1
Fifth stage
Medicine
Lec-3
.د
فاخر
24/11/2015
RHEUMATOID ARTHRITIS
Definition
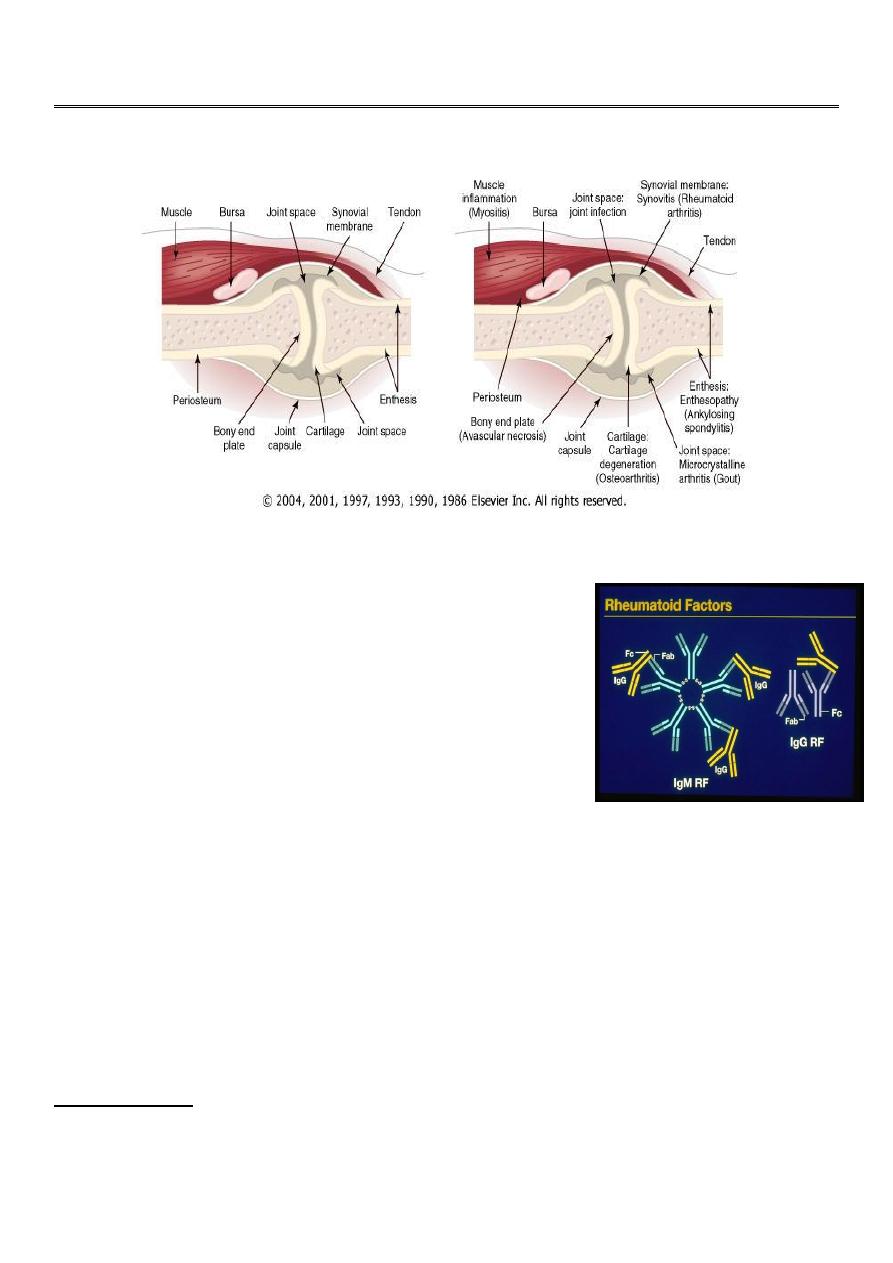
Chronic systemic inflammatory disorder affected synovium
bone, cartilage, ligaments with extra-articular manifestations
RA is a chronic disease that leads to joint damage within the
first 2 years, causes marked functional limitation and a 30%
loss of work within the first 5 years, and shortens life by 5 to
7 years.
Epidemiology
RA occurs throughout the world and in all ethnic groups. The prevalence is lowest in black
Africans and Chinese, and highest in the Pima Indians of Arizona. In Caucasians it is around
1.0-1.5% with a female:male ratio of 3:1. Before the age of 45, the female:male ratio is 6:1.
Prevalence increases with age, with 5% of women and 2% of men over 55 years being
affected.
Etiology
Genetic factors:
Family studies have demonstrated an increased risk for disease in siblings of persons
affected with RA. Concordance in monozygotic has been found to be 12% to 15% and 4% in
dizygotic twins.
2
Enviromental:
viruses (e.g., parvovirus B19, Epstein-Barr virus), Mycoplasma, and other bacteria (e.g.,
streptococci).
Urbanization: has a major impact on incidence & severity of R.A.
cigarettes smoking
Cellular immunity
Histopathology
The synovium of RA assumes the appearance of a reactive lymph node because of the
extensive infiltration by plasma cells, macrophages, and lymphocytes in the form of large
lymphoid follicles.
One characteristic feature of RA is the invasion of and damage to cartilage, bone, and
tendons by an infiltrating inflammatory synovial tissue mass called the pannus
3
Clinical Characteristics of Rheumatoid Arthritis
Diagnosis of RA is made with four or more of the following
Morning stiffness (> 1 hour
Arthritis of three or more joint areas
Arthritis of hand joints
Symmetrical arthritis
Rheumatoid nodules
Rheumatoid factor seropositive (rheumatoid factor positive )
Radiological changes
Duration of 6 weeks or more
Articular Morning stiffness, "gelling"Symmetrical joint swellingPredilection for wrists,
proximal interphalangeal, metacarpophalangeal, and metatarsophalangeal jointsErosions of
bone and cartilageJoint subluxation and ulnar deviationInflammatory joint fluidCarpal
tunnel syndromeBaker's cyst
Joints Affected :
Typically involves elbows, wrists, MCP, and PIP joints
1
st
& 2
nd
cervical vertebrae frequently involved
Unaffected joints :
Thoracolumbar spine, DIPs & SI joints
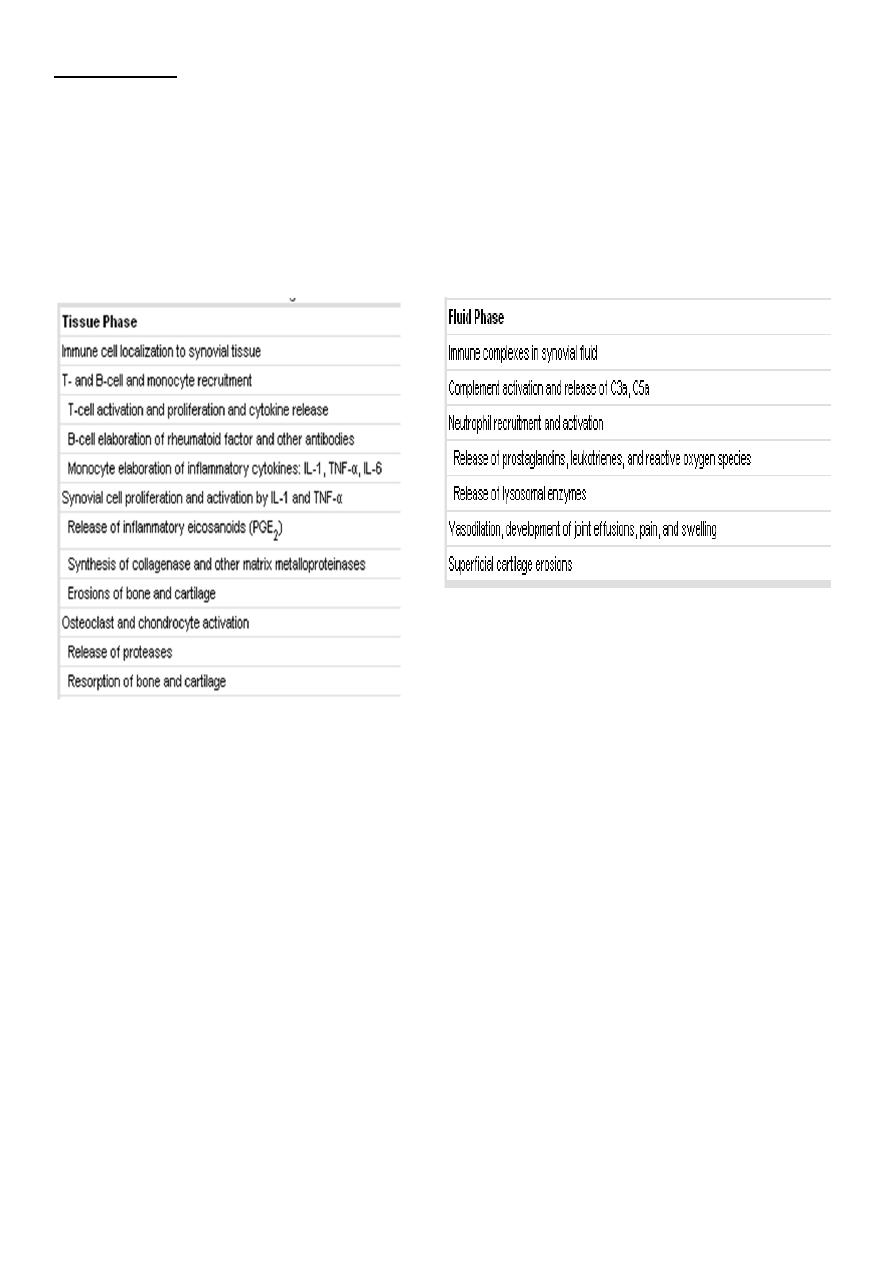
Rheumatoid Arthritis: PIP Swelling
Swelling is confined to the area of the joint capsule
Synovial thickening feels like a firm sponge
Rheumatoid HAND
An across-the-room diagnosis - Prominent ulnar
deviation in the right hand - MCP and PIP swelling in
both hands - MCP sublaxation - Synovitis of left wrist
4
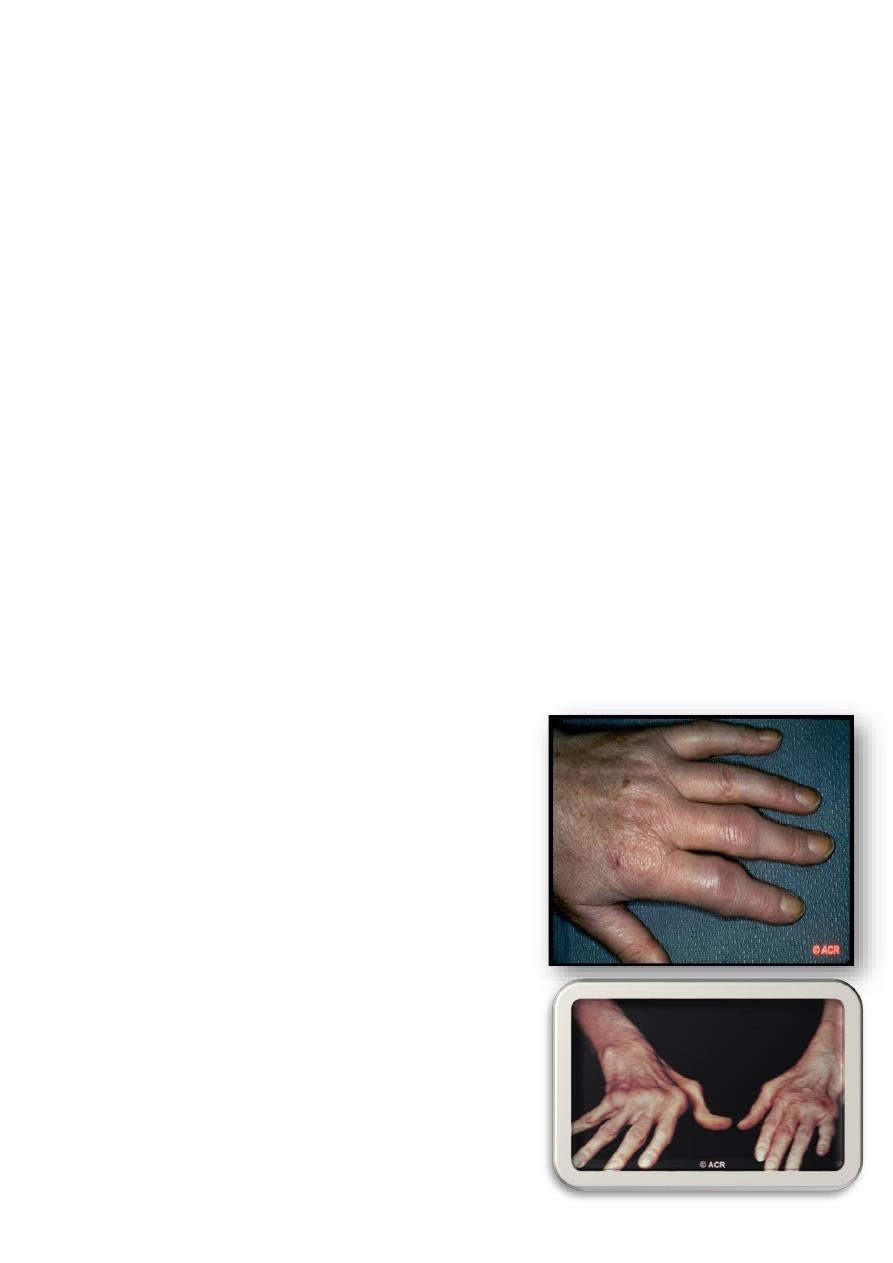
Rheumatoid arthritis: swan-neck and boutonnière
deformity, hand
hyperextension of the DIP joint of the finger
(boutonniere deformity, occurs as a consequence of
synovitis with stretching of, or rupture of, the PIP
joint through the central extensor tendon with
concomitant volar displacement of the lateral bands.
Hyperextension at the PIP joint with flexion of the DIP
joint (swan-neck deformity, may be initiated by
disruption of the extensor tendon at the DIP joint
with secondary shortening of the central extensor
tendon .
Rheumatoid arthritis: carpal tunnel syndrome, hand
Rheumatoid arthritis: subluxation and muscle
artrophy, hands
Rheumatoid arthritis: ruptured right popliteal cyst

5
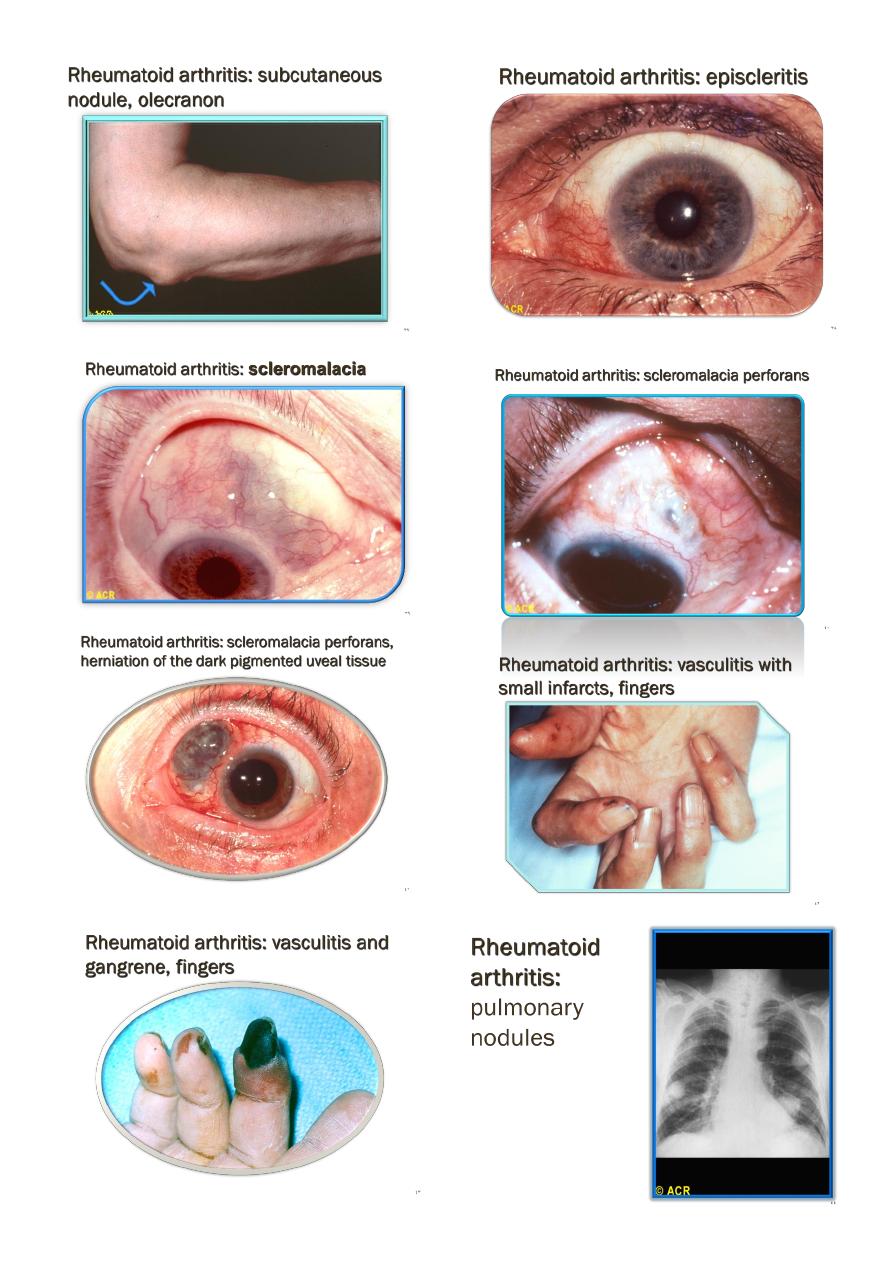
EXTRA-ARTICULAR MANIFESTATIONS OF RHEUMATOID DISEASE
Haematological
Anaemia
Thrombocytosis
Eosinophilia
Lymphatic
Splenomegaly
Felty's syndrome
Nodules
Sinuses
Fistulae
Ocular
Eapiscleritis
Scleritis
Scleromalaciaa
Keratoconjunctivitis sicca
Vasculitis
Digital arteritis
Ulcers
Pyoderma gangrenosum
Mononeuritis multiplex
Visceral arteritis
Cardiac
Pericarditis
Myocarditis
Endocarditis
Conduction defects
Coronary vasculitis
Granulomatous aortitis
Pulmonary
Nodules
Pleural effusions
Fibrosing alveolitis
Bronchiolitis
Caplan's syndrome

6
Neurological
Cervical cord compression
Compression neuropathies
Peripheral neuropathy
Mononeuritis multiplex
Cutaneous features
Subcutaneous rheumatoid nodules occur almost exclusively in seropositive patients,
usually at sites of pressure or friction such as the extensor surfaces of the forearm,
sacrum, Achilles tendon and toes
Cardiovascular features
Asymptomatic pericarditis occurs in approximately 30% of patients with seropositive
RA, with pericardial effusions and constrictive pericarditis being rare complications.
Occasionally, granulomatous lesions result in heart block, cardiomyopathy, coronary
artery occlusion or aortic regurgitation.
Laboratory Tests
Raised inflammatory markers . Reasonable correlation with clinical activity
Mild anemia & thrombocytosis
S. Rheumatoid factor (Agglutination method). Positive in near 70-80% cases (western
countries). Not specific
Anti-CCP (citrulline – containing proteins) antibodies. Similar sensitivity to RF but
more specific (up to 95%)
Examination of joint fluid
the most helpful laboratory procedure. The fluid is inflammatory, with more than 10,000
white blood cells and a predominance of polymorphonuclear leukocytes, typically 80% or
more. Rheumatoid factor, an IgM antibody directed to IgG, is found in 80 to 90% of patients
with RA..
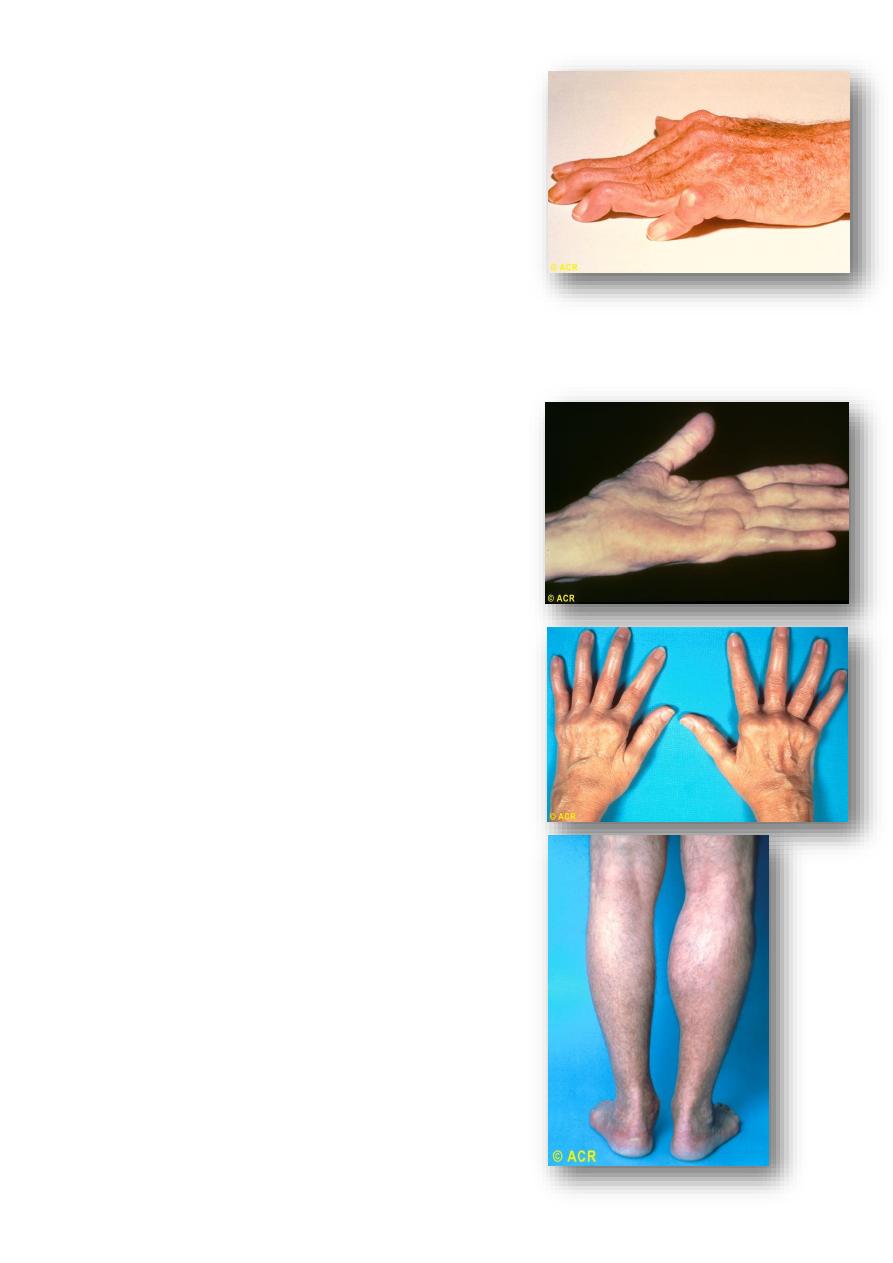
XR-Findings
Peri articular osteopenia
Marginal erosions (at least months of persistent activity)
Joint space narrowing (cartilage loss)
Ankylosis (wrists)
Deformities
7
8
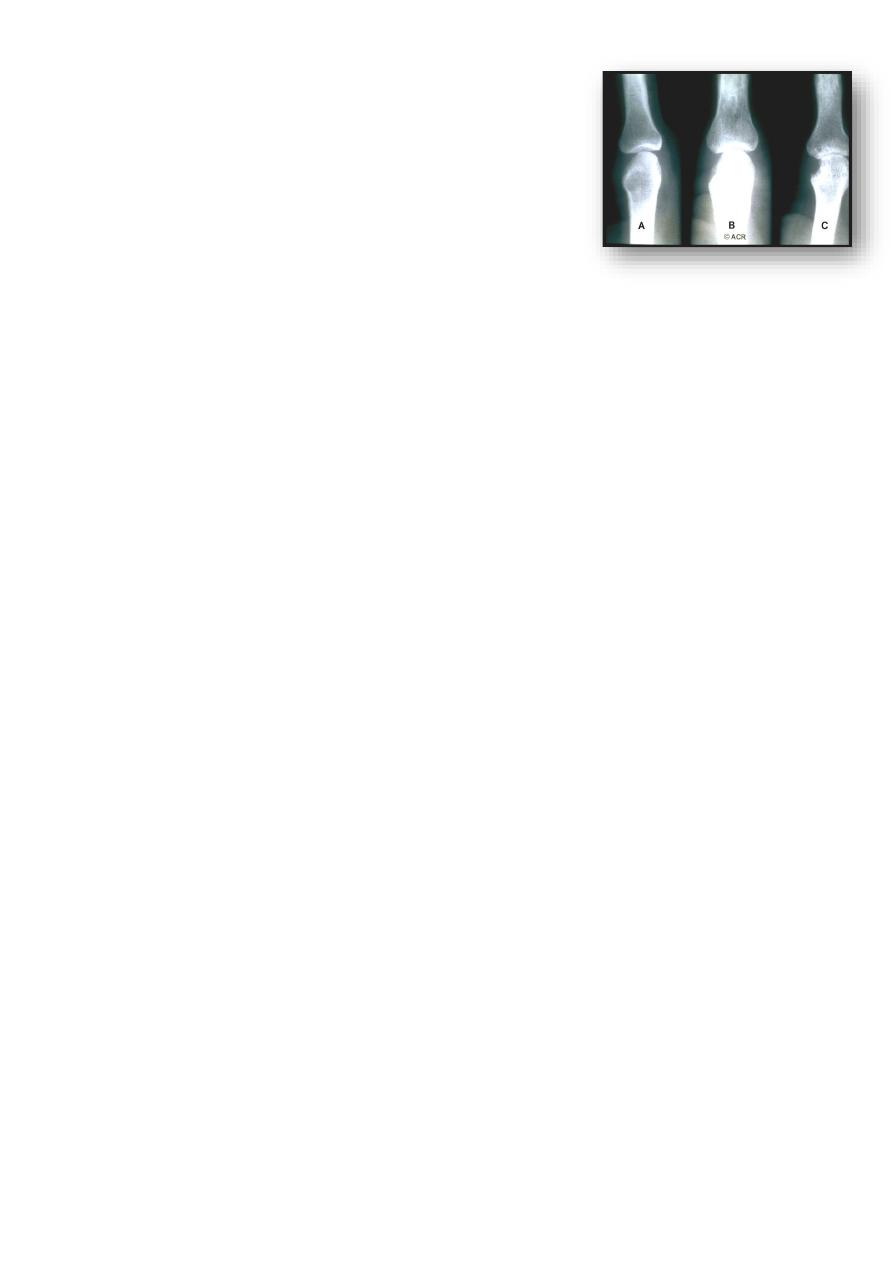
Joint damage progression in R.A. hand
Soft-tissue swelling, no erosions
Thinning of the cortex on the radial side and minimal
joint space narrowing
Marginal erosion at the radial side of the metacarpal
head with joint space narrowing
Prognosis
The following factors at presentation are associated with a poor prognosis: higher baseline
disability
female gender
involvement of MTP joints
positive rheumatoid factor
disease duration of over 3 months.
