1
Fifth stage
ENT
Lec-12
د.سعد
16/12/2015
Stridor
Stridor is noisy respiration produced by turbulent airflow through the narrowed air passages. It could
be inspiratory, expiratory or mixed.
Laryngeal stridor:
1- Congenital: e.g. Laryngeal web, larygomalacia, congenital vocal cord paralysis.
2- Traumatic: external, internal.
3- Inflammatory:
Acute: e.g. acute laryngitis, diphtheritic laryngitis.
Chronic laryngitis: TB.
4- Neoplastic: Benign: multiple papilloma of larynx, fibroma.
Malignant: carcinoma.
5- Neuromuscular: e.g. lesions of the base of the skull.
Extra-laryngeal stridor: e.g. retropharyngeal abscess, parapharyngeal abscess, tumors of thyroid
gland…etc.
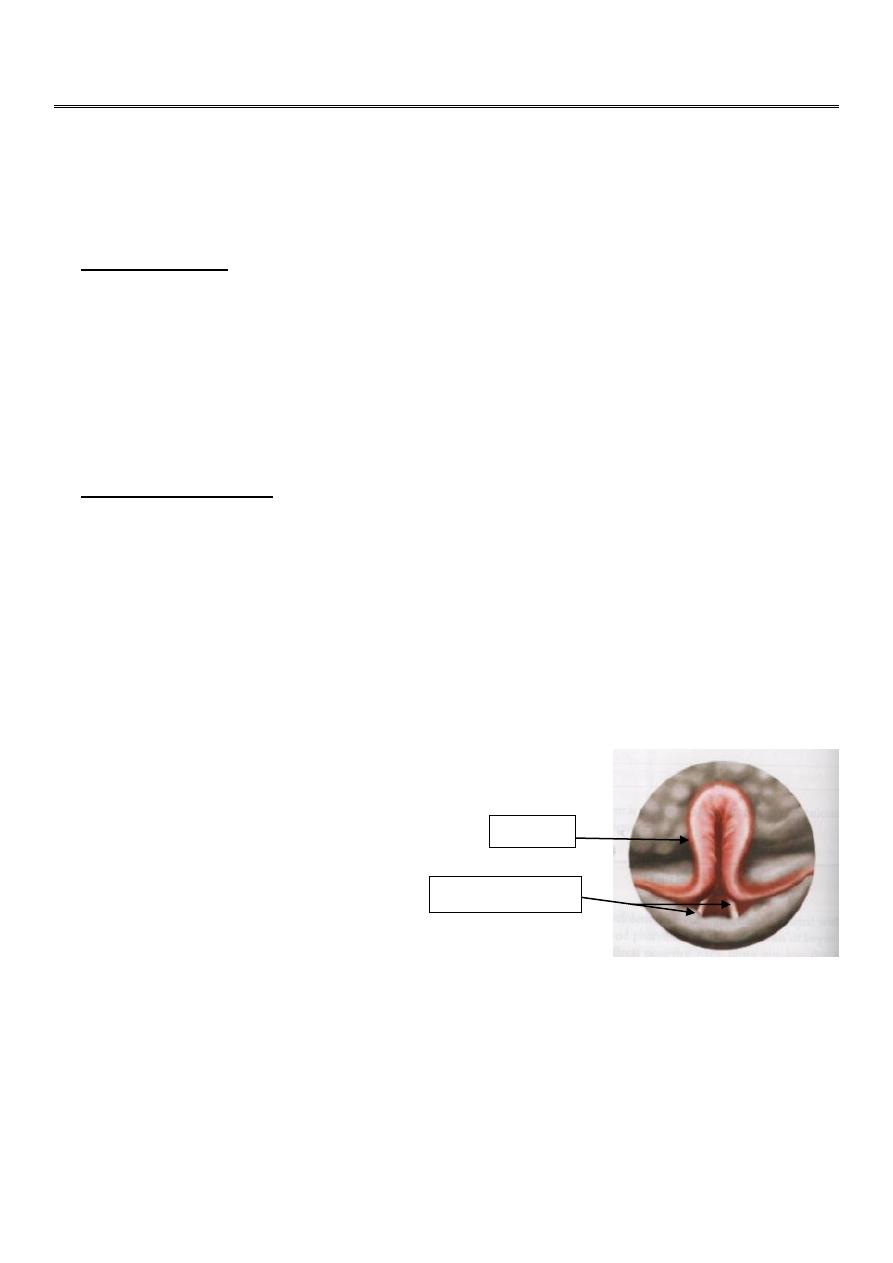
Laryngomalacia
It is the most common congenital abnormality of the larynx. It is characterized by excessive flaccidity
of supraglottic larynx which is sucked in during inspiration producing stridor and sometimes cyanosis.
Stridor is increased on crying but subsides on placing the child in prone position; cry is normal (i.e.
voice is unchanged).
The condition manifests at birth or soon after and usually disappears by 2 years of age. Direct
laryngoscopy shows elongated epiglottis, curled upon itself (omega-shaped
), floppy aryepiglottic
folds and prominent
arytenoids. Flexible laryngoscopy is very useful to make the diagnosis.
Treatment: conservative and reassurance. Tracheostomy may be required for some cases of severe
respiratory obstruction.
Congenital vocal cord paralysis
Caused by birth trauma (e.g. forceps delivery) or anomaly of CNS.
Epiglottis
Aryepiglottic folds
2
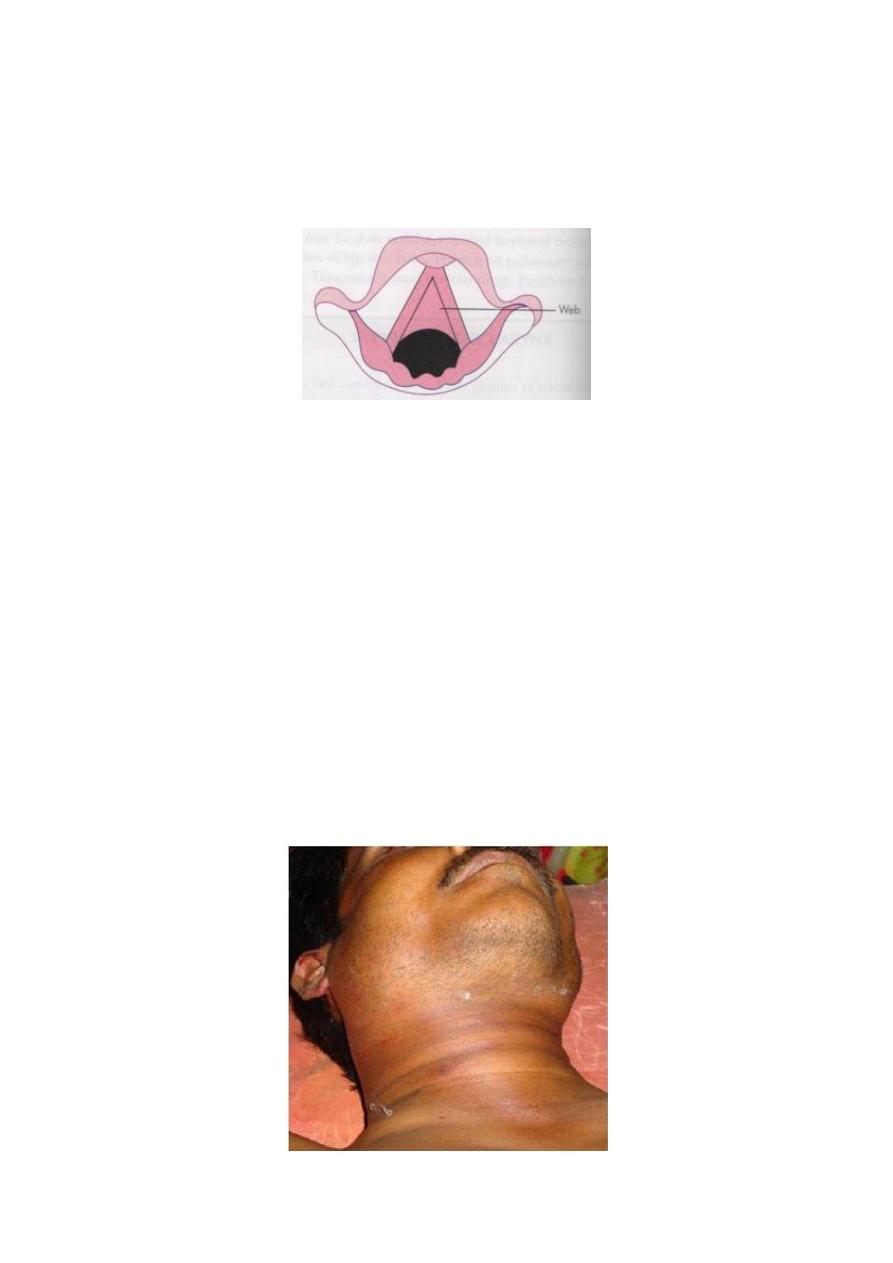
Laryngeal web
It is due to incomplete recanalisation of the larynx. Mostly, the web is seen between the vocal cords
in the anterior half of the glottis. The presenting features are airway obstruction, weak cry or aphonia
dating from birth.
Treatment: depends on the thickness of the web. Thin webs can be cut with a knife or CO2 laser.
Thick ones may require excision via laryngofissure.
Traumatic conditions
Aetiology
1- External trauma: blow on the neck, strangulation, car accident.
2- Internal trauma: F.B., instrumental injury as oesophagoscope and laryngoscope.
Pathology
1- Haematoma and oedema of supraglottic or subglottic region.
2- Tear of mucosa leading to subcutaneous emphysema.
3- Fracture of the hyoid bone, thyroid cartilage, or cricoid cartilage (the latter is fatal).
4- Dislocation of cricoarytenoid or cricothyroid joints.
5- There may be associated injury to the great vessels.
Clinical features: respiratory distress, hoarseness, painful and difficult swallowing, laryngeal pain
marked on speaking or swallowing and haemoptysis when there is tear of mucosa.
O/E: bruises, tenderness and surgical emphysema.
Investigation: X-ray soft tissue of the neck and CT scan is required.
3
Treatment:
Conservative:
1- Hospital admission and observation for respiratory distress.
2- Voice rest.
3- Humidification of inspired air.
4- Steroid in full dose to resolve oedema and prevent scarring and stenosis.
5- Analgesics.
6- Antibiotics to prevent perichondritis and cartilage necrosis.
Surgical: Tracheostomy and open reduction.
Burns and scalds
Aetiology
1- Inhalation of irritant fumes or gases
2- Swallowing of corrosive fluids.
3- Inhalation of steam.
Clinical features: Respiratory distress is the presenting symptom, pain and dysphagia are usual.
Treatment is conservative (the same as in laryngeal trauma). Tracheostomy is done when the airway
is compromised.
Radiotherapy reactions
Severe local reaction may follow radical radiotherapy; this is aggravated by smoking, drinking of
spirit and local infection. Dyspnoea occurs at the onset followed by discomfort during swallowing.
Severe pain with foul smell indicates perichondritis or cartilage necrosis.
Treatment: systemic antibiotics and steroids. Tracheostomy is rarely indicated.
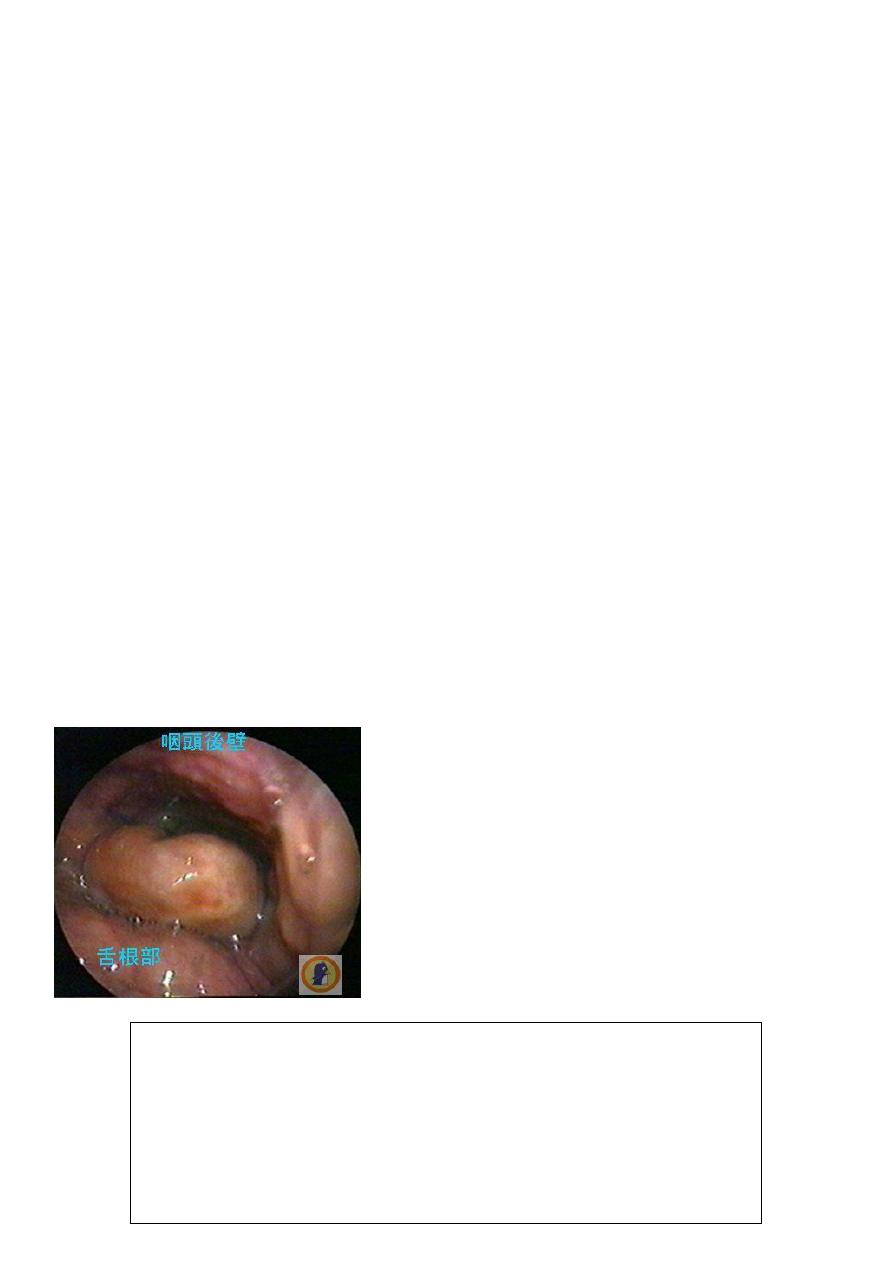
Acute Epiglottitis
Is a serious condition affects mainly children (2-7 years)
caused by bacterial infection (H. influenzae). Dyspnoea and
stridor are common presenting
Symptoms in children. They are rapidly
progressive and fatal unless relieved. Fever
may go up to 40°C. Depressing the tongue
should be avoided for fear of precipitating
complete obstruction or be done in the
operation theater where the facilities for
intubation are available.
Lateral soft tissue x-ray of neck may show
swollen epiglottis (thumb sign).
Treatment:
1) hospitalization
2) antibiotics (ampicillin or 3
rd
generation cephalosporin)
3) steroid
4) I.V. fluid
5) humidification of inspired air with oxygen
6) Intubation or tracheostomy may be required

4
Inhaled Foreign Bodies
F.B in the larynx is a rare condition but a sharp F.B. such as pin or glass may be impacted in the
larynx. Large F.B. such as a bolus of food is almost immediately fatal when impacted in the larynx.
Clinical features: Three stages:
1- Initial period of chocking, gagging and wheezing: this lasts for a short time. FB may be
coughed out or it may lodge in the larynx or further down in the tracheobronchial tree.
2- Symptomless interval: because the respiratory mucosa adapts to the presence of FB. This
interval varies with the size and nature of FB.
3- Later symptoms: caused by obstruction of the airway due to inflammation or trauma induced
by FB and depends on the site of its lodgment. Laryngeal FB, if large, may totally obstruct the
airway leading to sudden death. A partially obstructive FB will cause discomfort or pain in the
throat, hoarseness, croupy cough, aphonia, dyspnoea, wheezing and haemoptysis.
Treatment: Removal by direct laryngoscopy as soon as possible. Emergency tracheostomy may be
necessary.
Intubation injury
Aetiology
It occurs in patient with prolonged intubation in the intensive care unit, and it is due to:
1- Rough intubation with inadequate muscle relaxant.
2- Prolonged period of intubation.
3- The use of too large tubes.
4- Inadequate fixation of the tube, so the tube moves up and down leading to mucosal abrasion.
Pathology
1- Superficial mucosal abrasion.
2- Granuloma formation which is commoner in women 4:1
3- Subglottic oedema more in children.
Clinical features
Hoarseness and sometimes dyspnoea.
Prevention
Avoidance of blind intubation, the use of approximate size tube, good fixation and the use of portex
tube rather than rubber which is so irritant. Tracheostomy should be done if intubation is required for
more than few days.
Treatment
Voice rest.
Endoscopic removal of granuloma.

5
Clinical Approach to Stridulous Child
History
Stridor is a physical sign not a disease. Attempt should always be made to discover the cause. It is
important to elicit:
1- Time of onset to find whether cause is congenital or acquired.
2- Mode of onset. Sudden onset (FB, oedema), gradual and progressive (laryngomalacia, juvenile
papilloma).
3- Duration. Short (FB, oedema, infection), long ( laryngomalacia, laryngeal stenosis).
4- Relation to feeding. Aspiration in laryngeal paralysis.
5- Cyanotic spells. Indicate needs for airway maintenance.
6- Aspiration or ingestion of a FB.
7- Laryngeal trauma.
Physical examination:
a- Stridor is always associated with respiratory distress. There may be recession of suprasternal
notch, intercostal spaces and epigastrium during inspiratory efforts.
b- Note whether stridor is inspiratory, expiratory or biphasic which indicate the probable site of
obstruction.
c- Fever is associated with infection.
d- Stridor of laryngomalacia disappears when the baby lies in prone position.
e- Examination of nose, tongue, jaw and pharynx and larynx can exclude local pathology in these
areas. Fiberoptic laryngoscopy and direct laryngoscopy under general anesthesia are required.
Radiography:
1- X-ray of chest and soft tissue neck both AP and lateral view.
2- CT scan/MRI.
Treatment
Once the diagnosis has been made, treatment of exact cause can be planned.
