
1
Fifth stage
Medicine
Lec-10
د.بشار
15/12/2015
Subarachnoid Hemorrhage (SAH)
Subarachnoid hemorrhage is sudden bleeding into the subarachnoid space. The most
common cause of spontaneous bleeding is a ruptured aneurysm. Symptoms include
sudden, severe headache, usually with loss or impairment of consciousness.
Etiology
Subarachnoid hemorrhage is bleeding between the arachnoid and pia mater. Spontaneous
(primary) subarachnoid hemorrhage usually results from ruptured aneurysms. A congenital
intracranial saccular or berry aneurysm is the cause in about 85% of patients. Bleeding may
stop spontaneously. Aneurysmal hemorrhage may occur at any age but is most common
from age 40 to 65.
Less common causes are mycotic aneurysms, arteriovenous malformations, and bleeding
disorders.
Pathophysiology
Blood in the subarachnoid space causes a chemical meningitis that commonly increases
intracranial pressure for days or a few weeks. Secondary vasospasm may cause focal brain
ischemia; about 25% of patients develop signs of a transient ischemic attack (TIA) or
ischemic stroke. Brain edema is maximal and risk of vasospasm and subsequent infarction
(called angry brain) is highest between 72 h and 10 days. Secondary acute hydrocephalus is
also common. A 2nd rupture (rebleeding) sometimes occurs, most often within about 7
days.
Symptoms and Signs
Headache is usually severe, peaking within seconds. Loss of consciousness may follow,
usually immediately but sometimes not for several hours. Severe neurologic deficits may
develop and become irreversible within minutes or a few hours. Sensorium may be
impaired, and patients may become restless. Seizures are possible. Usually, the neck is not
stiff initially unless the cerebellar tonsils herniate. However, within 24 h, chemical
meningitis causes moderate to marked meningismus, vomiting, and sometimes bilateral
extensor plantar responses. Heart or respiratory rate is often abnormal. Fever, continued
headaches, and confusion are common during the first 5 to 10 days. Secondary
hydrocephalus may cause headache, obtundation, and motor deficits that persist for
weeks. Rebleeding may cause recurrent or new symptoms.
Diagnosis
Usually noncontrast CT and, if negative, lumbar puncture
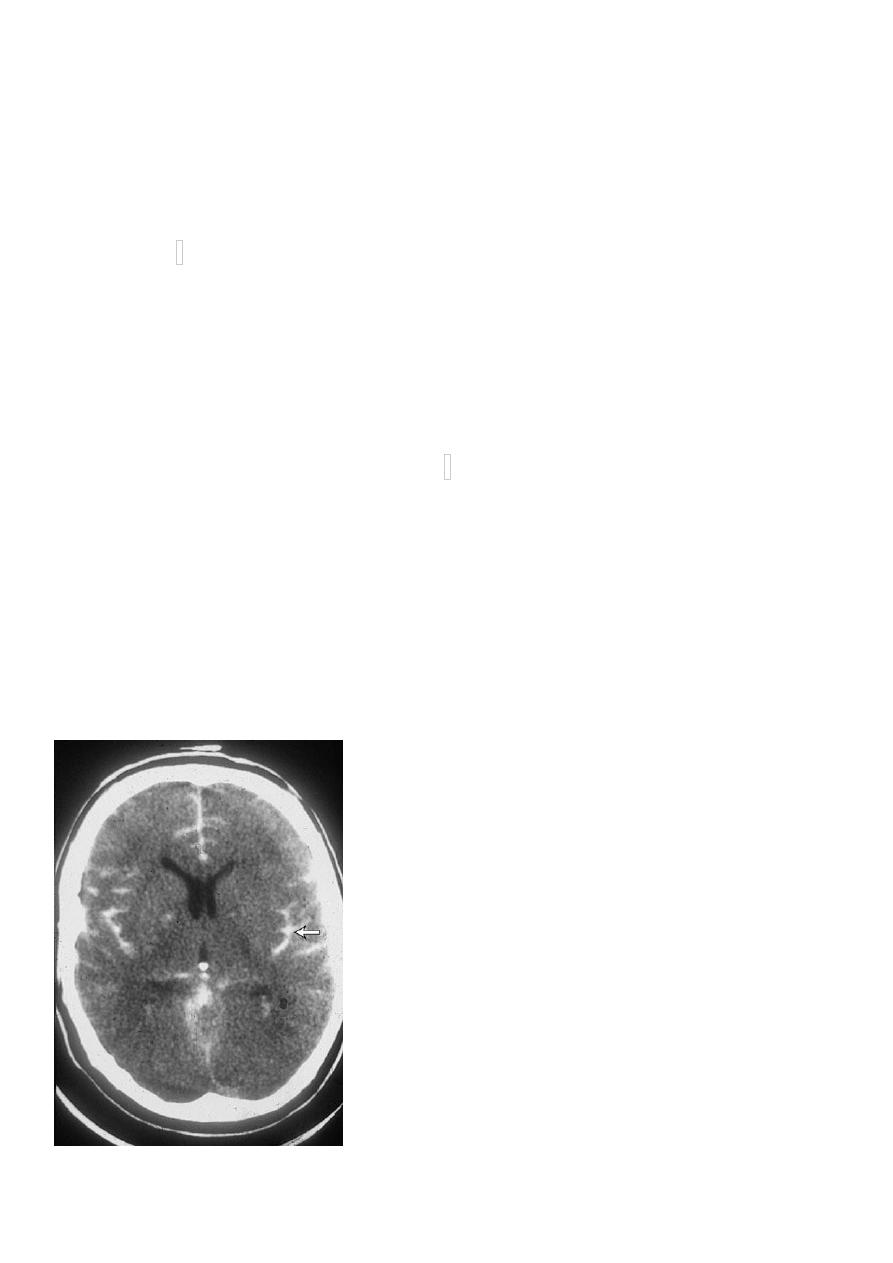
Diagnosis is suggested by characteristic symptoms. Noncontrast CT is > 90% sensitive and is
particularly sensitive if it is done within 6 h of symptom onset. MRI is comparably sensitive
2
but less likely to be immediately available. False-negative results occur if volume of blood is
small or if the patient is so anemic that blood is isodense with brain tissue. If subarachnoid
hemorrhage is suspected clinically but not identified by neuroimaging or if neuroimaging is
not immediately available, lumbar puncture is done .
CSF findings suggesting subarachnoid hemorrhage include numerous RBCs, xanthochromia,
and increased pressure. RBCs in CSF may also be caused by traumatic lumbar puncture.
Traumatic lumbar puncture is suspected if the RBC count decreases in tubes of CSF drawn
sequentially during the same lumbar puncture. About 6 h or more after a subarachnoid
hemorrhage, RBCs become crenated and lyse, resulting in a xanthochromic CSF supernatant
and visible crenated RBCs (noted during microscopic CSF examination); these findings
usually indicate that subarachnoid hemorrhage preceded the lumbar puncture. If there is
still doubt, hemorrhage should be assumed, or the lumbar puncture should be repeated in
8 to 12 h.
In patients with subarachnoid hemorrhage, conventional cerebral angiography is done as
soon as possible after the initial bleeding episode; alternatives include magnetic resonance
angiography and CT angiography. All 4 arteries (2 carotid and 2 vertebral arteries) should be
injected because up to 20% of patients (mostly women) have multiple aneurysms.
On ECG, subarachnoid hemorrhage may cause ST-segment elevation or depression. It can
cause syncope, mimicking MI. Other possible ECG abnormalities include prolongation of the
QRS or QT intervals and peaking or deep, symmetric inversion of T waves.
Prognosis
About 35% of patients die after the first aneurysmal subarachnoid hemorrhage; another
15% die within a few weeks because of a subsequent rupture. After 6 mo, a 2nd rupture
occurs at a rate of about 3%/yr. In general, prognosis is grave with an aneurysm, better
3
with an arteriovenous malformation, and best when 4-vessel angiography does not detect a
lesion, presumably because the bleeding source is small and has sealed itself. Among
survivors, neurologic damage is common, even when treatment is optimal.
Treatment
Treatment in a comprehensive stroke center Nicardipine if mean arterial pressure
is > 130 mm Hg
Nimodipine
to prevent vasospasm
Occlusion of causative aneurysms
Hypertension should be treated only if mean arterial pressure is > 130 mm Hg; euvolemia is
maintained, and IV nicardipine is titrated as for intracerebral hemorrhage .Bed rest is
mandatory. Restlessness and headache are treated symptomatically. Stool softeners are
given to prevent constipation, which can lead to straining. Anticoagulants and antiplatelet
drugs are contraindicated.
Vasospasm is prevented by giving nimodipine
60 mg po q 4 h for 21 days to prevent
vasospasm, but BP needs to be maintained in the desirable range (usually considered to be
a mean arterial pressure of 70 to 130 mm Hg and a systolic pressure of 120 to 185 mm Hg).
If clinical signs of acute hydrocephalus occur, ventricular drainage should be considered.
Aneurysms are occluded to reduce risk of rebleeding. Detachable endovascular coils can be
inserted during angiography to occlude the aneurysm. Alternatively, if the aneurysm is
accessible, surgery to clip the aneurysm or bypass its blood flow can be done, especially for
patients with an evacuable hematoma or acute hydrocephalus
