
Baghdad medical college
Department of surgery
Ophthalmology
Practical ophthalmology
For fifth grade students
2015-2016

History
1-Chief complaints
BURNING
.
Blepharitis, dry eye syndrome, conjunctivitis corneal defect ,episcleritis, ocular
toxicity (medication, makeup, contact lens
solutions), contact lens-related problems.
CROSSED EYES IN CHILDREN
, Esodeviations in Children (eyes turned in),
Exodeviations in Children (eyes turned out).
DECREASED VISION
See page
DISCHARGE
DOUBLE VISION (DIPLOPIA)
1. Monocular (diplopia remains when the
uninvolved eye is occluded)
--Refractive error, incorrect spectacle alignment,
--corneal opacity or irregularity(including corneal or refractive surgery),
-- iris defects (e.g., iridectomy).
--Cataract Dislocated natural lens or lens
implant,
-- macular disease, retinal detachment,
CNS causes (rare), nonphysiologic
.
2. Binocular (diplopia eliminated when either
eye is occluded)---- neuromuscular imbalance
— Typically intermittent: Myasthenia gravis,
.
— Constant: Isolated sixth, third, or fourth
nerve palsy; orbital disease

internuclear ophthalmoplegia;
vertebrobasilar artery insuffi ciency; other
CNS lesions; spectacle problem.
EYELID CRUSTING
More Common. Blepharitis, meibomitis,
conjunctivitis.
Less Common. Canaliculitis, nasolacrimal
duct obstruction, dacryocystitis.
EYELIDS DROOPING (PTOSIS)
EYELID TWITCH
--Orbicularis myokymia (related to fatigue,
excess caffeine, medication, or stress)
--cornealor conjunctival irritation (especially from an
eyelash, cyst, or conjunctival foreign body),
--dry eye,
-- blepharospasm (bilateral), hemifacial
spasm
EYES “BULGING” (PROPTOSIS)
1. Infl ammatory: Thyroid eye disease (TED),
idiopathic orbital infl ammatory syndrome
(IOIS), sarcoidosis, Wegener granulomatosis,
etc.
2. Infectious: Orbital cellulitis, subperiosteal
abscess, etc.
3. Neoplastic (benign and malignant): Dermoid
cyst, capillary hemangioma, rhabdomyosarcoma,
metastasis, lymphangioma,
optic nerve glioma, neurofi broma, leukemia,
lymphoproliferation (including lymphoma),
neurilemmoma, mucocele, etc.
4. Trauma: Orbital fracture, retrobulbar hemorrhage,
orbital foreign body, carotidcavernous
fi stula, etc.
5. Malformation: Congenital, vascular, etc.
.

FLASHES OF LIGHT
More Common. Retinal break or detachment,
posterior vitreous detachment,
migraine, rapid eye movements (particularly
in darkness), oculodigital stimulation.
Less Common. CNS (particularly occipital
lobe) disorders, vestibulobasilar artery insuffi
ciency, optic neuropathies, retinitis, entoptic
phenomena, hallucinations.
FLOATERS
ITCHY EYES
Conjunctivitis (especially allergic, vernal, and
viral),
blepharitis
dry-eye syndrome,
topical
drug allergy
LIGHT SENSITIVITY (PHOTOPHOBIA)
1. Abnormal eye examination
More Common. Corneal abnormality (e.g.,
abrasion or edema), anterior uveitis.
Less Common. Conjunctivitis (mild photophobia),
posterior uveitis, scleritis, albinism
total color blindness, aniridia, mydriasis of any
etiology (e.g., pharmacologic, traumatic), congenital
glaucoma.
2. Normal eye examination: Migraine, meningitis,
retrobulbar optic neuritis, subarachnoid
hemorrhage, trigeminal neuralgia, or
a lightly pigmented eye.
NIGHT BLINDNESS
More Common. Refractive error (especially
undercorrected myopia), advanced glaucoma
or optic atrophy, small pupil (especially from
miotic drops), retinitis pigmentosa, congenital
stationary night blindness, status-post
panretinal photocoagulation drugs (e.g., phenothiazines,
chloroquine, quinine).
Less Common. Vitamin A defi ciency, gyrate
atrophy, choroideremia.
PAIN
1. Ocular:
-- Dry-eye syndrome, blepharitis,
--Infectious conjunctivitis, episcleritis, scleritis infl amed pinguecula or pterygium,
--foreign body
--corneal disorder
--eye strain from uncorrected refractive error.
--Angle closure glaucoma
2. Periorbital :
--Inflammation: hordeolum, preseptal
cellulitis, dacryocystitis, dermatitis (e.g.,
contact, chemical, varicella zoster, or herpes
simplex),
--Referred pain (e.g., dental, sinus),
.
3. Orbital:
--Sinusitis ,
-- orbital cellulitis,
idiopathic orbital infl ammatory syndrome
orbital tumor or mass, optic neuritis, acute
dacryoadenitis,
--migraine or cluster headache,
diabetic cranial nerve palsy.
4. Asthenopia: Uncorrected refractive error, phoria
or tropia, convergence insuffi ciency,
RED EYE
See page
“SPOTS” IN FRONT OF THE EYES
1. Transient: Migraine.
2. Permanent or long-standing
. Posterior vitreous detachment,
intermediate or posterior uveitis, vitreous
hemorrhage, vitreous condensations/debris.
TEARING
1. Adults

Lacrimation —emotional states ,Corneal abnormality
(e.g., abrasion, foreign body or rust ring,
recurrent erosion, edema), anterior uveitis,…..etc
--nasolacrimal duct obstruction,
punctal occlusion, lacrimal sac mass,
--pump failure(congenital or seventh nerve palsy).
2. Children:
Ophthalmia neonatorum
Nasolacrimal duct obstruction
congenital glaucoma,
2-Past ocular history
: Ask about
-use of glasses or contact lens
-previous ocular diseases
-chronic ocular disease
-previous eye surgery ,laser treatment
3-Past medical history
-
systemic diseases having ocular manifestation
Diabetes(cataract, diabetic retinopathy)
Hypertension(hypertensive retinopathy)
Autoimmune diseases
(Dry eyes,Episcleritis,Scleritis,Corneal ulcers,Uveitis)
Thyroid disorders
Soft tissue involvement(lid sewlling conjunctival hyperemia…)
Lid reraction
Exophthalmos (proptosis)
Extraocular muscle dysfunction
Optic nerve dysfunction
-
systemic diseases contraindicate drug treatment
Lung disease for beta blocker
Kidney disease for Carbonic anhydrase inhibitors
4-Family history
: importnant to ask for a positive family history especially in
Corneal diseases(keratoconus corneal dystrophies)
Glaucoma cataract squint retinal diseases
5-Drug history
: Ask about current and prior ocular drugs

Green—miotics
Red---mydriatics
Yellow or blue---beta blocker
Orange---CA inhibitors
Gray---NSAIDs
Tan---Anti-infective
Pink—steroid
Purple—adrenergic agonist
Turquoise---PG analogue
Physical examination
1-VA and refraction
2-Pupil examination
*controlled by
Sphincter muscle—parasympathetic
Dilator muscle ------ sympathetic
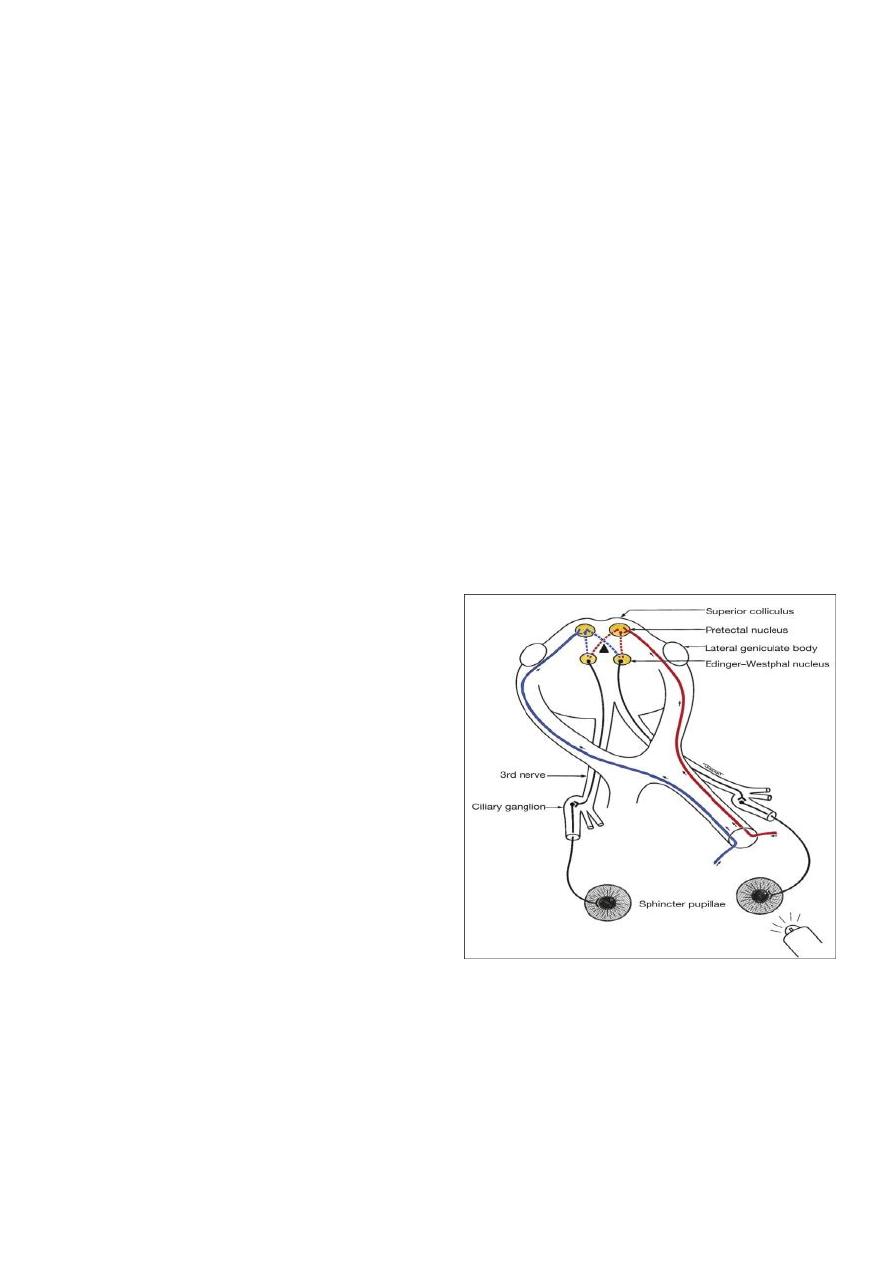
*Afferent Pathway of the Pupil Light
Reflex
Axons from retinal ganglion cells (input)
↓
Optic nerve → Optic chiasm → Optic tract
↙
Edinger-Westphal ← Pretectal nucleus
nucleus
*
Purpose::To examine the afferent and efferent neurological pathways responsible for pupillary function
*Procedure:: consists of four steps
Observation (screen for anisocoria)
Direct and consensual response
Swinging flashlight test
Near reflex test
The first three steps should be performed on every patient
The last step should be done when a relative afferent pupillary defect (RAPD) is found in the third step
Afferent Pupillary Defect
Absolute Afferent Pupillary Defect (amaurotic pupil)
• Complete optic n. lesion
• No light perception
• Both pupils are equal in size
• When the affected eye is stimulated by light neither pupils react
• When the normal eye is stimulated both pupils react normally
• The near reflex is normal in both eyes
Relative Afferent Pupillary Defect (RAPD)- Marcus Gunn Pupil
• Incomplete optic n. lesion or severe retinal disease
• Never caused by a dense cataract
• The difference in pupillary reaction between the two eyes is highlighted by ‘Swinging Flashlight Test’
Near reflex
• Convergence
• Accommodation
• Miosis
• Instruct the patient to look at the distant target
• The examiner holds up a target containing fine detail approximately 25cm from the patient
• Ask the patient to fixate the near target and look for pupil constriction
• Note the speed of the constriction and the roundness of each pupil
Light-Near Dissociation
Unilateral
• Afferent Conduction defect
• Adie Pupil
Bilateral
• Neurosyphilis
• Encephalitis
• Chronic Alcoholism
Efferent Pupillary Defect>>>>Anisocoria
Causes of anisocoria
• Physiological anisocoria (20% of population have inequality of pupil size but it is usually < 1mm difference)
• Sympathetic tract lesion (Horner’s syndrome)
• Parasympathetic tract lesion (oculomotor n. palsy, Adie’s pupil)
• Argyl Robertson syndrome
• Pharmacological
• Iris damage (traumatic mydriasis, iritis, angle closure glaucoma, siderosis

• Anisocoria in light: parasympathetic problem
– Cranial nerve III defect
– intracranial pressure
– drug-induced mydriasis
– Adie’s pupil
– iris damage
– simple anisocoria
• Anisocoria in dark: sympathetic problem
– Horner’s syndrome
– simple anisocoria
Oculomotor Nerve Palsy
s
causes
:
Medical (pupil sparing)
• Hypertension
• Diabetes
Surgical (pupillary involvement)
• Aneurysm
• Trauma
• Uncal herniation
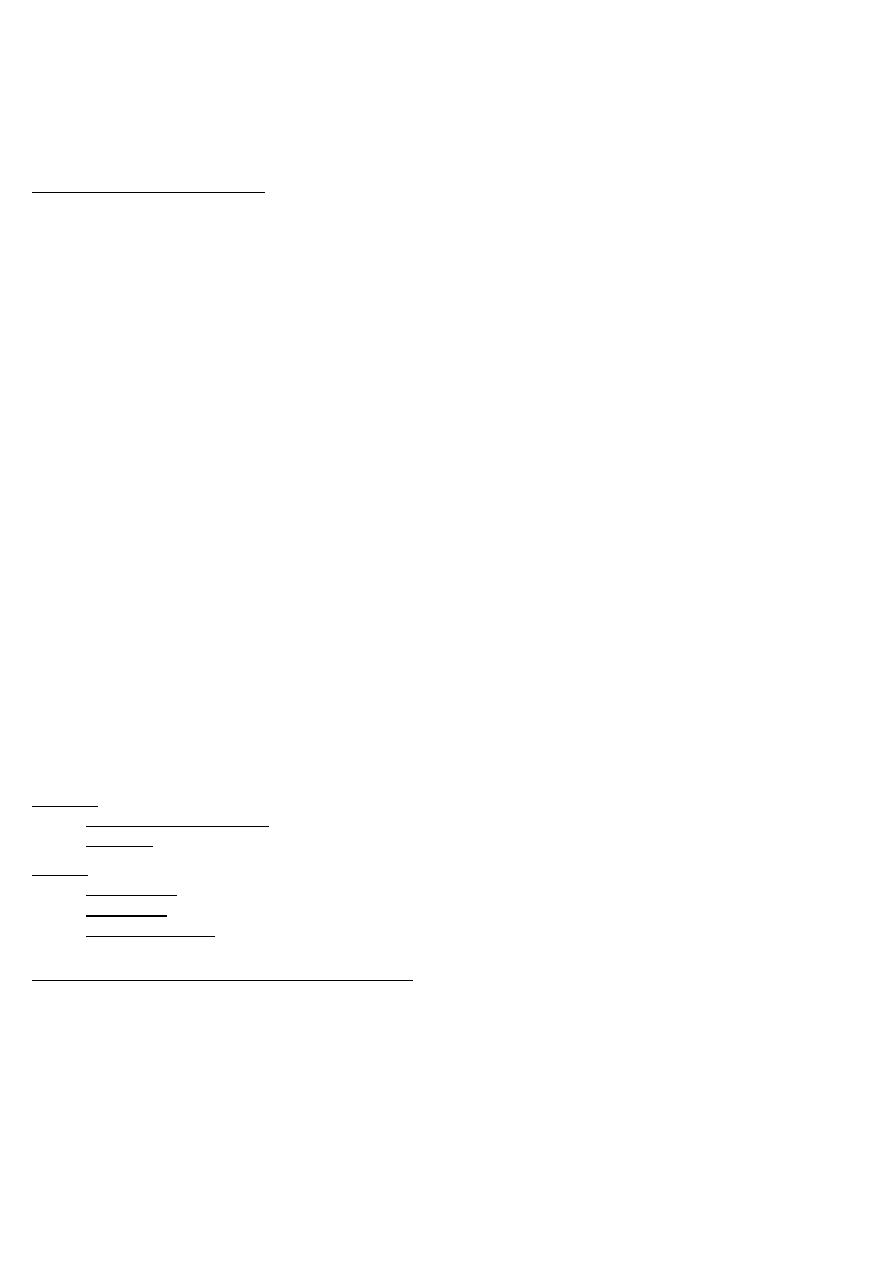
3-Visual Field assessment
1- Confrontation test: subjective, for detecting of peripheral visual field defects
2- Kinetic Method: Goldman’s perimetry ( Kinetic because a target with fixed
illumination is continuously moved until it is no longer seen) mainly for peripheral
field defects like Bitemporal hemianopia, homonymous hemianopia
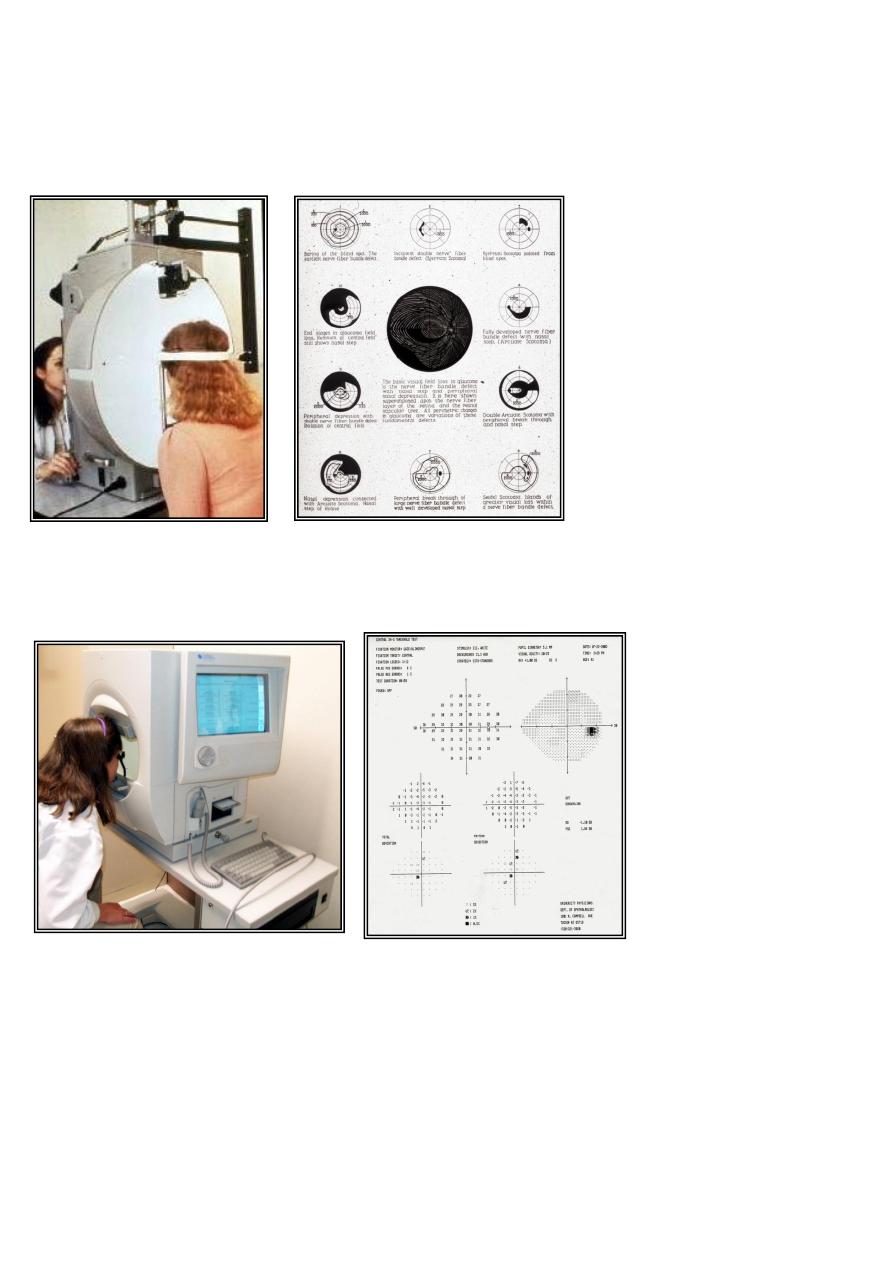
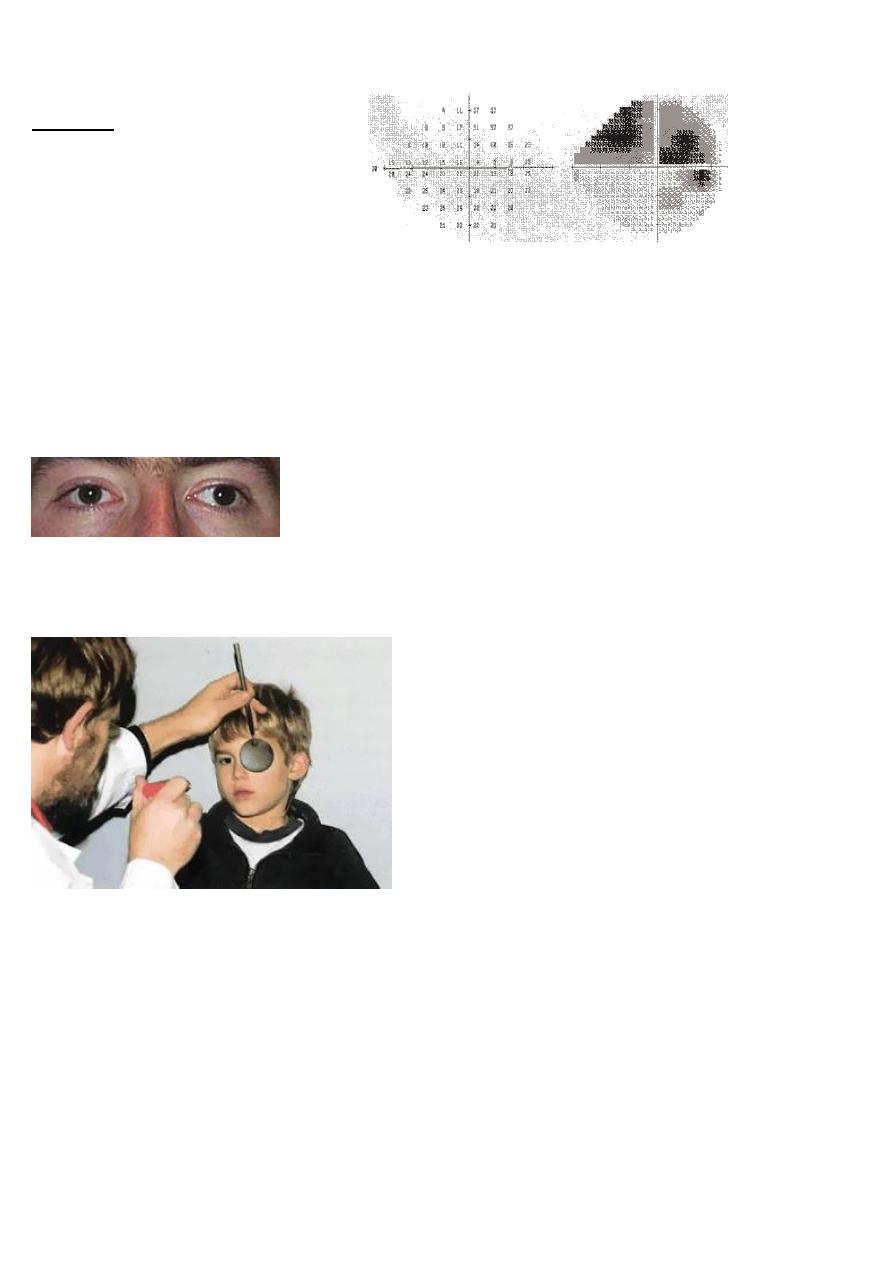
3- Static: Humphrey Field Analyser (the target is not moving but its illumination
intensity is changed until it is no longer seen) mainly to detect central visual field
defects for e.g. in Glaucoma and Optic nerve diseases
Scotoma visual loss in an area.
*Absolute no vision
*Relative loss of vision (depressed)
4- motility and alignment tests
a-
Hirschberg test
Shine penlight into eyes from 30 cm –corneal light reflex should be in the center and similar in both eyes
b-Cover test
Place a target 30 cm from the patient's eyes for fixation and cover one eye.. observe the movement for fixation in the
non-covered eye ---this test confirm the presence of manifest squint(-tropia) and detect its type:
--eye moves outward to refixate—esotropia
---eye moves inward to refixate--- exotropia
---eyes move up to refixate---hypotropia
---eyes move down to refixate—hypertropia
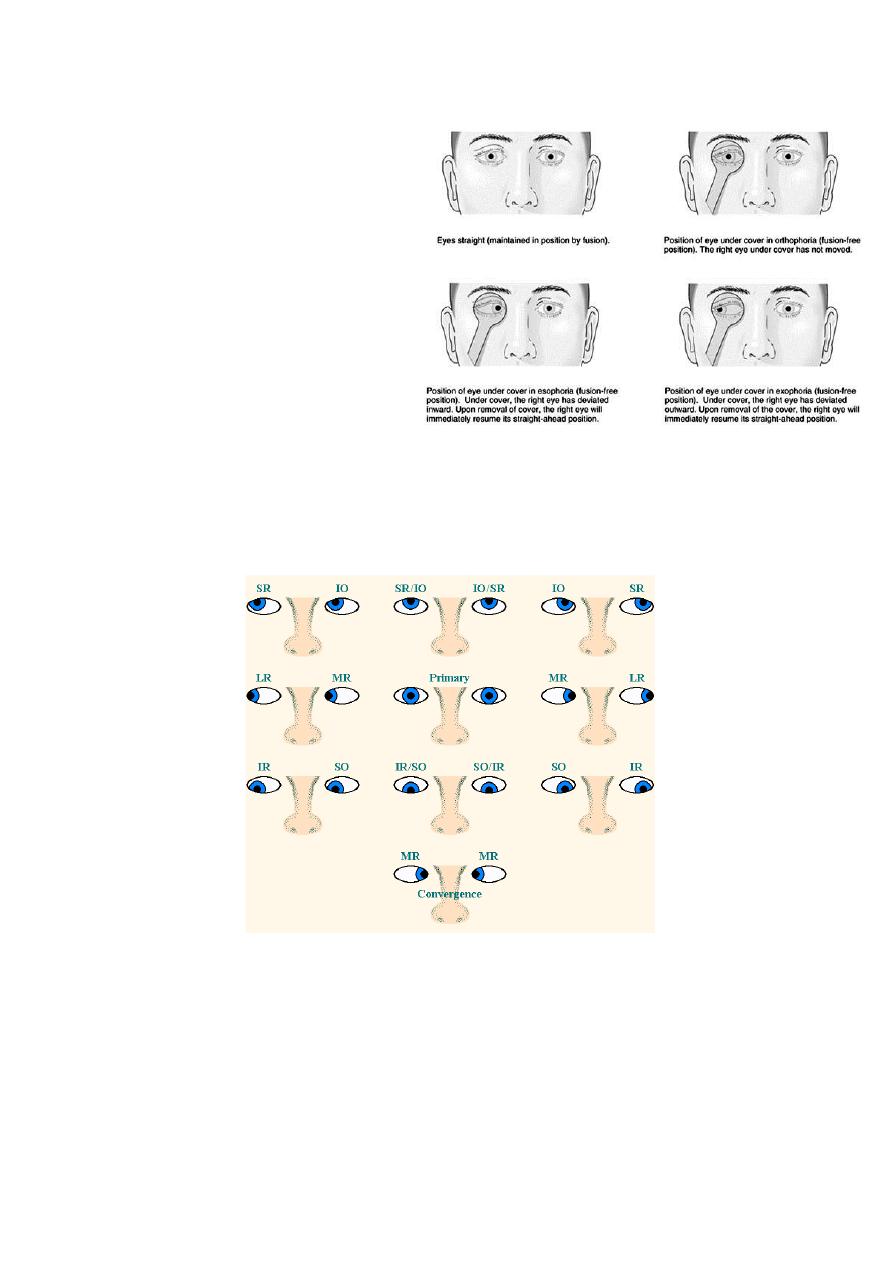
c-Cover uncover test
place a target infront of the patient eyes for fixation
cover one eye and uncover it and observe the
movement of the eye under the cover
this test detect the presence of latent squint(-phoria)
and determine its type
--eye move outward on removing the cover—esophoria
-- eye move inward on removing the cover--exophoria
--eye move up on removing the cover--- hypophoria
--eye move down on removing the cover-----hperphoria
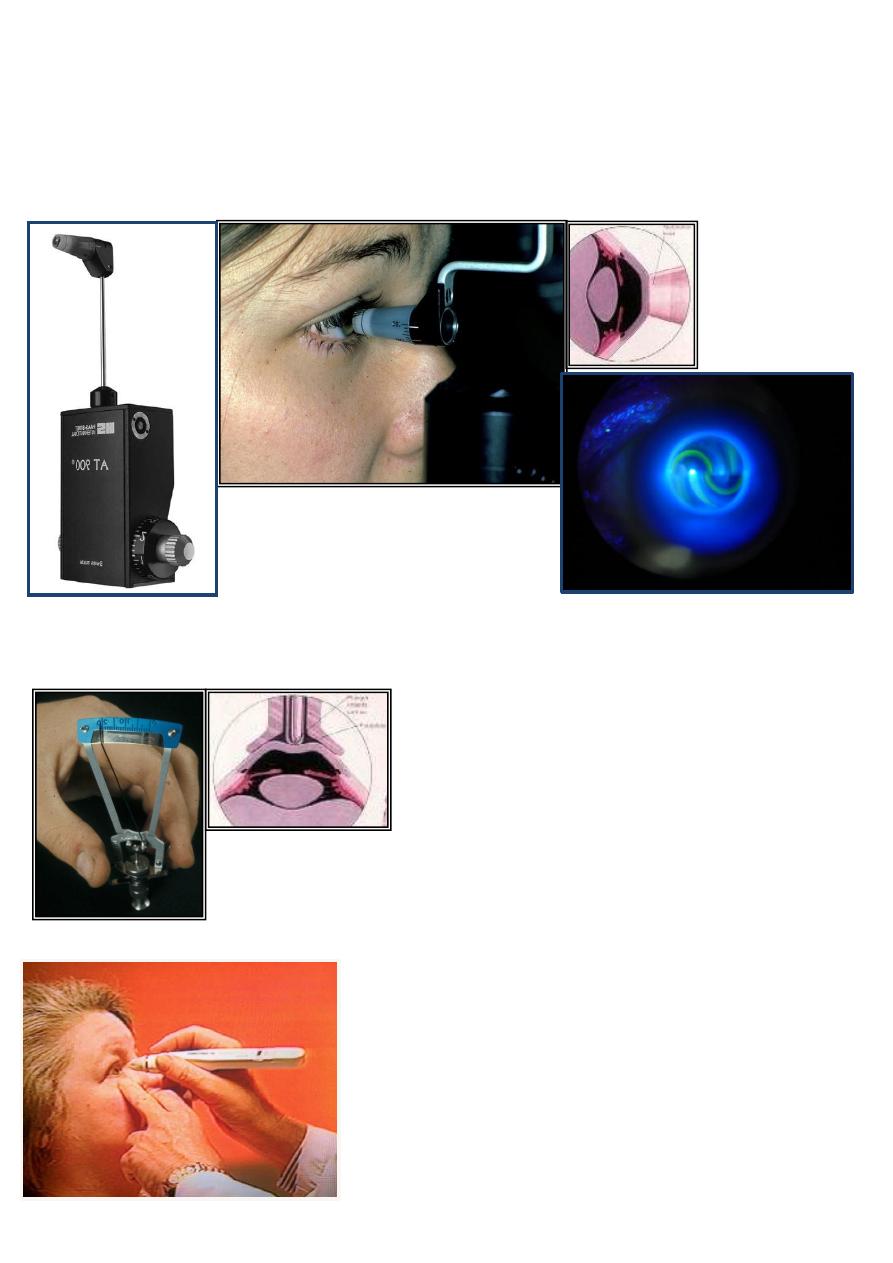
d-Ocular motility test
--Examine the six cardinal position
--notice the presence of ophthalmoplegia,diplopia,nystagmus
5- Intraocular pressure measurement
**Applanation method
1-
Goldman’s Applanation tonometry : incorporated with the slit-lamp, the most
accurate method
**Indentation method
1-Shiotz method
2-Tonopen
2-
Tonopen

**Air puff tonometer: rapid screening technique
**Crude method by digital palpation
Normal range: 10-21 mm Hg
Diurnal flucuation normally < 6 mmHg
Women have slightly higher pressures
Normal central corneal thickness: 545 – 550 u
Add or subtract 0.6 mmHg for each 10 u change in central corneal thickness
6-External Ocular examination
**
Inspect the orbit for exo/enophthalmos
**inspect the four L's
Lid:sign of inflammation ,chalazion, ptosis, entro/ectropion
Lashes: trichiasis, madarosis, poliosis
Lacrimal apparatus: Dacryoadenitis,Dacryocystits
Lymph nodes:preauricular, submandibular
7-Anterior segment examination
By slit lamp
Basic Design :
1. Mechanical system
2. Illumination system
3. Biomicroscope /0bservation system
Associated instruments:
Applanation Tonometer/ Gonioscopic Lens/ Fundoscopy Lens/Micrometer Eyepieces/ Image archiving device/Laser delivery system
Mechanical system
:
Basic 3 parts :
1. Motorized table (Base)
2. Patient positioning frame
3. Joystick
It concern with :
Positioning & adjustment of patient and observer
system together with joystick
Providing base to other parts
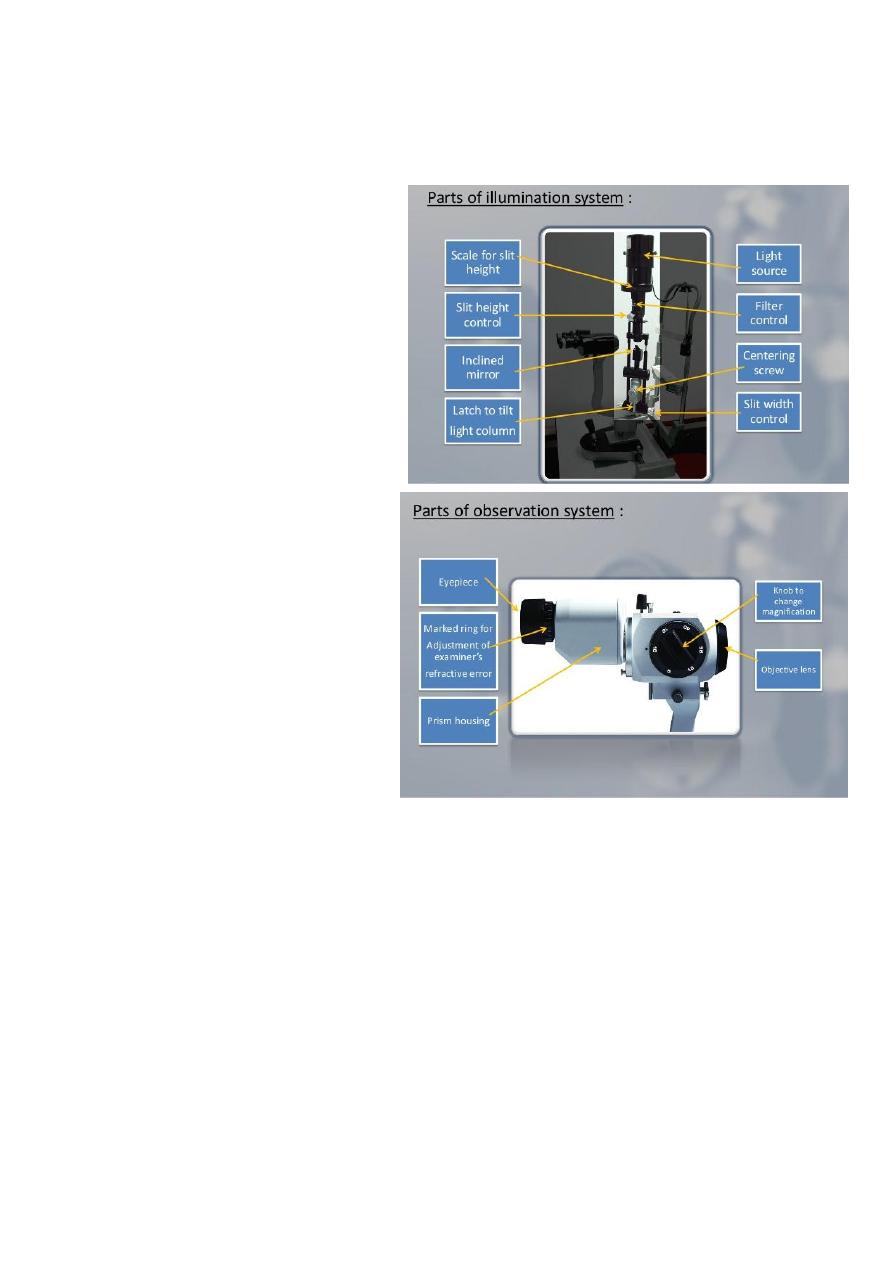
Illumination system :
Provides a bright, evenly illuminated, finely focused, adjustable slit of light at the eye.
Contains the following components:
- Light source
-Condenser lens system
-Slit and other diaphragms
- Filters
-Projection lens
-Reflecting mirror or prisms
Observation part::
-eyepiece
-prism housing
-knobe to change magnification
-objective lens
Examine the following:
Lid and lashes
Conjunctiva:
For conjunctival reactions chemosis membrane
Pterygium pinguecula concretions
sclera
For redness ,nodule ,discoloration
-episcleritis
scleritis
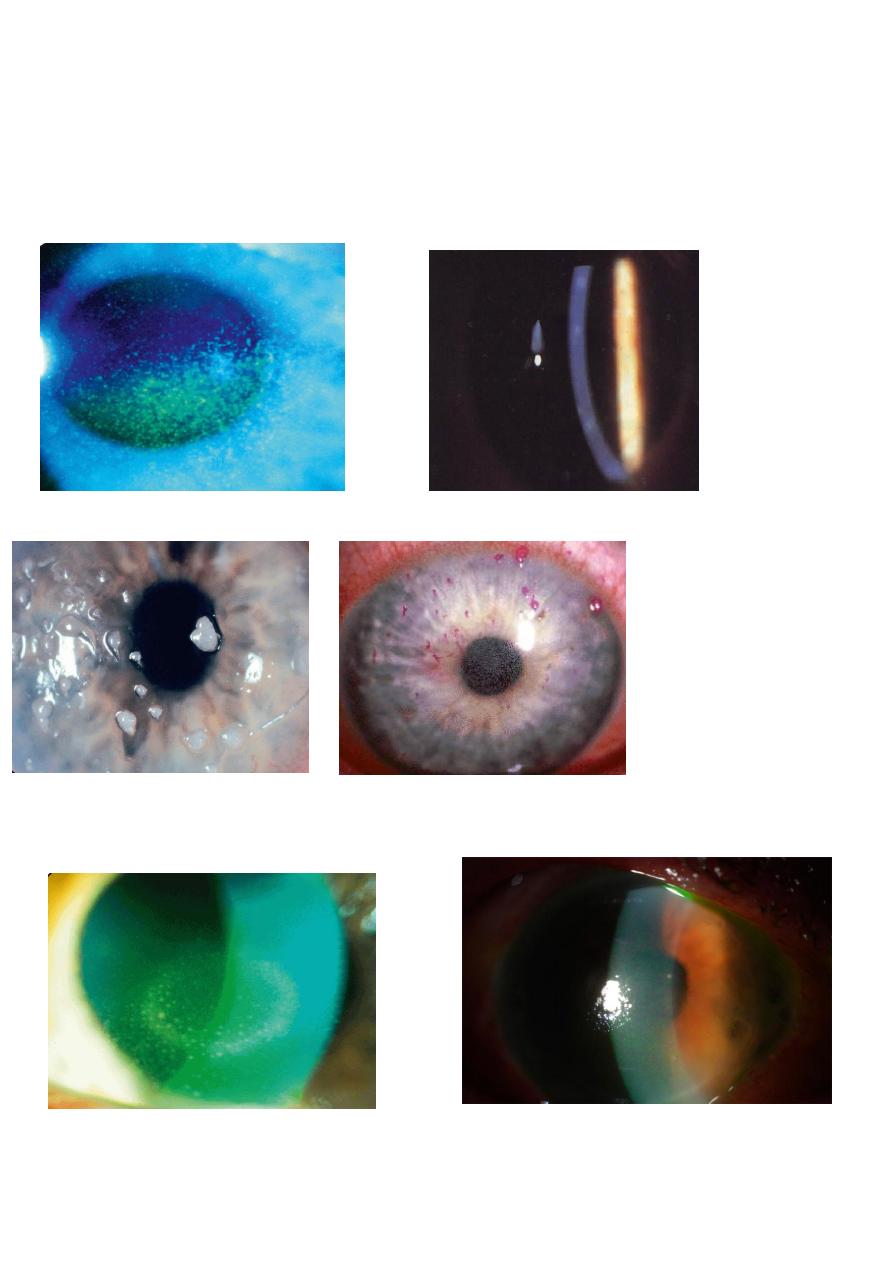
Cornea:
can use
fluorescein stain with cobalt-blue filter for depothelialized cornea
Rose Bengal stain for devitalized cornea
1-Epithelial signs:
a-Punctate epithelial erosions(PEE) b- Punctate epithelial keratitis (PEK):
Filaments:
e- Pannus:
3-
Stromal signs
a-
Stromal infiltration:
b-Stromal oedema
:
b- Vascularization:
3- Descemet's membrane signs:
a- Breaks:
b- Folds (Striate keratopathy):
Anterior chamber: Examine for
Blood(hyphema) pus(hypopyon)
Iris
Cells(AC reaction) Depth

Lens: Examine for
Opacity(Cataract
)
Ectopia lentis Intraocular lens
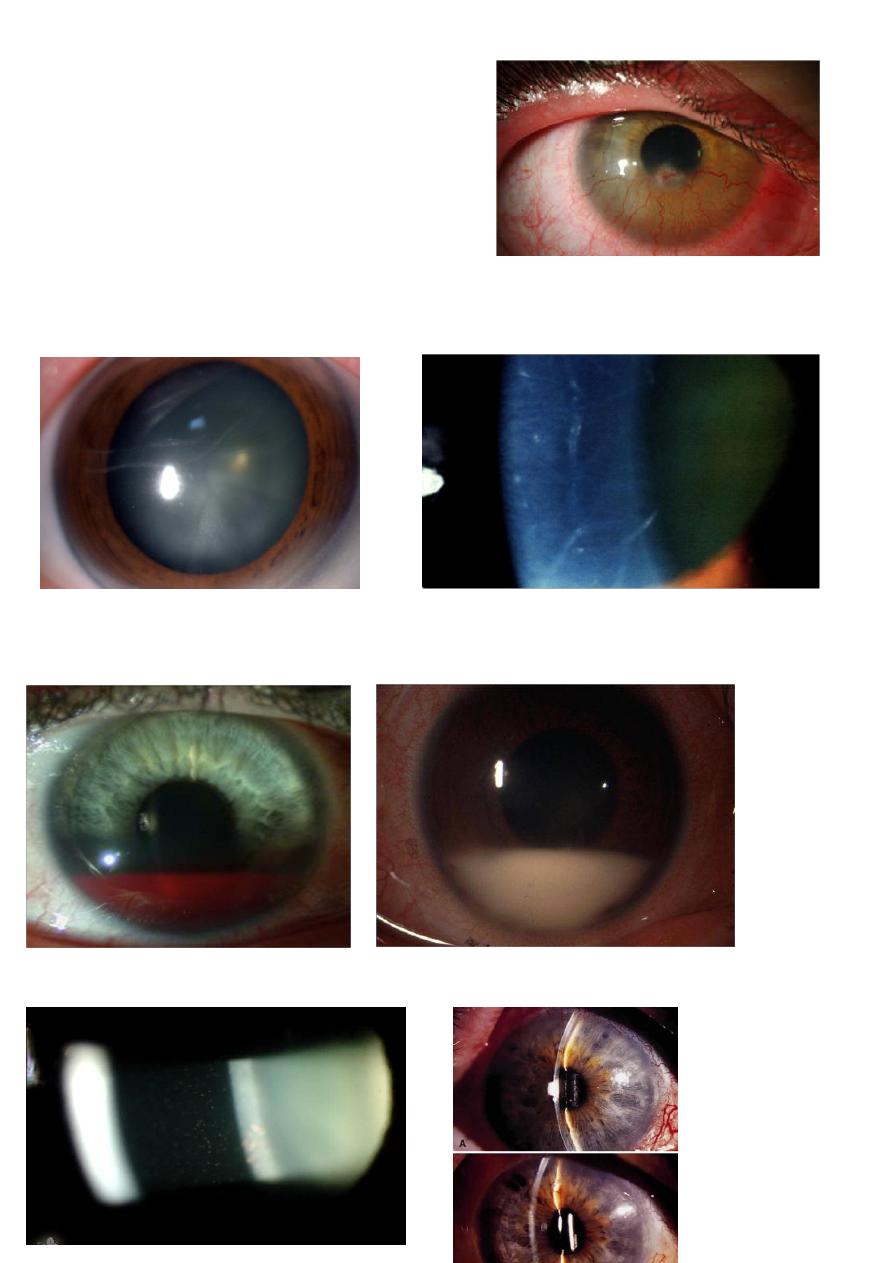
8-Fundoscopy/Ophthalmoscopy
1- Direct Ophthalmoscope
This instrument provides a quick means for
fundal examination especially the optic disc.
It characterised by the following
o Magnified view of the fundus about 15 times
o Limited field, only 6 degrees
o Image formed is erect
o Can be affected by refractive errors of the patient
o Monocular no stereopsis ( 3D image)
2- Indirect Ophthalmoscope:
It is composed of head mounted light source and a
condensing lens of either 20 or 30 dioptric power
in front of the eye being examined.
Thus forming a real image between the condensing
lens and the observer.

Indirect Ophthalmoscope has the following features:
o Magnification is less than that obtained with the direct ophthalmoscope ( 3-5
times only)
o The field is larger about 25 degree
o Image is inverted and laterally reversed
o The image is little affected by refractive errors
o Binocular vision ( stereoscopic view)
3- Slit lamp
a-with condensing lens
Slit lamp can also be used to examine the posterior segment (vitreous and retina)
with the use of high power condensing lens; 66, 78 and 90 dioptric power. It is
mainly to examine the central 30 degrees.
b-For examining the peripheral retina we should use a special lens called 3-mirrors
lens
c-Hruby lens(-58 diopter_
d-Panfundoscopic lens
4-Fundus camera with or without fluorescein angiography
5-ultrasound scan(A-scan/B-scan)
6-physioelectrical test
a-ERG
b-EOG
c-VEP
Examine for
Optic disc
C/D ratio
Disc margin and color (Optic disc swelling)
Macula
Exudative maculopathy Drusen(AMD) Macular hole
RED EYES
History
Is the vision affected ?
Unilateral or bilateral ?
Painful or painless ?
Associated signs and symptoms ?
Examination:
1- Check visual acuity (VA)
2- Check pupillary reflexes
3- Check IOP (intraocular pressure)
4- Slit lamp examination
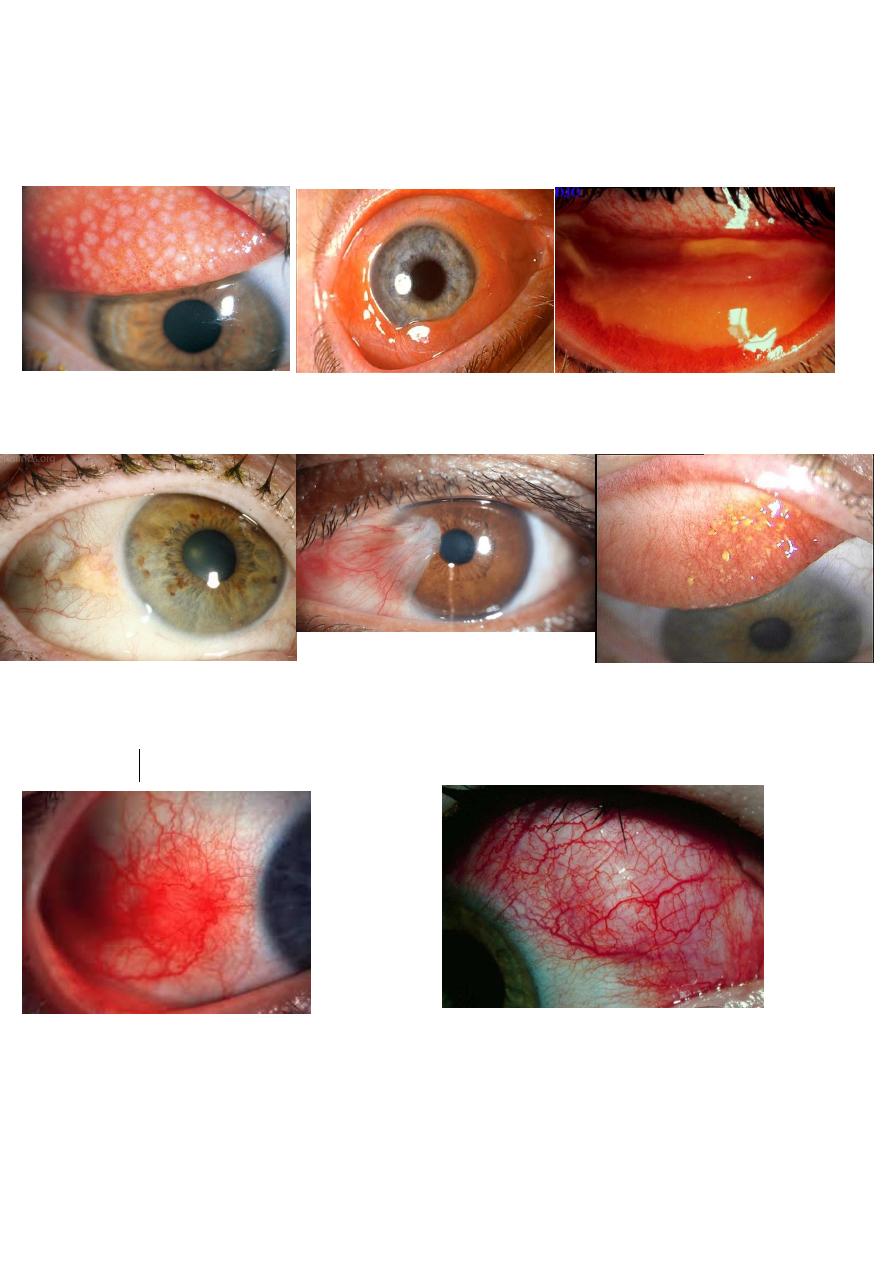
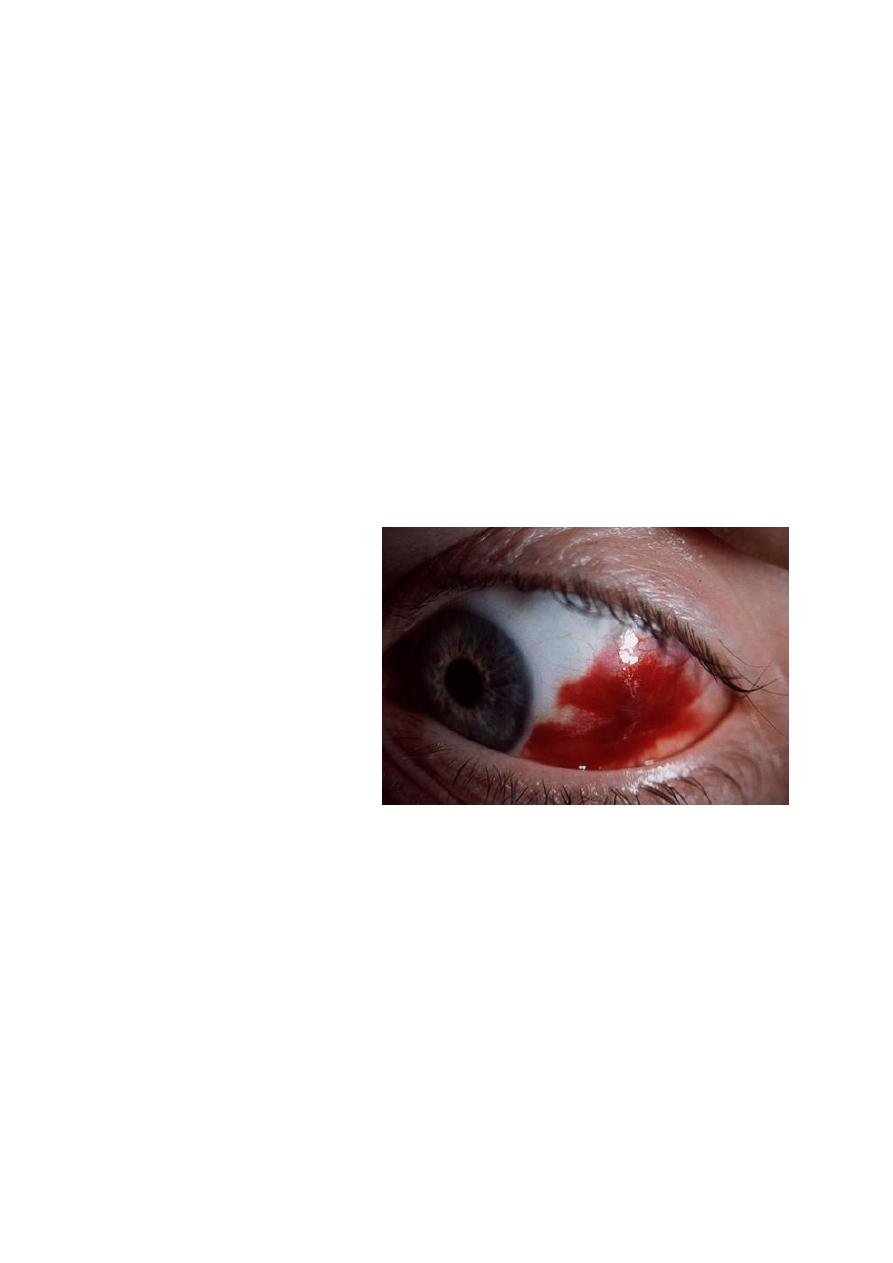
**Red Eye with normal/ near normal vision
a-Painless
Subconjunctival Haemorrhage
b-Red Eye with pain or discomfort
1- Conjunctivitis
2- Episcleritis
3- Scleritis
4- Uveitis
1- Allergic Conjunctivitis:
-Bilateral, itchy and burning sensation, watery or mucoid discharge.
Vision is usually normal
-On Slit lamp papillary reaction is seen on the palpebral conjunctiva.
-Treatment
Artificial tears
Topical Antihistamine
Topical steroids for severe cases
2- Bacterial Conjunctivitis:
-Unilateral then may become bilateral, purulent discharge, foreign body sensation
Vision is normal and papillary reaction can be seen.
-Treated with topical antibiotic
3- Adenoviral Keratoconjunctivitis
-Might be preceded by a history of upper respiratory tract infection
Unilateral then bilateral, foreign body sensation, watery discharge, eyelid oedema
with conjunctiva hyperemia and chemosis.
Vision is normal unless the cornea is involved. Slit lamp examination shows follicular
reaction
Tender preauricular lymph adenopathy
-Treatment: Self-limited, Artificial tear and precautions should be taken to avoid viral
transmission ( Highly Contagious)
Red Eye with impaired vision
>>>>Either with normal IOP:
1- Corneal abrasion/ulcer
2- Keratitis
3- Anterior uveitis
4- Endophthalmitis
Corneal ulcer
•
Infection
–
Bacterial: Adnexal infection, lid malposition, dry eye, CL
–
Viral: HSV, HZO
–
Fungal:
–
Protozoan: Acanthamoeba in CL wearer
•
Mechanical or trauma
•
Chemical: Alkali injuries are worse than acid
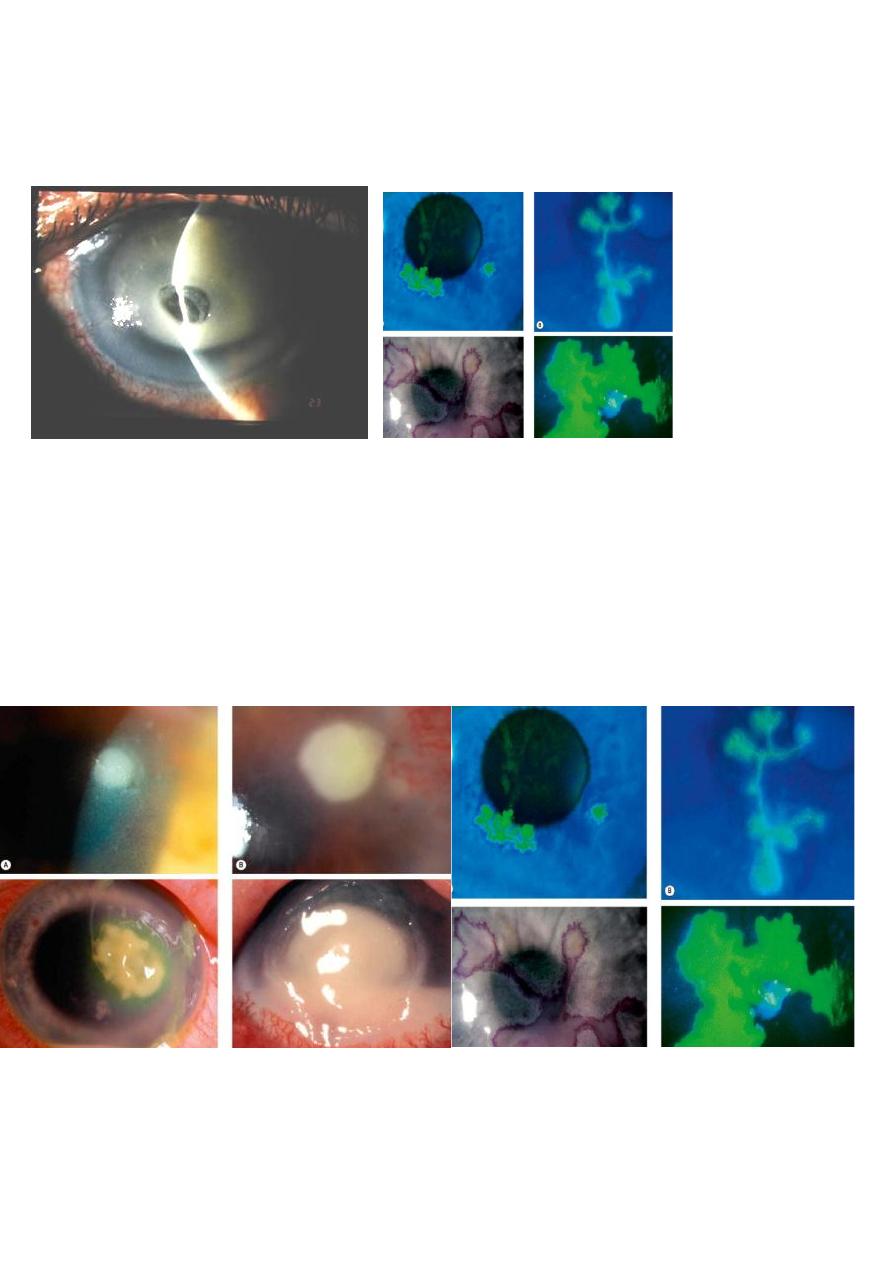
B) Microbial Keratitis
History of contact lens wearing ,trauma, immunocompromised patients
Blurred vision, severe pain, watery then purulent discharge
Special stains like sodium fluorescine strip can be used during slit lamp
examination to visualise the ulcer.
Treatment involves admission of the patient, corneal scrapping for culture and
sensitivity and hourly administration of concentrated topical antibiotics
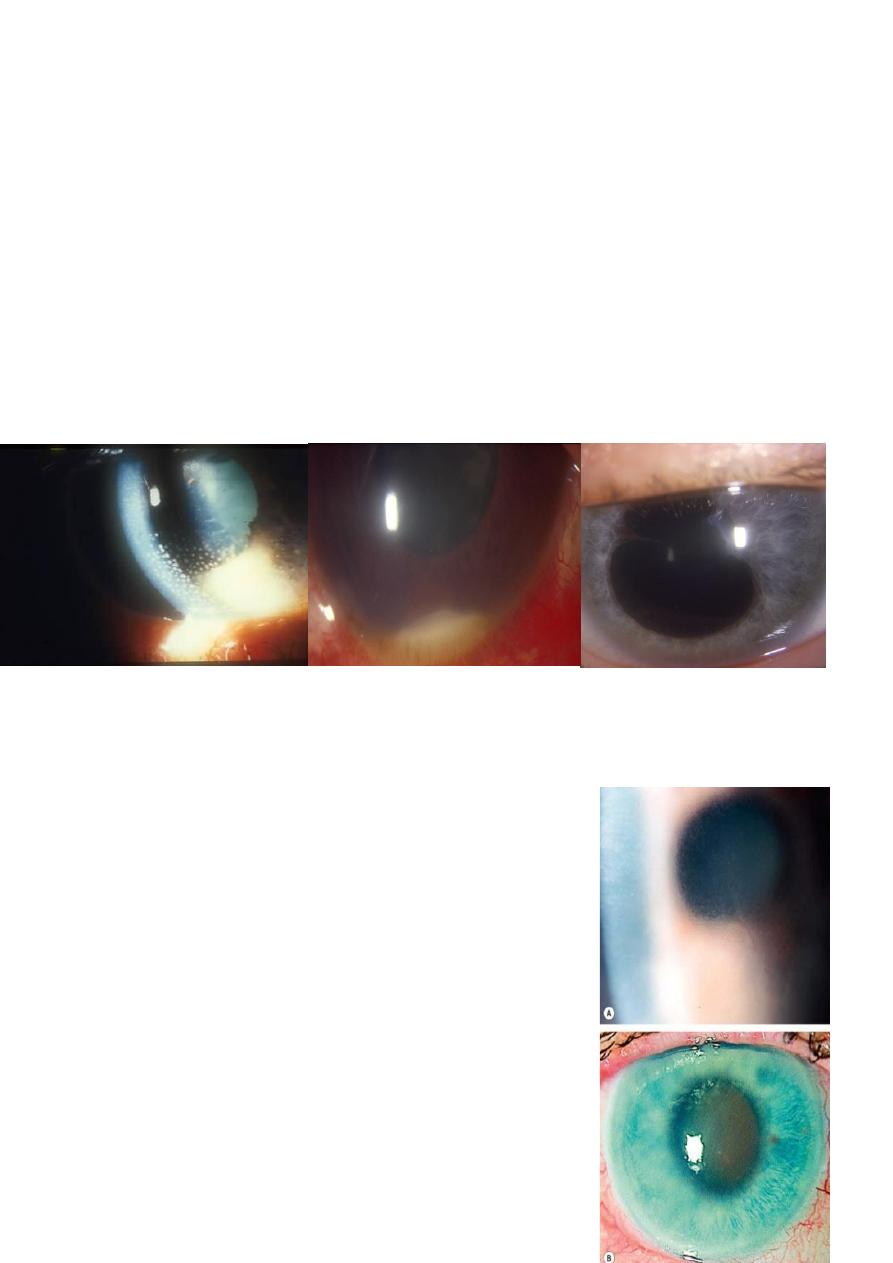
C) Anterior Uveitis
Could be unilateral or bilateral
Photophobia, watery discharge, ciliary injection ( a circle of conjunctival hyperemia
surrounding the cornea)
Vision is normal initially then starts to decrease.
Slit lamp examination: inflammatory cells in the anterior chamber, turbid aqueous
and keratic precipitates.
Management include a detailed history, examination and thorough investigations
may be needed to define the underlying aetiology
Keratic precipitate Hypopyon Posterior synechae
.
>>>>ORHigh IOP
Acute Angle Closure Glaucoma
-

Loss of Vision
History
Painful or painless
Sudden or gradual
Associated symptoms
Examination
Visual acuity and refraction
IOP
Pupillary examination
Slit lamp exmination
A) Transient : in which vision returns to normal within 24 hours
1- Amaurosis fugax due to transient ischemic attack (TIA)
2- Papilloedeama: bilateral optic disc swelling due to high intracranial pressure
3- Migraine
B) Visual loss lasts more than 24 hour
Can be further classified into
1- Sudden painless
o Vitreous haemorrhage
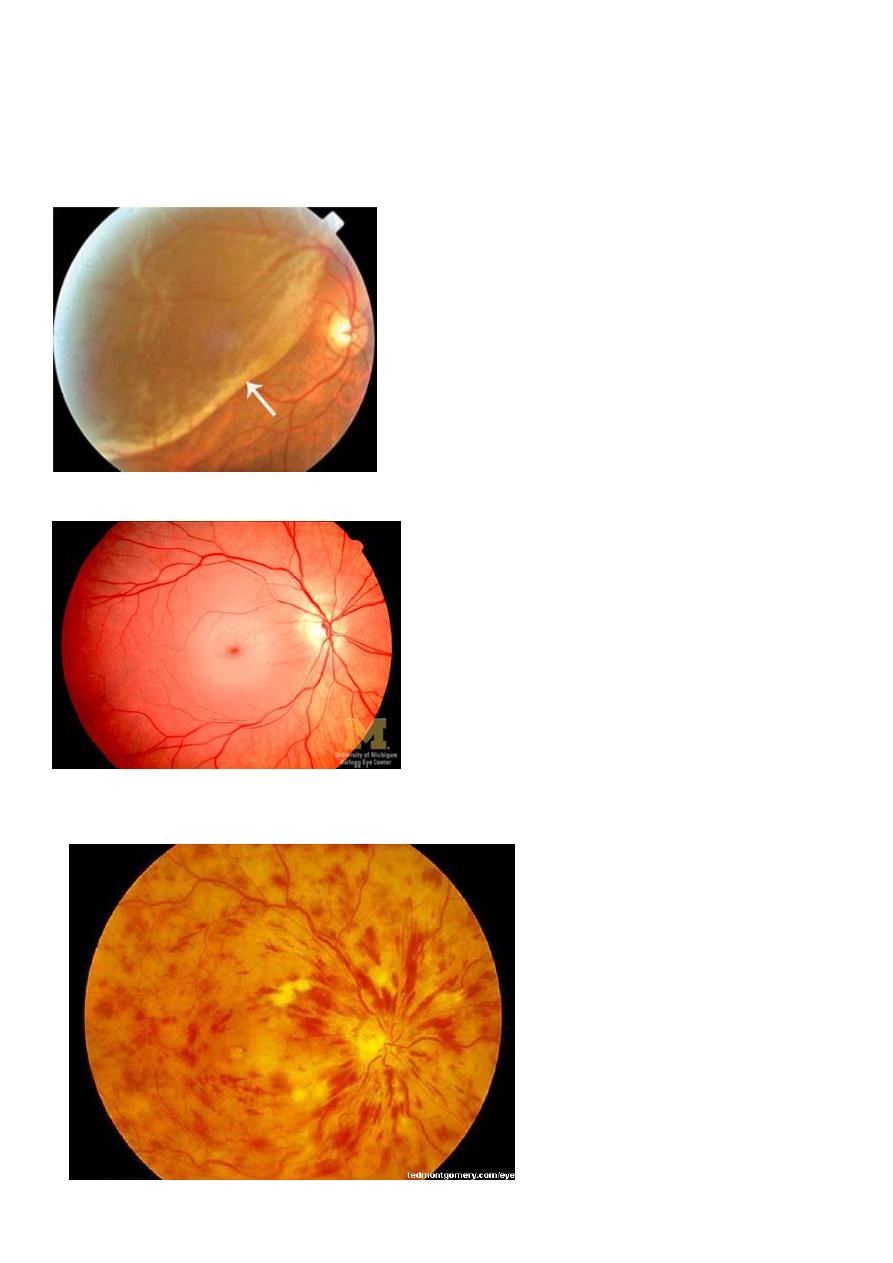
o Retinal detachment
o Central retinal artery occlusion
o Central retinal vein occlusion
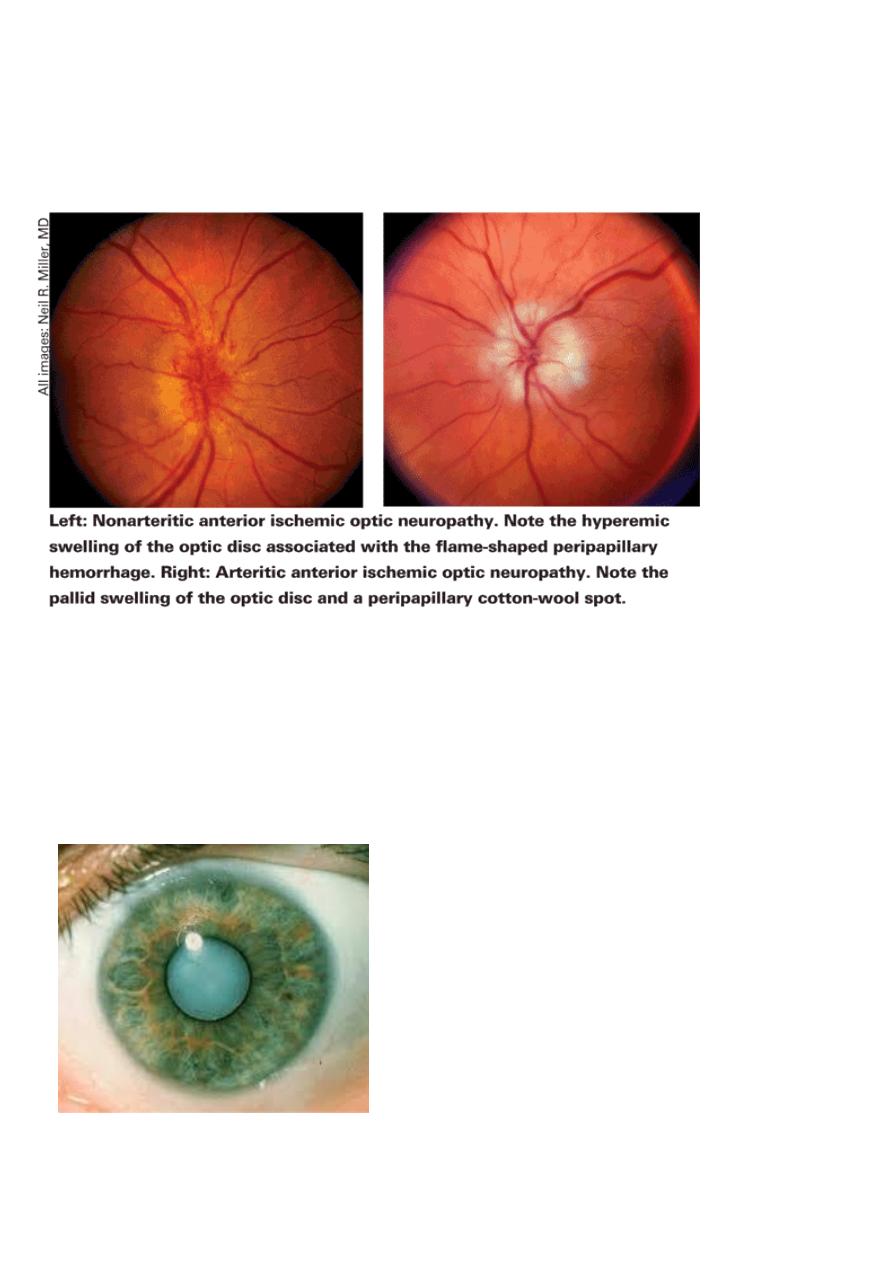
o Ischemic optic neuropathy
2- Gradual painless
o Refractive errors /presbyopia
o Cataract
o o Diabetic retinopathy
o Age related macular degeneration (ARMD)
3- Painful loss
o Acute angle closure glaucoma
o Optic neuritis
o Uveitis
o Endophthalmitis
1- Watery eye in neonates:
o The most important one is congenital glaucoma it should be excluded first, baby
has large cloudy cornea and watery eye
o Ophthalmia neonatorum: any red eye in the first 28 days of life, usually of
infectious origin, treated with topical antibiotics
o Delayed recanalization of the nasolacrimal duct: tear outflow obstruction leads to
spill over of tears ( epiphora)
2- Leukocorea ( white pupil)
1- First of all Retinoblastoma should be excluded
2- Congenital cataract
3- Congenital Vitreous anomalies
4- Retinopathy of prematurity
5- Retinal detachment
Strabismus
MISALIGMENT OF VISUAL AXES
*TYPES
MANIFEST
(-tropia)
VS
LATENT
(-phoria)
::::::::COVER-UNCOVER Test
COMITANT
(angle of squint is same in all gaze direction)
VS
INCOMITANT
-
PARALYTIC
-:::::::OCULAR motility
test)
ESOtopia –EXOtropia-HYPERtropia-HYPOtropia(cover test)
ACCOMDATIVE
VS
NON-ACCOMADATIVE
Refractive :excessive hypermetropia congenital infantile esoptropia,,,etc
Non refractive :high AC/A ratio
Mixed

MANAGEMET
*
WHY
(aim of management)?
1-restore binocular single vision
2-cosmetic
HOW
?
HISTORY
EXAMINATION
Hirschberg test
Ocular motility
Cover test
COVER-UNCOVER,
VA AND REFRACTION
FUDOSCOPY
TREATMENT
CORRECT REFRACTIVE ERROR
CORRECT AMBLYOPIA
SURGURY
GLAUCOMA
A disease of progressive optic neuropathy with loss of retinal neurons and their axons (nerve fiber
layer)+characteristic VF defect/+- Increased IOP
Intraocular pressure is not the only factor
responsible for glaucoma!
91.5 % of people with elevated IOP will never have the damage associated with glaucoma.
Some patients with glaucoma do not have
elevated IOP.
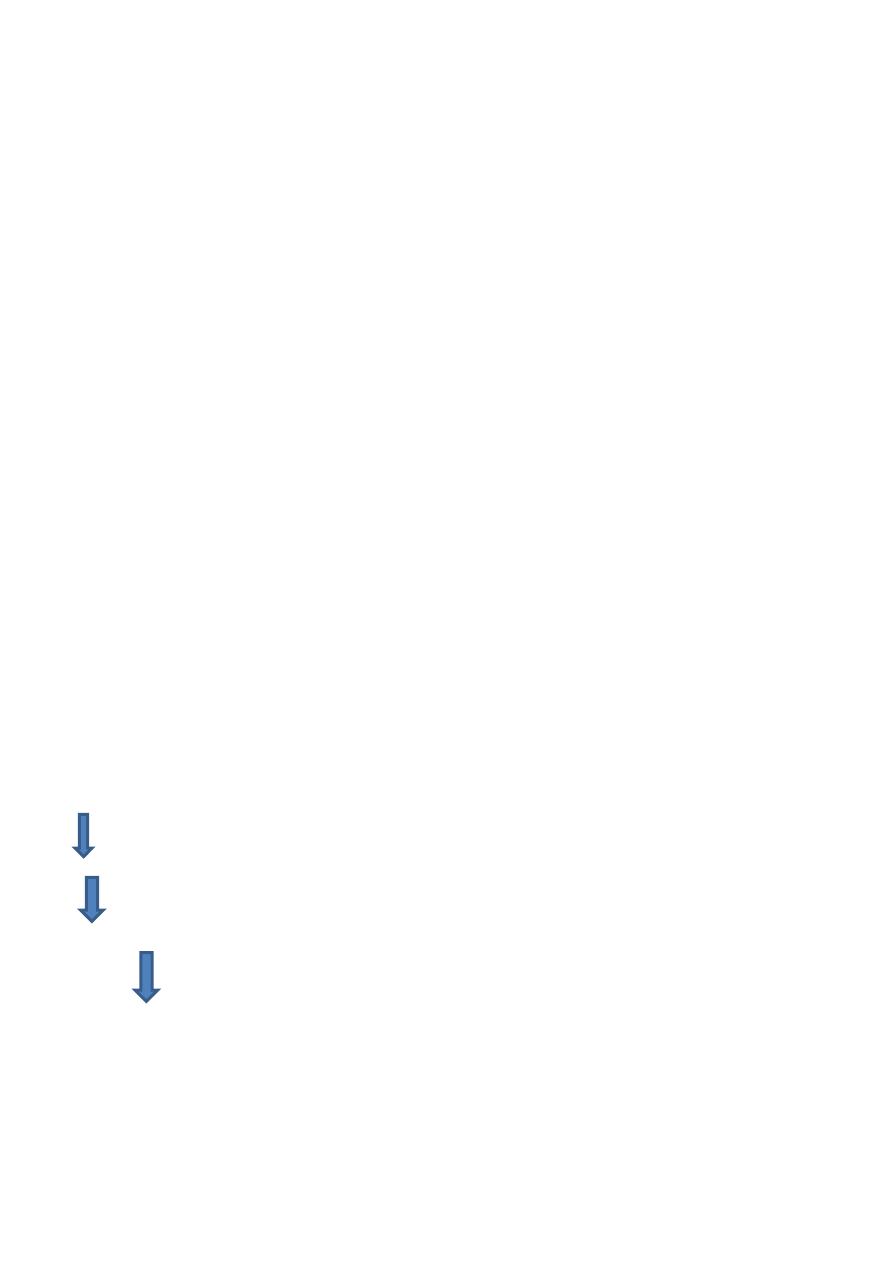
Anatomy of anterior chamber angle
Types of glaucoma
I. Primary:
A. Congenital
b. Adult (common types)
1. open angle
2. closed angle
II. Secondary
A. Inflammatory(Acute anterior uveitis)
B. neovascular
D.lens related(Phacolytic,phacomorphic,anaphylactic)
primary Open Angle Glaucoma
\
Risk Factors
IOP Diabetes
Aging Myopia
Race Gender
Family history Cardiovascular
Hormones
Symptoms
Usually none until late
Signs
- Elevated IOP
- Glaucomatous Visual field loss
(paracentral,arcuate scotoma)
-Glaucomatous disk changes
C/D ratio 0.4 or
asymmetry between both eyes of 0.2
-
Open angle by gonioscpe
Treatment;
lowering the IOP by Decreasing the secretion or increase drainage of aqueous
Medical
Beta-blockers
Carbonic anhydrase
inhibitors
Alpha-2 agonists
Prostaglandin
analogues
pilocarpine
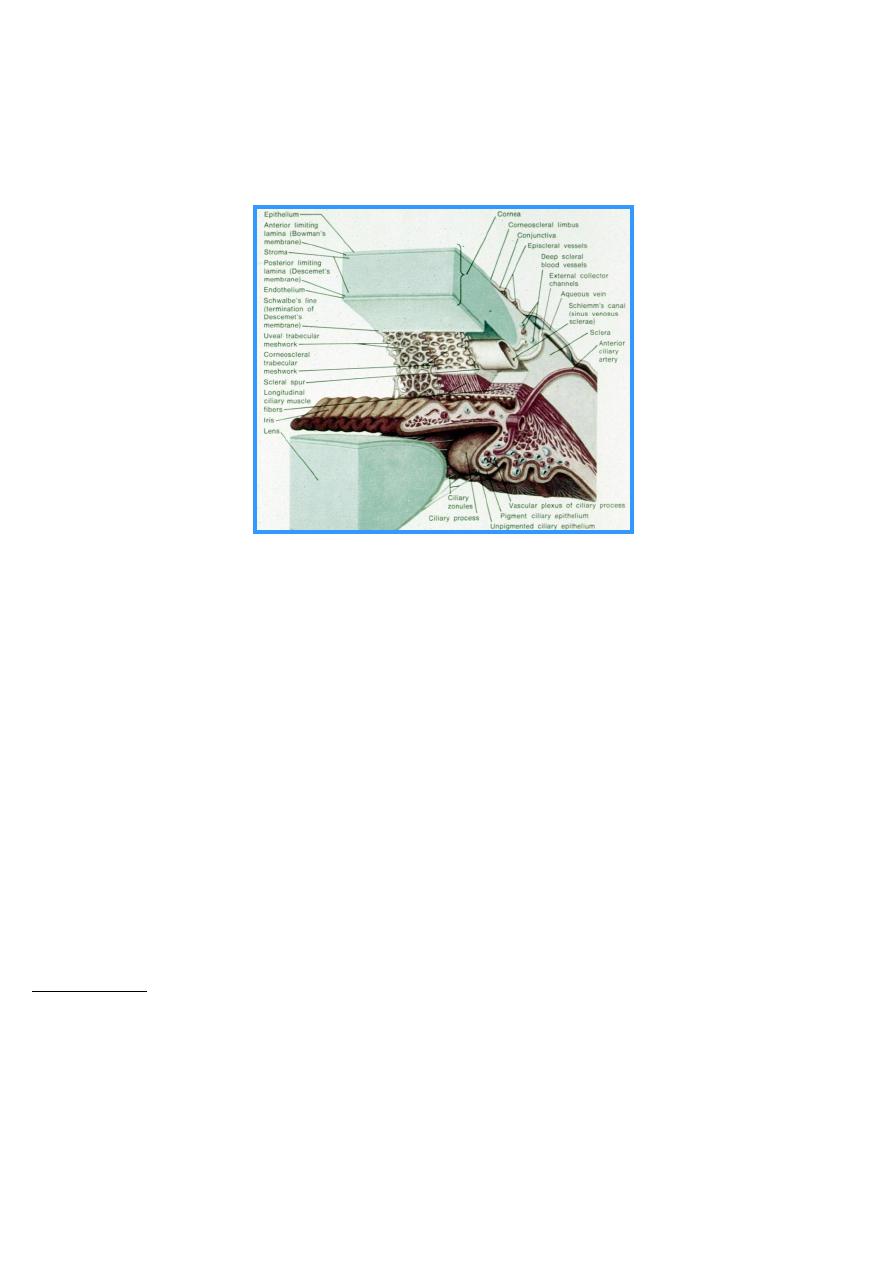
Surgical
Argon laser trabeculoplasty
k
Trabeculectomy
Cyclodestruction
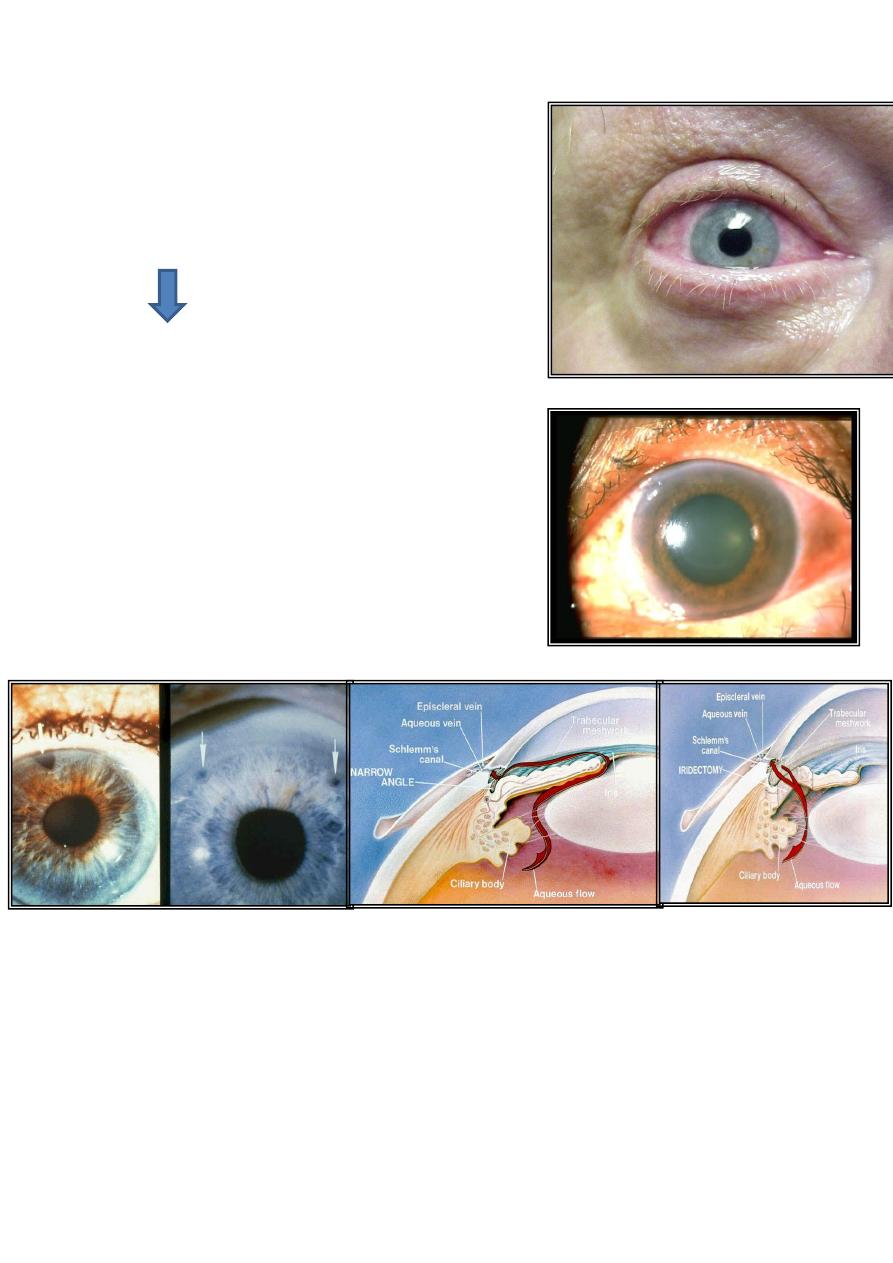
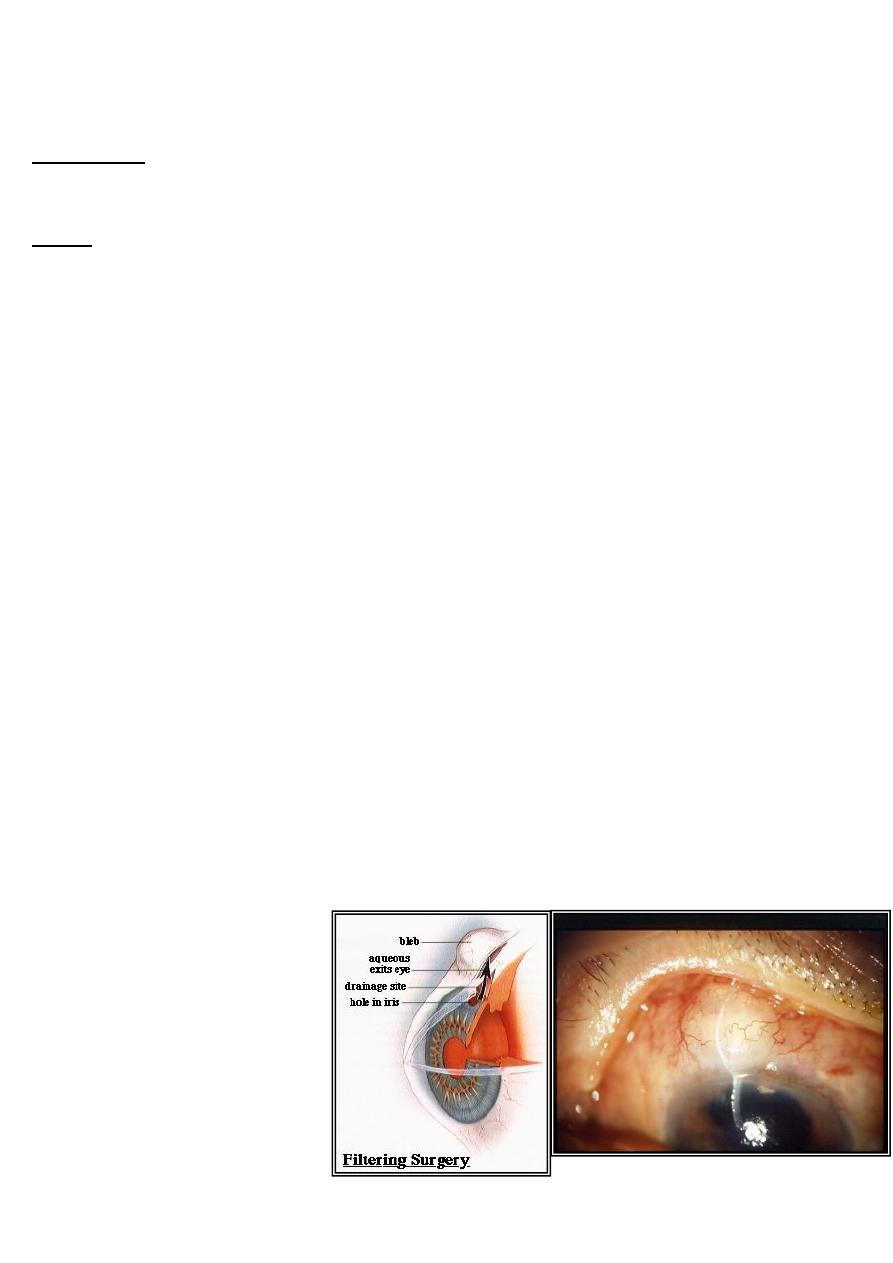
Angle closure Glaucoma
Latent/Acute/chronic
A serious Ophthalmic emergency
Sudden onset of severe ocular pain with N&V, blurring of
---
vision and coloured halos around lights
Fixed mid-dilated pupil and oval in shape
Narrow or occludable angle
Very high IOP > 50 mmHg
Corneal oedema
Treatment
--
-
Systemic carbonic anhydrase inhibitors like Acetazolamide
-
Topical B-Blocker and pilocarpine
-
Topical Steroids
-
Peripheral laser iridotomy to break pupillary block
.
Congenital Glaucoma
Anterior segment agenesis-no trabecular meshwork-
--Symptoms
Irritability
Photophobia
watery eye
Poor vision
--Signs
Elevated IOP
Buphthalmos
Haab’s striae
Corneal clouding
Glaucomatous cupping
corneal diameter >12mm at 1 year
>13 mm at any age
Treatment
--
Surgery
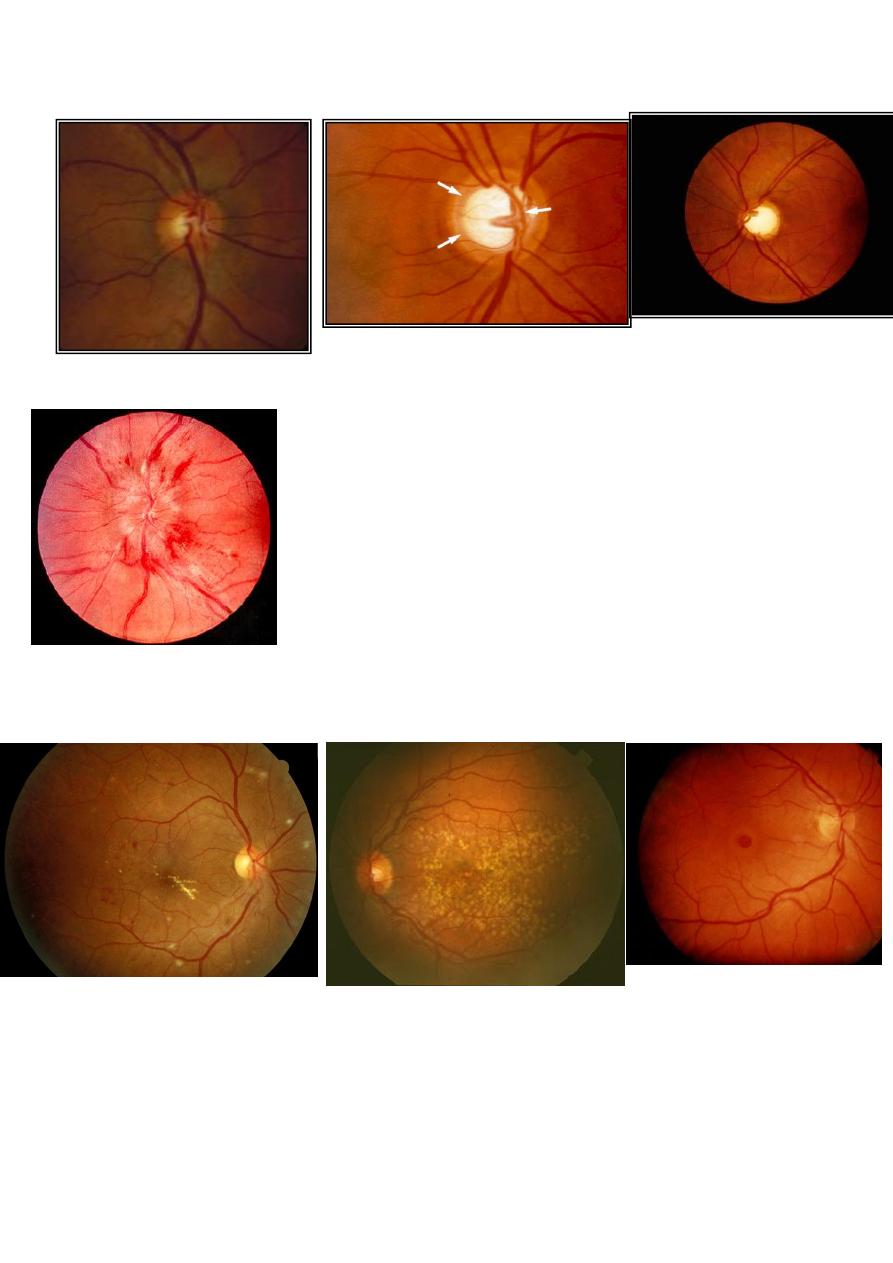
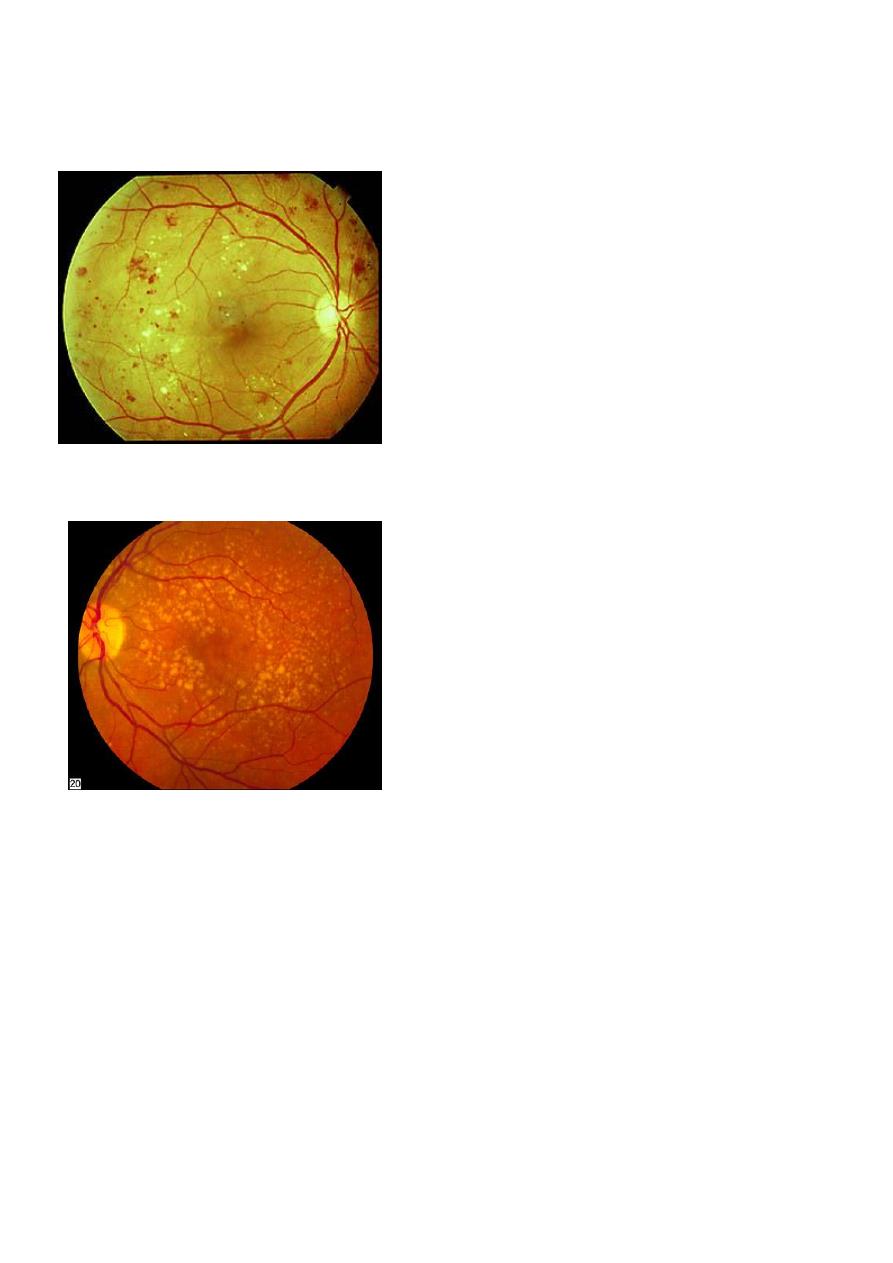
DIABETIC RETINOPATHY
• Diabetic retinopathy (DR) is a microangiopathy primarily affecting the arterioles, capillaries
and post-capillary venules.
• The main pathology in DR is: either
• microvascular occlusion>>ischemia>>AntiVEGF>>neovascularization.
• Or microvascular leakage.>>>Occur due to breakdown of inner BRB>>>Lead to
intraretinal haemorrhages and Oedema
Classification
---
1.
Background DR.
2.
pre-proliferative DR.
3.
Proliferative DR.
4.
Advance DR.
Maculopathy which may or may not be associated with one of the above changes
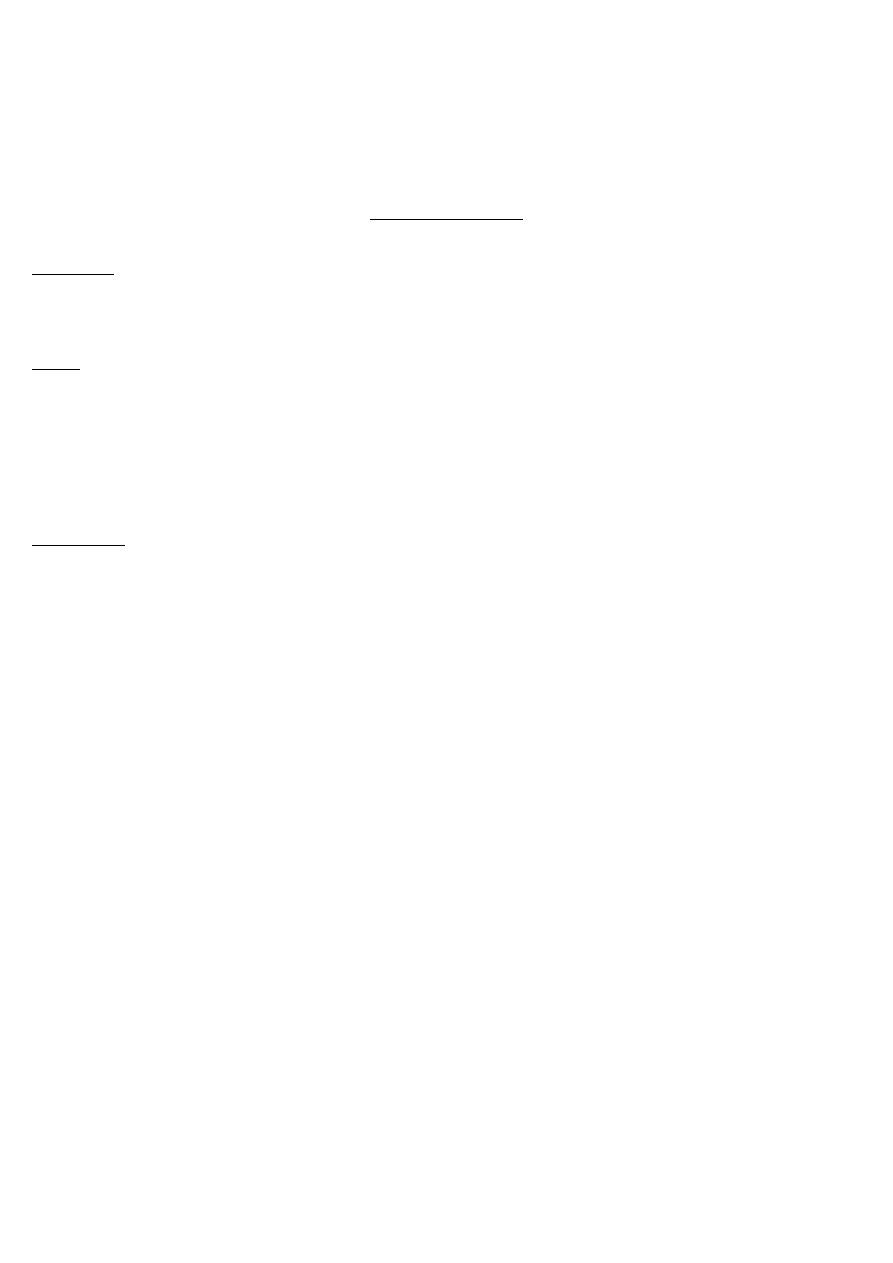
Background DR.
Characterised by the following features:
1.
Microaneurysm
2.
Hard exudates
3.
Intraretinal haemorrhages
Blot and Dot
Flame shape
microaneurysm
Retinal haemorrhages
Exudate
chronic localized retinal oedema and develop at
the junction of normal and oedematous retina.
They are composed of lipoprotein and lipid-filled
macrophages
Management of Background DR
• It requires NO treatment, but should be reviewed every 6 months. In addition, patients
need to control of diabetes and associating factors as hypertension, hyperlipidemia and
renal impairment.
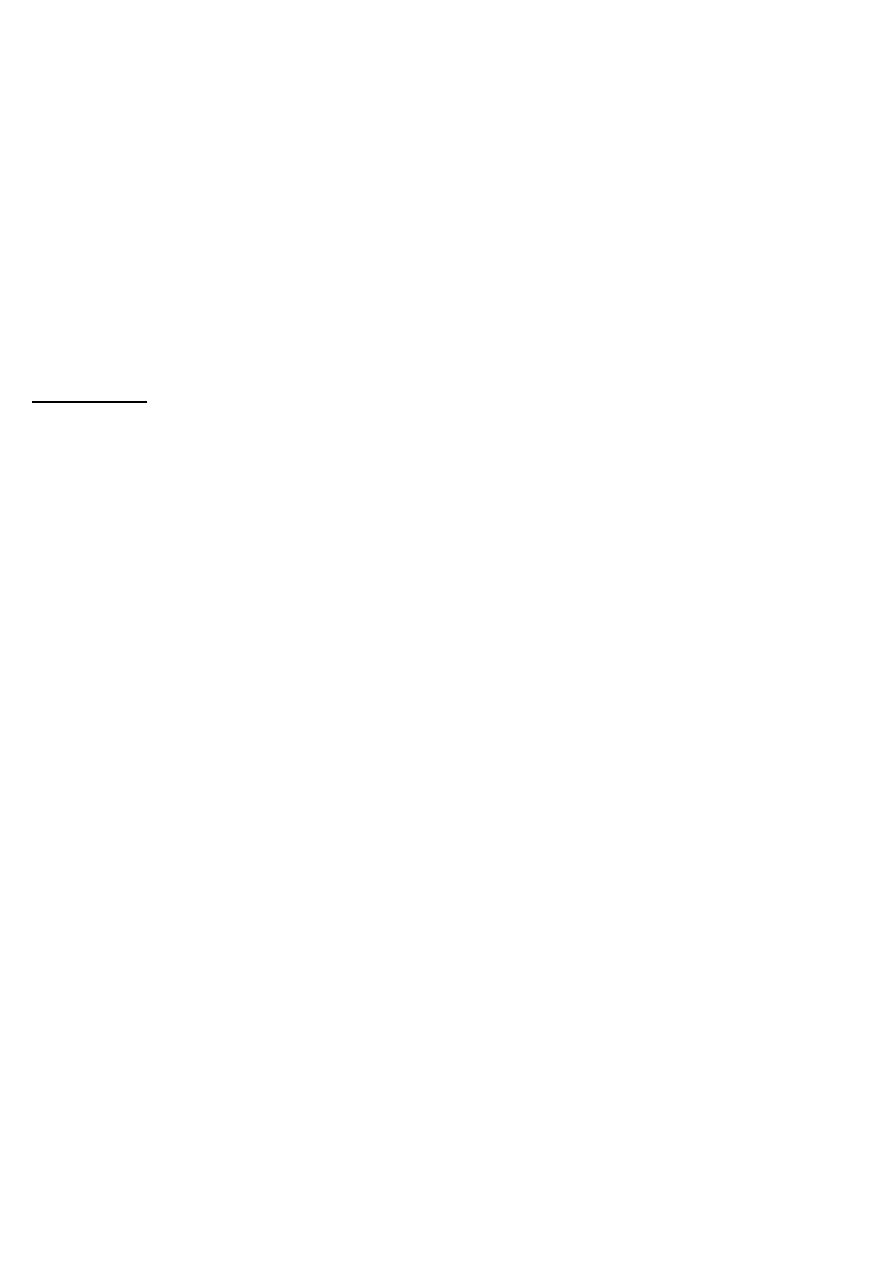
Preproliferative DR
• Characterised by the following features in addition to those found in background DR.
1-Cotton wool spots Are focal infarction of retinal nerve fiber layer due to occlusion
of pre-capillary arterioles subsequent build-up of
transported material within the axis
(axoplasmic stasis) are responsible for
the white appearance of the lesions.
2-Intraretinal Microvascular abnormalities (IRMA)
Represent shunts that run from retinal arterioles
to venules, bypassing the capillary bed
.
Often seen adjacent to areas of marked capillary
hypoperfusion
Management
• Should be watched closely every 3 months because of the risk of PDR (Proliferative
Diabetic Retinopathy) is high
• . Laser photocoagulation is usually not needed unless:
1.
Regular follow-up is not possible.
2.
Vision in the fellow eye has been already lost due to PDR.
Proliferative DR
• Affects 5-10% of the diabetic population
• Neovascularization is the hallmark of PDR
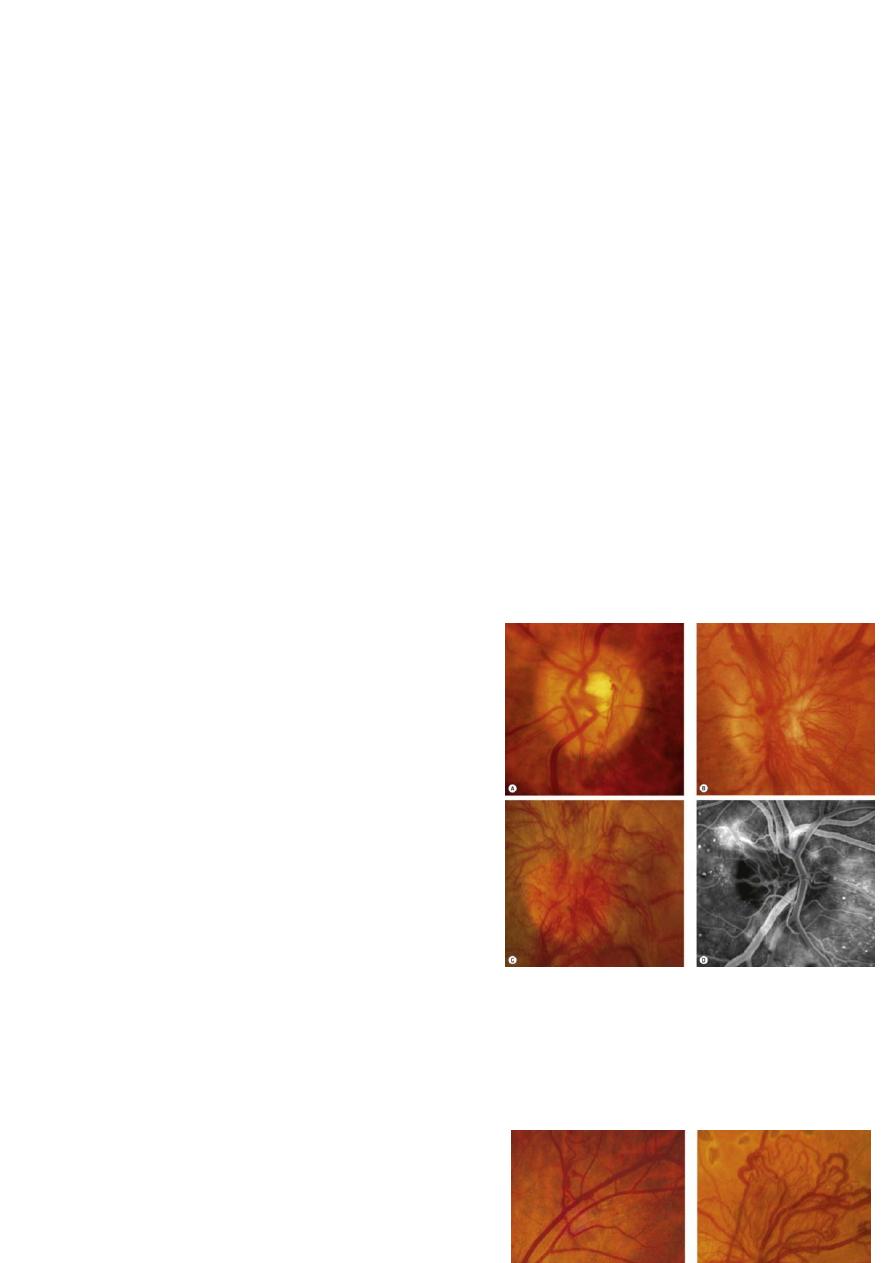
Neovascularisation of the disc (NVD)
Neovascularisation elsewhere (NVE)
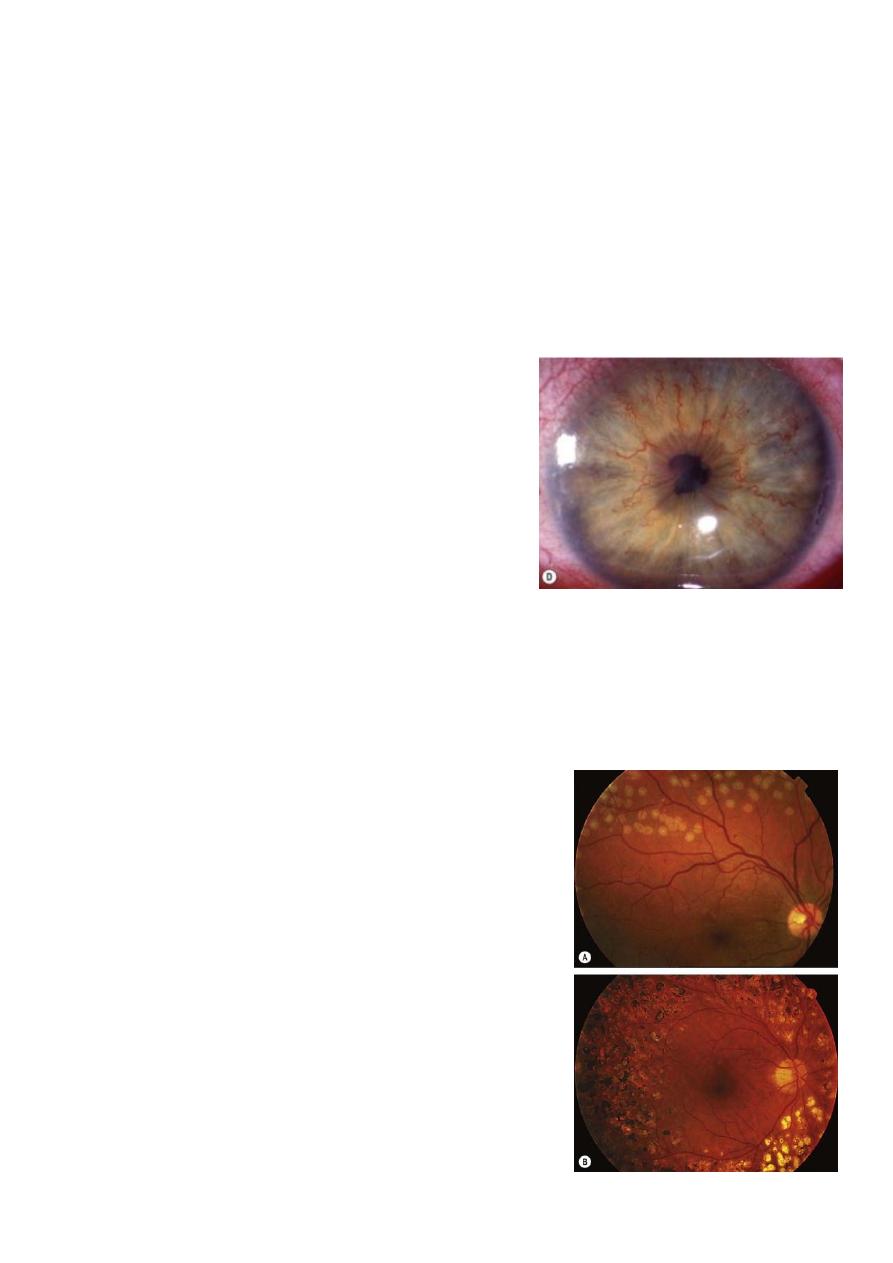
Neovascularisation of the Iris (NVI) or whats called rubeosis irides
NVD
NVE
These new BV are abnormal and fragile,
might lead to spontaneous rupture and
bleeding ( preretinal or vitreous haemorrhage)
leads to sudden drop of vision and other vision
threatening complications like tractional retinal
detachment SO WE SHOULD INTERVENE PROMPTLY
NVI
Management
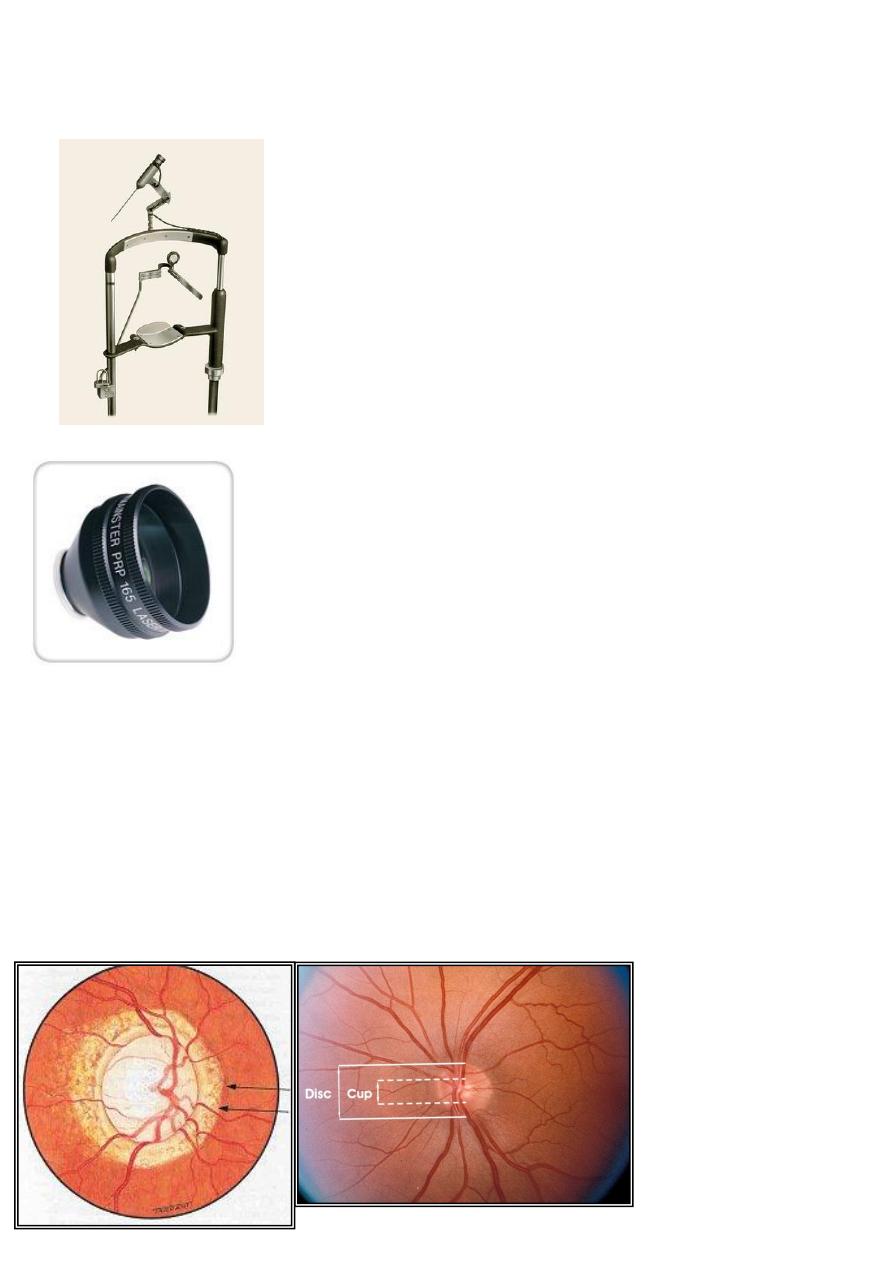
Pan-Retinal Photocoagulation (PRP):
A destructive procedure, where we destroy all normal retinal tissue around the temporal
arcades (temporal blood vessels) in order to decrease retinal ischaemia by decreasing O
2
demand. Then the neovascularization resolves spontaneously (no hypoxia → no growth factors).
Side effects of PRP:
1- Constriction of visual field (loss of peripheral visual field).
2-Nyctalopia (night vision)
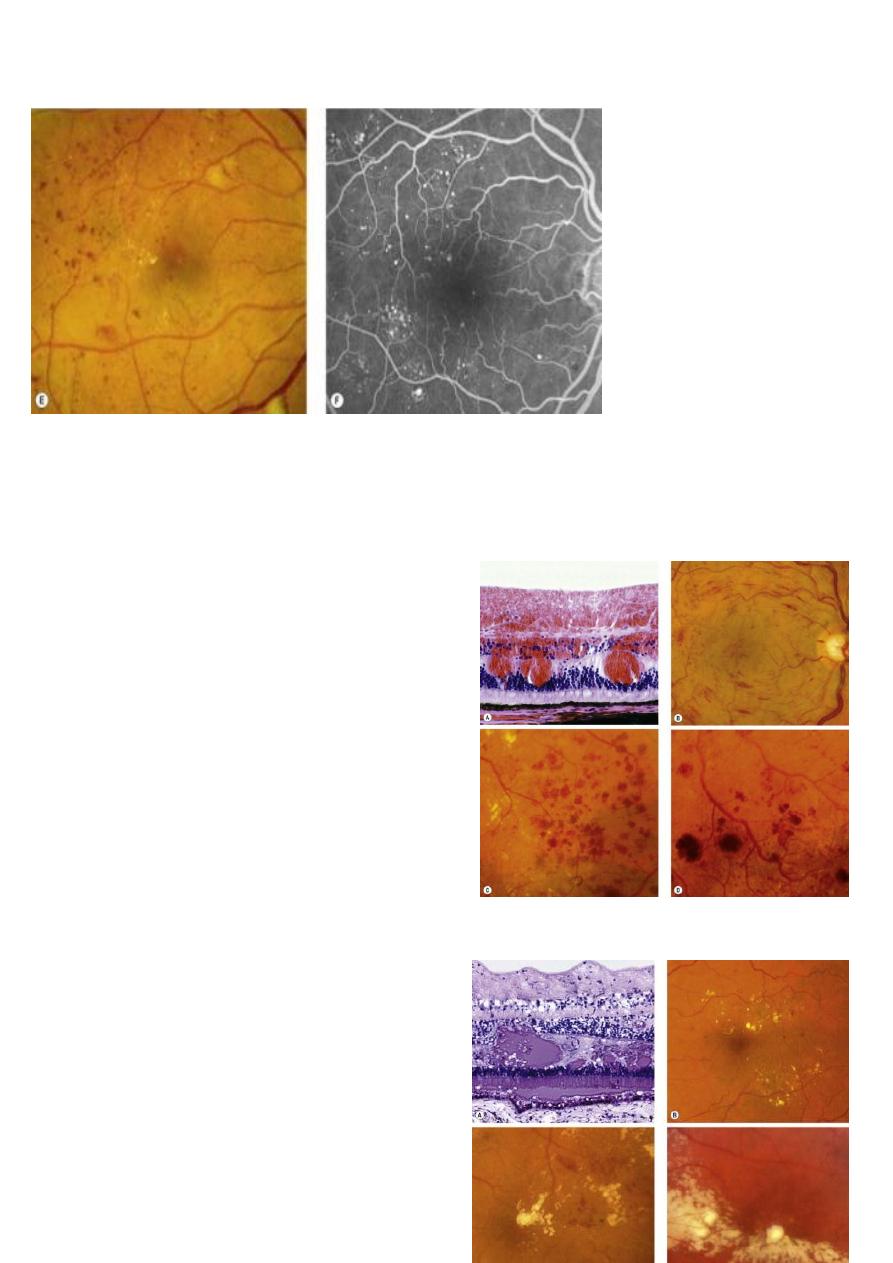
Maculopathy
• It is the involvement of the fovea by either oedema and exudates (leakage) or ischaemia
(occlusion). Diabetic maculopathy is the most common cause of visual impairment in
diabetic patients particularly those with type 2 diabetes.
• Is might be associated with: a- Background DR.
b- Pre-proliferative DR.
c- Proliferative DR.
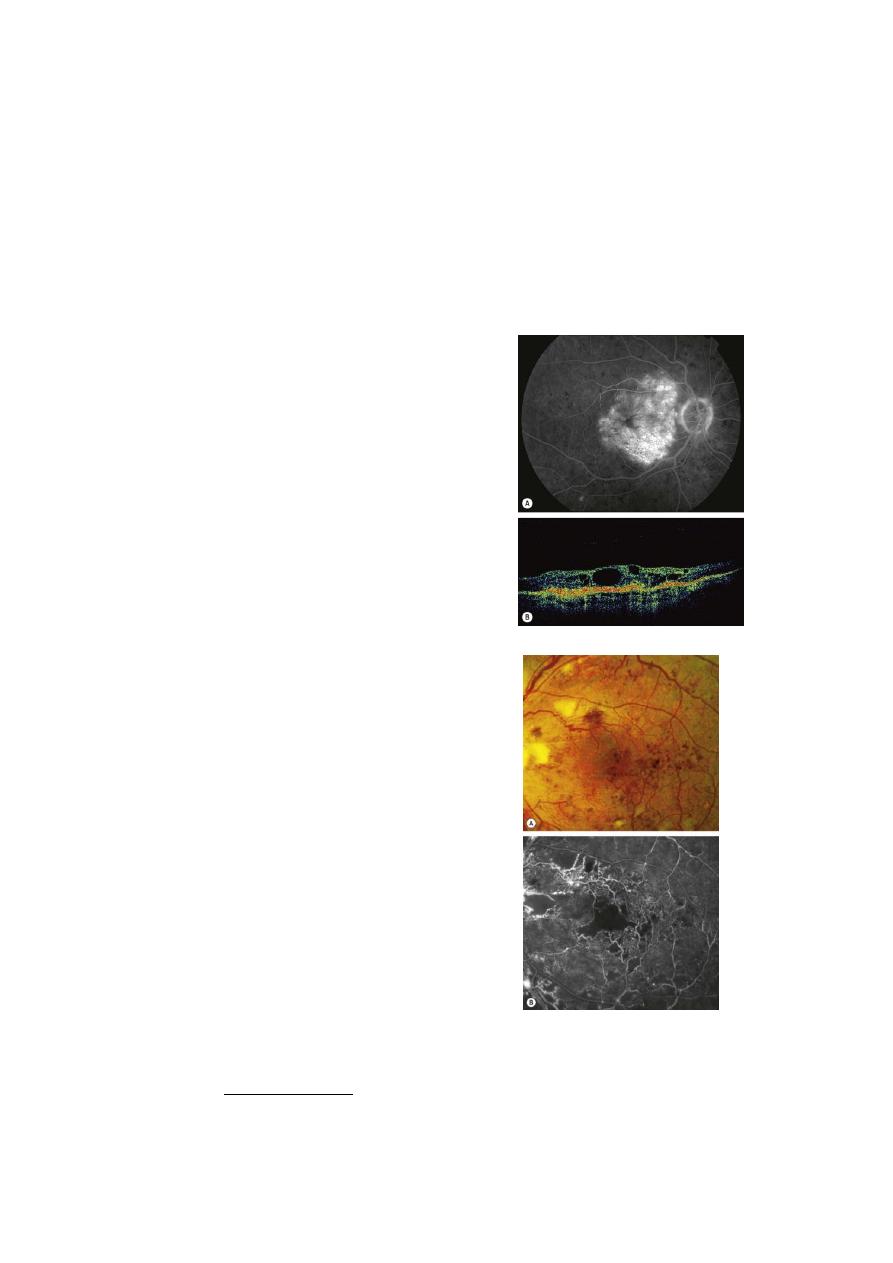
Macular edema
Ischemic Maculopathy
Management
• First , we should do FFA to differentiate between Ischaemic and exudative maculopathy
Tretement options for exudative type include:
1.
Focal laser treatment for focal maculopathy
2.
Macular grid laser for diffuse
3.
Intravitreal VEGF
4.
Intraviteal Steroids
For ischaemic maculopathy
:
No treatment available, if the ophthalmologist is not well oriented and he do focal
photocoagulation for such cases, he will going to induce more ischaemia and more deterioration
of visual acuity laser is contraindicated in ischaemic maculopathy
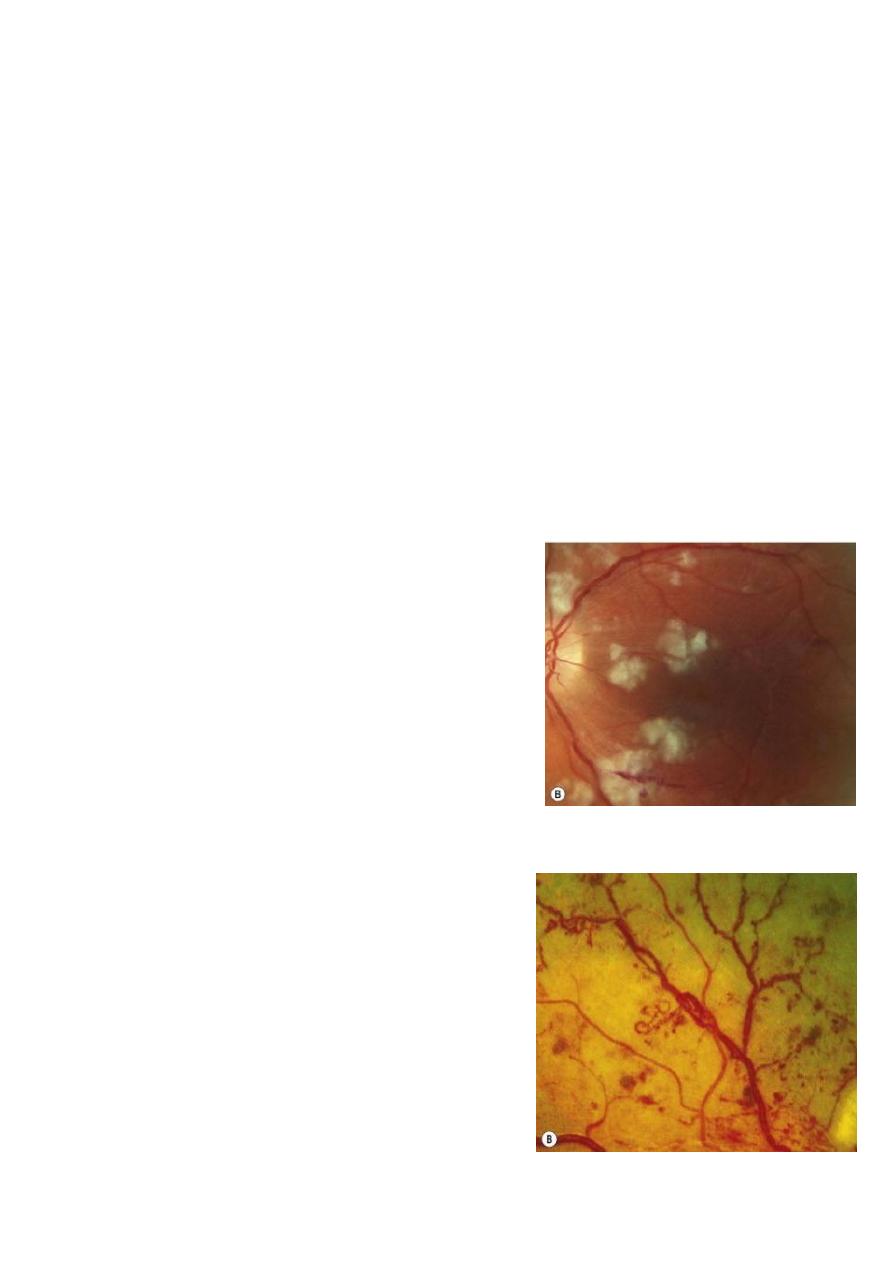
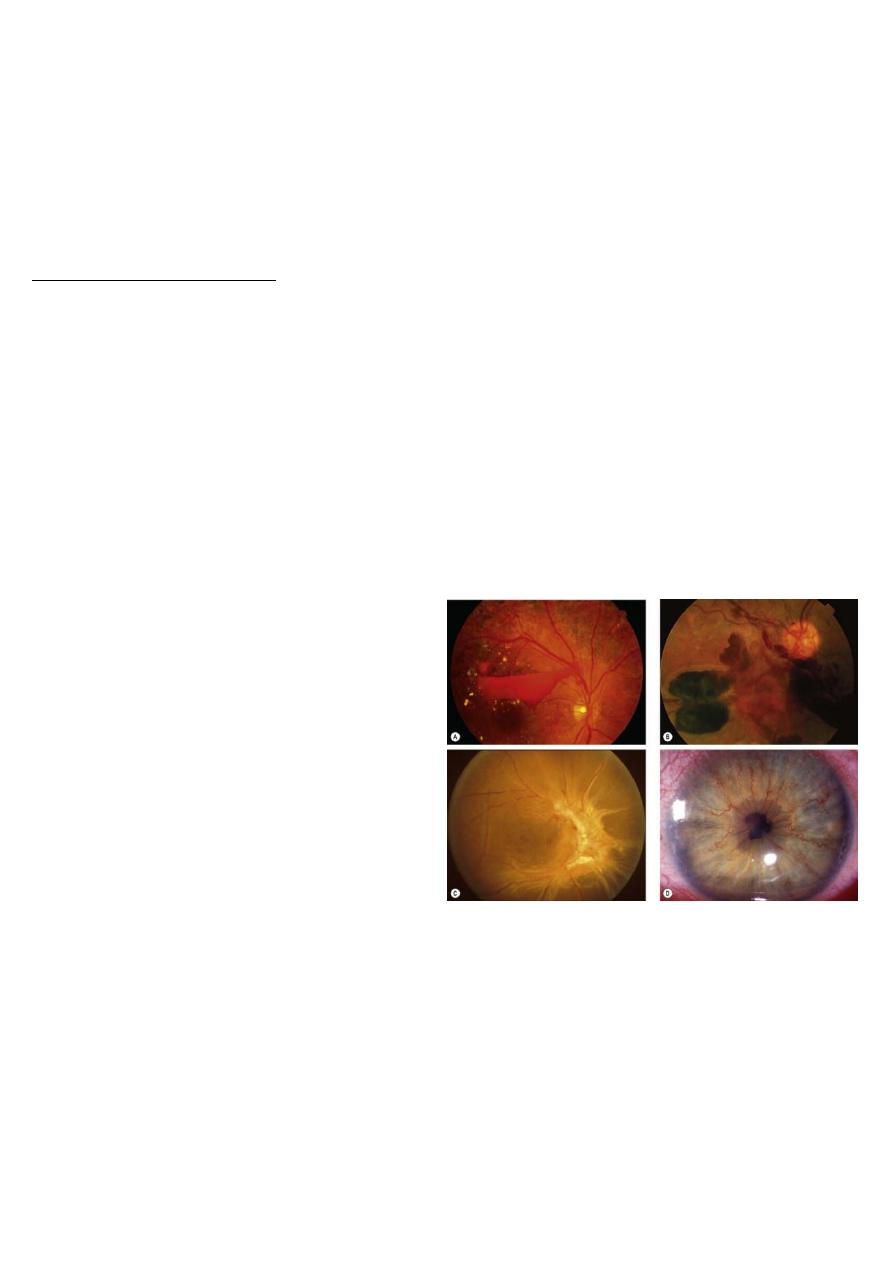
Advanced diabetic eye disease (ADED):
Serious vision-threatening complication of diabetic retinopathy occurs in patients who have not
had laser therapy or in whom laser photocoagulation has been unsuccessful or inadequate.
• It includes:
1- Hemorrhage. (pre-retinal or intravitreal).
3- Tractional RD: due to fibrovascular
membranes formation or fibrous tissue
formation due to organization of pre-retinal
or intravitreal hemorrhage.
3- Neovascular glaucoma
(A) Retrohyaloid haemorrhage; (B) intragel haemorrhage; (C) tractional retinal detachment; (D)
rubeosis iridis
Treatment
• Vitrectomy + Retinal reattachment surgery + Endolaser (PRP).
• Endolaser: done in the theatre by applying the laser through a fiberoptic probe in the eye,
instead of using slit-lamp biomicroscope

