-
1
-
Session
)
Neurology
(
MEDICINE
-
:
History taking
##
-
:
usually pt comes complaining of
-
sensory symptoms :
-
1
-ve one :- loss of sensation
+ve one:- paraesthesia
-
motor symptoms:
-
2
*Paraesis
*Paralysis
*Plegia
Involuntary movement
+ve symptom.
What lesion?
Where is the lesion?
3-weakness :- the pattern of weakness
*Hemiplegia indicates contralateral brain lesion.
*Monoplegia indicates peripheral neuropathy,brachial plexus injury.
*Tetraplegiaif the lesion in cervical area of spinal cord(above T1)
4-disturbed level of consciousness.
5-headache.(mostly along nerve course).
6-visual disturbance
7-speech disturbance
8-sphinecteric dysfunction
9-personality changes(unless purely psychiatric disease ).
10-vertigo.
- ve symptoms
## for every symptom,u should know the
# onset of it ,i:e
Insidious since 2days , I begin to feel weakness in my right leg.
Subacute MS :-over months or wks symptoms develops.
# Course of the disease:- "progression"
if progressively worsening SOL
attack epilepsy,TIA
remitting with relapsing MS.
Family History:-
very important to ask patient about: has migraine ,her sister , mother may have the same.
Parkison disease (10%)is familial.
Drug history : valium taking with appearance of its side effects.
#Cranial nerve examination:-
--They provide motor and sensory innervation for the head and neck.
--damage of motor neurons results in cranial nerve palsy (central or peripheral?).
--For every nerve u should be aware of :
1-name of nerve.
2-is it sensory or motor?
3-has autonomic fibers or NOT?
4-its nucleus in which part of brain?
5-how to examine this nerve?
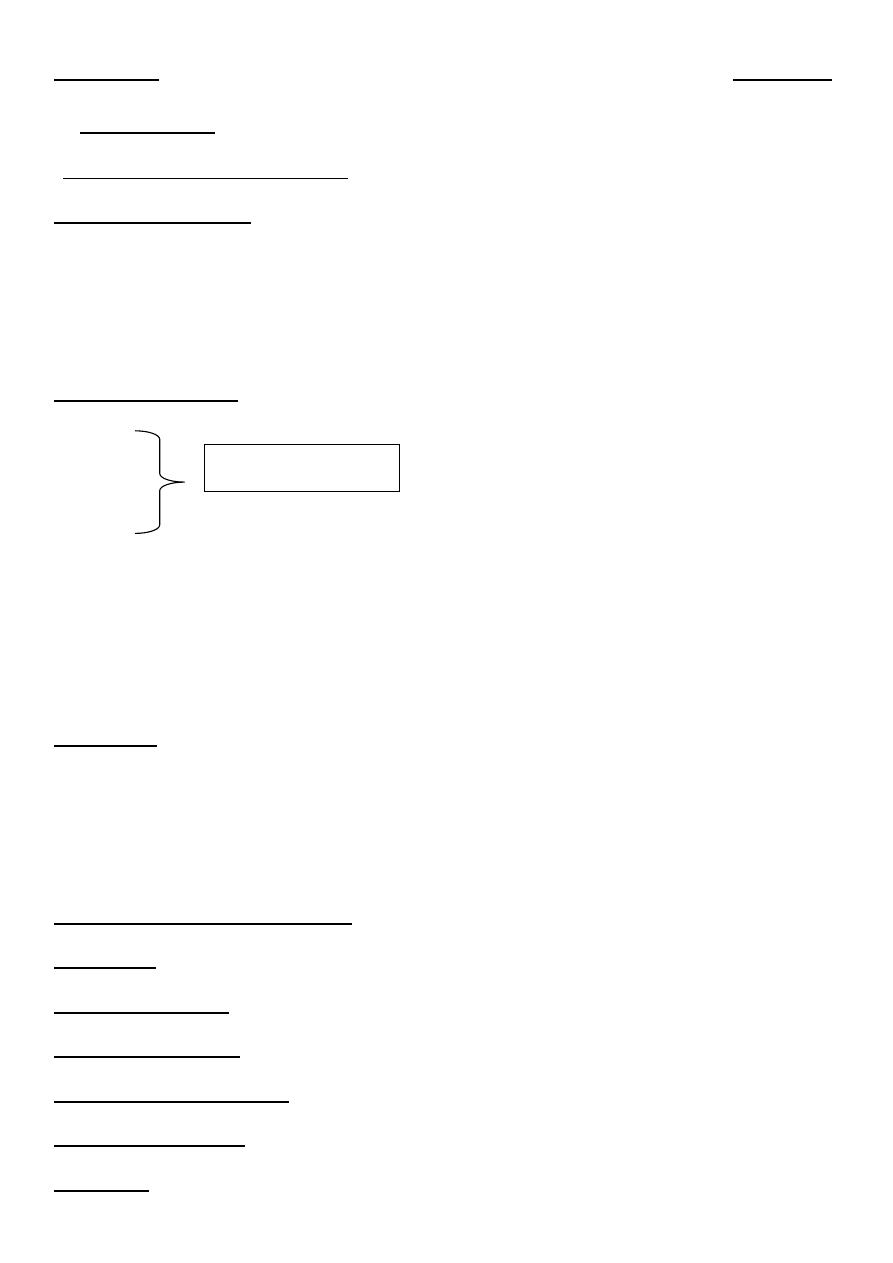
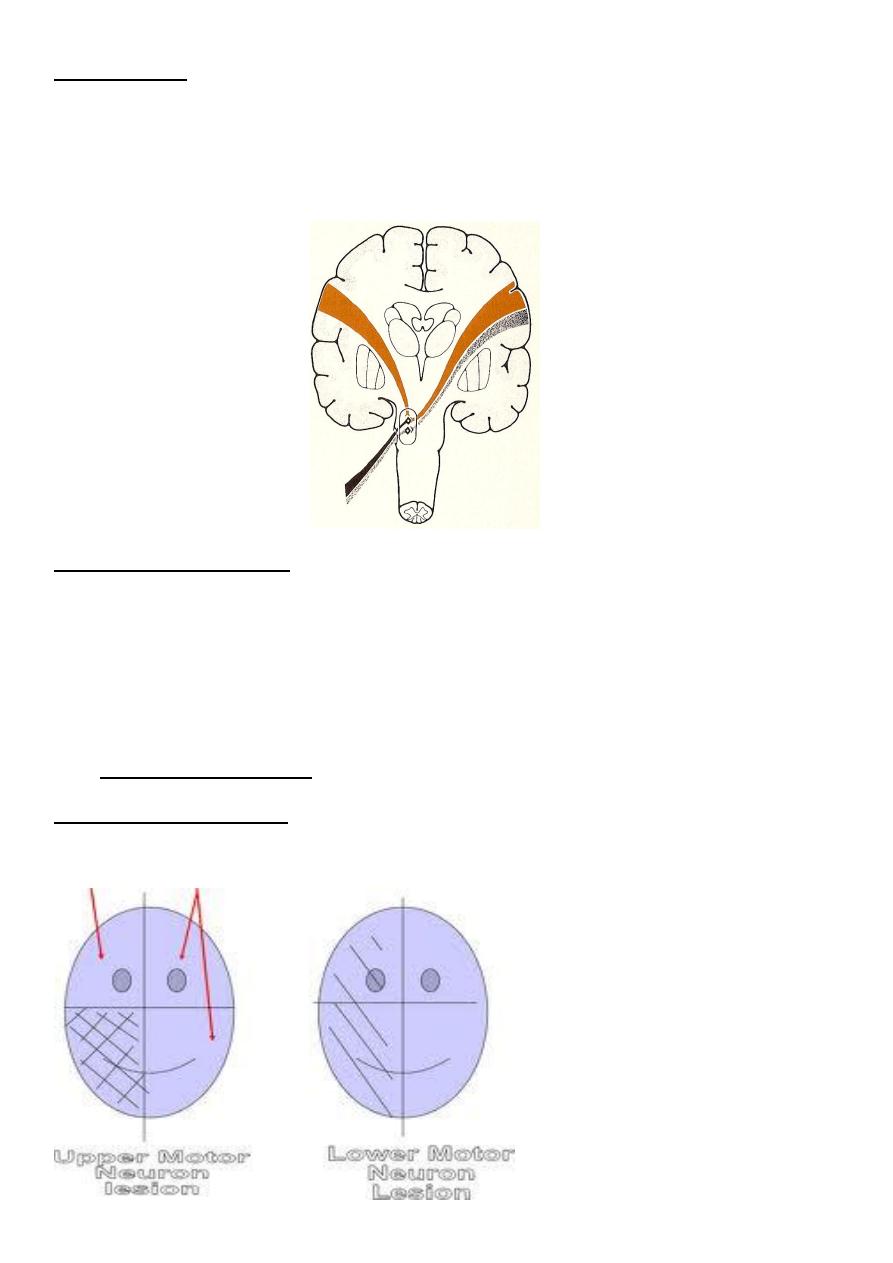
--The upper motor neuron – lesion results in an upper motor neuron weakness, central
palsy . ( in: cortex, internal capsule, or brain stem above the nucleus )
--The lower motor neuron :- lesion results in an lower motor neuron weaknesss, peripheral
p. ( in: the nucleus in the brain stem (the cell bodies form nuclei) or in any lower part of the
cranial nerve.)
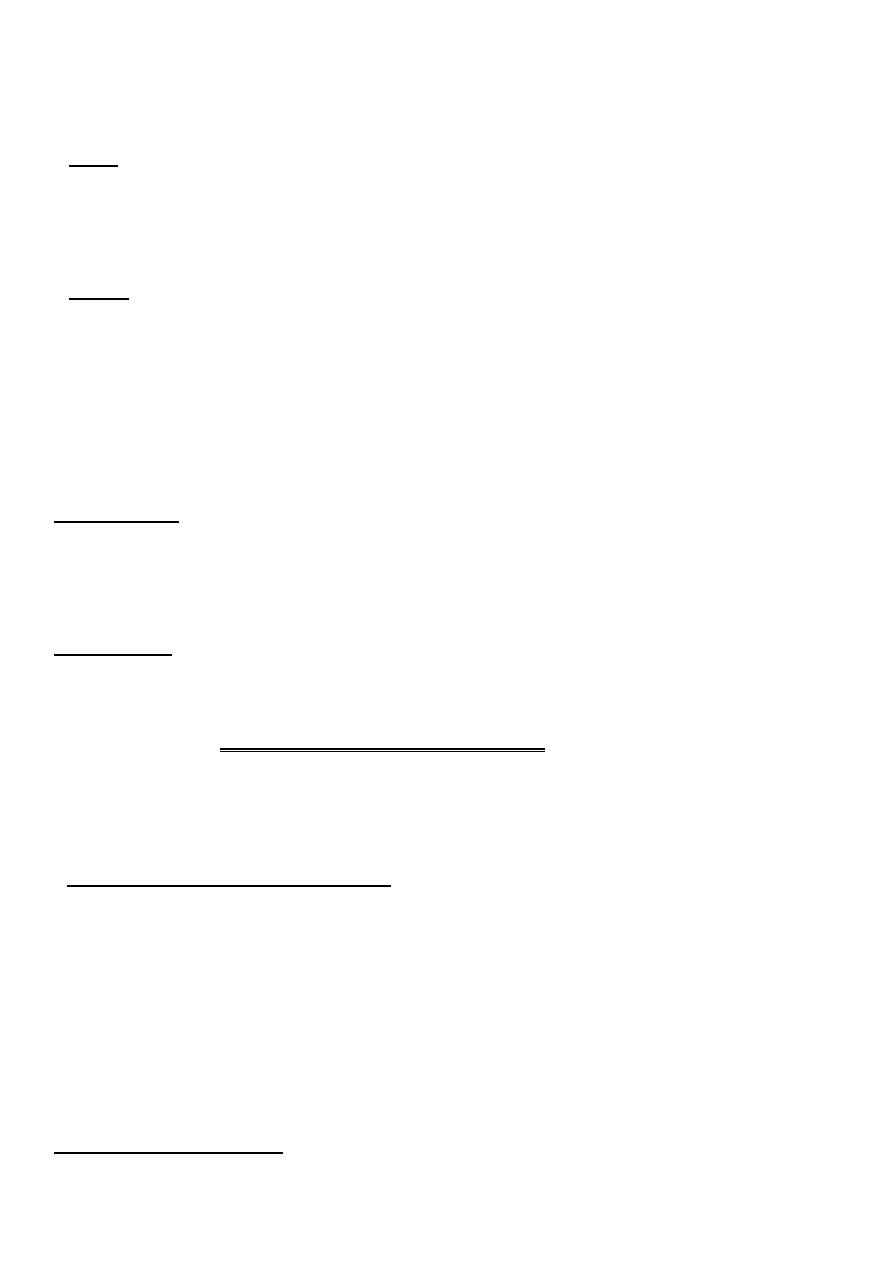
1. olfactory nerve:-
Function :- olfaction
Purely sensory
Exam:-from macloed.
*The subastance you should use in the exam must be:-
1-popular
2-not irritating
And there is no local disease (flu)
**this nerve commonly affected in fracture of anterior cranial fossa (as there will be
fracture of cribriform plate).
**hyposmia/anosmia: bilateral and transient – rhinitis
**temporal lobe epilepsy :-olfactory hallucination(he/she smells unpleasant odors)
2. optic nerve:-
Function :- vision
Commonly affected if there is trauma to frontal , temporal , occipital lobes.
Each eye should be examined alone in optic nerve.
a- visual acuity : by snellen chart, if not present any thing in the room ,,if not
ask the
patient to count the fingers in your hands ,if not:move your hand
can he
appreciate your hand movement,if not
light perception:-if not
patient is blind.
b- visual field :-by perimetry (NOT present)-
confrontation method.
The visual field normally is NOT circular ,it is cut by the presence of nose(laterally),by the
frontal bones(above).
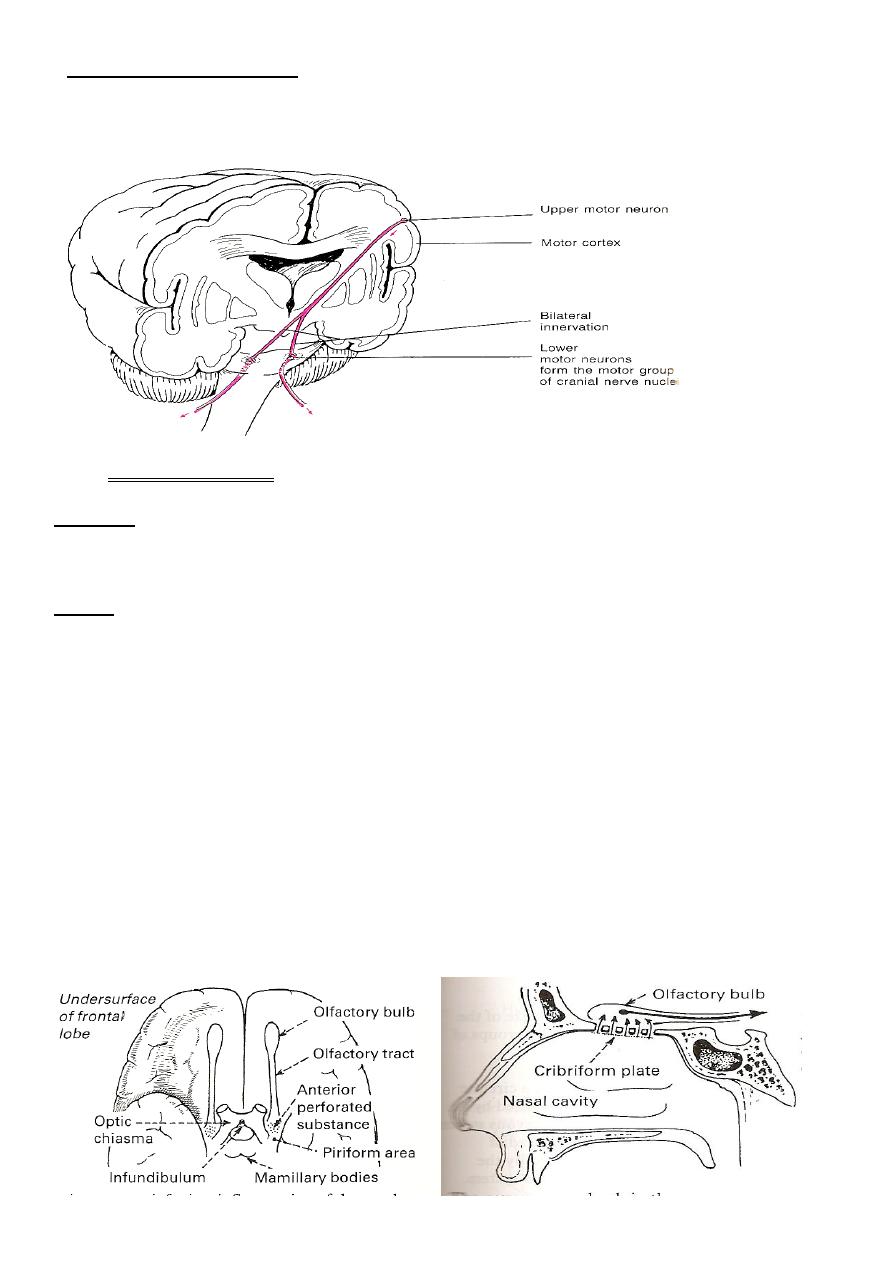
# Defects in visual fields:-
a- Homonymous:-the nasal field is affected in the right,while the temporal field is
affected in the left.
b- heteronymous:-temporal fields are affected (in rt side & lt side) or both nasal fields
are affected.
* bitemporal hemianopia commonly results from pituitary tumours (most common &
typical visual field defect).
• damage anterior to the chiasma:
– scotoma
– monocular blindness
lesion at the chiasma:
– heteronymous hemianopsia
• damage posterior to the chiasma:
– homonymous hemianopsia
• lesion in the optic radiation:
– quadrantanopsia
• lesion to the visual cortex:
– one side – homonymous hemianopsia
– bilateral – cortical blindness
----------------------------
c- color vision
d- fundoscopy: examine the lt eye from the lt side in your lt eye.
e- reflexes. afferent & efferent.
3. (
3
rd
,4
th
,6
th
)cranial nerves
should be examined all together in both eyes.
*Scotoma:- loss of vision in a point surrounded by normal visual field.
*In the confrontation exam :-the distance between the dr. and the pt. should not be more
than 70cm & At the same level of pt. (because visual field is NOT circular normally).
--Impaired occular muscles movement from Lesions of the cranial nerves (peripheral
palsy):
• III (oculomotor)
• IV (trochlear)
• VI (abducens)
– with paralytic strabismus
– with double vision (diplopia)
Occulomotor nerve palsy:-
• ptosis (levator palpebrae m.)
• divergent strabismus (the affected eye deviates laterally)
• paralysis of the eye movements and accommodation
• pupil dilatation (mydriasis),
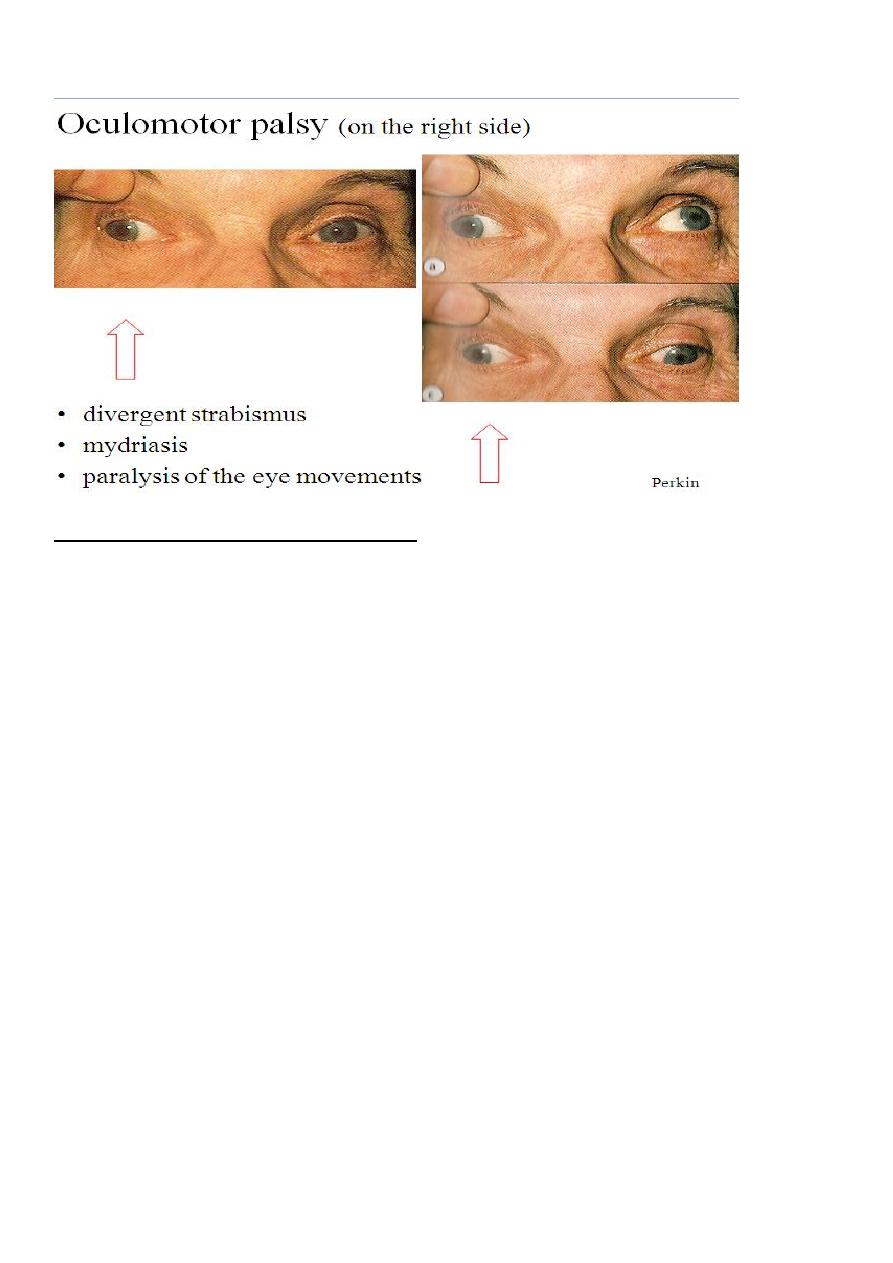
• reaction to light is absent
III, IV, VI cranial nerve examination:-
• palpebral fissures (symmetrical? ptosis?)
• position of the bulbs (parallel? strabismus convergent or divergent?)
• ocular movements (full range? limitations?)
• nystagmus (direction? degree?)
pupils
– shape, size in mm (dilated – mydriasis,constricted – miosis)
– reaction to light (light reflex):
– direct and consensual
– near reaction to accommodation and convergence
Trochlear palsy(4thCN)palsy:-
• weakness of downward gaze
• double vision when looking downwards
• the head may tilt to the opposite side to minimise the diplopia
• diplopia is vertical
Right fourth nerve palsy, the paretic eye turns up- and outwards; head tilting
Abducent nerve
• convergent strabismus
• failure of abduction on the affected eye
(on looking to the paralysed side)
• horizontal diplopia
Left sixth nerve palsy (looking to the left)
.
Tone :-resting muscle contraction.
**Before any eye exam perform
:-
#
inspection
for
1- squint: occurs when there is unopposed tone.
2- ptosis
3- pupil: has radial(dilate the pupil) & circular (constrict the pupil)muscle fibers
4- proptosis: mostly non neurologic cause.
5- nystagmus:-oscillatory movement of the eye.
**Then after u complete inspection:-
#put the muscle in action
.
Note :-when the patient follow your hand in (H)pattern he use the (oblique)group of
muscles in the eyes,as the eyes are adducted.
Always u should ask the pt "tell me when you see the moving object appears as two
objects for you)?
Try always to fix the pt's head with your hand (only the eyes should move).
**when to examine eye reflexes?
1- if you are aked to examine the 7
th
CN
examine the corneal reflex also.
2- optic nerve exam .
3- occulomotor nerve exam
4- neurological exam
5- sensory examination.
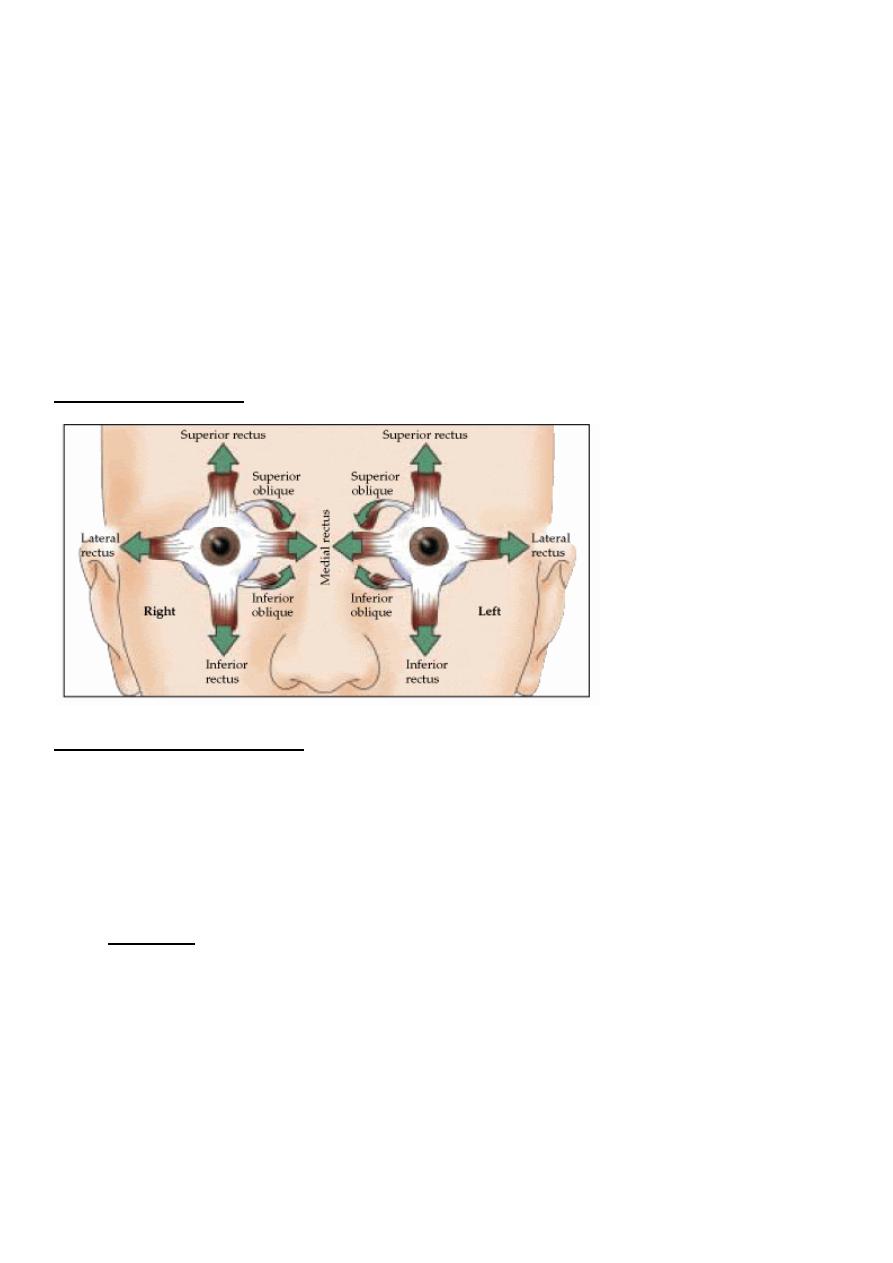
*muscles of the eye :-
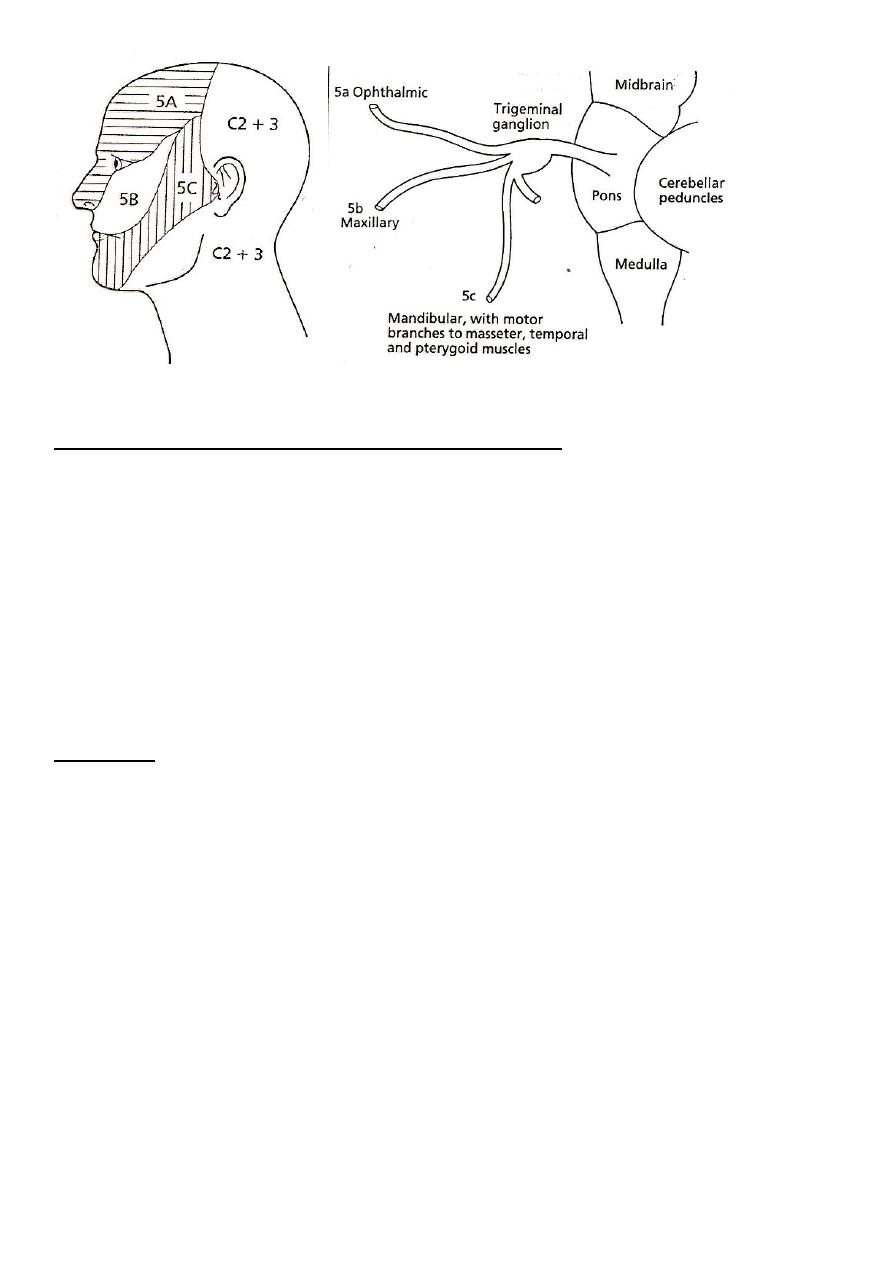
Trigeminal nerve(5thCN)
– sensory fibres for facial sensation (3 divisions) :-
ophthalmic,maxillary&mandibular
– motor fibres (in the mandibular division) innervate the muscles of mastication
(masseter, pterygoids and temporalis)
• disorders:
– sensory loss
– muscle weakness, atrophy (in peripheral palsy)
– neuralgia
Mandibular branch is Motor to the muscles of mastication
1- pterygoid:-pulls the mandible forward in opening of the mouth(in the midline of the
face)
2- temporalis:-elevate the mandible & retract it.
To examine this muscleput your hand on the muscle , then ask the patient to clench his
teeth.
3- masseter:-raises the mandible to occlude the teeth in mastication.
*this muscle is located at the angle of jaw.
On exam
:-
sensation (each division separately) for
– pain
– temperature
– light touch
corneal reflex – blink response (trigemino-facial response .) – symmetrical?
Note :- Corneal reflex:- cornea is transparent ,has no specific color ,it covers the colored
part of iris.
Afferent: 7
th
cn
Efferent: 5
th
cn
masseter reflex (jaw jerk)
Facial nerve:-
*commonly involved in problems.
*all cranial nerve nuclei receives from two sides except the facial nerve which receive in its
upper part only from two but in its lower half receive only from one side .
upper motor neuron lesion → central paralysis:
the upper branch is less affected(because the rostral part of the nucleus is innervated
bilaterally)
paralysis is marked on the muscles in the lower half of the face,
on the opposite side
**** Upper spares the upper :-means UMN lesion will spare the wrinkling & eye closure .
lower motor neuron lesion →peripheral paralysis:
paralysis of all facial muscles on the same side
**Lower part of face ,only receives from contralateral side.
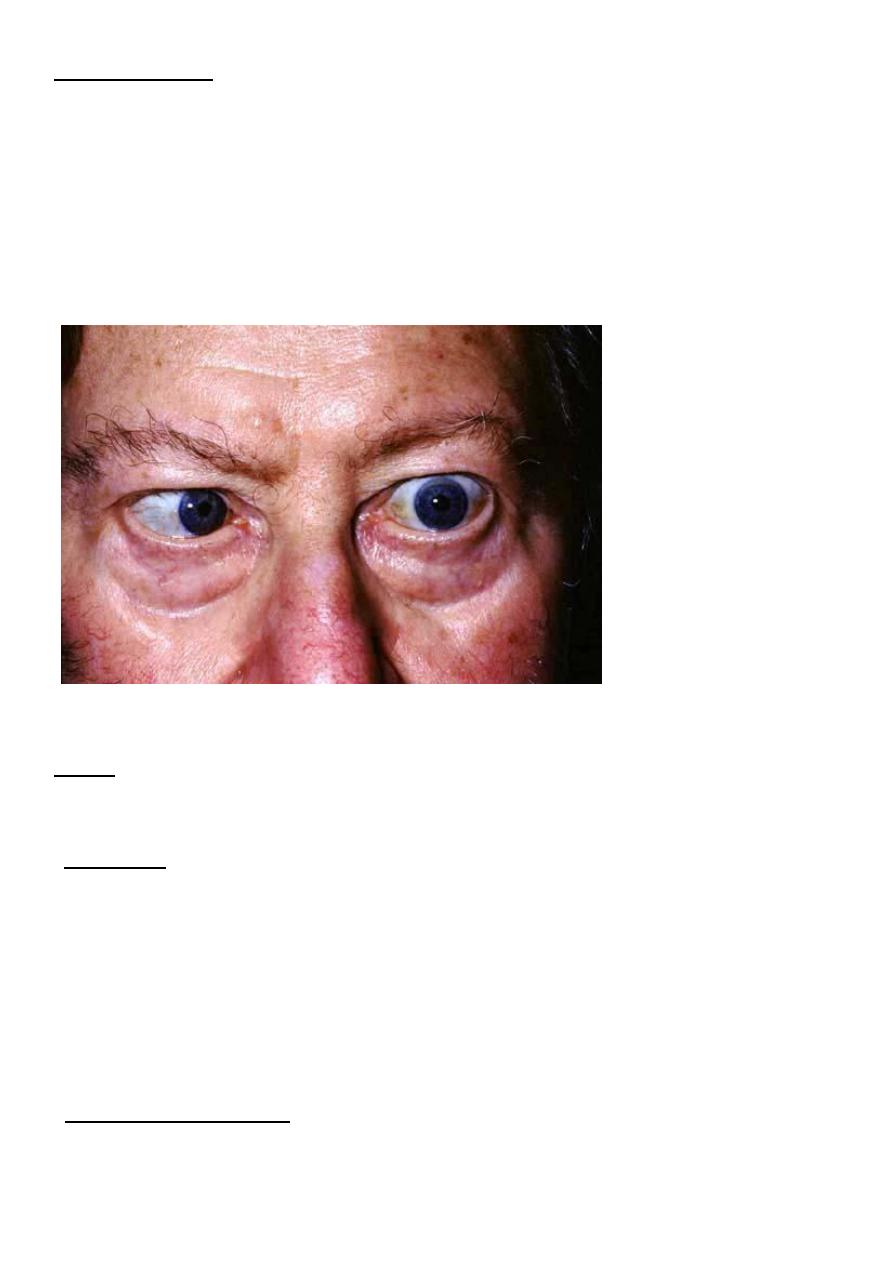
Bilateral 7thCN palsy Bells palsy.
--there will be wide palpebral fissure
--tongue deviate to normal side
IX, X, XI cranial nerve examination:-
• swallowing difficulty?
• assess the soft palate
– at rest (symmetrical? palatal arch is drooped?)
– during phonation (elevation?)
– gag reflex (pharyngeal) – symmetrical?
–
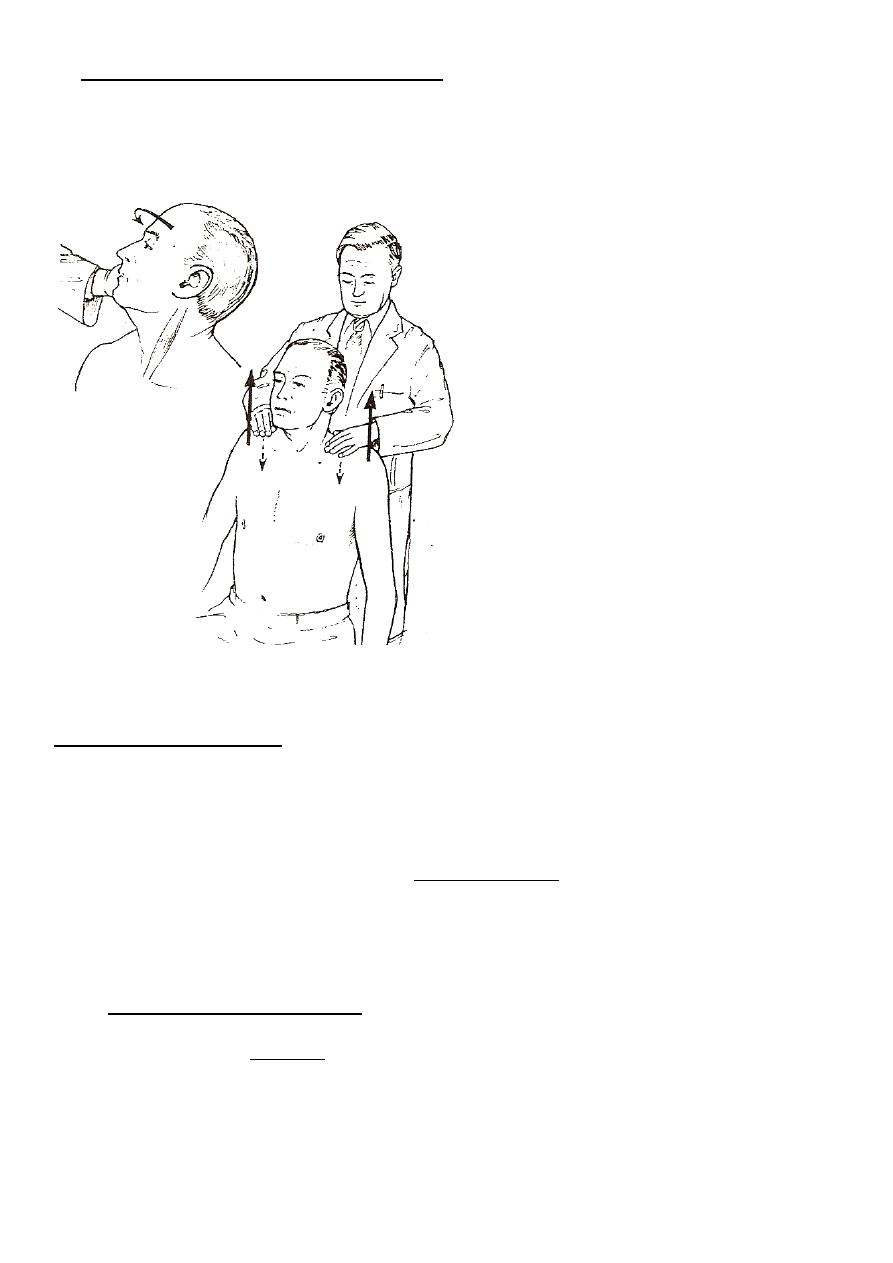
accessory nerveXI (external branch):
– sternomastoid muscle
– trapezius muscle
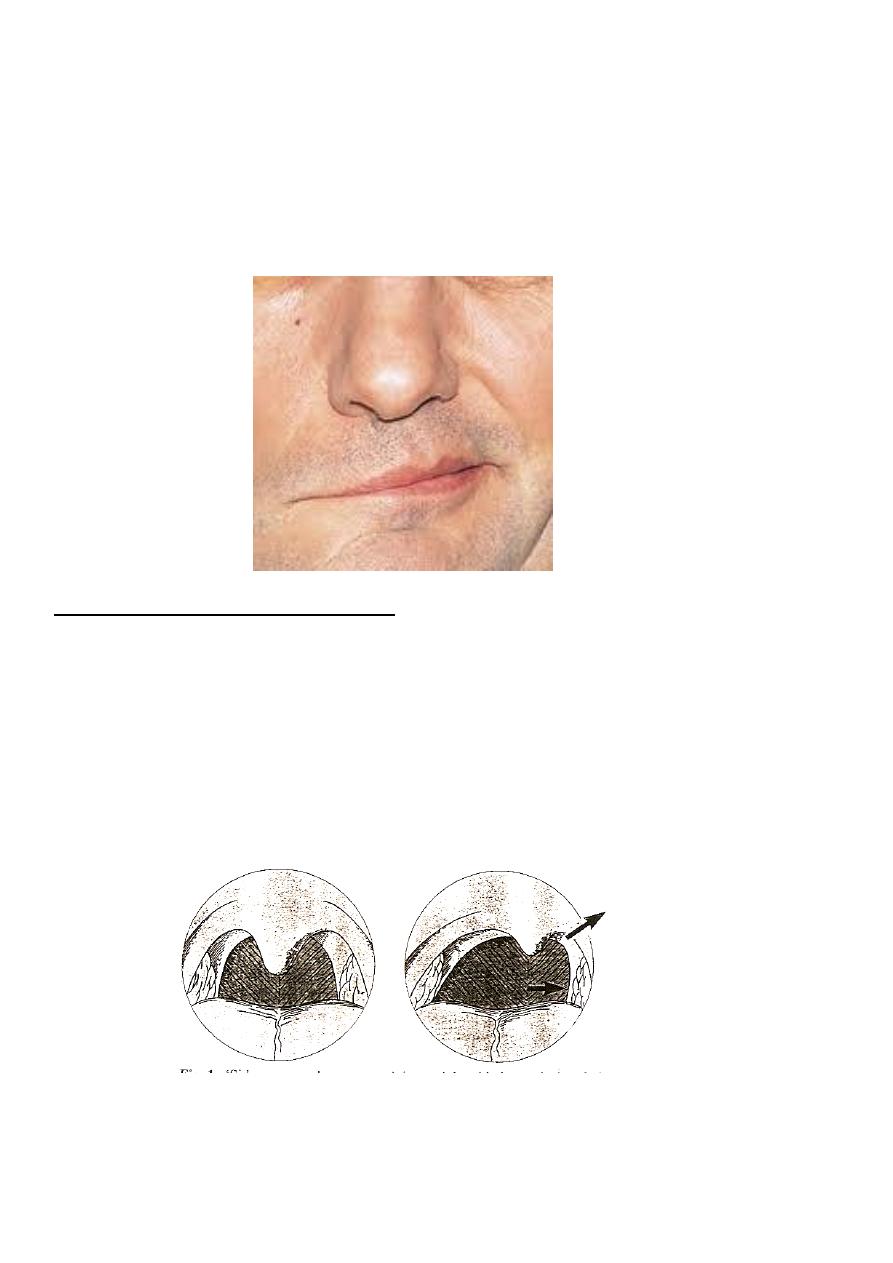
Hypoglossal nerve (XII)
Abnormal finding:-
– lower motor neuron paralysis
• tongue deviates to the side of the lesion
• atrophy
• Fasciculation
– upper motor neuron paralysis
tongue deviates opposite to the lesion
mild weakness
note :- in a normal person there may be tongue fasciculation (normally)on protruding
the tongue,so always inspect the tongue in its resting position in the mouth then ask
the pt to protrude it.
--3
rd
& 4
th
cranial nerves are located in mid brain
--5
th
,6 th ,7
th
are located in pons
--9
th
, 10
th
,11
th
are located in oblongata.
palsy:
Bulbar
1-lower motor neuron lesion, peripheral palsy
2-Dysarthria
3-Dysphagia
4-masseter reflex absent
5-tongue atrophy with fasciculation
cause :-GBS
Pseudobulbar palsy:-
1-upper motor neuron lesion, central palsy
2-dysarthria,
3- dysphagia,
4-masseter reflex increased
5-emotional lability (unprovoked crying or laughing)
cause: cerebrovascular disease
