1
Rheumatology sessions
Part1: History
Ask about any pain or stiffness in muscles, joints or back.
“Do you have any trouble getting up or down stairs?”
“Do you have any difficulty getting dressed?”
How symptoms started (mechanism of injury)?
Onset and Duration of complaint.
Location of pain or symptoms.
Exacerbating or relieving maneuvers.
Nature of symptom (continuous or intermittent).
Aggravating and reliving factors.
Radiation of pain.
Work of the patient, and the effect of disease on the work.
Family history.
Part2: Physical examination in general
Inspection:
Observe how the patient moves as they go into the room or move from chair to
table.
Look for asymmetry between sides.
Swelling:
o Confined to joint like in inflammation and infection.
o Beyond the joint like in systemic diseases.
Deformities:
o Varus deformity.
o Valgus deformity.
Atrophy:
o Disuse atrophy.
o Nerve injury.
Erythema or redness.
Bruises, scarring, psoriatic lesions.
Palpation:
Palpate for tenderness.
Palpate for swelling.

2
Palpate for warmth.
Palpate each area of the structure in turn evaluating for pain, and abnormalities as
compared to the other side.
Range of movement:
Active
Ask the patient to move his joint.
Watch for decreased or increased movement of the joint compared to the other side
as well as the normal.
Watch for pain with movement.
Listen for crepitus or “popping”.
Watch for abnormal movements.
Passive
Move the joint passively, comparing the end points to the active.
Again note any decreased or increased movement.
Pain with the movement,
Crepitus or “popping”.
Movement reduced in
Contractor of muscle.
Trauma.
Nerve injury.
Capsule problem.
Investigations:
Radiological: X-ray, CT, MRI, US.
Blood test: CBC, serum phosphatase, serum calcium, serum phosphate, serum uric
acid.
ESR, CRP.
Serological test.
Part3: The neck
Inspection:
From front, side, and back.
See swelling, scar, atrophy, LN enlargement.
3
Palpation:
Tenderness over cervical spine and para-spinal muscles.
LN palpation.
Thyroid examination (for goiter).
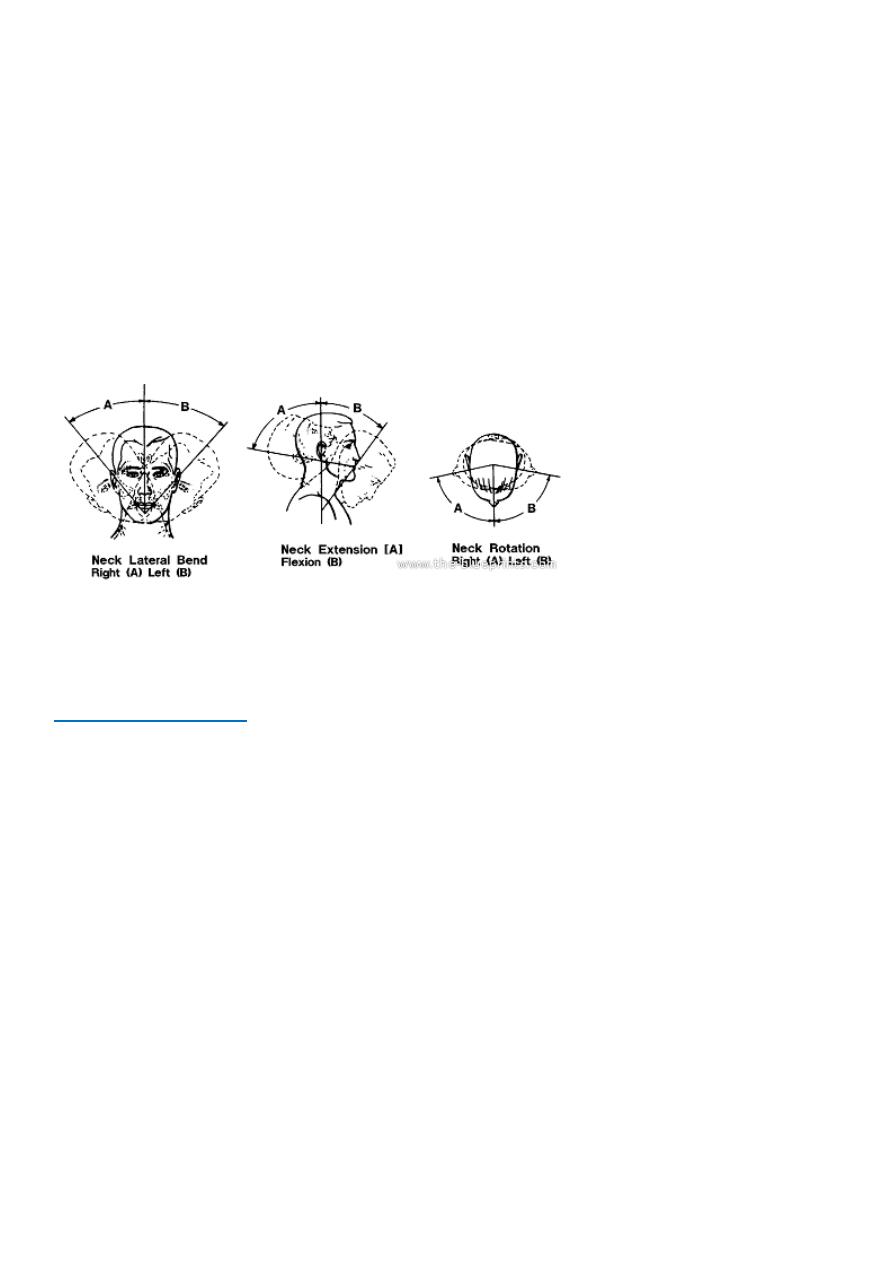
Movement:
Flexion: chin must touch the upper part of sternum.
Extension: the face become parallel to wall.
Lateral rotation: 80-85 degree normally.
Lateral bending: 60 degree.
See this video: www.muhadharaty.com/lecture/1186
Part4: The back
Back pain:
Very common.
Could be due to:
o Infection like brucella.
o Mechanical (disc prolapse).
o Metastasis (breast cancer, prostatic cancer).
o Could be part of systemic diseases like T.B.
Inspection:
From side kyphosis, atrophy, discoloration, swelling, cyst, lipoma, curvature of
lumbar vertebra.
From back scar, deformity, discoloration, scoliosis.
Scoliosis:
o Could be fixed (congenital or fracture).
o Could be due to leg length discrepancy.

4
Palpation:
hotness, tenderness.
Percussion:
by fixed fist.
Movement:
Flexion: normally the tip of finger reach the mid-shaft.
Extension: normally 30-40 degree.
Lateral flexion: hand reach the knee.
Schober test:
Put a point in the back at level of posterior superior
iliac spine.
Put another point 10 cm above the first one.
Put third point 5 cm below the first point.
Then use tap measure, and ask the patient to lean
forward.
The distance between second and third point must
be increased by 5 cm or more, so it will become 20
cm (10+5+5).
If the distance not increased by 5 cm it means there
is movement restriction of the back.
Straight leg rising test:
Ask the patient to lie on his back.
Elevate his leg in a striated manner.
Normally the leg rises to 70 degree without pain.
If pain occur at 70 degree or below it means there is problem (+ve test).
If pain occur above 70 degree it means nothing (-ve test).
Neurological examination:
Knee jerk: L4 mainly, and L5.
Ankle jerk: S1 mainly, and S2.
Notes:
Scoliosis fixed or positional (which is due to pain or leg length discrepancy).
Disc prolapse commonly between L4,L5 or L5,S1.
Schober test proper (0 – 10 cm) // Modified Schober test (5 – 0 – 10 cm).
See this video: www.muhadharaty.com/lecture/1192
5
Part5: The shoulder
Joints of the shoulder:
Glenohumeral.
Sternoclavicular.
Acromioclavicular.
Scapular thoracic (not a true joint).
Inspection:
as examination of joints in general.
Palpation:
as examination of joints in general.
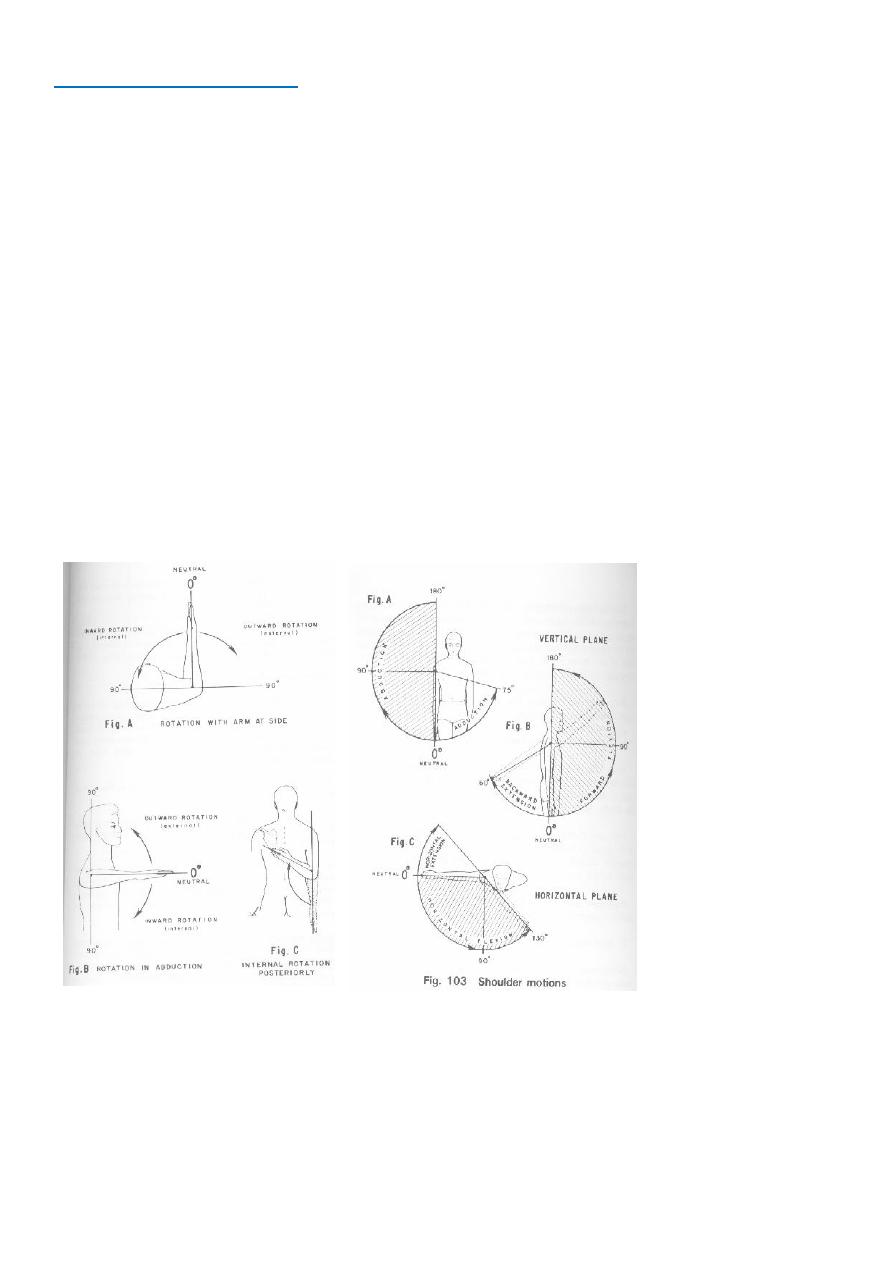
Movements:
Flexion (120 degree), extension (60 degree).
F → c4, c5
E → c6, c7
Adduction (120 degree), abduction (160-170 degree).
Internal rotation, external rotation.
Notes:
Causes of restricted shoulder joint movement
infection, inflammation, trauma,
clacified tendon.
Wing scapula
due to injury to long thoracic nerve of serratus anterior muscle.
See this video: www.muhadharaty.com/lecture/1187

6
Part6: The elbow
Inspection:
Inspect the carrying angle, and any nodules or swelling.
Front:
o At the overall alignment of the extended elbow
o CUBITUS VALGUS.
o Scars: suggestive of previous injury / surgery.
o Swelling / erythema of the joint: may suggest acute injury / inflammatory
arthritis / infection.
o Carrying angle 11-13 degrees – female tend to have more significant carrying
angles than male.
Side:
o Scars / Swelling / bruising / Erythema / rash / tophi.
o Fixed flexion deformity: often post traumatic.
o Olecranon bursitis: the swelling overlying the olecranon is often most noticeable
from this angle.
o Swelling of synovitis between the lateral epicondyle and olecranon.
Back:
o Rheumatoid nodules firm lumps on the elbow / olecranon – indicate systemic
rheumatoid disease.
o Psoriatic plaques well defined pink / red elevated lesions with silvery scale.
Palpation:
Lateral and medial epicondyles, olecranon, radial head, groove on either side of the
olecranon.
Temperature a particularly warm joint may indicate inflammatory arthritis or
infection.
Palpate the joint lines including the epicondyles & olecranon for any localized
tenderness.
Bursae fluid-filled sacs which are usually soft, but if acutely inflamed or infected
may be firm.
Bony contours, sponginess, tenderness.
Palpate for ulnar nerve tenderness over its course.
Palpate for bicipital tendinitis.
Movements:
Elbow flexion – extension: normal range is 0 – 145º // range less than 30–110° will
cause functional problems.
F → c5, c6.
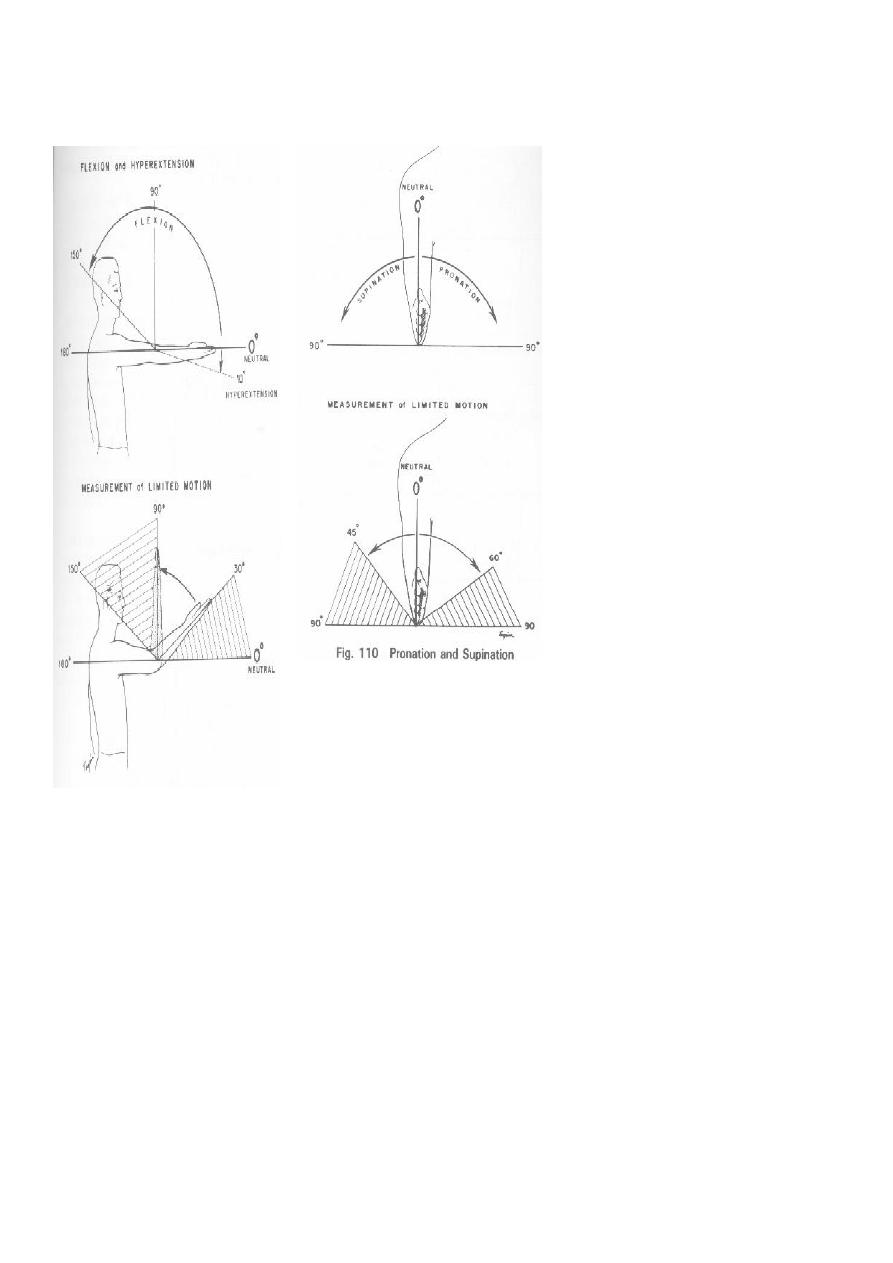
7
E → c7, c8.
Pronation 85º and Supination 90º.
When moving the joint passively assess for crepitus.
Other test:
Varus test: Tests for ligamentous stability of the lateral collateral ligament.
Valgus test: Tests the medial collateral ligament.
Golfer’s elbow test: While palpating the medial epicondyle, the forearm is supinated
and the elbow and wrist are extended. Positive if pain over the medial epicondyle.
Tennis elbow test: Ask the patient to actively extend the wrist whilst the elbow is
flexed. Localized pain over the lateral epicondyle and may be referred down the
extensor aspect of the arm suggests a diagnosis of lateral epicondylitis.
Tinel’s of the elbow: Percussion of the ulnar nerve in the grove. Positive if radiating
sensation down arm into hand.
Test for tennis elbow: do extension of wrist against resistant.
Test for golfers elbow: do flexion of wrist against resistant.
8
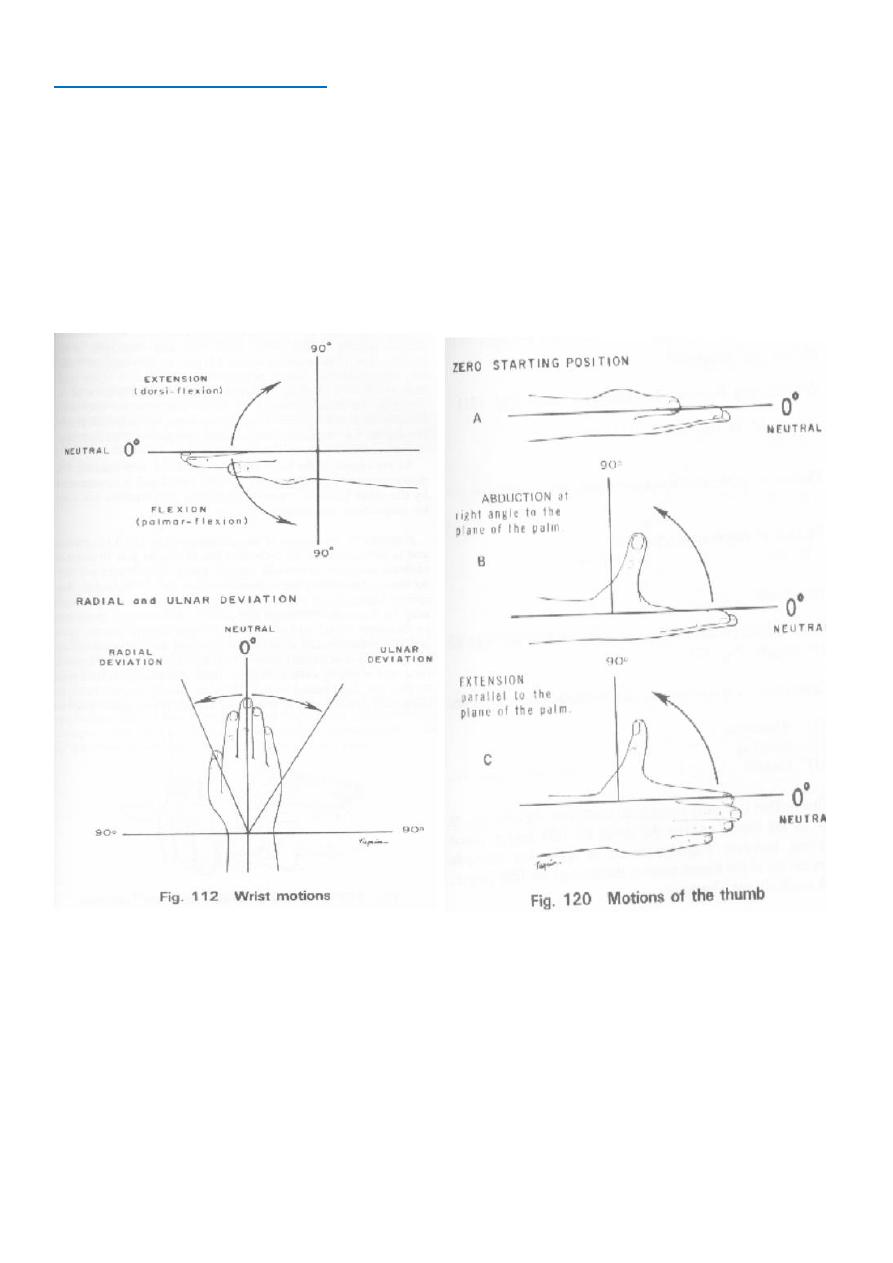
Part6: Wrist and hand
Inspection:
for swelling or deformities like swan-neck, z deformity, boutonniere.
Palpation:
anatomic snuff box, volar and dorsal aspects of the wrist, all joints of the
fingers.
Movement:
Flexion, extension, ulnar and radial deviation of the wrist.
Patient make a fist and extend and spread the fingers.
Function of the hand:
Benching grip.
Grasp. قلم
Thumb to side of index. مفتاح السيارة
Palmar grasp. كرة
Hook grip.
ع
القة
Grip strength.
عمود
الزئبق
See this video: www.muhadharaty.com/lecture/1188
9
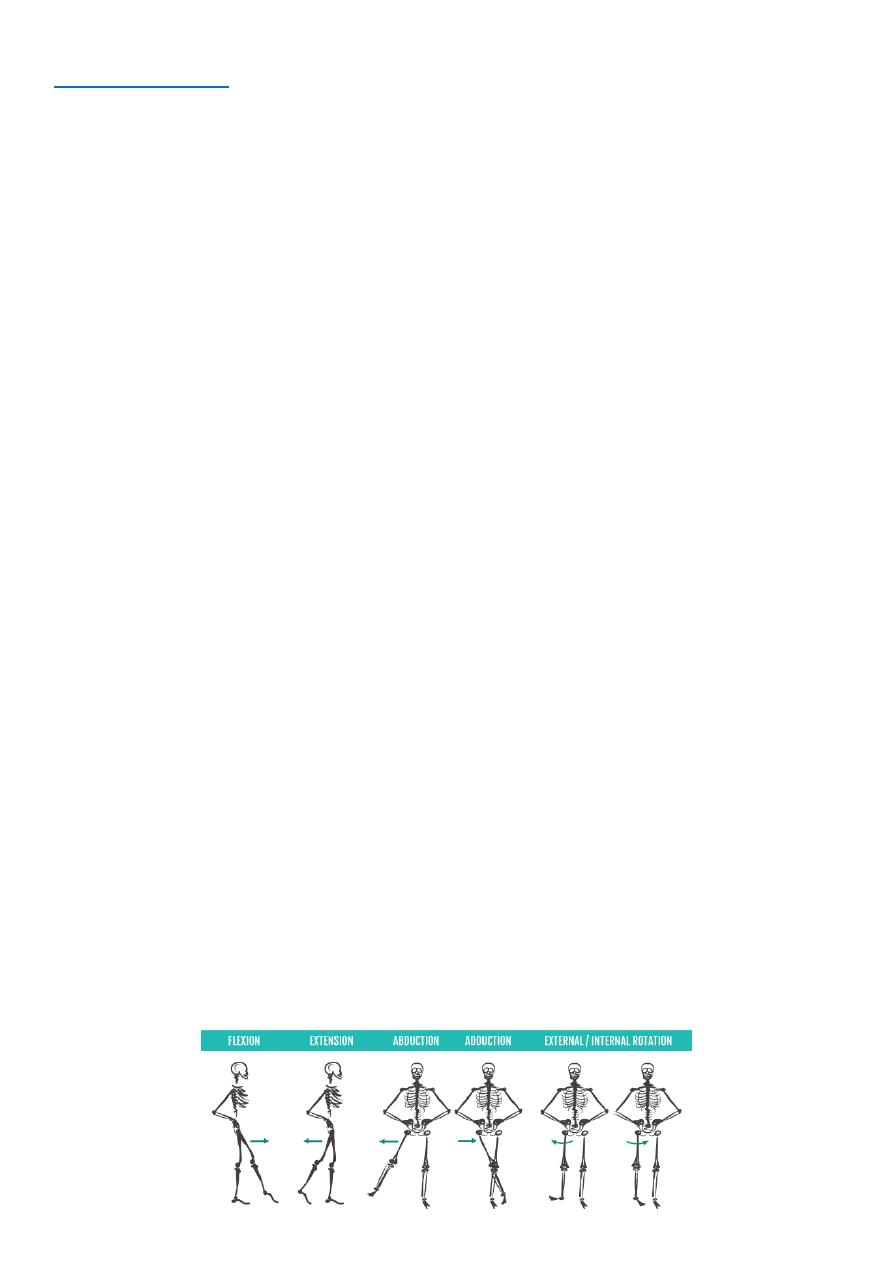
Part7: The hip
Gait:
Observe patient from behind, the side and in front.
Assess speed /smoothness /turning.
Note any evidence of antalgic gait or trendelenburg gait.
Assess the patient’s footwear – unequal sole wearing – abnormal gait.
Inspection:
As inspection of joints in general.
Palpation:
Ask patient to lay down on a bed.
Palpate the tissues overlying the hip joint for tenderness / warmth – inflammation /
infection.
Palpate greater trochanter tenderness (often indicative of trochanteric bursitis).
Tenderness over the lesser trochanter and ischial tuberosity is common in sporting
injuries.
Movement:
Flexion assess the degree of flexion in each hip individually – normal ROM is 120°
Hip extension (passive):
o Position patient prone.
o Place a hand on the pelvis to assess for movement.
o Lift one leg at a time to assess range of extension.
o Normal ROM is 0-20°.
Internal rotation This can be assessed with the hip & knee joint flexed at 90° /
Rotate the foot laterally / Normal ROM 40°.
External rotation This can be assessed with the hip & knee joint flexed at 90° /
Rotate the foot medially / Normal ROM 45°.
Abduction whilst stabilising the contralateral iliac crest, use your other hand abduct
the hip until you feel the pelvis begin to tilt – normal ROM is 45°.
Adduction whilst stabilising the contralateral iliac crest, use your other hand to
adduct the patient’s leg across the midline as far as possible – normal ROM is 30°.
10
Special tests:
Assess leg length
Ask the patient to lie supine and stretch both legs out as far as possible equally to
eliminate any soft-tissue contracture/ abnormal posture.
Measure apparent leg length umbilicus to the tip of medial malleolus.
Thomas’s test
Place hand under patient’s spine.
Passively flex both legs (hips/knees) as far as you are able to.
Your hand should detect that the lumbar lordosis is now flattened.
Ask patient to fully extend the hip you are assessing: Incomplete extension suggests a
fixed flexion deformity at the hip joint.
Repeat the test to assess the contralateral hip joint.
= DO NOT PERFORM ON PATIENTS WITH HIP REPLACEMENTS
– can cause dislocation!
Trendelenburg’s test
Place hands on the iliac crests on either side of the pelvis.
Ask the patient to stand on one leg for 30 seconds.
Observe your hands to see which moves up or down.
Normally the iliac crest on the side with the foot off the ground should rise up.
Repeat the test on the opposite side.
The test is deemed positive (abnormal) if the pelvis falls on the side with the foot off
the ground.
This abnormal result suggests weak hip abductors on the contralateral side of the
pelvis.
See this video: www.muhadharaty.com/lecture/1191
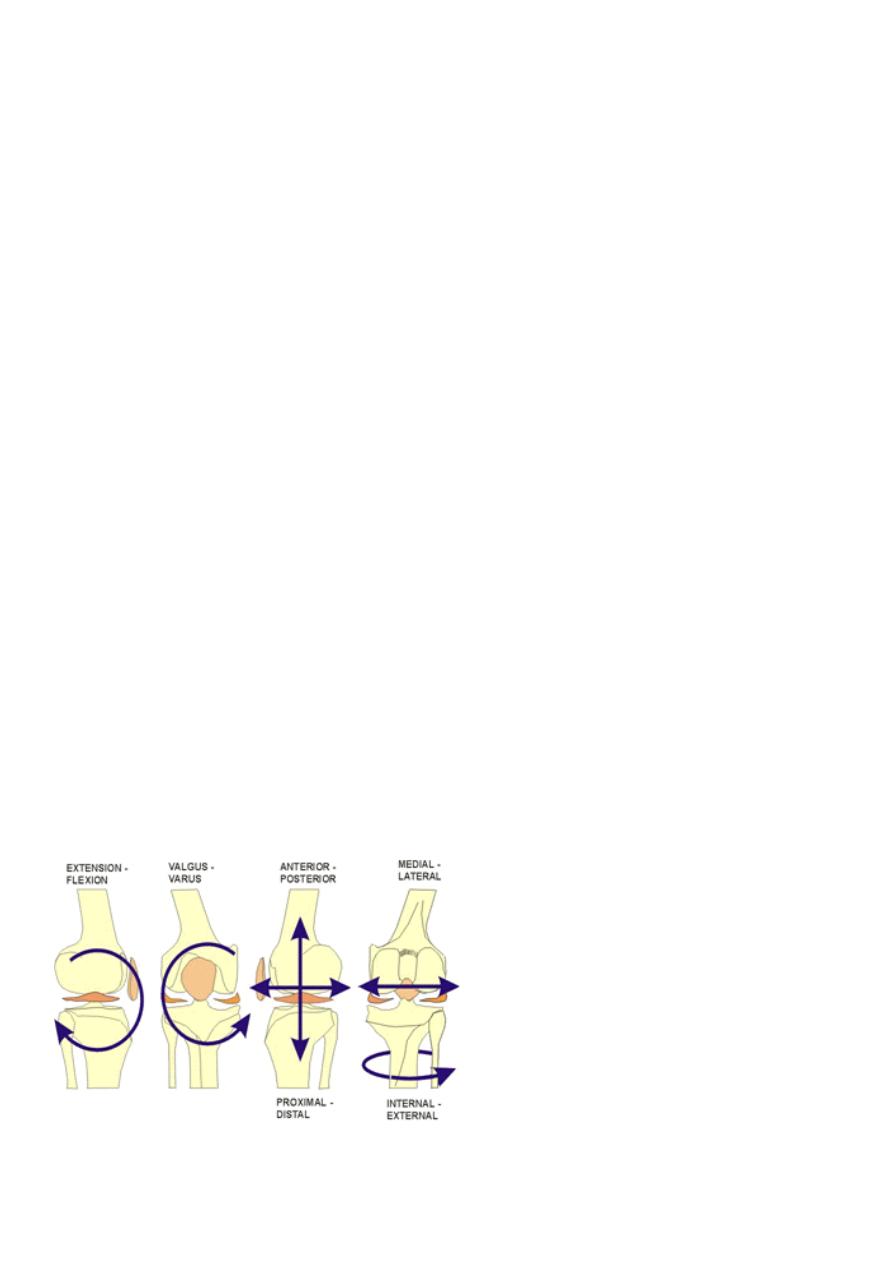
Part8: The knee
Inpection:
Always compare both knee joints.
Deformity.
Redness:
o +ve = septic arthritis or gout.
o -ve = RA, SLE, OA.
11
Palpation:
Tenderness.
Swelling, deformity, atrophy, scar.
Temperature (normally knee joint colder than surrounding tissue).
Movement:
Flexion.
Extension.
Ligaments:
Medical collateral (valgus).
Lateral collateral (varus).
Posterior cruciate ()باتجاه المريض, Anterior cruciate (ضيرملا هاجتا سكع) called drawer
test.
Meniscus:
Medical meniscus prone position + pressure + internal screwing.
Lateral meniscus prone position + pressure + external screwing.
McMurray test:
o To test the medial meniscus, the examiner palpates the postero-medial aspect of the knee while
extending the knee and externally rotating the tibia. A valgus stress is also applied.
o To test the lateral meniscus, the examiner palpates the postero-lateral joint line while extending
the knee and internally rotating the tibia. A varus stress is also applied.
o See this video: https://www.youtube.com/watch?v=lx-6uvKfbBE
Patellar tap test:
It is test for effusion of knee joint.
Called ballottement test.
See this video: www.muhadharaty.com/lecture/1190
12
Part9: The foot
Inspection:
As the examination of joint in general.
Palpation:
Ask the patient to lay on a bed.
Assess temperature & compare between legs ↑ temperature may
indicate inflammatory pathology.
Assess pulses in both feet posterior tibial & dorsalis pedis.
Palpate the achilles tendon assess for thickening or swelling.
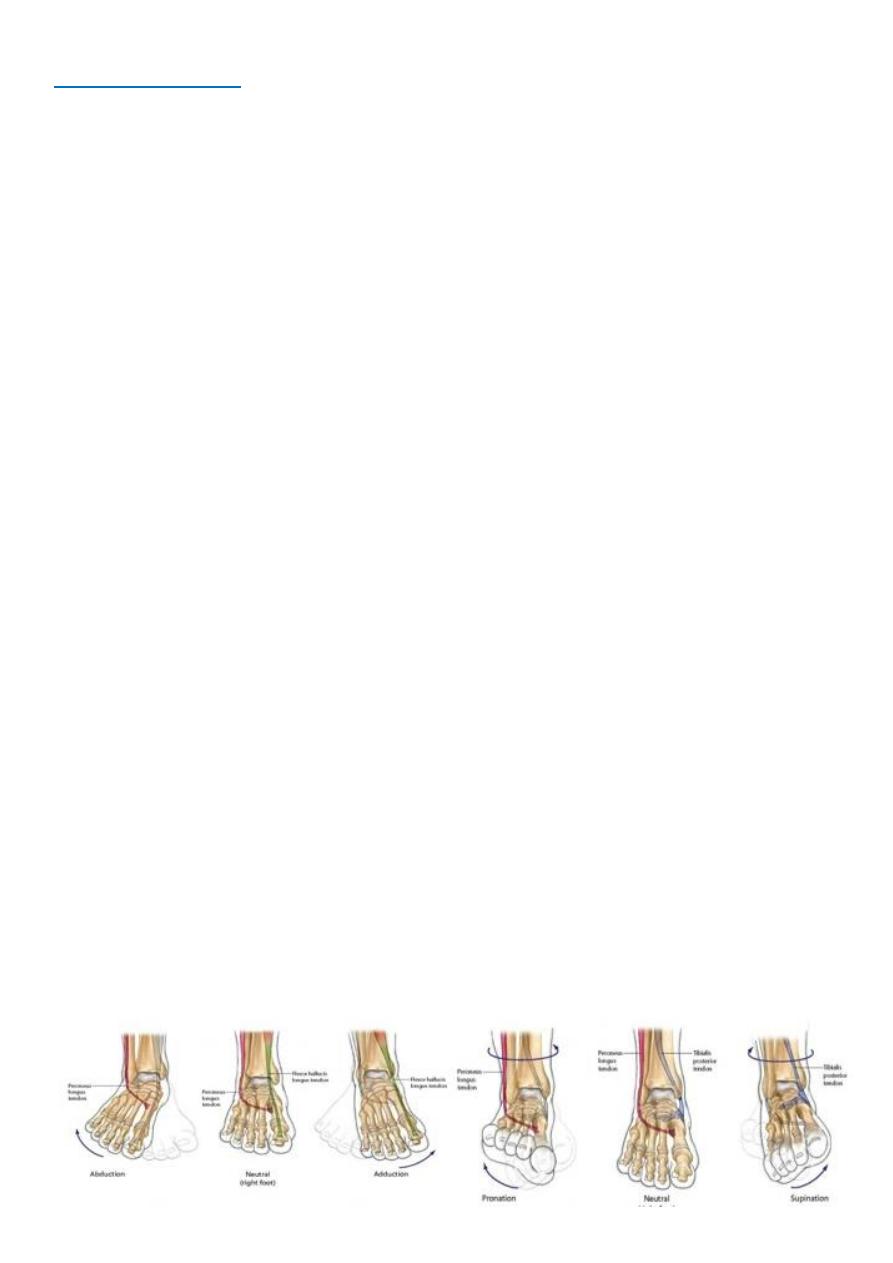
Movement:
Assess each of the following movements actively & passively (feeling for crepitus)
Foot plantiflexion “push your toes downwards, like pushing a car pedal” – 30-40 º
Foot dorsiflexion “point your toes towards your head” – 12-18 º
Foot inversion grasp ankle with one hand & heel with the other – turn sole towards
midline.
Foot eversion grasp ankle with one hand & heel with the other – turn sole away
from midline.
Midtarsal joints hold ankle with one hand whilst moving the tarsus up/down then &
side to side.
Toe flexion “curl up your toes”.
Toe extension “point your toes towards your head”.
Toe adduction “hold this paper between your toes & don’t let me pull it away”.
Toe abduction “spread out your toes as far as you can”.
Thomson’s (Simmond’s) test:
Simmond's test is used to assess for rupture of the achilles tendon.
Ask patient to kneel on a chair with their feet hanging off the edge.
Squeeze each calve in turn.
Normally the foot should plantarflex.
If the achilles tendon is ruptured there will be no movement of the foot.
