THE PANCREAS
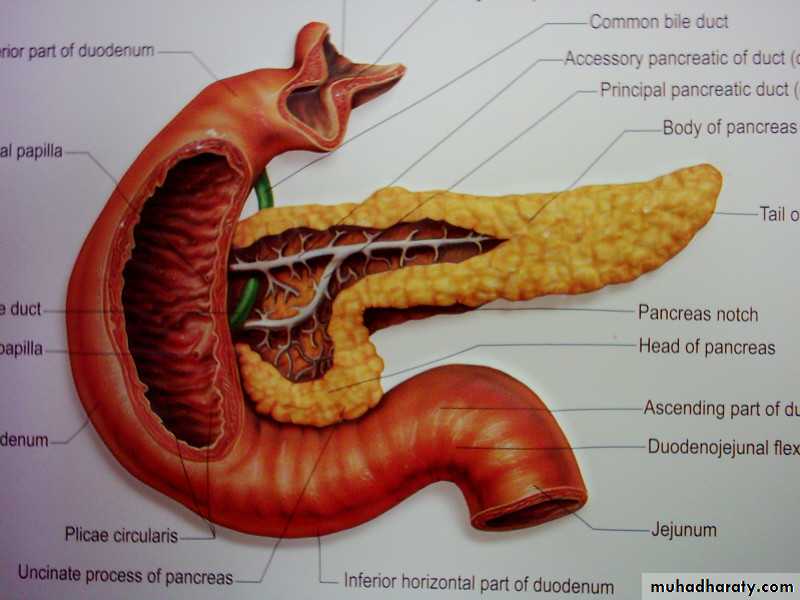
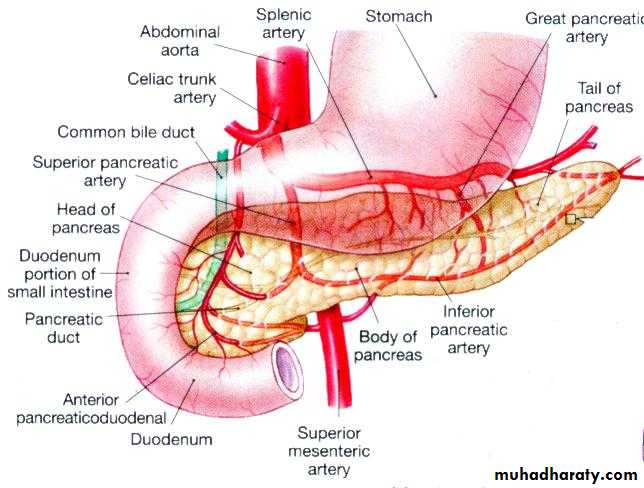
It is a retroperitoneal organ, it’s weight about 80 gm.
It secretes digestive enzymes in an alkaline bicarbonate rich fluid.Surgical physiology
Endocrine function .A cells which secrete glucagon.
B cells which secrete insulin.
C cells which secrete somatostatin.
Exocrine function.
lipase, amylase, as well as proteolytic enzymes as trypsinogen and chemotrypsinogen.Congenital Anomalies
1. Agenesis = incompatible with life
2. Pancreas Divisum = persistence as dorsal and ventral pancreasPredisposes to Chronic Pancreatitis
3. Annular pancreas = pancreatic head encircles the duodenum
Risk of Intestinal obstruction
4. Aberrant (or Ectopic) pancreas = located in the stomach, SI, Meckel’s Diverticulum, submucosal, yellow-gray nests
5. cystic fibrosis:
6. cystic disease of the pancreas
Pancreas - Pancreas Divisum
Pancreas - Annular pancreas
PANCREATITIS
• Acute pancreatitis: A single episode of pancreatitis in a previously normal gland. characterized by abdominal pain and raised pancreatic enzymes.
• Pathogenesis: autodigestion of the pancreas following premature activation of its proteolytic enzymes. And it returns to normal when the primary cause is removed.
•
AETIOLOGY
Biliary tract disease(50-70%):If the cause is gall stones, cholecystectomy is indicated in the same admission.
Alcohol abuse: 25%
Post ERCP:
Abdominal trauma:
Following surgery: biliary, upper gastrointestinal and cardiothoracic.
• Ampullary tumor
• Rare causes : as hypercalcemia, hyperparathyroidism, autoimmune pancreatitis, hereditary pancreatitis, malnutrition.• Viral infection (mumps)
• scorpion bite
• Idiopathic:
• Drugs: corticosteroids, thiazides, estrogen.
Pathology
• The peritoneal cavity :• blood stained exudates
• fat necrosis in greater omentum and peritoneum.
• Pancreas :
• edematous.
• hemorrhagic.
• necrotizing pancreatitis.
•
Acute Pancreatitis
• hemorrhage in the head of the pancreas
• fat necrosisCOMPLICATION systemic
• Cardiovascular: shock, arrhythmias• Pulmonary: ARDS
• Renal failure
• Hematological: DIC
• Metabolic: hypocalcemia, hyperglycemia, hyperlipidemia.
• Gastrointestinal: ileus
• Neurological: confusion, irritability
• local complication
Acute fluid collectionpancreatic necrosis
Pancreatic abscess
Pseudocyst
Pleural effusion
Portal/ systemic vein thrombosis
Pseudo-aneurysm
Clinical Picture
• occur at any age, with a peak in young men and older women.
• Symptoms
• Pain: severe reaching its maximum intensity within minutes, and persist for hours or days. It is constant in nature and intensity and refractory to analgesia. epigastric radiated to the back, may relieve on leaning forward.
• Nausea, Vomiting, retching, and hiccough.
• Peripheral vascular collapse and shock
• Death occurs from shock, ARDS, and renal failure
Signs
• General: The patient may be well or severely ill, with profound shock, toxicity and confusion.• Tachypnoea, tachycardia, and hypotension may be present.
• Body temperature may be normal or subnormal.
• Mild icters may develop caused by biliary obstruction.
• Abdominal:
• Mild epigastric tenderness and rigidity.• Distention due to ileus, or ascites.
• Bluish ecchymosis discoloration of the skin may be visible after 2-3 days in the flanks (Grey Turner sign ), or around the umbilicus (Cullen’s sign).
• Tender, palpable mass in the epigastric region.
Pancreatitis with retroperitoneal hemorrhage
Grey Turner’s sign
Cullen’s signRanson score
Investigation
Serum amylase :three to four times above normal is indicative of the disease, increase within24 hours.Serum lipase: increase specially in alcoholic pancreatitis
Urine amylase: increase and is of diagnostic value.
Serum calcium: may fall
Plain X-ray: abdomen may show sentinel loop, (local ileus).
Colon cut off sign
Calcified gall stones or pancreatic calcification.
Sentinel loop
Colon cut off sign• A chest radiograph may show a pleural effusion, and a diffuse alveolar interstitial shadowing may suggest ARDS.
• Ultrasonography can confirm the diagnosis of the pancreatic enlargement and edema, and the presence of gall stones.
• In doubt CT scan must be performed.
• Cross-sectional MRI
• EUS and MRCP: assess pancreatic parenchyma
• ERCP: allows identification and removal of stones in the common bile ducts.
Differential diagnosis
• Perforated peptic ulcer .• Acute cholecystitis.
• High intestinal obstruction.
• Acute mesenteric vascular occlusion.
• Acute myocardial infarction.
TREATMENT conservative treatment
• Admission to the ICU• Analgesia
• Aggressive fluid administration
• Oxygenation
• Monitoring of vital signs, CVP, urine output and blood gases.
• Frequent monitoring of hematological and biochemical parameters.
Nasogastric drainage
Antibiotic prophylaxis
CT if clinical deterioration or signs of sepsis develops.
ERCP within 72 hours for severe gallstone pancreatitis, or signs of cholangitis.
Supportive therapy for organ failure
If nutritional support is required, consider entral feeding.
Surgical treatment
Laparotomy when diagnosis is uncertain, shows white spots of fat necrosis, ascites, retroperitoneal hemorrhage, or pancreatic necrosis.The necrotic tissue is excised, a drain is left.
Treatment of local complication, a Pseudocyst, or abscess.
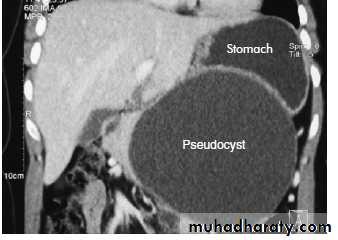
Pancreatic Pseudocyst
Is a collection of amylase rich fluid enclosed in a wall of fibrous or granulation tissue. The fluid aspirate should be sent for CEA, amylase and cytology.Etiology:
Acute pancreatitis
Pancreatic trauma
Pseudocyst
Complications
• Clinical Picture:
• History of trauma or pancreatitis.• Epigastric mass and pain
• Persistent amylase elevation
• 20-40% of these cases are resolved spontaneously within six weeks.
• Differential diagnosis
• Epigastric Abdominal masses
• Abscess or acute fluid collection
• Cystic tumor of the pancreas.
• Investigation:
• Barium meal• U/S, CT, MRI to monitor alteration in the size of the cyst.
• Fluid aspirate and send for CEA, amylase, and cytology.
• ERCP and MRCP
TREATMENT
Most cysts resolve spontaneously and need follow up only.
Thick wall cysts
size over 6 cm
persistent more than 12 weeks are less likely to resolve.
Liable for complication
The wall is mature for internal drainage. Transgastric cysto-gastrostomy.
• Internal drainage
• Cystgastrostomy• Cystjejunostomy
• External drainage
• May cause pancreatic fistula
• Excision
• Small, tail location
•