
1
Fifth stage
Medicine
Lec-6
.د
فاخر
22/12/2015
SERONEGATIVE SPONDYLO ARTHROPATHIES
This term is applied to a group of inflammatory joint diseases
1-Ankylosing spondylitis
2-Reactive arthritis, including Reiter's syndrome
3-Psoriatic arthropathy
4-Arthritis associated with inflammatory bowel disease (Crohn's disease, ulcerative colitis)
The synovitis is non-specific and is often indistinguishable from RA. However, the
distinctive feature of this group of diseases is the marked degree of extrasynovial
inflammation, especially of the enthesis but also of the joint capsule, periosteum,
cartilage and subchondral bone. There is a striking association with carriage of the HLA-
B27 sacroiliitis, uveitis or balanitis
Understanding of the cause is incomplete but an aberrant response to infection is
thought to be involved in genetically predisposed individuals. In some situations, a
triggering organism can be identified, as in reactive arthritis following bacterial
dysentery or chlamydial urethritis
CLINICAL FEATURES COMMON TO SERONEGATIVE SPONDARTHRITIS
1. Asymmetrical inflammatory oligoarthritis (lower > upper limb)
2. Sacroiliitis
3. inflammatory spondylitis
4. Inflammatory enthesitis
5. Absence of nodules and other extra-articular features of RA
6. Male predominance in A.S. & in Re A
7. Association with HLA-B27
8. Mucosal surface inflammation-conjunctivitis, buccal ulceration, urethritis, prostatitis,
bowel ulceration Pustular skin lesions, nail dystrophy
9. Anterior uveitis
10. Aortic root fibrosis (aortic incompetence, conduction defects)
11. Erythema nodosum
2
Ankylosing Spondylitis
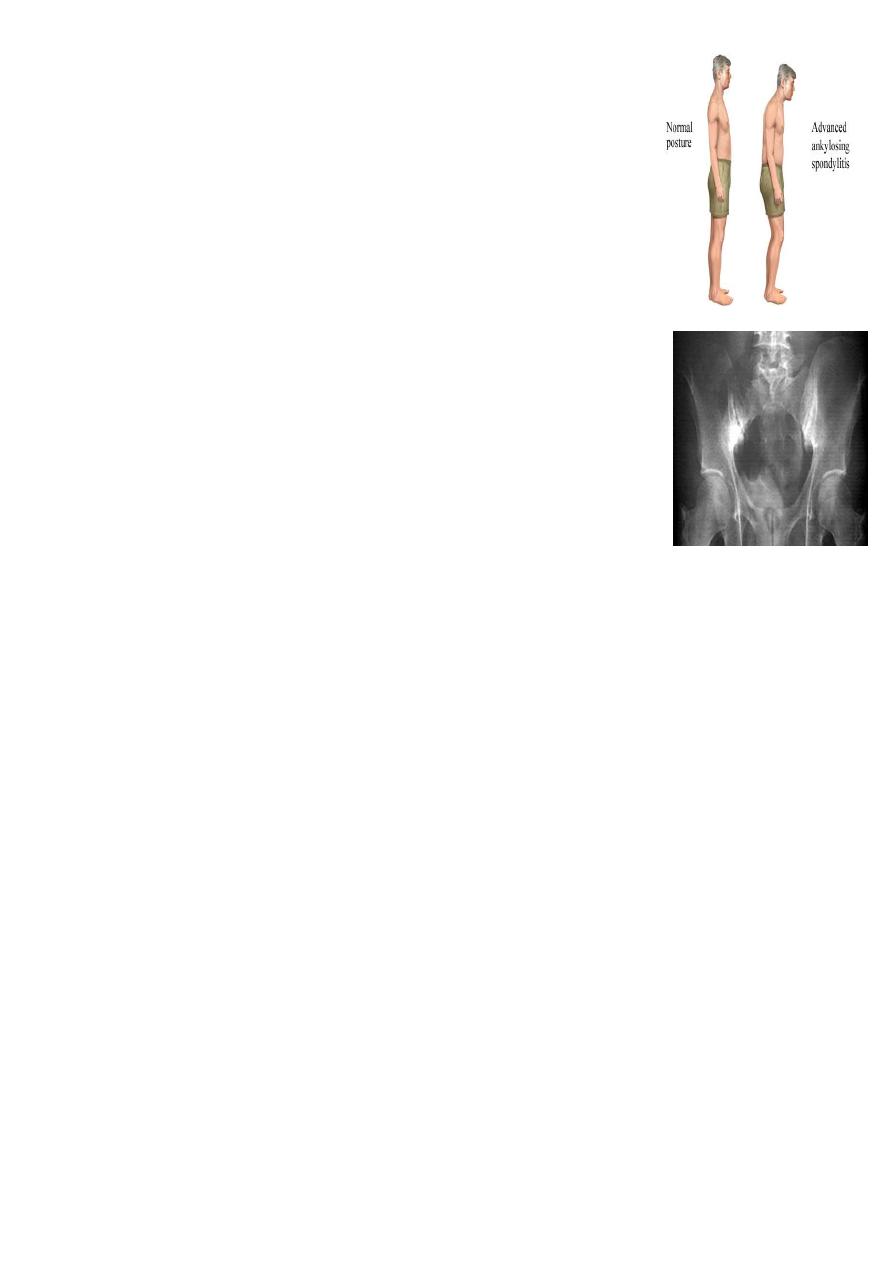
Ankylosing spondylitis (AS) is characterised by a chronic
inflammatory arthritis predominantly affecting the sacroiliac joints
and spine, which can progress to bony fusion of the spine. The
onset is typically between the ages of 20 and 30, with a male
preponderance of about 3 : 1. In Europe, more than 90% of those
affected are HLA-B27-positive. The overall prevalence is less than
0.5% in most populations
Ankylosing spondylitis is thought to arise from an as yet ill-defined
interaction between environmental pathogens and the host immune
system in genetically susceptible individuals. Increased faecal carriage
of Klebsiella aerogenes occurs in patients with established AS and may
be relate to exacerbation of both joint and eye disease
1. General Features
The cardinal feature is low back pain and early morning stiffness
with radiation to the buttocks or posterior thighs. Symptoms are exacerbated by
inactivity and relieved by movement. The disease tends to ascend slowly, ultimately
involving the whole spine, although some patients present with symptoms of the
thoracic or cervical spine. As the disease progresses, the spine becomes increasingly
rigid as ankylosis occurs.
Early physical signs include a reduced range of lumbar spine movements in all
directions and pain on sacroiliac stressing. As the disease progresses, stiffness increases
throughout the spine and chest expansion becomes restricted. Spinal fusion varies in
its extent and in most cases does not cause a gross flexion deformity, but a few
patients develop marked kyphosis
Pleuritic chest pain aggravated by breathing is common and results from costovertebral
joint involvement. Plantar fasciitis, Achilles tendinitis and tenderness over bony
prominences such as the iliac crest and greater trochanter may all occur, reflecting
inflammation at the sites of tendon insertions (enthesitis) .
Up to 40% of patients also have peripheral arthritis.
This is usually asymmetrical, affecting large joints such as the hips, knees, ankles and
shoulders. In about 10%
of cases, involvement of a peripheral joint may antedate spinal symptoms, and in a
further 10%, symptoms begin in childhood, as in the syndrome of oligoarticular juvenile
idiopathic arthritis
3
Extraskeletal Features
Anterior uveitis (25%)
Conjunctivitis (20%)
Cardiac valve involvement / aortitis / conduction defects / pericarditis
Apical pulmonary fibrosis
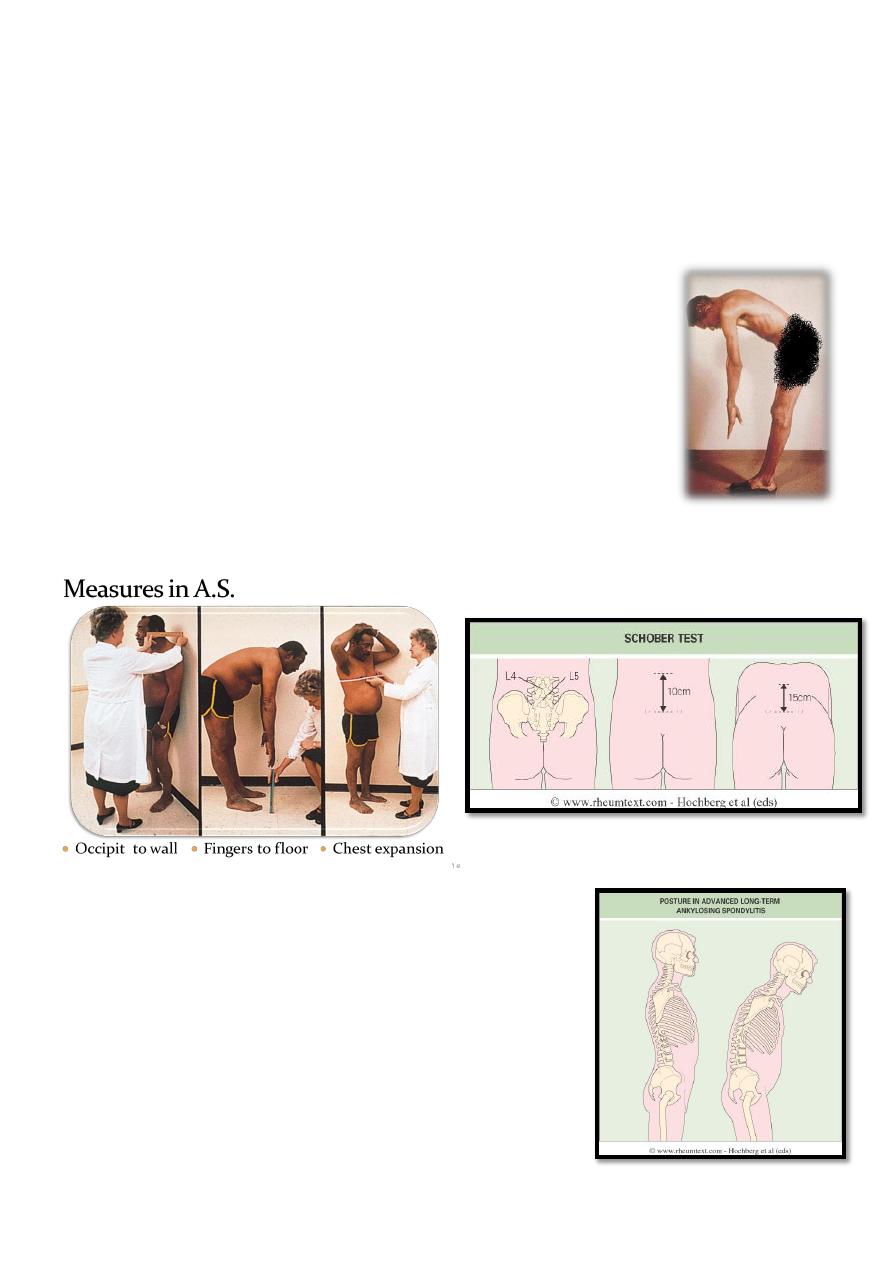
Spine Examination
Inspection :
o Posture (spine & lower limbs)
Palpation :
o Sacroiliac joints
o Chest expantion
Range of movement :
o Finger to floor measurement
o Occipit to wall
o Schober test
INVESTIGATIONS
ESR & C-reactive protein
Blood count, renal & liver profiles when therapy
indicates
HLA-B27 test when diagnostic difficulty is present
4
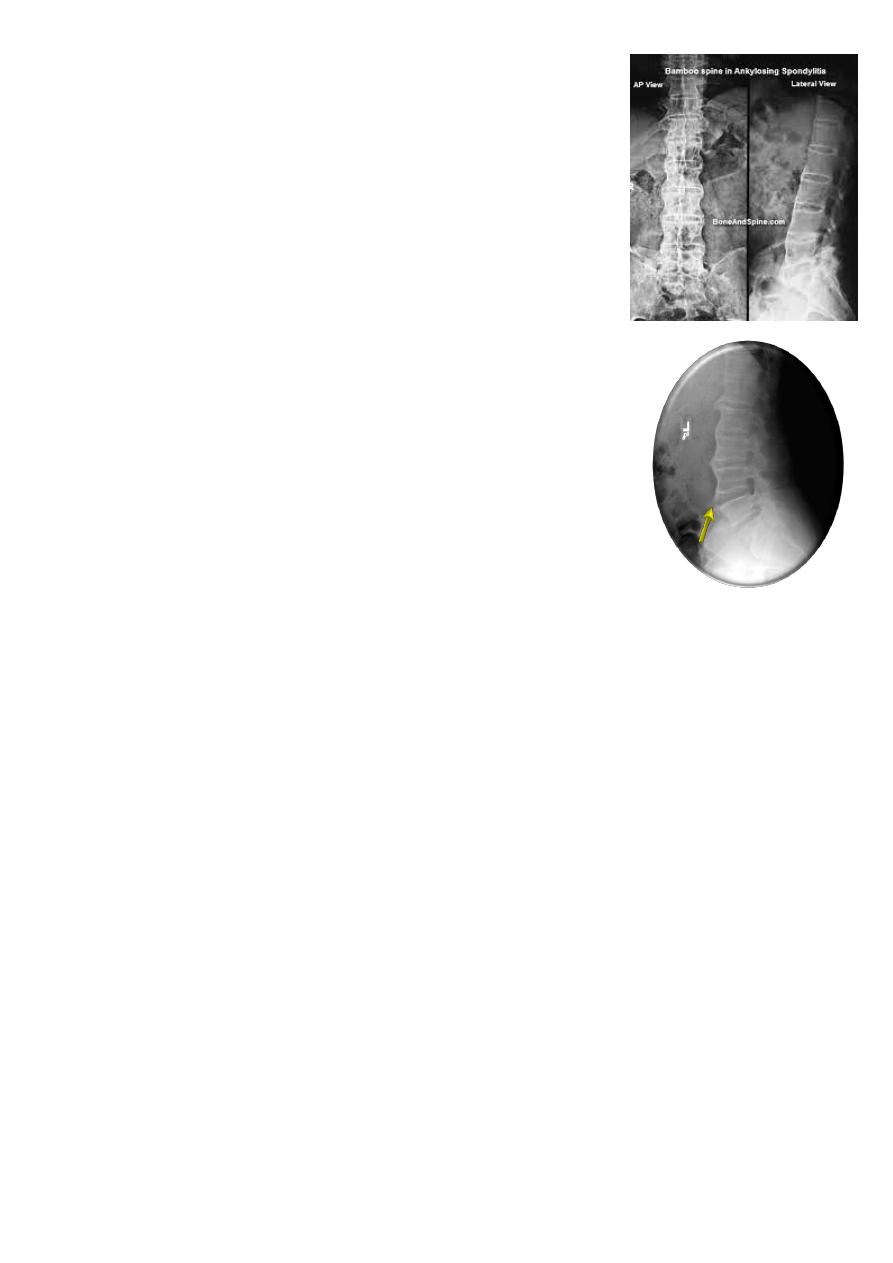
X-Rays:
Sacroiliac joints :
Sclerosis ankylosis joint obliteration
Spine XR :
Squared vertebrae (periosteitis)
Syndysmophytes = bony bridging (post inflammatory
calcification)
Bamboo spine (advanced cases)
DISH
“non spondylitic vertebral anterior enthesopathy “
Management
The aims are to relieve pain and stiffness, maintain a maximal
range of skeletal mobility and avoid deformity
NSAIDs are effective in relieving symptoms but do not alter the course of the disease.
The slow-acting antirheumatic drugs sulfasalazine, methotrexate or azathioprine may
control persistent peripheral joint synovitis but appear to have little or no impact in
suppressing axial disease.
However, recent studies have shown that anti-TNF therapy may improve the symptoms and
signs of ankylosing spondylitis,
Local corticosteroid injections can be useful for persistent plantar fasciitis and other
enthesopathies. Oral steroid may occasionally be required for acute uveitis but should
otherwise be avoided. Severe hip, knee or shoulder restriction may require surgery.
5
Reactive Arthritis
Reiter’s syndrome & related conditions
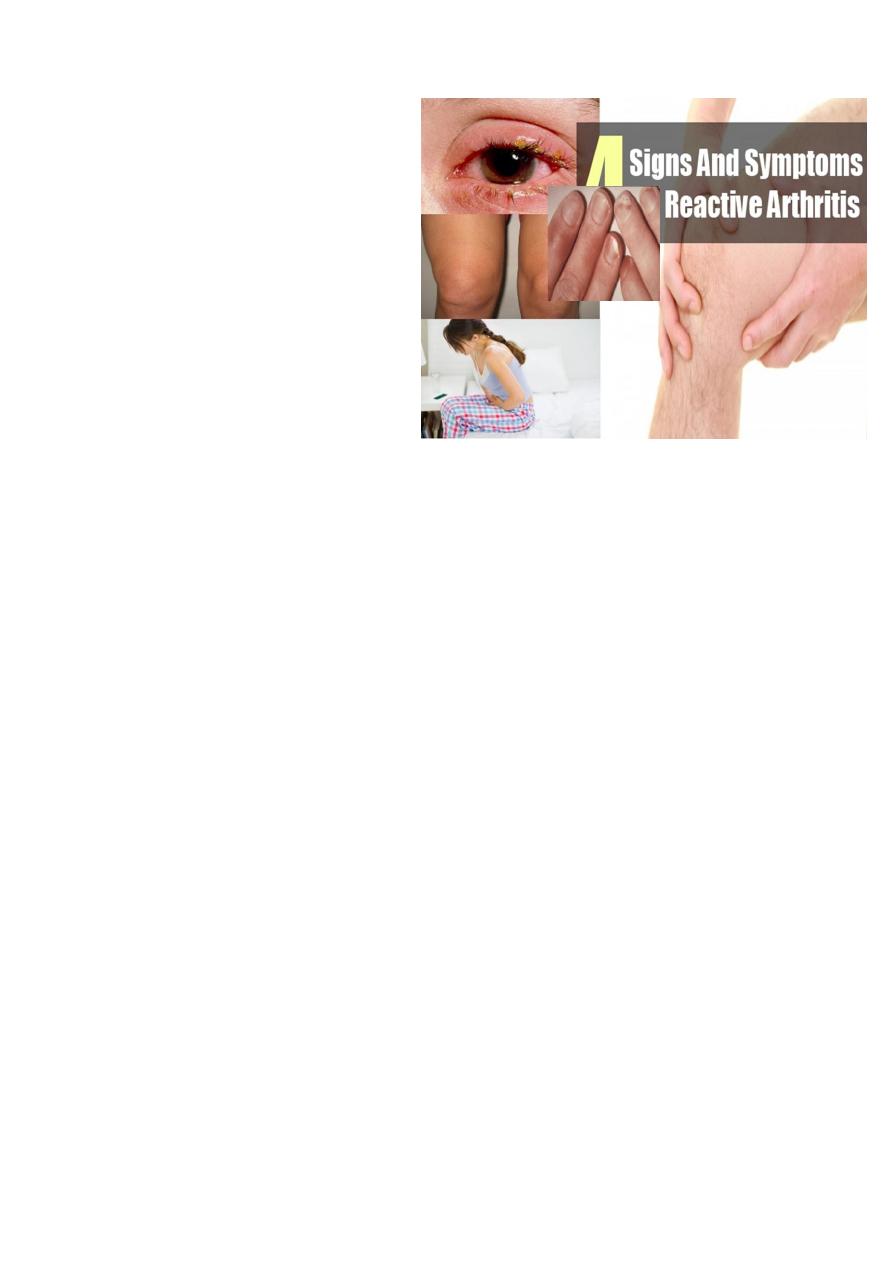
Reactive Arthritis: General Features
Non infective arthritis that follow an
extra articular infection by usually 1-
4 weeks
Yersinia, Salmonella, Shigella,
Compylobacter (GIT) & Clamydia
(genitourinary)
Recurrence of arthritis does not
need recurrence of the initiating
infection .
Epidemiology
Reactive arthritis is predominantly a disease of young men with a sex ratio of 15:1 and
is possibly the most common cause of inflammatory arthritis in men aged 16-35;
however, it may occur at any age. Between 1% and 2% of patients with non-specific
urethritis seen at clinics for sexually acquired diseases have reactive arthritis. Following
an epidemic of Shigella dysentery, 20% of HLA-B27-positive men develop reactive
arthritis.
History
The onset is typically acute, with development of urethritis, conjunctivitis (in about 50%)
and an inflammatory oligoarthritis affecting the large and small joints of the lower limbs 1-3
weeks following sexual exposure or an attack of dysentery. There may be considerable
systemic disturbance with fever, weight loss and vasomotor changes in the feet.
Reactive Arthritis: Skeletal Presentation
Asymmetric oligoarthritis in lower limbs, usually of acute onset
Acute monoarthritis, confused with septic arthritis
Sacroiliitis, can be acute & unilateral, with or without oligoarthritis
Sacrospondylitis specially in chronic or recurrent cases
Enthesitis .
6
REITER'S DISEASE
Non-specific urethritis
Conjunctivitis (∼50%)
Reactive arthritis
Reactive Arthritis: Extra articular Features
Conjunctivitis / Anterior uveitis
Mucocutanious lesions :
o Oral ulcers
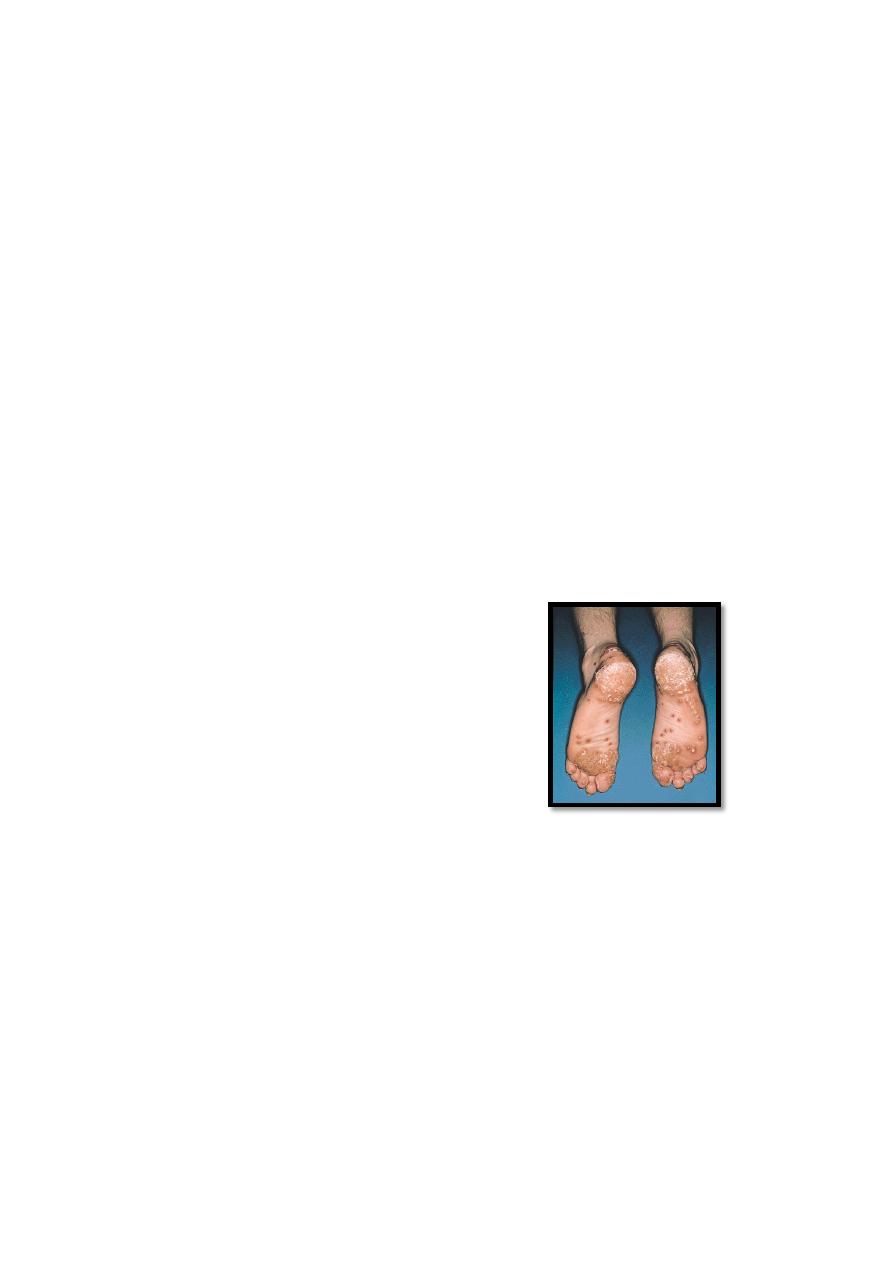
o Keratoderma blennorhagica (indistinguishable from pustular psoriasis)
o Circinate belanitis (coalescing skin erosion giving a circular pattern)
Persistance (sometimes) of the initiating infection (urethritis / cervicitis / diarrhea)
Nail dystrophy
Circinate balanitis (20-50%)
Keratoderma blennorrhagica (15%)
Nail dystrophy
Buccal erosions (10%)
Reactive Arthritis
Keratoderma blennorhagica
10-30% of cases
Can occur at other sites
Investigations
The acute phase response is usually evident from a raised ESR and CRP.
Aspirated synovial fluid is inflammatory (low viscosity, turbid) and often contains giant
macrophages (Reiter's cells).
Urethritis may be confirmed in the 'two-glass test' by demonstration of mucoid
threads in the first void specimen that clear in the second.
High vaginal swabs may reveal Chlamydia on culture.
Management
NSAIDs are helpful during the acute phase, together with judicious aspiration of joints
and intra-articular or other local corticosteroid injections.
7
Systemic steroids are rarely required. Severe progressive arthritis and intractable
keratoderma blennorrhagica occasionally warrant antirheumatic therapy with
azathioprine or methotrexate.
Non-specific chlamydial urethritis is usually treated with a short course of tetracycline.
Anterior uveitis is a medical emergency requiring topical, subconjunctival or systemic
corticosteroids
Inflammatory Bowel Disease (IBD) associated arthritis (enteropathic arthritis)
Axial Disease
A.S. like but equal sex distribution & can occur after age of 40
HLA-B27 association 50-70%
May precede IBD & has an independent course
Peripheral arthritis occur in up to 50% of cases
Psoriatic Arthritis
EPIDEMIOLOGY
Approximately 20% of all patients with seronegative polyarthritis
have psoriasis. The onset is usually between 25 and 40 years of
age, most commonly in patients with current or previous skin
psoriasis (70%) but in some cases (20%) it predates the onset of
psoriasis. A small minority of patients have synchronous onset of
skin and joint features (5%) or have arthritis but never develop
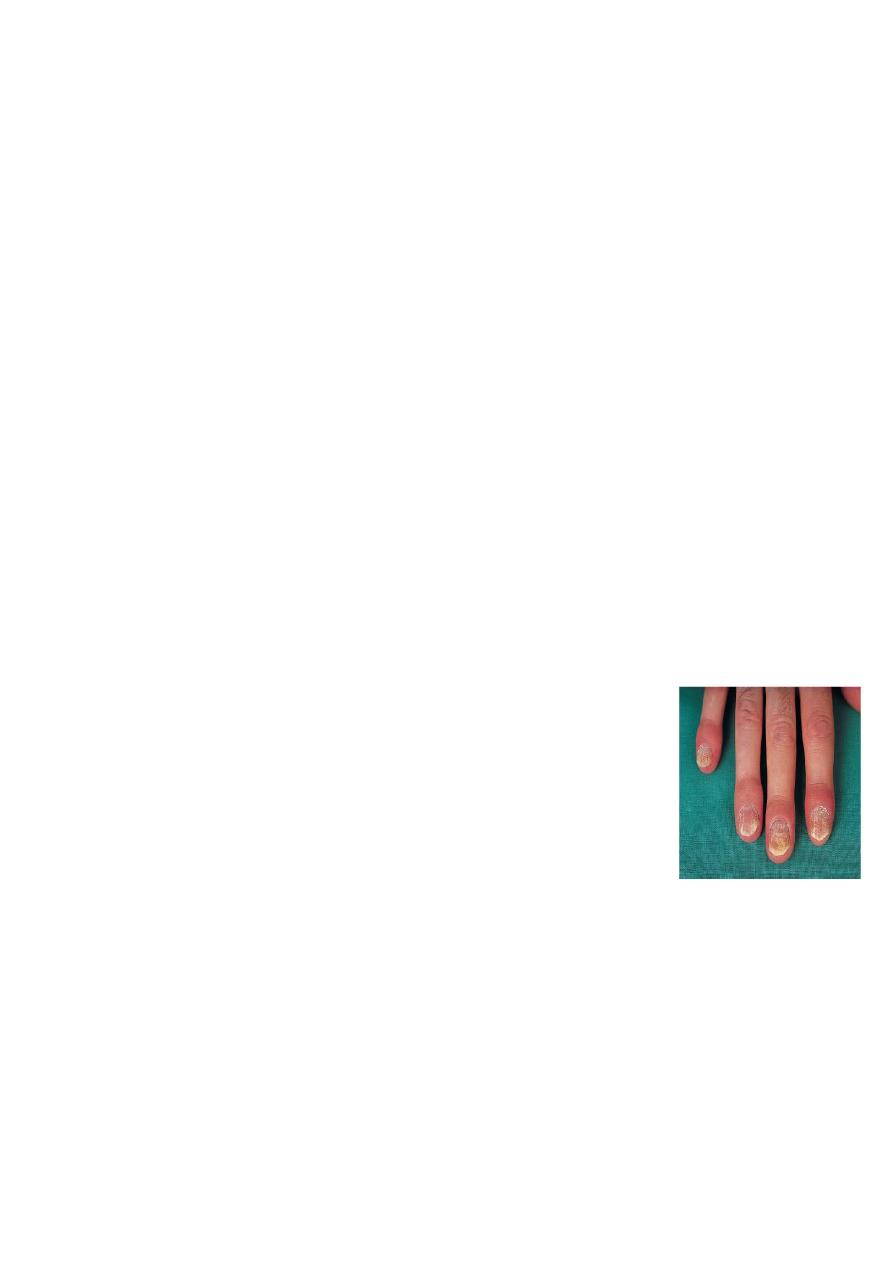
skin lesions (5%). The association with nail dystrophy is stronger
than with skin plaques.
Course of the disease
Asymmetrical inflammatory oligoarthritis (40%). This may affect lower and upper limb
joints, often with the combination of synovitis and periarticular inflammation
Symmetrical polyarthritis (25%). This predominates in women and may strongly
resemble RA, with symmetrical involvement of small and large joints in both upper and
lower limbsPredominant distal interphalangeal joint
(DIPJ) arthritis (15%). This is a very characteristic form that mainly affects men.
8
Psoriatic spondylitis (15%). This presents a similar clinical picture to ankylosing
spondylitis but tends to be less severe. It may occur alone or with any of the other
clinical patterns of peripheral arthritis.
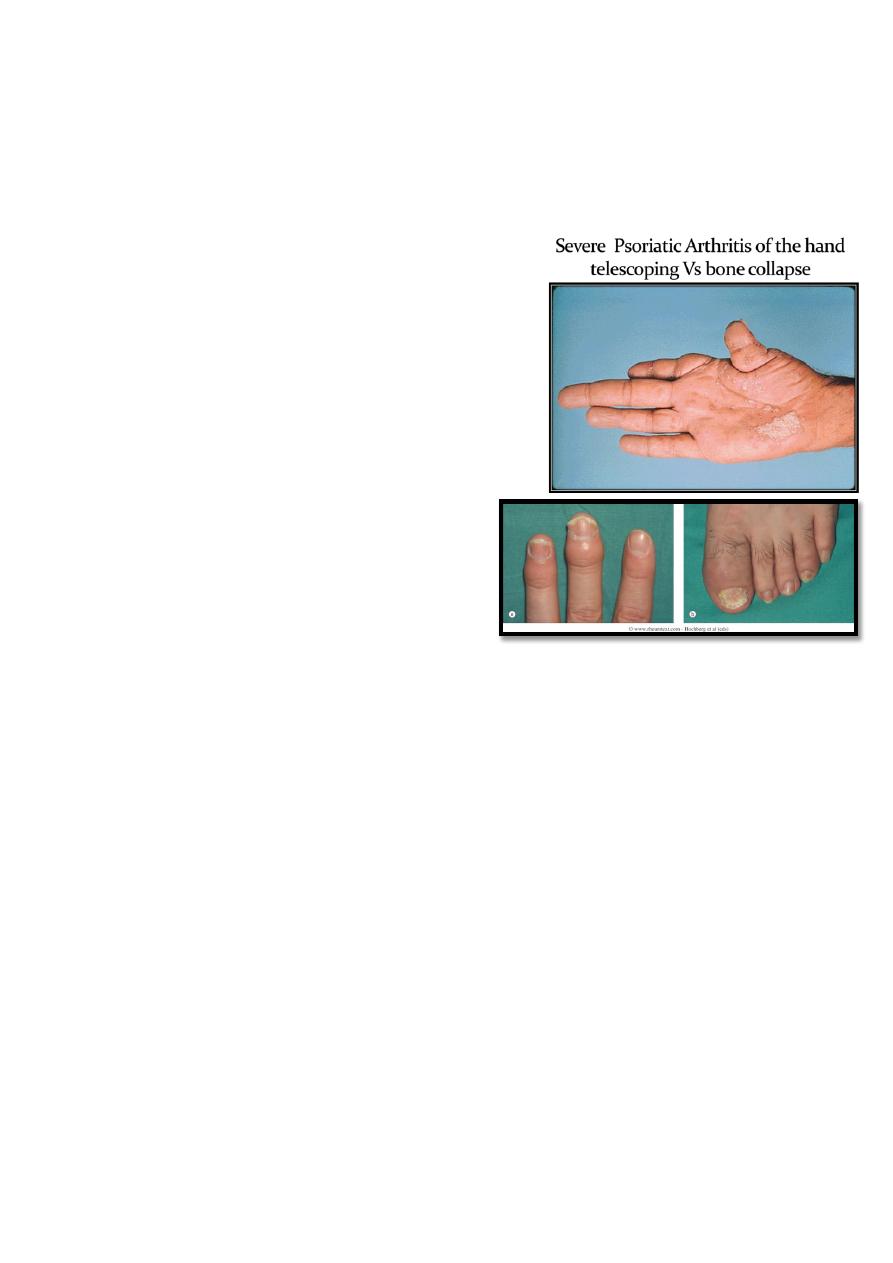
Arthritis mutilans (5%).
1. General Considration
Psoriasis affects 1-3% of population & PsA occurs
in 7-42% of psoriasis cases
May precede skin lesions (13-17% of cases)
Joint severity is independent of skin severity
Increased risk in the first degree relatives
Equal sex ratio
HLA-B27 association with axial involvement (40%)
Very Chareteristic Joint Features
DIP arthritis (erosion)
Dactylitis (sausage fingers)
Extra articular Features
Skin lesions
Nail changes :
o Pitting & onycholysis, more common in PsA (85%) than in uncomplicated psoriasis
(30%)
Eye involvement :
o Conjunctivitis
o Anterior uveitis, mostly in spondylitic cases who are B27 +ve
Investigations
The ESR and CRP may be raised, especially with polyarticular disease, but are often
unimpressive. Tests for rheumatoid factor and antinuclear antibody are generally
negative.
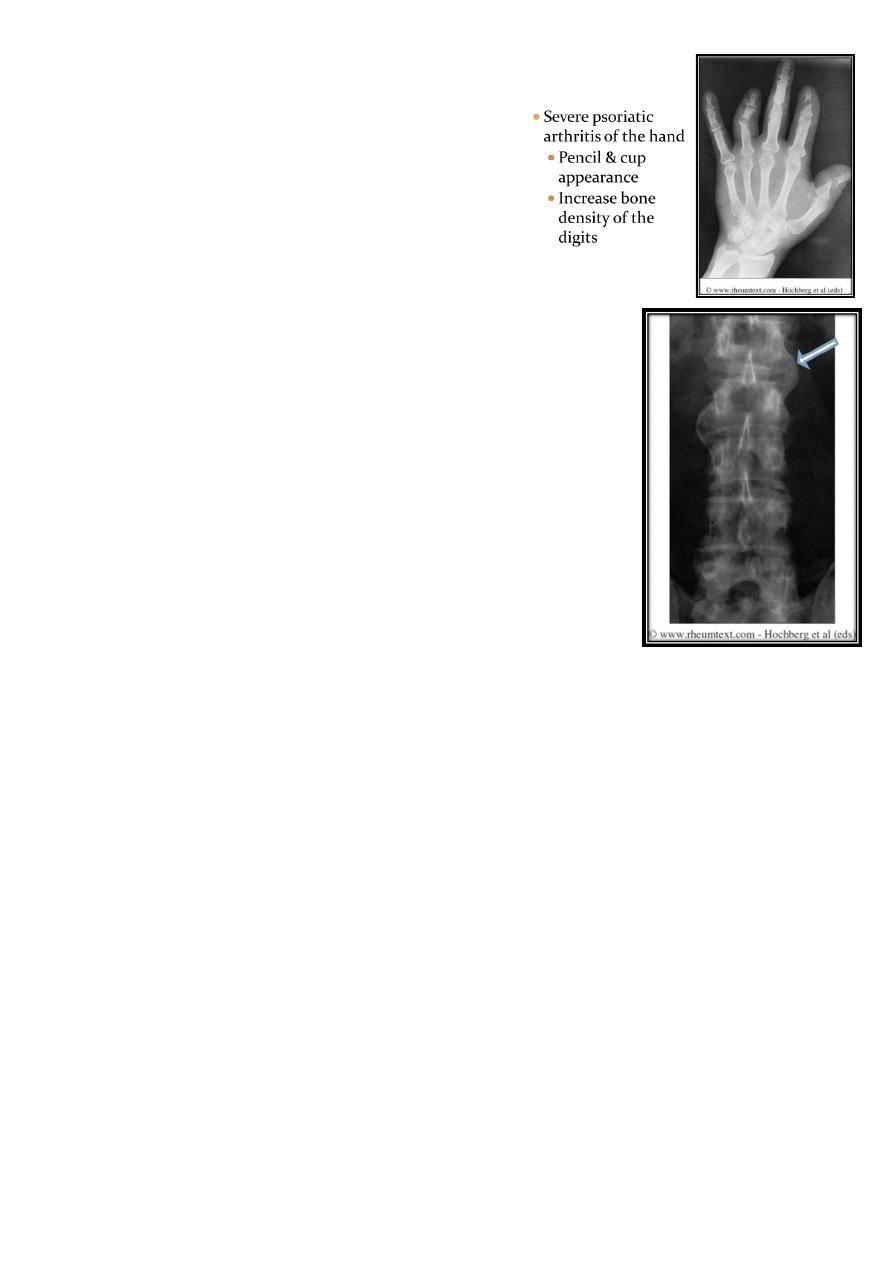
X-rays may be normal or show erosive change with joint space narrowing. Features
that permit distinction from RA include marginal proliferative erosions, retained bone
density and increased sclerosis of small bones
9
Characterstic XR Features
DIP erosions
Increased sclerosis of small bones (digits)
fluffy periostitis of large joints
Pencil-in-cup appearance of DIP joints
Course asymmetrical non marginal syndesmophytes (similar to
chronic reactive spondylitis)
Management
The prognosis is better than for RA, except in arthritis mutilans. Symptomatic agents
such as simple analgesics, and topical or oral NSAIDs are usually all that is required.
Intra-articular injections may help to control florid synovitis temporarily. In general,
splints and prolonged rest are avoided because of the increased tendency to fibrous
and bony ankylosis.
The same regime of regular exercise and attention to posture should be prescribed as
in those with spondylitis
For persistent peripheral arthritis sulfasalazine, methotrexate or azathioprine may be
required but these have little or no benefit for axial disease. Methotrexate and
azathioprine may also help severe skin psoriasis. Antimalarials should be avoided since
they can give exfoliative reactions. The retinoid acitretin is effective in treating the
arthritis as well as the skin lesions
