo-pituitary-ovarian axis is functionally complete during the latter half of fetal life. FSH levels are
suppressed from 20 weeks gestation by the production of E. by the placenta & fetus itself.
At birth, the fetus is seperated from placenta then E.decreased. Then FSH level rises & remains elevated for 6-18
months after birth then decrased.
*During childhood, FSH pulses are almost undetectable, and at around the age of 8-9 y, a change occurs in the
function of GnRH cell. The GnRH spikes & subsequent FSH increase during the night time hours over a period of 1-2
y. After a period of 4-5 y, a fully functional production of GnRH with normal adult frequency & pulse lead to
establishment of ovulatory menstrual cycle.
See fig .1

2
Physiology of puberty
*Activation of hypothalamo-pituitary-gonadal axis
*
Induces & enhances progressive ovarian & testicular sex hormone secretion
.
*
Responsible for biological, morphological &psychological changes.
influencing factors
*
genetic factors
*enviromental factors eg. nutritional status.
*leptin.....regulates appetite & metabolism through hypothalamus.
*
psychological factors
*geographic location.
Puberty; Girls
It involve five stages in girls ;
1-growth spurt
2-breast development ( thelarche).
3-pubic hair growth (pubarche)
4-axillary hair growth
5-menstruation (menarche)
Adrenarche -occurs between ages 6-8 ,the result of development of a new zone of adrenal cortix, so the adrenal
cortix secretes increased level of androgens such as DHEA & DHEAS that responsible for appearance of pubic &
axillary hair, body odour & acne.
Growth spurt is characterized by an acceleration in the growth rate around age 9-10y leading to a mean peake
growth velocity around age 12 of about 9 cm/ y. By the age of15 most girls have achieved their final height because
of the production of estrogen from the ovary at this time eventually closes the epiphyses.
thelarche, its the first phenotypic sign of puberty, characterized by appearance of breast bud, usually occuring at the
begining of puberty around age 10 in girls noticed as a firm, tender lump directly under the center of the nipple, may
occur on one side first or both sides simultaneously, the full development take around 5 yrs.
pubarche, the onset of growth of pubic hair, stimulated by androgens released by the ovary & adrenal gland. Its
usually occurs around age of 11 & it is often accompanied by growth of axillary hair.
3
Menarche ( first menstrual cycle ) the average age is between 12 &13 y or 2.5 yrs after the development of breast
buds. The adolescent MC is usually irrigular for the 1st 1-2 yrs after menarche, reflecting anovulatory cycles.
Ovarian development
*rising levels of plasma gonadotrophins........stimulate ovary to produce increasing amounts of estradiol.....secondary
sex characteristics;
......breast growth & development
......reproductive organ growth & development
......fat redistribution
......bone maturation.
*increase ovarian volume to reach 4cm³ post pubertal preparing to ovulation.
Uterine development
*pr-epubertal uterus is tear-drop shaped.
*following production of estrogens, uterus become pear shaped.
*uterine body increases in length & thickness.
*vaginal mucosal surface become thicker & more pink in color in response to increasing level of E.
Body shape, fat distribution & bone age
In response to rising levels of estrogen, the lower half of pelvis &thus hips widen. The bony pelvis acquires female
characteristics.
Bone age correlates well with the onset of secondary sexual charact. & menarche, its determined by X-ray of the left
wrist comparing them with an index population.
Examination
*general examination
*examine in supine position to differentiate between true breast enlargement versus adiposity.
*genital examination; pubic hair, cliteromegaly suggests androgen excess &virilisation.
*mild acne normal in early puberty but rapid onset & progression may suggest androgen excess.
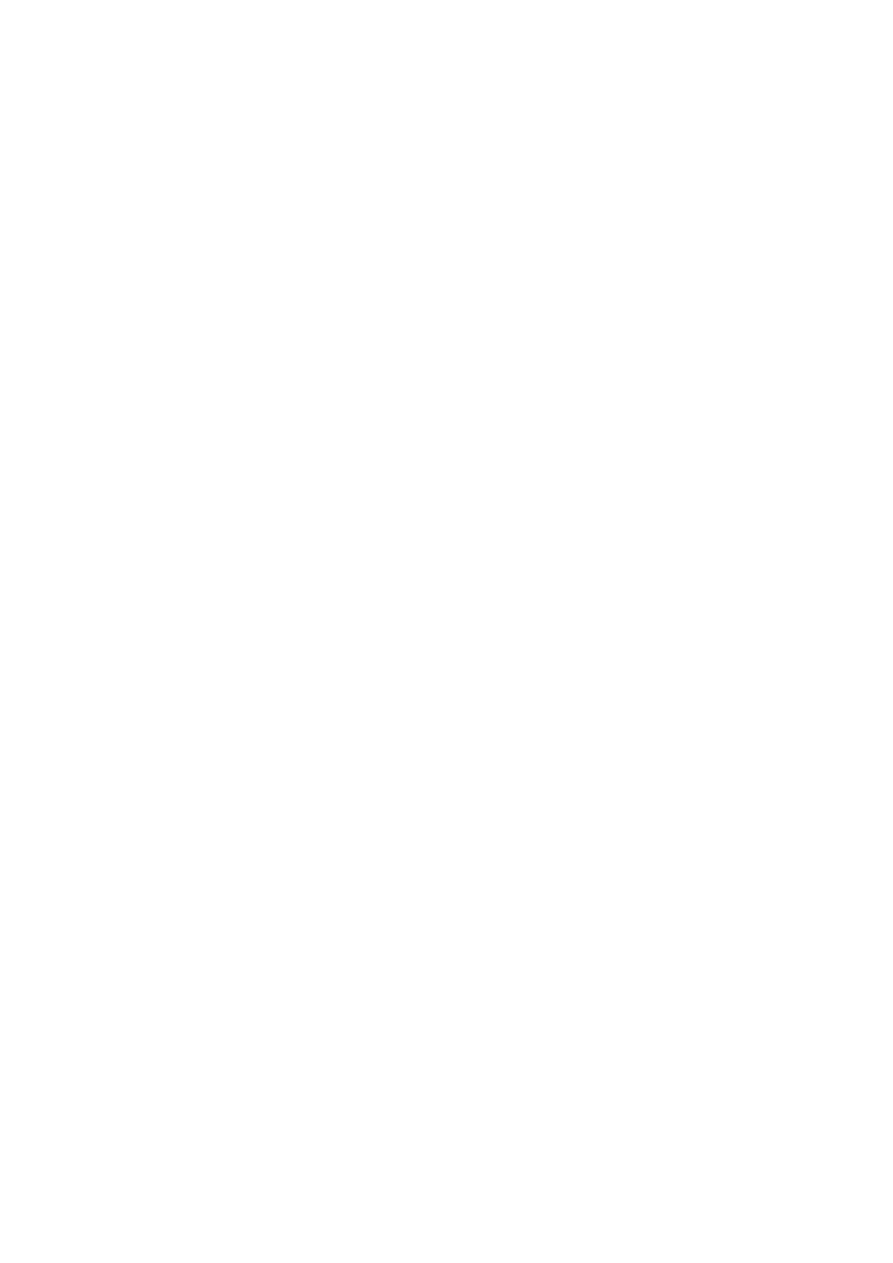
*Pubertal stages (
Tanner
)
P1...prepubertal ( typically age 10 &younger )
P2... early development of subareolar breast bud+/- small amount of pubic & axillary hair.
P3... increase in size of palpable breast tissue & areola, increased dark curled pubic/axillary hair.
P4... breast tissue & areola protrude above breast level. Adult pubic hair but no spread to medial thights.
P5... mature adult breast. Pubic hair extends to upper thigh. See fig.2
4
Fig.2 Tanner staging, female
Puberty
:
boys
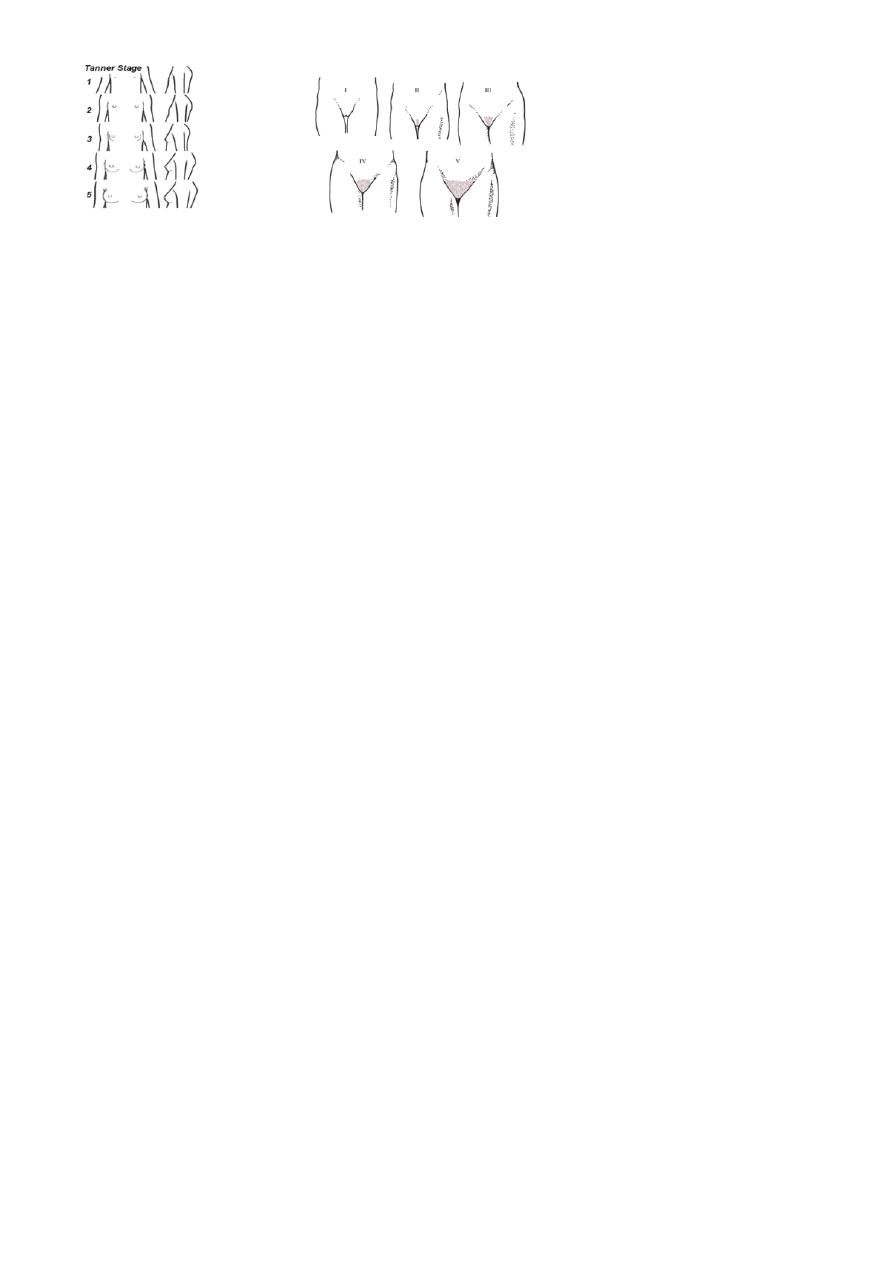
*testicular enlargement (12-13yrs) is first sign. Prepubertal testis-2ml diameter, puberty begins when volume
reaches 4ml.
*penile growth & scrotal changes , pubic hair occur approx 1-2 yrs after testicular enlargement.
*late signs, growth spurt, acne,voice deepening, facial hair, pubert growth spurt occur later than in female.
Examination
*general examination.
*abdominal examination
*genital examination
......testicular growth associated with enlargement of seminiferous tubules, epididymus, seminal vesicles & prostate.
......prader orchidometer for assessment of testicular volume. See fig.3, 4
......growth spurt,voice deepening, facial hair.
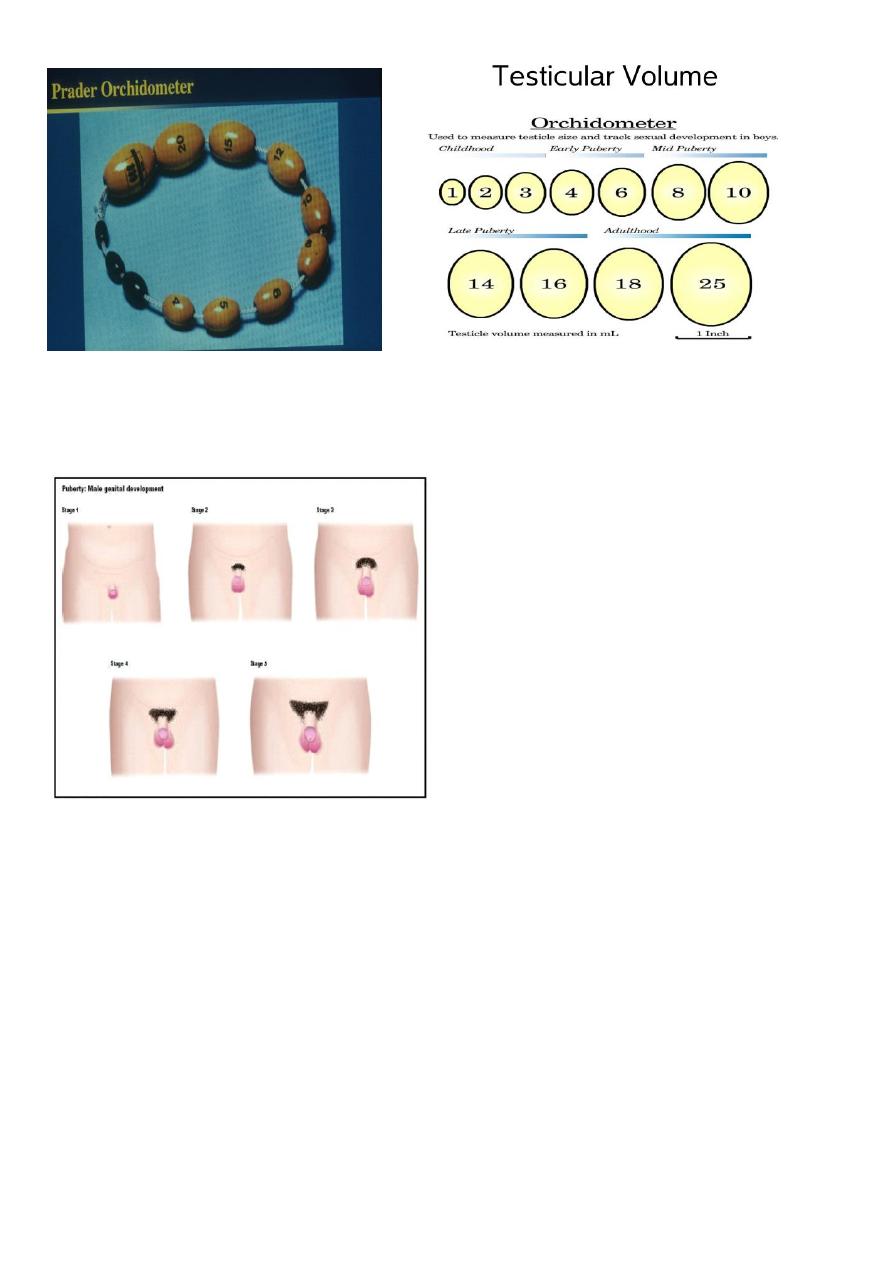
*Pubertal stages (
Tanner
)
P 1...prepubertal (testicular volume < 2 ml, small penis) typically age 9 & younger.
P 2...enlargement of scrotum & penis, few long dark pubic hair.
P 3...lengthening of penis. Further growth of testes & scrotum. Pubic hair darker, coarser & more curled.
P 4...penis increases in length & thickness. Increased pigmentation of scrotum. Adult pubic hair but no spread to
medial thighs.
P 5...genitalia adult in size & shape. Pubic hair spread to medial aspect of thighs.
See fig.5
5
Fig.3 prader orchidometer Fig.4 testicular volume
Fig.5
Tanner staging, male
Precocious puberty
Refers to the development of secondary sexual characteristics <8yrs in girls & <9yrs in boys.
5 times more common in girls. Its usually due to early onset of normal puberty (80%) but in boys, its usually due to
intracranial tumour (40%).
In girl, pregnancy can reported as early as 5.5 yrs !
In boy, testicular biobsies has shown stimulation of all elements of testis & spermatogenesis as early as 5-6 yrs.
Causes may be;
1-Gonadotrophin dependant
-idiolathic (constitutional) in 95%.
-congenital (hydrocephalus).
-acquired (irradiation/ surgery, sever head trauma)

6
-tumours (gliomas).
-hypothyroidism (TSH act on FSH receptors).
-Mc Cune Albright Syndrome (patchy cutaneous pigmentation &fibrous dysplasia of skeletal system).
2-Gonadotrophin independant
-virilisation of female (CAH).
-feminisation of boy (estrogen producing leydig tumour).
-adrenal tumour.
-ovarian tumour.
-exogenous androgens, estrogen.
-HCG-secreting tumour (teratoma).
Treatment
*-Psychological support.
*-GnRH agonists are useful , most commonly used preparation is leuprolide acetate in a dose of 0.25-0.3 mg/kg I.M.
once every 4 wk. Other preparation goserelin acetate (Zoladex).its effective at suppressing the secondary sexual
characteristics of puberty &the first few yrs of use are to improve height prognosis.
In gonadotrophin independent ,in girl, aromatase inhibitors as letrozole (1.25-2.5 mg/d orally) or antiestrogen as
tamoxifen. In boy, combination of antiandrogens ( such as spironolactone 50-100 mg twice daily or flutamide 125-
250 mg twice daily)
*-treat systemic disease
*-surgery to remove tumour.
Delayed puberty
Puberty delay if
*no breast development by age 13 in female
*no menses by age of 15
*testicular size <2.5 cm or 4 ml or pubic hair is not present by age of 14 in male.
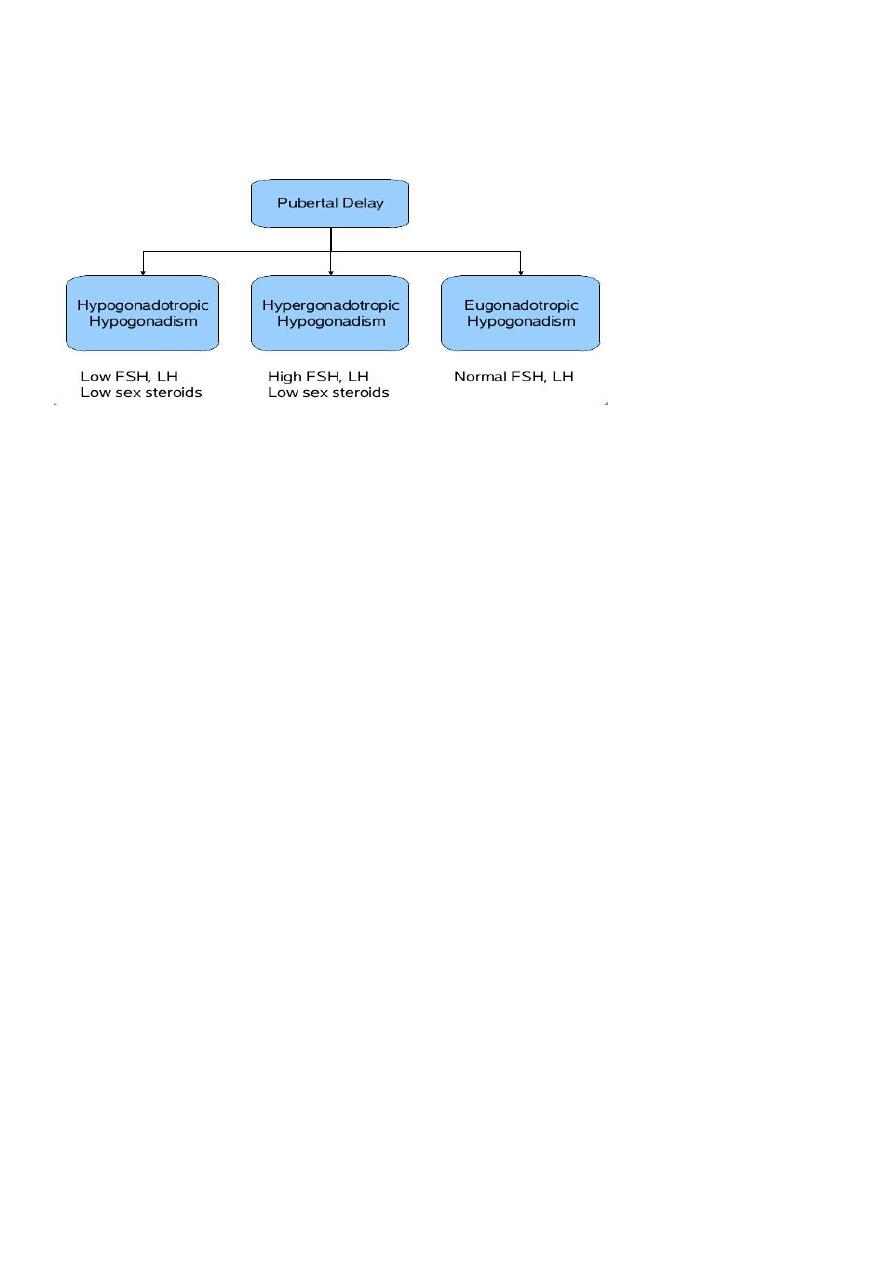
Causes may be;
1-Hypogonadotrophic
-idiopathic (familial/ sporadic)
-chronic illness (renal failure/ Crohns dis).
-malnutrition.
-exercise.
.-tumour of pitutary/ hypothalamus (craniopharyngioma).

7
-hypothyroidism (interferes with gonadotrophin secretion)
-hyperprolactinemia, PCOS.
-isolated GnRH deficiency........(Kallman's Syndrome)
2-Hypergonadotrophic
-congenital (Turner syndrome/ klinefelters syndrome, complete androgen insensitivity, mixed gonadal
dysgenesis)
-acquired......irradiation/ chemotherapy.
......................surgery
......................testicular torsion, trauma
......................infection (mumps orchitis).
......................autoimmunity.
3-Eugonadotrophic
-congenital anatomic anomalies
...........imperforate hymen
...........vaginal atresia
...........vaginal aplasia
In these cases,, secondary sexual characteristics are normal.
See Fig.6.
Treatment
*Psychological support.
*Treat systemic disease
*Promote puberty/ growth if necessary.
in male case.
.... testosterone,it cause virilization, accelerates development of secondary sexual characteristics & stimulate growth
spurt).
Its either oral form, testosterone undecanoate 40mg daily or I.M.injection 50-200mg using testosterone esters have
been used for a period of 6-12 months or use transdermal patches.
.....hCG 200-500 Units, can use to stimulate development of secondary sexual characteristics, increase testicular size
& to stimulate fertility.
In female case
......estrogen replacement, initial replacement at age of 10-12 yrs &should continue over coure of normal puberty
(approx 3 yrs). Effect of estrogen on growth plate is dose dependent, higher dose stimulate epiphyseal growth plate
8
closure, to start with 2mcg/day ethinylestradiol. Once adose of 10-15 mcg ethinylestradiol have been reached, a
break through bleeding becomes apparent & when this occur, progesterone should be added to prevent
endometrial hyperplasia.
*in some cases of hypogonadotrophic, pulsatile administration of GnRH has resulted in induction of puberty.
Fig.6 causes of puberty delay
Assessment of puberty
History
**Parents
Important to ask about onset of puberty in parents
.....menarche (more reliable in mothers as they remember onset).
.....male growth spurt.
Parents heights
** body changes
Thelarche (galactorrhea)
Pubarche/ adrenarche (pubic & axillary hair, body odour & acne).
Menarche
**past medical history ( history of brain tumour, radiation, chemotherapy, known genetic disorder)
**activity level, is exercise excessive or is this an athlete with a high level of training.
**nutritional habits
**growth history, previous growth chart can be extremely helpful
**review of systems
.....CNS, visual changes, visual field abnormalities,headache, anosmia.
.....Cardiac,congenital anomaly.
.....Respiratory, asthma
.....Renal

9
.....GIT, diarrhea
**medication, history of drug intake.
Physical examination
1-Examination of growth
.....height
.....weight
.....BMI
.....upper to lower segment ratios
2-Pubertal assessment ( Tanner staging )
.....axillary hair
.....pubic hair & staging
.....genital development & staging
.....breast development & staging
3-Neurological assessment
4-fundoscopy & visual field evaluation
5-abdominal exam.
.....mass
Investigations
*lab studies
.....FBC, LFT, Urea & electrolyte
.....Hormone levels (FSH, LH, TSH, T4, estrogen, testosterone, prolactin, DHEAS ,17 OHP, adrenal androgen & HCG
level).
*karyotype if indicated.
*diagnostic imaging
.....Pelvic US (ovarian tumour)
.....Testicular US (tumour).
.....Adrenal US
*Bone age radiography
*Brain MRI in all males & patients with neurological signs or symptoms.
Treatment
According to the case.
11
Vaginal bleeding in infancy
Female infant may have vaginal bleeding during the 1st wk of life. Mainly due to withdrawal of maternally derived
estrogen which had crossed the placenta in pregnancy.
Causes of vaginal bledding in children;
-Foreign body
-Trauma
-Genital tumour
-Vulvovaginitis
-Precocious puberty
-Exogenous hormone usage
-Condyloma acuminata
Normal menstrual cycle
The endocrine control of ovarian function
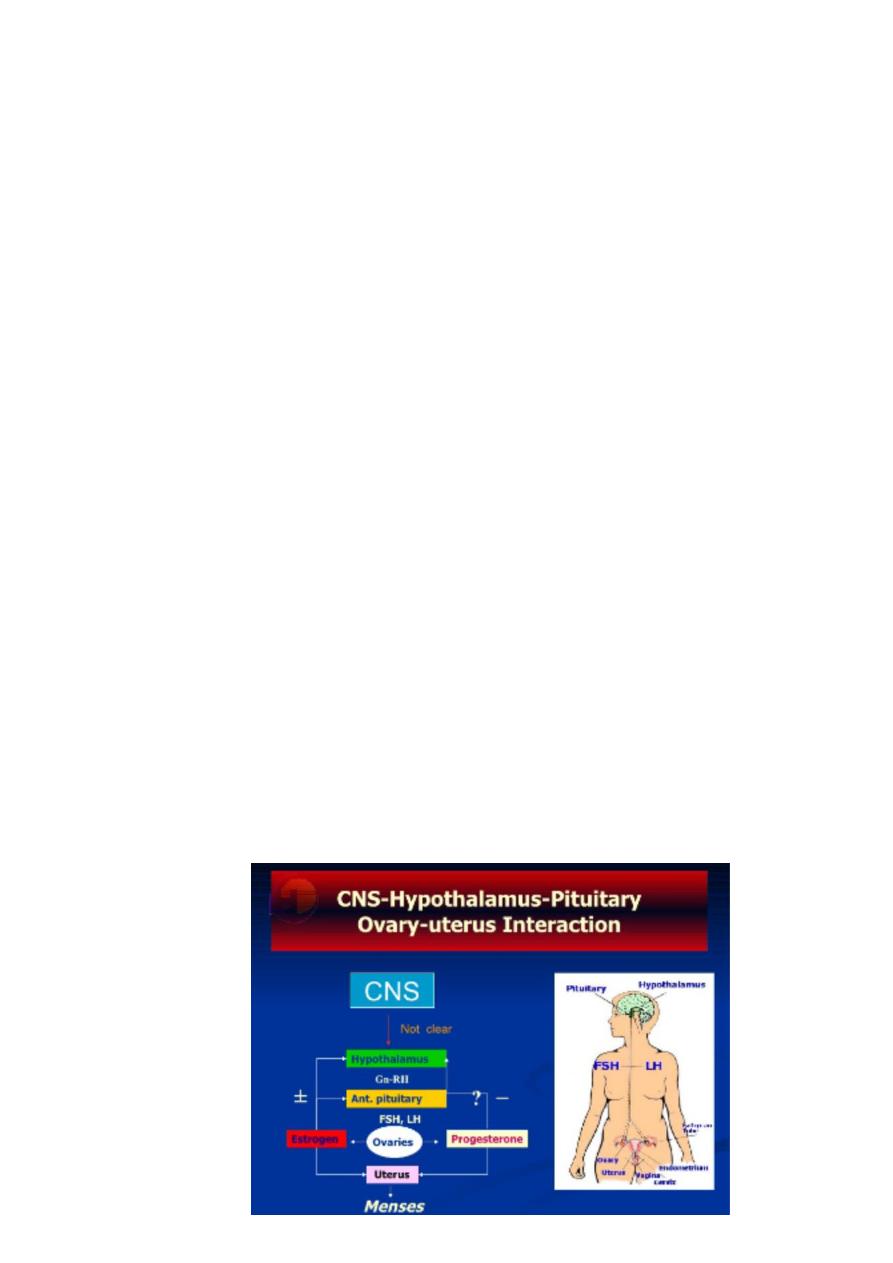
Each menstrual cycle (MC) represent a complex interaction between hypothalamus, pitutary, ovaries & uterus.
The hypothalamus central nervous system discharges GnRH which is transport to anterior pitutary gland, where it
stimulates the gonadotrophs which secrete the gonadotropins; FSH & LH.These hormones stimulate the gonads to
synthesize & secrete sex steroid.
Hormone release in the (HPO) axis is regulated by a negative feedback on gonadotrophs in the anterior pitutary& by
indirect inhibition at the level of hypothalamus. Stimulation & negative inhibition complete the pathway between
hypothalamus, pitutary & ovaries. See
Fig.1
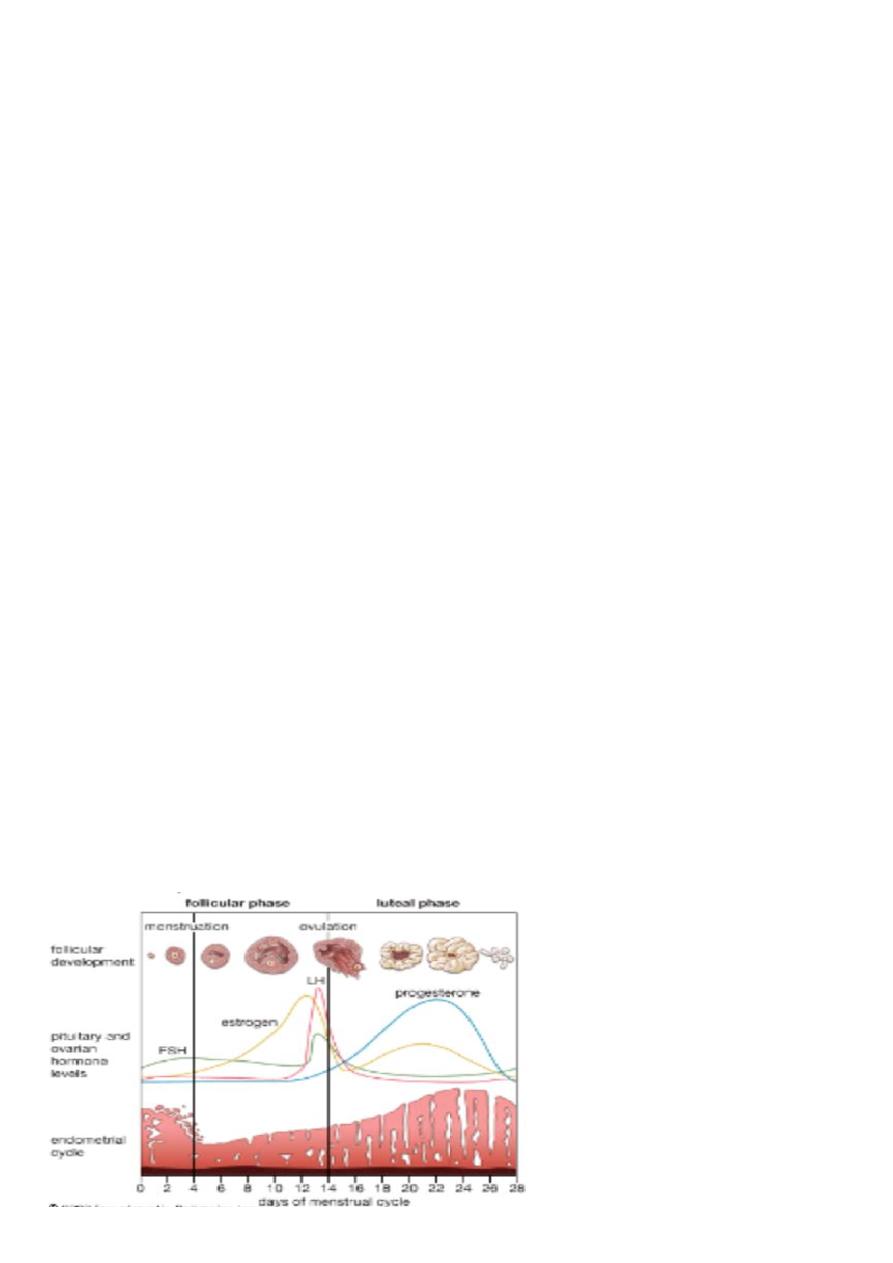
MC divided into two phases, the follicular & luteal phases, which describe changes in the ovary over the length of the
cycle, & the proliferative & secretory phases, which describe concurrent changes in the endometrium over the same
period of time.
Fig.1 HPO-U interaction
11
Follicular phase
The development of oocytes is the key event in this phase.
FSH stimulates the growth of approx 5-15 primordial ovarian follicles,
The most advanced follicle at mid-follicular phase becomes the dominant follicle
LH stimulates theca cells to produce androgens which are converted to estrogen.
FSH stimulates granulosa cells to produce estrogen (E.) which causes endometrial thickening &thining of cervical
mucous to allow easier passage of sperm.
FSH production inhibited by rising E.& inhibin.
Declining FSH causes atresia of all follicles but not the dominant follicle as its protected from the decrease in FSH by
its increased number of FSH receptors.
Ovulation
Toward the end of follicular phase, estrogen levels surge to reach a critical level that triggers anterior pitutary to
release LH spike. The LH surge induces production of progesterone &prostaglandins within the follicle . The
progestrone & prostaglandins in turn are responsible for the rupture of follicular wall with release of a mature ovum
or ovulation within 24–48 hr of LH surge. The ovum passes into adjoining fallopian tube &swept down to uterus. This
process take 3-4 days. Fertilization of ovum must occur within 24 hr of ovulation or it degenerates.
Luteal phase
After ovulation, the granulosa &theca interna cells lining the wall of follicle form corpus luteum under stimulation by
LH. Corpus luteum synthesizes estrogen & progesteron which cause the endometrium to become more glandular &
secretory in preparation for implantation of fertilized ovum.
If fertilization occurs, the developing trophoblast synthesizes HCG (a glycoprotein very similar to LH) which maintains
corpus luteum , so it can continue production of E. & P.to support endometrium. This continues until the placenta
develops its own synthetic function at 8-10 wks gestation.
If fertilization does not occur, the corpus luteum degenerates, P.level fall, the endometrium is not maintained, &
menstruation occur.
See fig.2
Fig.2 Ovarian cycle

12
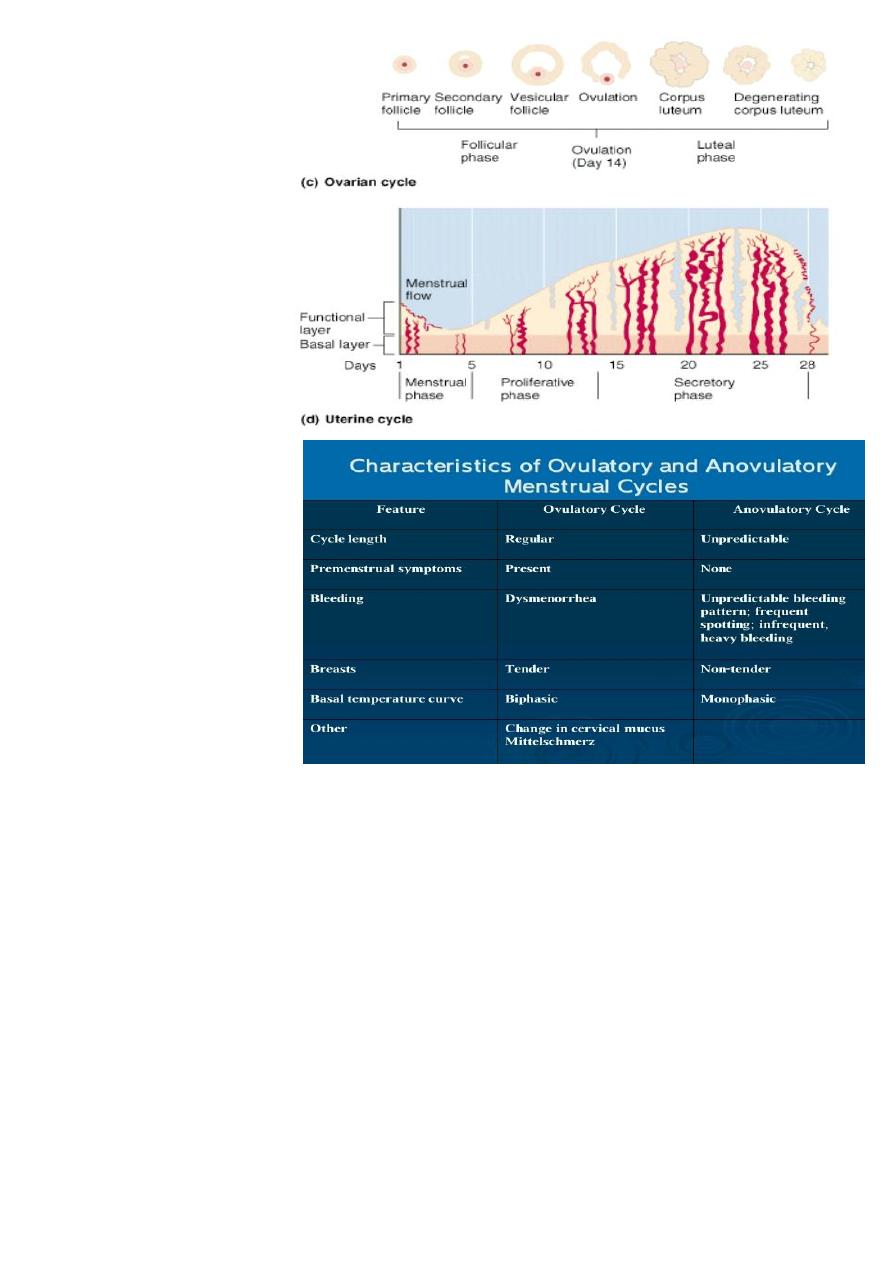
Menstruation
The endometrium of the uterus under go cyclical changes during MC.
During follicular phase, the endometrium is in the
proliferative phase,
growing in response to E.increasing the
endometrial thickness from 0.5-5 mm.
During Luteal phase, the endometrium enters the
secretory phase
that characterized by progestrone-induced
glandular secretory activity & endometrium become more thick &prepared to support implantation if fertilization
occur. If ovum is not fertilized, the corpus luteum degenerates after 14 days leading to a fall in E.& progesterone
levels. The withdrawal of progesterone causes the endometrium to slough , initiating the
menstrual phase
.
Asequence of intense spiral artery vasoconstriction &relaxation is generated. These events lead to ischemia & tissue
damage, shedding of functional layer of endonetrium & bleeding from fragments of arteries in the basal layer.
Haemostasis is then secured by spirl artery vasoconstriction &by the action of fibrinolytic system which inhibits scar
tissue formation & repair of endometrium with new vesseles formation lead to complete sessation of bleeding
within 5-7 days from the start of MC. See Fig.3
At the same time, FSH levels begin to slowly rise in the absence of negative feedback & the follicular phase start
again.
The secretory endometrium has 2 distinct zones;
Basal layer
Functional layer
Women may experience
Fluid retention, cramping, mood swing, wt.gain, breast tenderness, diarrhea & constipation.
Clinical features of normal menstrual cycle
*Menarche (first menstruation); average age between 12-13 yrs
*Cycle duration; 28 days +- 7 ds (from the start of one menses to the start of the next).
*Duration of flow; 2-8 days, its usually scanty viscoid at first then become bright red finally brown toward the end of
cycle, it contain no clot as the endometrium releases fibrinolytic substances (plasmin) which dessolve blood clot
formed in uterine cavity.
*Peak flow; 1st or 2nd ds.
*Normal menstrual loss; mean 30-35 ml/cycle (max. 80 ml). >80ml considered excessive loss(menorrhagia).
*Dysmenorrhoea, is a painful uterine contraction occur in some women.
Note
....The length of MC is determined by the length of the follicular phase.
Content of menstrual flow
*Partially haemolysied blood (red cell, degenerated platelet, fibrin, large amount of fibrin degeneration products).
*Fragments of endometrial tissue & cellular debris.
*Mucus
13
Fig.3 endometrial cycle
Characteristics of ovulatory &
anovulatory cycles.
Key terms and definitions
Menarche; first menstrual cycle.
Primary amenorrhea; absence of menstruation with or without signs of puberty.
Secondary amenorrhea; absence of menstruation for 6 months or more in a woman of reproductive age & not due
to pregnancy.
Dysfunctional uterine bleeding; irrigular bleeding unrelated to anatomical causes
Oligomenorrhea; menstrual interval greater than 35 days.
Menorrhagia; regular menstrual intervals, excessive flow & duration.
Anovulation; menstrual cycle without ovulation.
Mittleschmertz; pain with ovulation.
Molimina; symptoms preceding menses.
Dysmenorrhea; menstrual cramping/ pain.
